Abstract
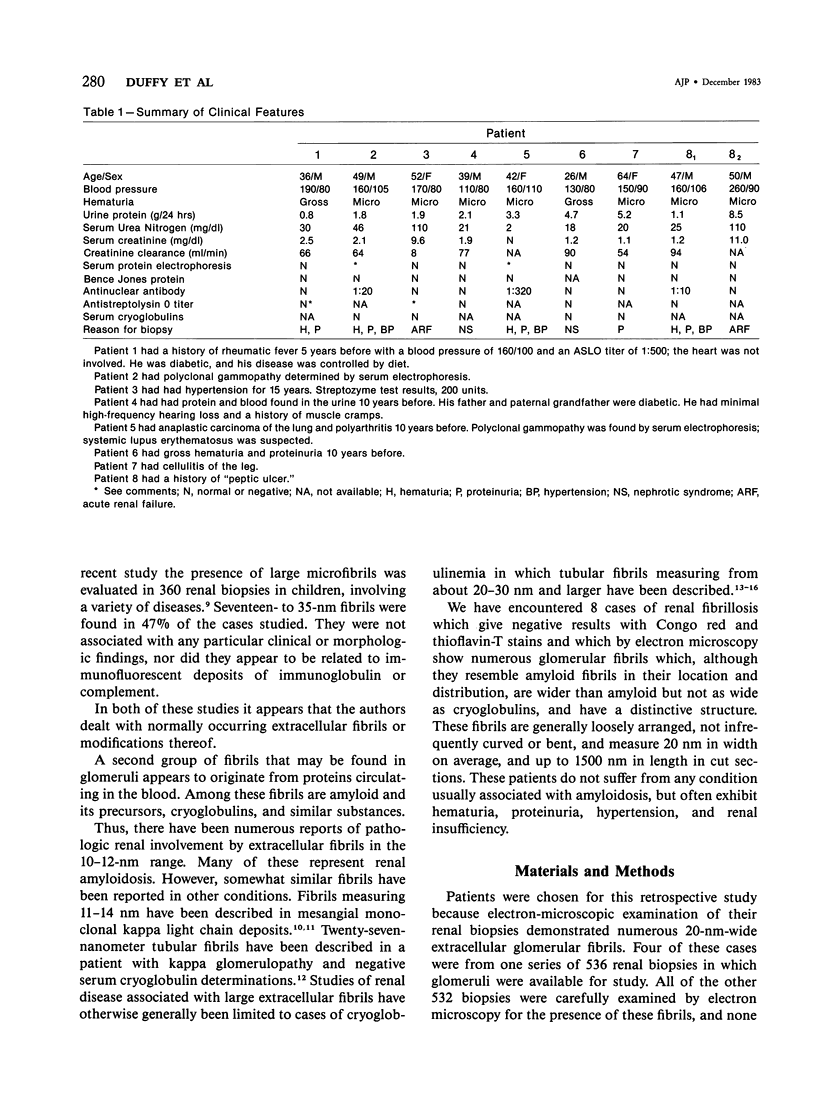
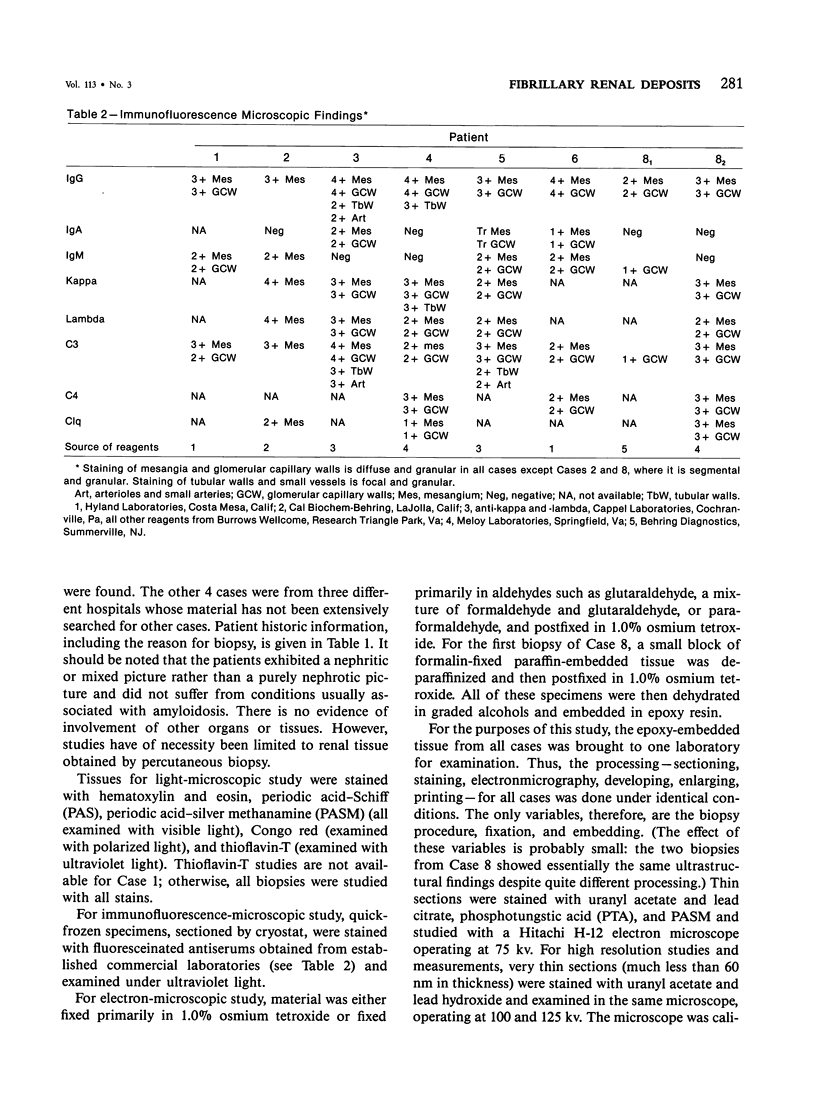
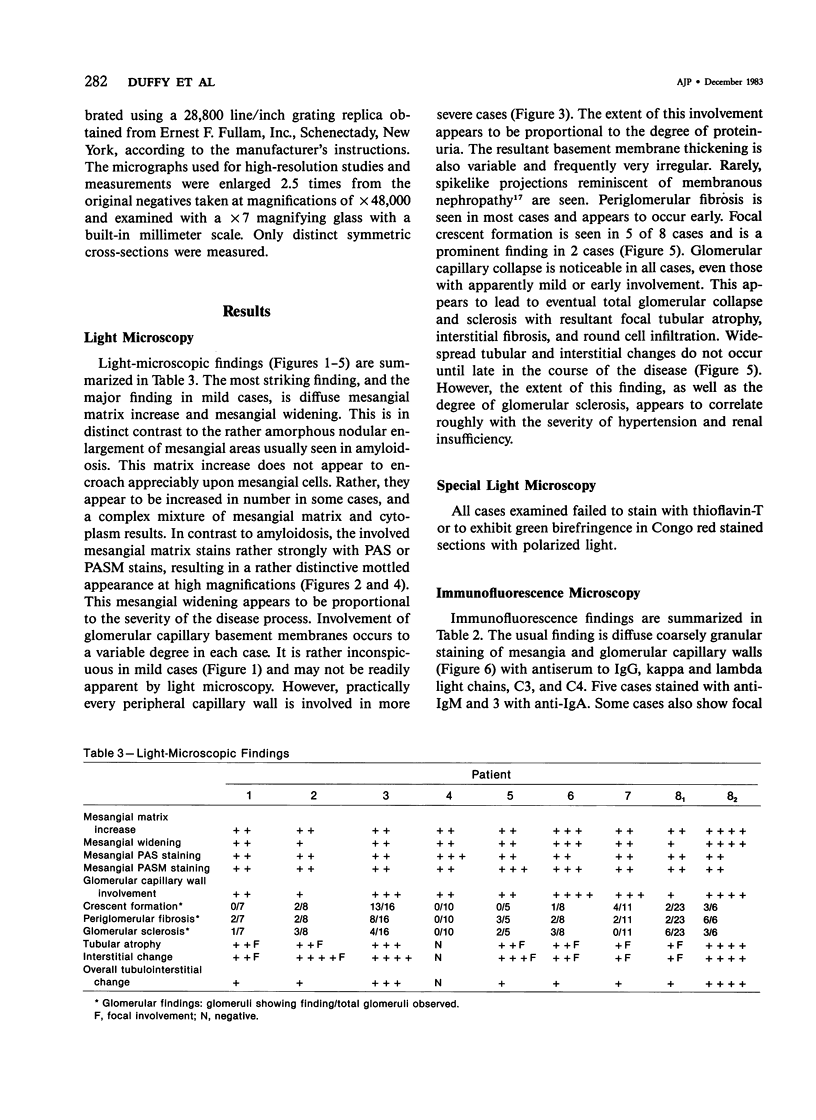
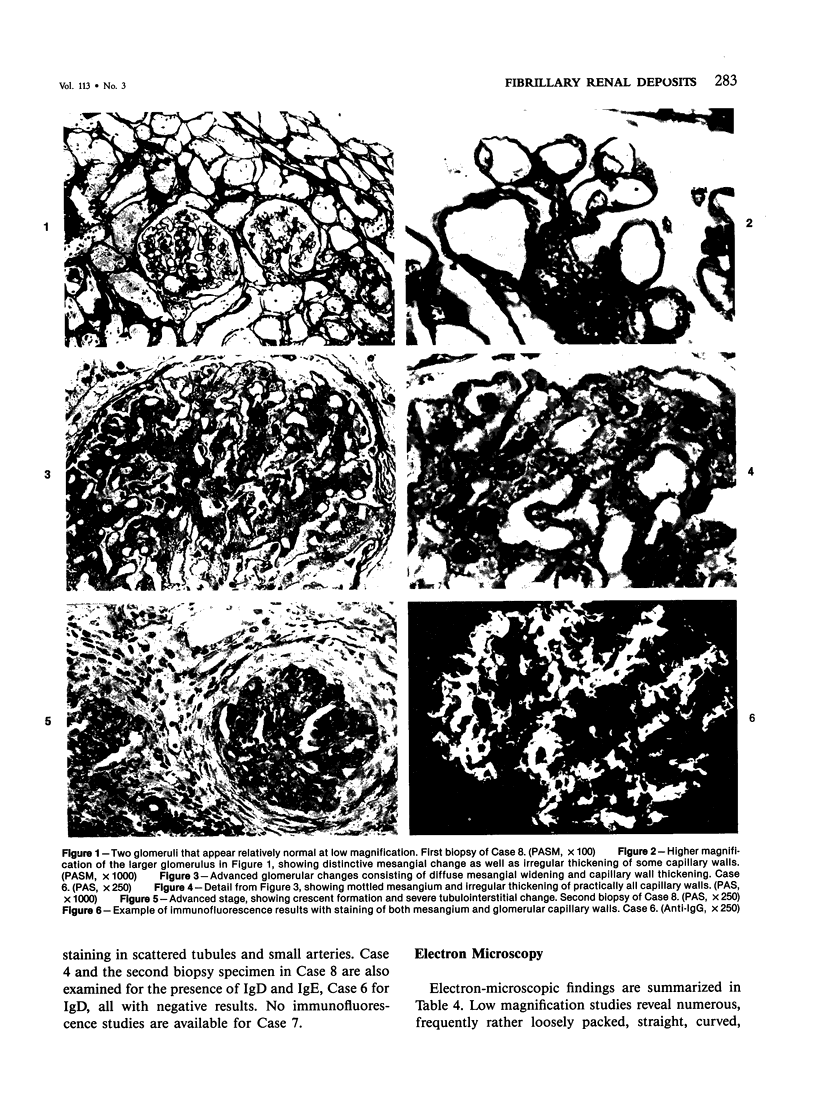
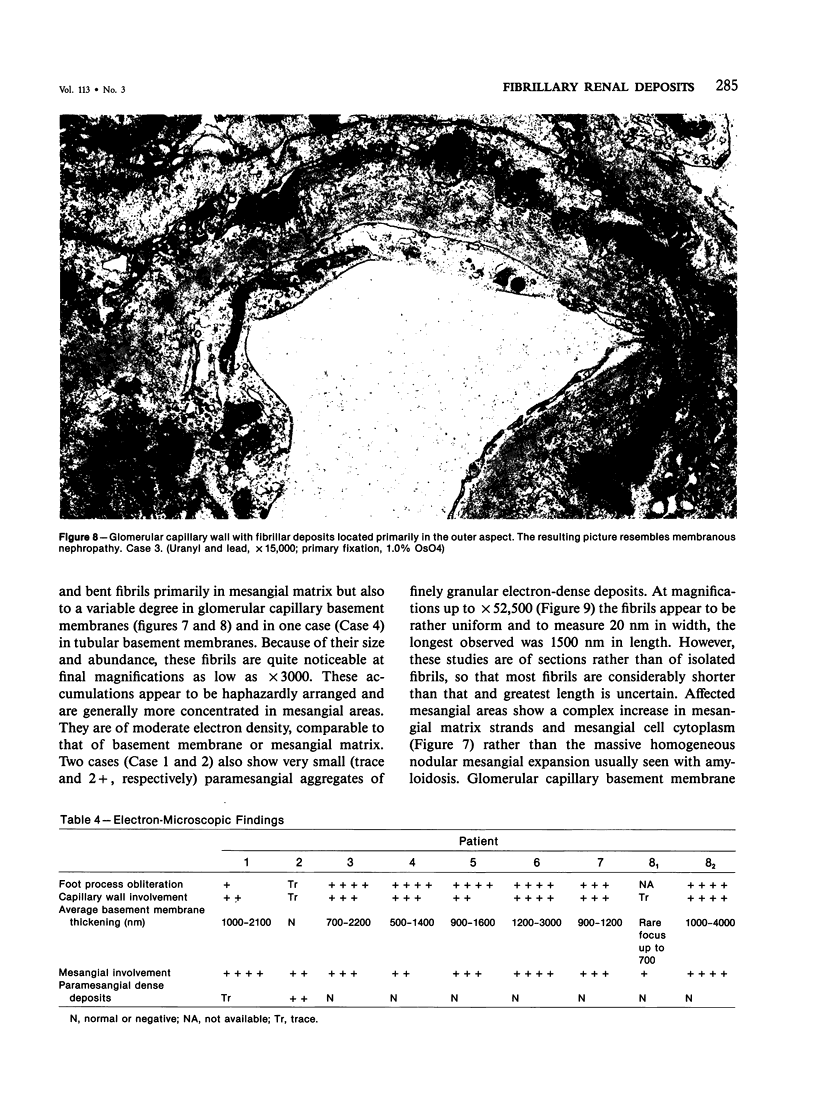
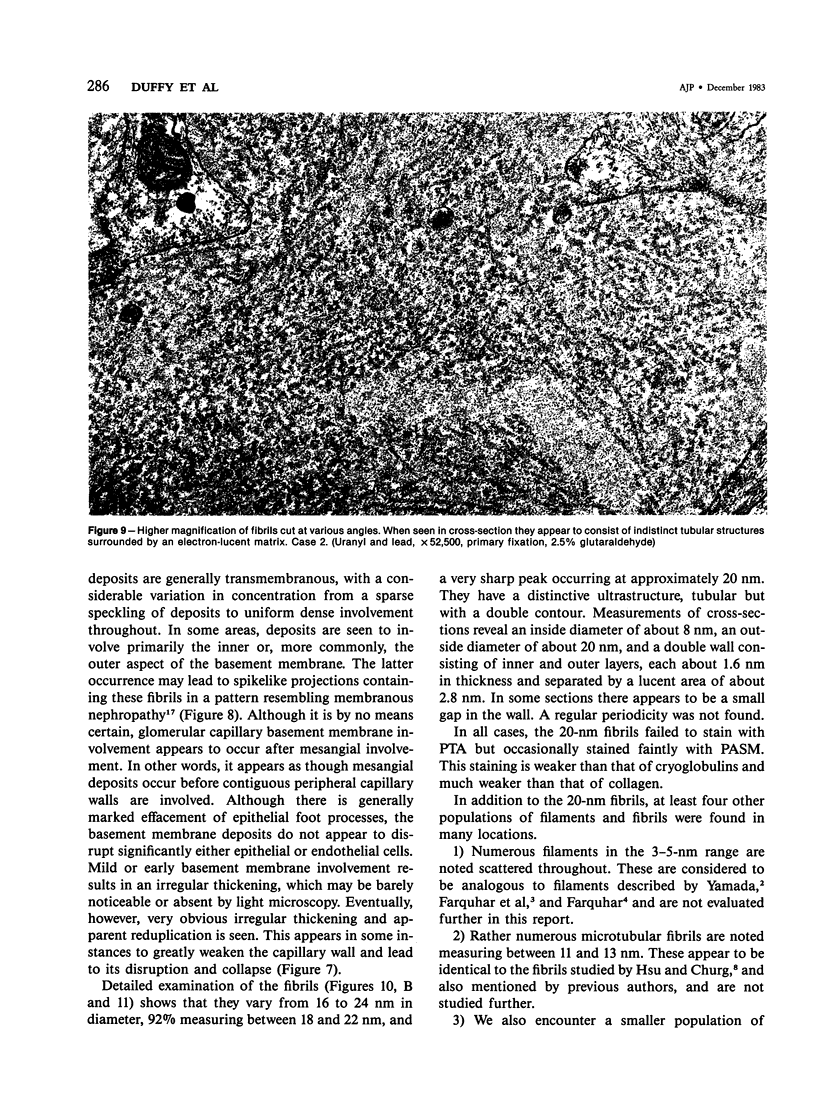
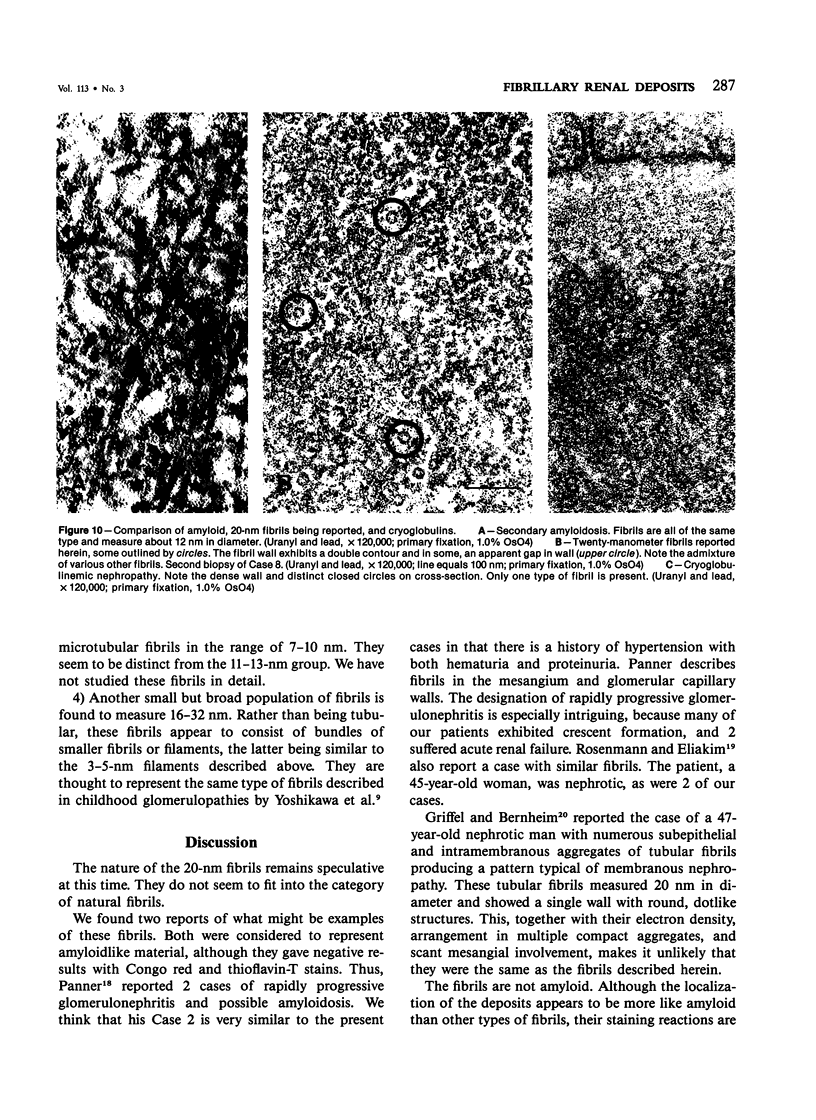
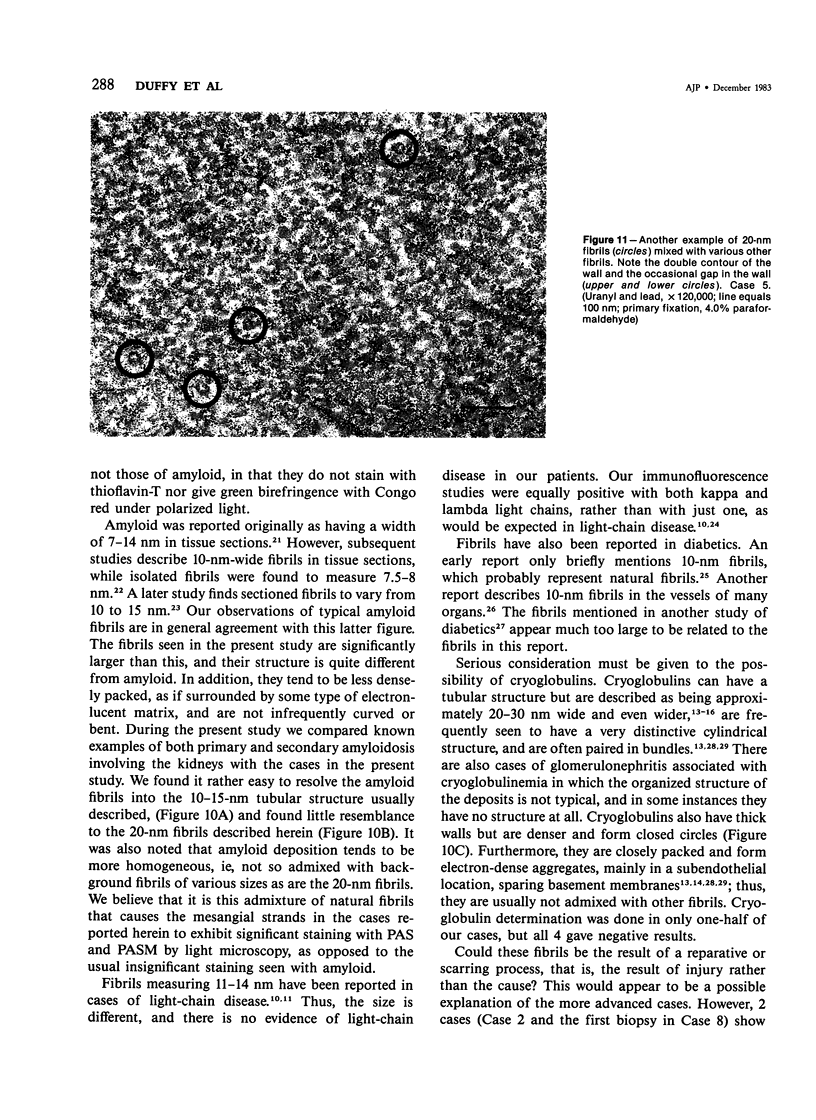
Fibrillary renal deposits and nephritis. The authors have studied 8 patients whose glomeruli contain abundant fibrils in their mesangial matrix and basement membranes. Although the location of these fibrils is very similar to that of amyloid, they are about twice the size of amyloid fibrils, averaging 20 nm in width, and fail to react as amyloid does with special stains. Immunofluorescence-microscopic studies are usually positive with antiserums to IgG, often IgM, and in some cases IgA, and also kappa and lambda light chains, C3, and C4. The fibrils are associated with diffuse mesangial widening and increased mesangial matrix strands. Although peripheral glomerular capillary