Abstract
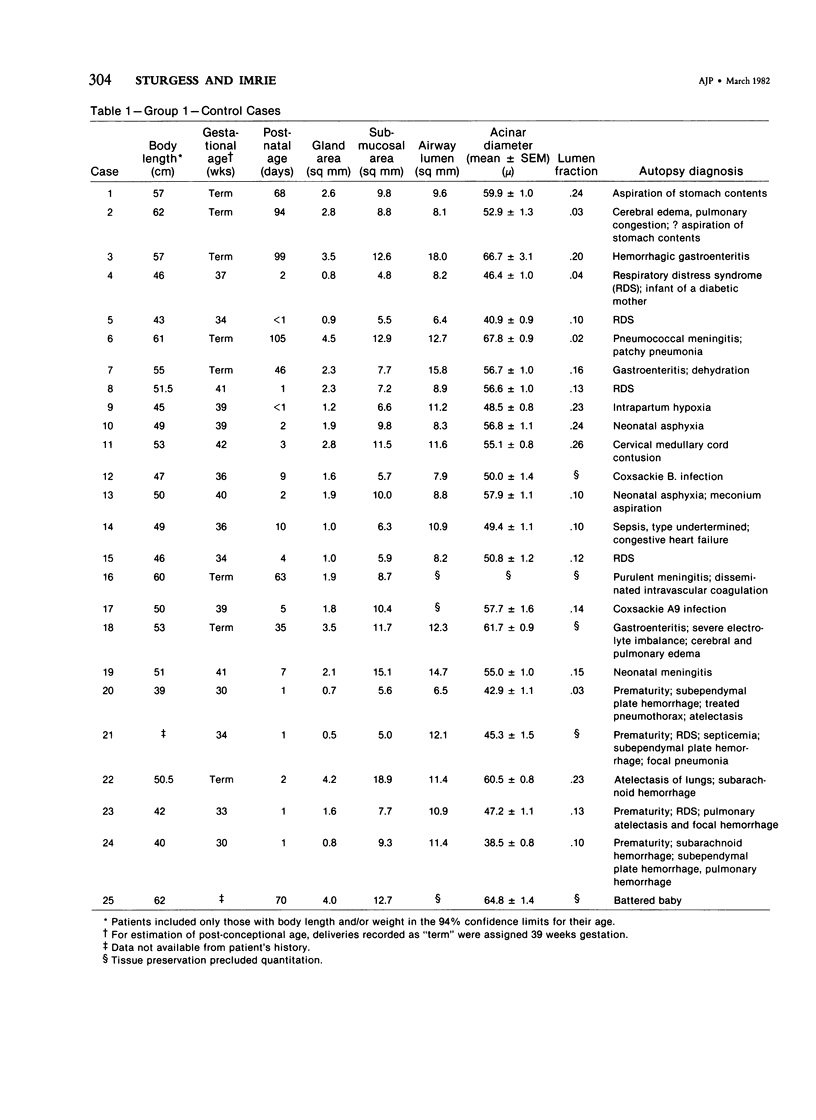
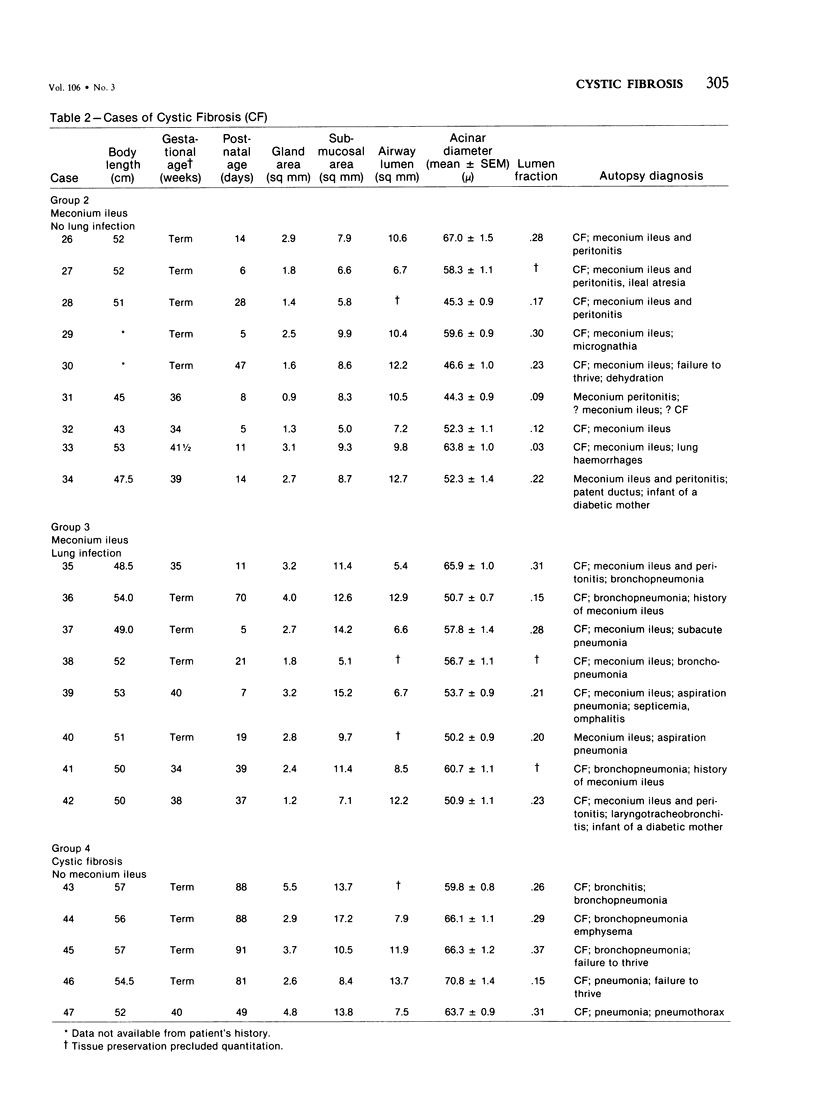
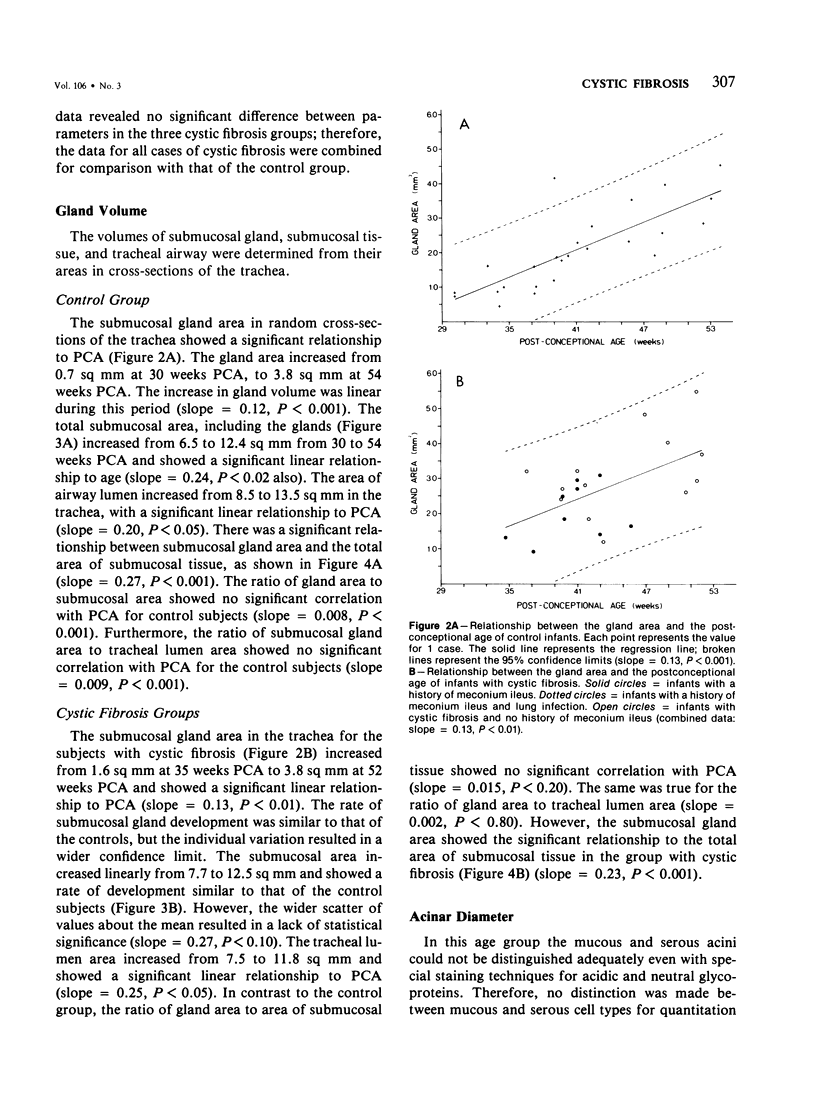
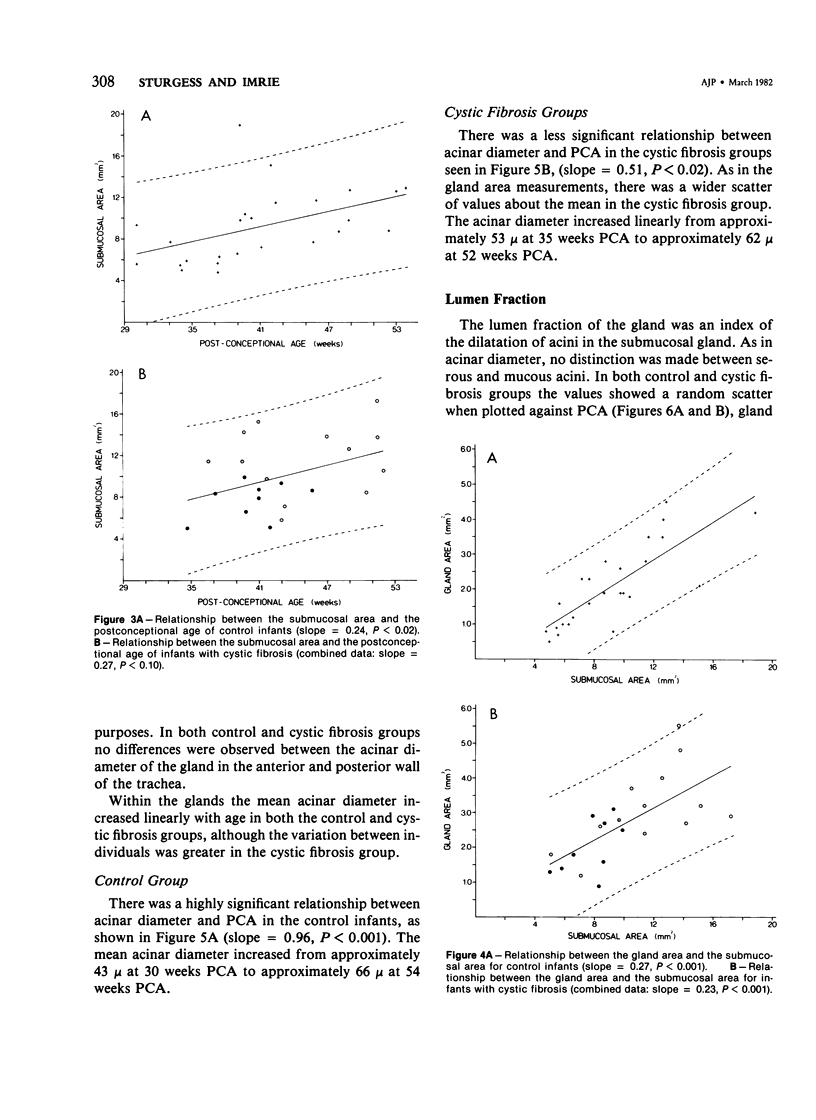
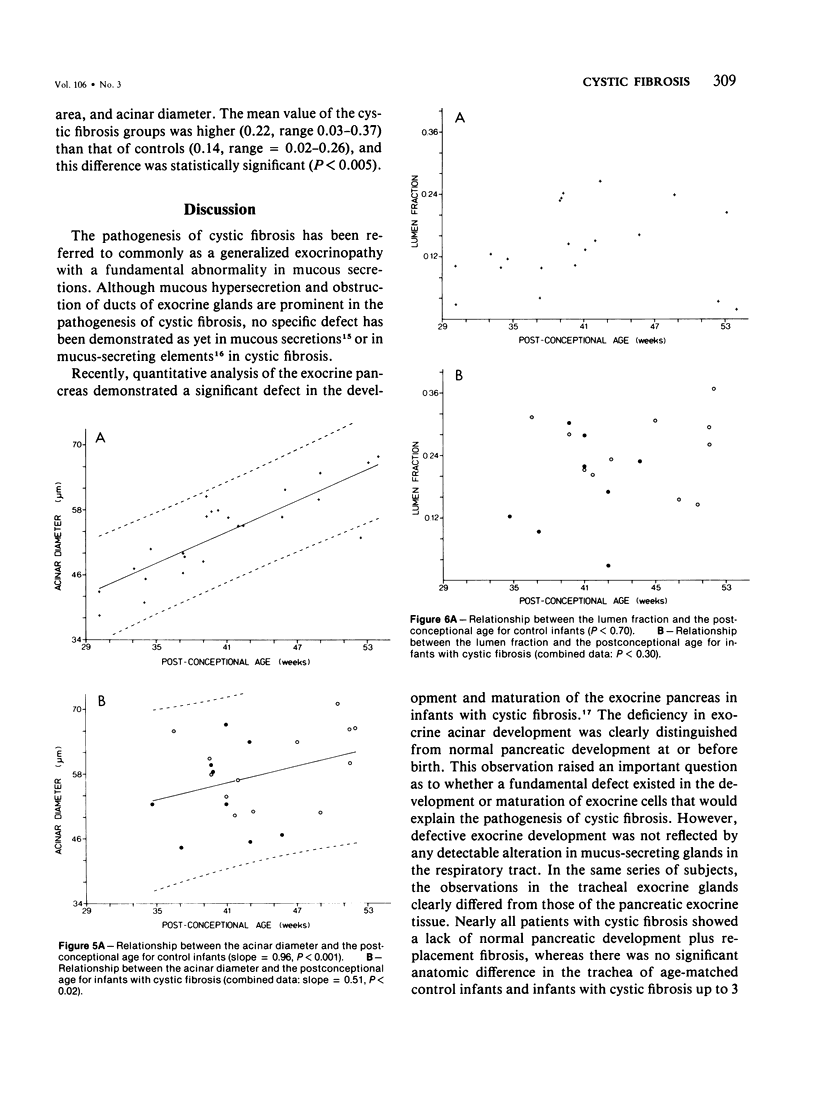
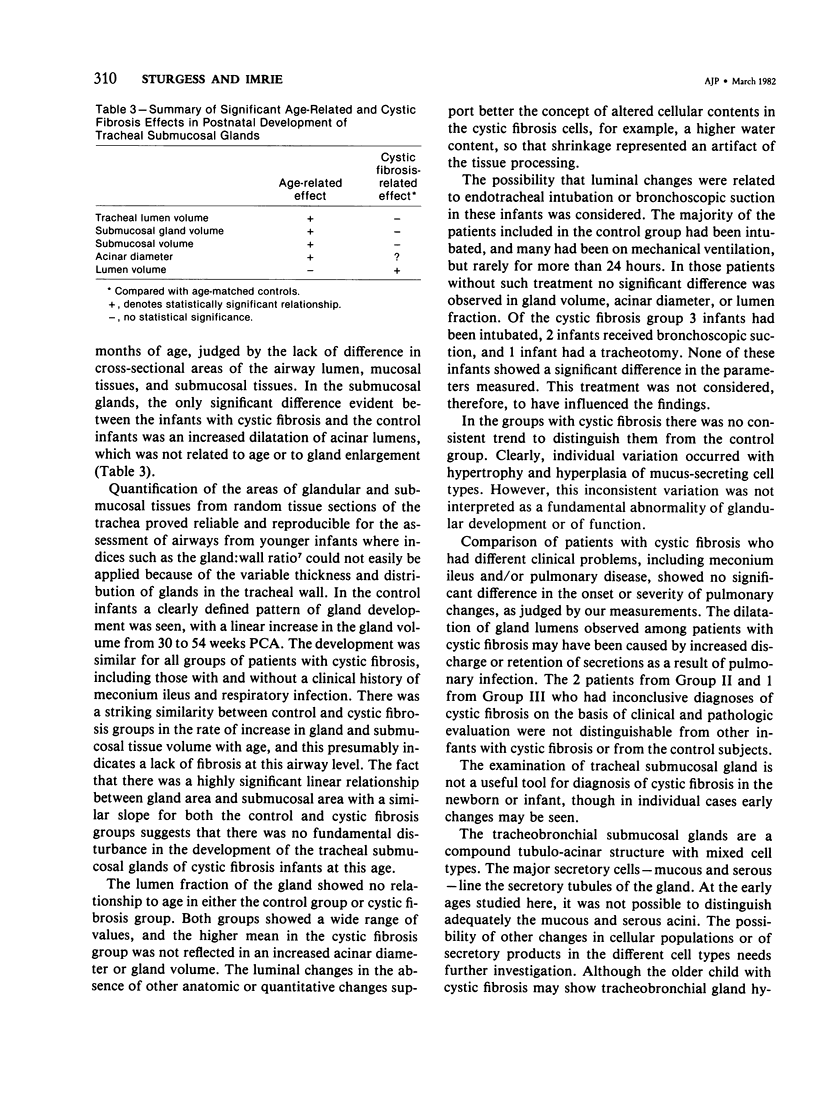
The development of the tracheal submucosal glands has been determined quantitatively in 22 infants with cystic fibrosis and in 25 control infants, all under 4 months of age. In cross-sections of normal trachea significant relationships were found between postconceptional age (PCA) and gland area (P less than 0.001), submucosal area (P less than 0.02), tracheal airway diameter (P less than 0.05), and acinar diameter (P less than 0.001). In infants with cystic fibrosis the pattern of development was similar to that of the control infants. No statistically significant differences were found between three subgroups of infants with cystic fibrosis, which included those with meconium ileus with no lung infection, those with meconium ileus with lung infection, and those with lung infection and no history of meconium ileus. The normal pattern of development of tracheal submucosal glands in infants with cystic fibrosis was in contrast to the deficiency of normal maturation seen in the exocrine pancreas of these infants. The lumen fraction, an index of dilatation of acinar lumina, showed no significant relationship with PCA in either the control group or the group with cystic fibrosis. However, statistically significant dilatation of acini was observed in the tracheal submucosal glands of infants with cystic fibrosis (0.14, P less than 0.005).
