Abstract
Background
Motivational interviewing is a technique used to promote change in addictive behaviour, initially used to treat alcoholism. Despite this, its effectiveness has not been sufficiently demonstrated for giving up smoking.
Aim
The aim of the study was to establish whether motivational interviewing, compared with anti-smoking advice, is more effective for giving up the habit.
Design of study
Randomised controlled trial.
Setting
Primary care in Albecete, Spain.
Method
Random experimental study of 200 smokers assigned to two types of interventions: anti-smoking advice (n = 86) and motivational interviewing (n = 114). Subjects in both groups were offered bupropion when nicotine dependency was high (Fagerström score >7). The success rate was evaluated by intention to treat; point prevalence abstinence was measured 6 and 12 months post intervention by personal testimony, confirmed by means of CO-oximetry (value < 6ppm).
Results
The measure of effectiveness of the treatment for giving up smoking after both 6 and 12 months, showed that the motivational interviewing action was 5.2 times higher than anti-smoking advice (18.4 % compared to 3.4%; 95% confidence interval = 1.63 to 17.13).
Conclusion
The results of our study show that motivational interviewing is more effective than brief advice for giving up smoking.
Keywords: clinical trial, motivation, motivational interviewing, psychological techniques, smoking, treatment effectiveness
INTRODUCTION
Smoking is the main cause of preventable death in developed countries.1 The natural history of untreated smoking involves an increased probability of cardiovascular, respiratory and neoplastic diseases. Every year, tobacco causes 3.5 million deaths throughout the world.
In Spain, every year 56 000 people die from diseases directly related to smoking.2 According to the 2001 National Public Health Survey, the prevalence of smoking in the Spanish population over 16 years of age was 34.4% in that year. Compared with the figures obtained in 1987, when the prevalence was 38.4%, a slight drop in smoking in Spain can be found.3 In men, smoking has gone down from 55% in 1987 to 42.1% in 2001. During the same period the habit in women increased from 23 to 27.2%.
Within the sphere of primary health care, treatment of tobacco addiction is one of the main challenges, in both primary and secondary prevention.
However, since utilisation by the general population of primary healthcare consultations is high (it is estimated that 75% of Spaniards consult their doctor at least once a year), with average frequency of 5.5 consultations per person yearly, this gives the GP and the health service numerous opportunities to deal with tobacco addiction.4
There are many types of interventions to aid in smoking cessation:5 anti-smoking advice given by doctors, structured actions in clinic consultations, self-help materials, nicotine substitutes, antidepressants and anxiolytics, aversion therapies, acupuncture and hypnotherapy.
How this fits in
Smoking is the main cause of preventable death in developed countries. Motivational interviewing is a useful tool for promoting change in addictive behaviour, although there is not sufficient proof of its effectiveness for smoking cessation. Evidence from this trial indicates that motivational interviewing may be a useful intervention for giving up smoking in primary healthcare settings.
Research into smoking by primary health care has, given its feasibility, traditionally been based on medical anti-smoking advice. It has been shown that brief medical advice is somewhat effective in promoting smoking cessation. Pooled data from 17 studies of brief advice versus no advice (or routine care) revealed a small but significant increase in the odds of quitting (odds ratio [OR] = 1.74, 95% confidence interval [CI] = 1.48 to 2.05) following brief advice. This equates to an absolute difference in the quit rate of 2.5% between those receiving physician advice and those receiving routine care only. More intensive advice may result in slightly higher rates of quitting. There is insufficient evidence to determine whether use of aids or providing follow-up support after offering the advice increases the quit rates any further.6
The apparent low efficacy is offset by the high number of smokers who may receive this treatment action, through minimum effort on the part of the physician.
More recently, recommendations from various agencies (WHO 20017 and CDC 20008) indicate the need to include motivational interviewing (MI) in the treatment of smoking.
MI, a technique described by Miller in 1983, initially used for treating alcoholism,9,10 is useful for promoting change in addictive behaviour. It is a patient-centred medical interview focused on examination and resolution of ambivalences regarding unhealthy behaviours or habits. The basic idea of this technique is that it is the patient who reflects on and expresses their problems and desire to change. The MI techniques allow the GP to bring about an increase in the patient's motivation, taking into account what their base motivational level is and always respecting their final decisions without penalising them. Prochaska11 et al, studying processes of change in people who had given up smoking, found that they were going through a series of stages, each one characterised by a particular mental attitude and level of motivational readiness. At present, the process of giving up smoking is studied mainly by following the model that these authors put forward. Most of the studies published using MI as a tool in the treatment of addictive behaviour deal with alcohol dependence. Nonetheless, numerous studies have applied the technique to tobacco addiction, though few of them compare effectiveness of MI with brief advice.12
The aim of the current study is to compare the effectiveness in smokers of three motivational interviews, versus anti-smoking advice for smoking cessation, at 6 and 12 months post intervention.