walls appear to be spared initially, their eventual involvement leads to glomerular capillary collapse and glomerular obsolescence. Crescent formation occurred in 5 cases, focally in 3 and diffusely in 2. Tubular basement membrane involvement was seen in 1 case. These patients exhibit hematuria, and proteinuria, and often hypertension and renal insufficiency. Proteinuria was in the nephrotic range in 3 patients in whom involvement of glomerular capillary basement membranes was extensive. Unless electron microscopy is applied to renal biopsies, these cases may be considered to represent mesangiocapillary or rapidly progressive glomerulonephritis, or amyloidosis. The nature of these fibrils is as yet not determined. It is likely that they have been called "atypical amyloidosis" in the past.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ainsworth S. K., Hirsch H. Z., Brackett N. C., Jr, Brissie R. M., Williams A. V., Jr, Hennigar G. R. Diabetic glomerulonephropathy: histopathologic, immunofluorescent, and ultrastructural studies of 16 cases. Hum Pathol. 1982 May;13(5):470–478. doi: 10.1016/s0046-8177(82)80030-0. [DOI] [PubMed] [Google Scholar]
- COHEN A. S., CALKINS E. Electron microscopic observations on a fibrous component in amyloid of diverse origins. Nature. 1959 Apr 25;183(4669):1202–1203. doi: 10.1038/1831202a0. [DOI] [PubMed] [Google Scholar]
- FARQUHAR M. G., WISSIG S. L., PALADE G. E. Glomerular permeability. I. Ferritin transfer across the normal glomerular capillary wall. J Exp Med. 1961 Jan 1;113:47–66. doi: 10.1084/jem.113.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraggiana T., Parolini C., Previato G., Lupo A. Light and electron microscopic findings in five cases of cryoglobulinemic glomerulonephritis. Virchows Arch A Pathol Anat Histol. 1979;384(1):29–44. doi: 10.1007/BF00427149. [DOI] [PubMed] [Google Scholar]
- Feiner H., Gallo G. Ultrastructure in glomerulonephritis associated with cryoglobulinemia. A report of six cases and review of the literature. Am J Pathol. 1977 Jul;88(1):145–162. [PMC free article] [PubMed] [Google Scholar]