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bedrossian C. W., Greenberg S. D., Singer D. B., Hansen J. J., Rosenberg H. S. The lung in cystic fibrosis. A quantitative study including prevalence of pathologic findings among different age groups. Hum Pathol. 1976 Mar;7(2):195–204. doi: 10.1016/s0046-8177(76)80023-8. [DOI] [PubMed] [Google Scholar]
- De Haller R., Reid L. Adult chronic bronchitis. Morphology, histochemistry and vascularisation of the bronchial mucous glands. Med Thorac. 1965;22(6):549–567. [PubMed] [Google Scholar]
- Esterly J. R., Oppenheimer E. H. Observations in cystic fibrosis of the pancreas. 3. Pulmonary lesions. Johns Hopkins Med J. 1968 Feb;122(2):94–101. [PubMed] [Google Scholar]
- Field W. E., Davey E. N., Reid L., Roe F. J. Bronchial mucus gland hypertrophy: its relation to symptoms and environment. Br J Dis Chest. 1966 Apr;60(2):66–80. doi: 10.1016/s0007-0971(66)80002-5. [DOI] [PubMed] [Google Scholar]
- Field W. E. Mucous gland hypertrophy in babies and children aged 15 years or less. Br J Dis Chest. 1968 Jan;62(1):11–18. doi: 10.1016/s0007-0971(68)80025-7. [DOI] [PubMed] [Google Scholar]
- Imrie J. R., Fagan D. G., Sturgess J. M. Quantitative evaluation of the development of the exocrine pancreas in cystic fibrosis and control infants. Am J Pathol. 1979 Jun;95(3):697–708. [PMC free article] [PubMed] [Google Scholar]
- Matsuba K., Thurlbeck W. M. A morphometric study of bronchial and bronchiolar walls in children. Am Rev Respir Dis. 1972 Jun;105(6):908–913. doi: 10.1164/arrd.1972.105.6.908. [DOI] [PubMed] [Google Scholar]
- Oppenheimer E. H., Esterly J. R. Cystic fibrosis of the pancreas. Morphologic findings in infants with and without diagnostic pancreatic lesions. Arch Pathol. 1973 Sep;96(3):149–154. [PubMed] [Google Scholar]
- REID L. Measurement of the bronchial mucous gland layer: a diagnostic yardstick in chronic bronchitis. Thorax. 1960 Jun;15:132–141. doi: 10.1136/thx.15.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid L., de Haller R. The bronchial mucous glands--their hypertrophy and change in intracellular mucus. Bibl Paediatr. 1967;86:195–199. [PubMed] [Google Scholar]
- Sturgess J., Reid L. Secretory activity of the human bronchial mucous glands in vitro. Exp Mol Pathol. 1972 Jun;16(3):362–381. doi: 10.1016/0014-4800(72)90011-1. [DOI] [PubMed] [Google Scholar]
- THURLBECK W. M., BENJAMIN B., REID L. Development and distribution of mucous glands in the foetal human trachea. Br J Dis Chest. 1961 Apr;55:54–64. doi: 10.1016/s0007-0971(61)80002-8. [DOI] [PubMed] [Google Scholar]
- di Sant'Agnese P. A., Davis P. B. Research in cystic fibrosis (second of three parts). N Engl J Med. 1976 Sep 2;295(10):534–541. doi: 10.1056/NEJM197609022951005. [DOI] [PubMed] [Google Scholar]