METHOD
This is a randomised experimental study to assess two actions: advice versus MI (Figure 1).
Figure 1.
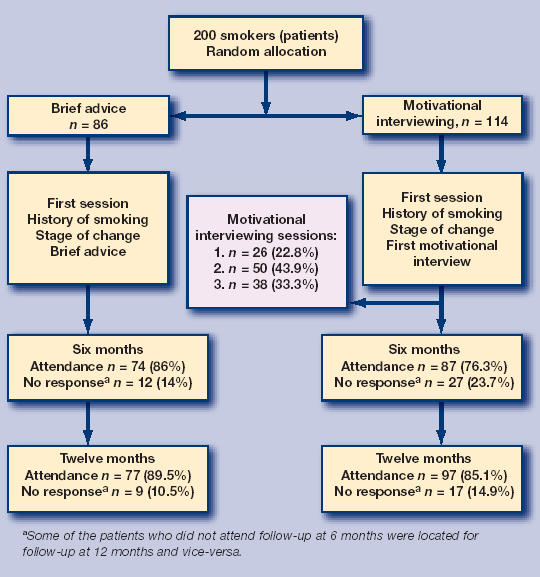
Flow diagram of trial.
Physicians
The two categories of interventions, as well as all initial and follow-up data collection and measures, were conducted by five family physicians working within the Spanish Public Health Care System in two different Health Centres in the city of Albacete. Both Centres attend to an urban population of approximately 48 000 persons each, 13% of whom are older than 65 years of age. The five doctors are members of the permanent staff in their respective centres, each one assigned to attend a roster of 1900 patients over the age of 14 years.
The five GPs had been given specific training in MI techniques by means of role-playing and video recordings, in order to establish and combine the basic contents, both of the brief individual action (anti-smoking advice) and the MI action.
Participants
All subjects in this study were patients on the rosters of the five physician–investigators described above. 200 active smoker patients between the ages of 15 and 75 years were recruited during regular visits to their respective GPs, for whatever reason. None of the subjects had been recipients of pre-selection cards nor publicity regarding the trial, nor were they chosen for the study with respect to any particular pathology.
A smoker was considered to be any person who replied ‘yes’ to the question: Do you smoke?
Patients were recruited over a period of 23 months; informed consent was requested from all those taking part in the trial. Exclusion criteria were existence of severe psychiatric disorder, a terminal illness or drug-addiction, or age <15 or >75 years.
The smokers participating in the study were assessed over a total period of 1 year, and follow-ups of the effectiveness of the interventions were conducted after 6 and 12 months post intervention.
Sample size calculation
Calculation of the sample size was made by considering an effectiveness in giving up smoking of 5% with anti-smoking advice and of 20% with MI, that is to say a relative effectiveness four times higher for MI over advice. Two groups of 100 subjects were necessary (α risk level of 0.05% and 90% capacity to detect the difference existing between groups).
Randomisation sequence generation
The patients were randomly assigned to either one of the actions groups by means of a non-block table of random numbers. The assignment sequence established resulted in one group of 86 patients receiving brief advice and another of 114 subjects assigned to MI.
Two hundred non-transparent sealed envelopes containing the interventions (either brief advice or MI) were prepared. Before the start of daily consultations, the GPs conducting the interventions would extract one of the envelopes, not knowing the type of action it contained. The first smoker patient who attended the consultation would be offered the possibility of taking part in the study. If they accepted and signed the informed consent form, the envelope would be opened, upon which the GP would learn of the patient's group assignment.
Intervention
After opening the envelope, patients in both groups were given verbal and written information about the study's purpose, aims and procedures.
The personal details of each patient were then collected (age, sex, educational level, employment), variables relating to tobacco consumption (presence of disease related to tobacco consumption — chronic obstructive pulmonary disease (COPD) and ischaemic heart disease — number of cigarettes smoked a day, age when the patient started smoking, years smoking) and stage of change, according to the five stages of change described by Prochaska-DiClemente:11 precontemplative, contemplative, action, maintenance and relapse.
The degree of nicotine dependency was assessed by Fagerström's test.13 Depending on the result that each smoker gives to each question, a certain mark is obtained, that may vary from 0–10 points.
A degree of slight dependency is considered when the test varies from 0 to 3 points; moderate dependency is from 4 to 6 points; a severe degree of dependency is 7 points or over.