- Franklin E. C., Zucker-Franklin D. Current concepts of amyloid. Adv Immunol. 1972;15:249–304. doi: 10.1016/s0065-2776(08)60687-2. [DOI] [PubMed] [Google Scholar]
- Frederickson R. G., Morse D. E., Low F. N. High-voltage electron microscopy of extracellular fibrillogenesis. Am J Anat. 1977 Sep;150(1):1–33. doi: 10.1002/aja.1001500102. [DOI] [PubMed] [Google Scholar]
- Gallo G. R., Feiner H. D., Katz L. A., Feldman G. M., Correa E. B., Chuba J. V., Buxbaum J. N. Nodular glomerulopathy associated with nonamyloidotic kappa light chain deposits and excess immunoglobulin light chain synthesis. Am J Pathol. 1980 Jun;99(3):621–644. [PMC free article] [PubMed] [Google Scholar]
- Griffel B., Bernheim J. Glomerular deposits in idiopathic membranous glomerulopathy. Arch Pathol Lab Med. 1980 Jan;104(1):56–57. [PubMed] [Google Scholar]
- Hsu H. C., Churg J. Glomerular microfibrils in renal disease: a comparative electron microscopic study. Kidney Int. 1979 Oct;16(4):497–504. doi: 10.1038/ki.1979.155. [DOI] [PubMed] [Google Scholar]
- Linder J., Croker B. P., Vollmer R. T., Shelburne J. Systemic kappa light-chain deposition. An ultrastructural and immunohistochemical study. Am J Surg Pathol. 1983 Jan;7(1):85–93. doi: 10.1097/00000478-198301000-00009. [DOI] [PubMed] [Google Scholar]
- Ogihara T., Saruta T., Saito I., Abe S., Ozawa Y., Kato E., Sakaguchi H. Finger print deposits of the kidney in pure monoclonal IgG kappa cryoglobulinemia. Clin Nephrol. 1979 Oct;12(4):186–190. [PubMed] [Google Scholar]
- Panner B. J. Rapidly progressive glomerulonephritis and possible amyloidosis. Arch Pathol Lab Med. 1980 Nov;104(11):603–609. [PubMed] [Google Scholar]
- Podack E. R., Müller-Eberhard H. J., Horst H., Hoppe W. Membrane attach complex of complement (MAC): three-dimensional analysis of MAC-phospholipid vesicle recombinants. J Immunol. 1982 May;128(5):2353–2357. [PubMed] [Google Scholar]
- Podack E. R., Tschopp J. Polymerization of the ninth component of complement (C9): formation of poly(C9) with a tubular ultrastructure resembling the membrane attack complex of complement. Proc Natl Acad Sci U S A. 1982 Jan;79(2):574–578. doi: 10.1073/pnas.79.2.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenmann E., Eliakim M. Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977;18(5):301–308. doi: 10.1159/000180846. [DOI] [PubMed] [Google Scholar]
- Schwartz M. M., Lewis E. J. The quarterly case: nephrotic syndrome in a middle-aged man. Ultrastruct Pathol. 1980 Oct-Dec;1(4):575–582. doi: 10.3109/01913128009140563. [DOI] [PubMed] [Google Scholar]
- Shirahama T., Cohen A. S. High-resolution electron microscopic analysis of the amyloid fibril. J Cell Biol. 1967 Jun;33(3):679–708. doi: 10.1083/jcb.33.3.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohar E., Ravid M., Ben-Shaul Y., Reshef T., Gafni J. Diabetic fibrillosis. A report of three cases. Am J Med. 1970 Jul;49(1):64–69. doi: 10.1016/s0002-9343(70)80114-0. [DOI] [PubMed] [Google Scholar]
- Stoebner P., Renversez J. C., Groulade J., Vialtel P., Cordonnier D. Ultrastructural study of human IgG and IgG-IgM crystalcryoglobulins. Am J Clin Pathol. 1979 Apr;71(4):404–410. doi: 10.1093/ajcp/71.4.404. [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Churg J., Grishman E., Mautner W., Dachs S. The Mesangium of the Renal Glomerulus: Electron Microscopic Studies of Pathologic Alterations. Am J Pathol. 1963 Oct;43(4):555–578. [PMC free article] [PubMed] [Google Scholar]
- Tarantino A., De Vecchi A., Montagnino G., Imbasciati E., Mihatsch M. J., Zollinger H. U., Di Belgiojoso G. B., Busnach G., Ponticelli C. Renal disease in essential mixed cryoglobulinaemia. Long-term follow-up of 44 patients. Q J Med. 1981;50(197):1–30. [PubMed] [Google Scholar]
- Tschopp J., Müller-Eberhard H. J., Podack E. R. Formation of transmembrane tubules by spontaneous polymerization of the hydrophilic complement protein C9. Nature. 1982 Aug 5;298(5874):534–538. doi: 10.1038/298534a0. [DOI] [PubMed] [Google Scholar]
- Tschopp J., Podack E. R. Membranolysis by the ninth component of human complement. Biochem Biophys Res Commun. 1981 Jun 16;100(3):1409–1414. doi: 10.1016/0006-291x(81)91981-1. [DOI] [PubMed] [Google Scholar]
- Tubbs R. R., Gephardt G. N., McMahon J. T., Hall P. M., Valenzuela R., Vidt D. G. Light chain nephropathy. Am J Med. 1981 Aug;71(2):263–269. doi: 10.1016/0002-9343(81)90127-3. [DOI] [PubMed] [Google Scholar]
- YAMADA E. The fine structure of the renal glomerulus of the mouse. J Biophys Biochem Cytol. 1955 Nov 25;1(6):551–566. doi: 10.1083/jcb.1.6.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa N., Cameron A. H., White R. H., Standring D. M. Microfibrils in glomerulopathies of children: an ultrastructural study. J Pathol. 1982 Feb;136(2):123–131. doi: 10.1002/path.1711360206. [DOI] [PubMed] [Google Scholar]
- Zollinger H. U., Mihatsch M. J. The value of electron microscopy in diagnostic pathology. Case 2. Ultrastruct Pathol. 1980 Jan-Mar;1(1):79–83. doi: 10.3109/01913128009141400. [DOI] [PubMed] [Google Scholar]