In all patients, the level of carbon monoxide in the air expired at the start of the study was measured by means of a micro smokerlyser carbon monoxide (CO) monitor14 (Bedfont Technical Instruments Ltd). CO values were used as abstinence markers, 6 and 12 months after the action. Figures of ≥10 ppm of CO indicate smokers; 6–10 ppm sporadic smokers, and <6 ppm, non-smokers.15
In the same first consultation, following data collection and CO measurements, the action assigned to each subject case was carried out.
Patients receiving anti-smoking advice were given one intervention session consisting of a personal talk by their physician, lasting approximately 3 minutes. The dangers of smoking were explained, as well as the advantages of giving it up. The information given in all advice consultations was the same and in accordance with the recommendations of the Smoking Department of the Spanish Pneumology and Chest Surgery Association (SEPAR).16
Patients assigned to MI were given the first of a total of three 20–minute interviews conducted in the physician's office. There was no established protocol for time lapse between interviews; rather, appointments for the subsequent session were set up with the GP at the patient's convenience.
Patients in both intervention groups showing high nicotine-dependency (Fagerström's test scores of ≥7), were offered the possibility of concurrent treatment with bupropion, the first non-nicotine medication approved for treating tobacco dependence.17
Outcome measures
All patients were contacted at 6 and 12 months post intervention for follow-up appointments. Smoking habits were assessed 6 and 12 months post intervention, by measuring number of cigarettes smoked a day, the degree of nicotine dependency according to Fagerström's test, stage of change, as well as level of CO in expired air in all those taking part in the MI group and in those in the advice group who reported abstinence.
The final primary variable measured was success index, namely point prevalence of abstinence at 6 and 12 months post intervention. Abstinence was subjectively ascertained by means of direct personal testimony, and objectively confirmed by obtaining values of less than 6 ppm of CO in expired air (reference value acknowledged as a cut-off point between smokers and non-smokers). Failure of abstinence was defined as continuation of the smoking habit or non-attendance of follow-ups to confirm abstinence.
Statistical analysis
Statistical analysis was made in blind form, without knowing the identification labels of the groups that were compared. The results were analysed using SPSS. First of all, a description was made of the variables studied in both groups, comparing the distribution of the determining factors that may have affected the final result, and then a comparison was made of the proportion of successes by means of the χ2 test.
In order to evaluate the modifying variables of the effect and avoid confusion factors, recourse was made to multivariant analysis, constructing a logistic regression model by the step-by-step inclusion method, in which the dependent variable was the success or failure of the anti-smoking action, after both 6 and 12 months.
The trial was analysed by intention to treat, evaluating each subject in the study group to which they were randomly assigned. The extent of the therapeutic effect and the accuracy in its estimation was considered, calculating the reduction in relative risk, the reduction in absolute risk and the absolute increase in benefit, as well as the number of patients it would be necessary to treat in order to avoid a negative result.
The study was approved by the medical research ethics committee of the Albacete University Hospital Complex (Spain) on 3 April 2003.
RESULTS
Demographic and smoking characteristics
The baseline characteristics of the two groups are shown in Table 1. Patients' average age was 38 years (range = 16–75 years), with a slight predominance of women over men (52.5 versus 47.5%).
Table 1.
Baseline characteristics of the smokers in both actions.
| Action | Motivational Interviewing n = 114 | Advice n = 86 |
|---|---|---|
| Mean age in years (SD) | 38.58 (12.17) | 38.44 (12.37) |
| Women (%) | 51.8 | 53.5 |
| Mean age in years when started smoking (SD) | 16.31 (3.70) | 17.13 (5.11) |
| Smokers in active employment (%) | 86.0 | 75.6 |
| Mean number of years of consumption (SD) | 21.40 (12.29) | 19.94 (12.15) |
| Mean number of cigarettes smoked a day (SD) | 19.40 (10.26) | 17.47 (10.24) |
| Mean CO-oximetry (SD) | 15.40 (9.00) | 15.10 (10.03) |
| Mean Fagerström's test score (SD) | 4.16 (2.71) | 3.87 (2.59) |
| COPD (%) | 8.8 | 4.7 |
| Ischaemic heart disease (%) | 2.6 | 1.2 |
| Precontemplative stage (%) | 56.1 | 70.9 |
| Contemplative stage (%) | 36.8 | 27.9 |
| Decision stage (%) | 7.0 | 1.2 |
COPD = coronary obstructive pulmonary disease.
Only 7% of smokers had been diagnosed with COPD and 2% with ischaemic heart disease. The majority (80.8%) of subjects were in active employment, while 19.2% were unemployed or retired. The average age for starting smoking was 16 years. Average consumption was 18 cigarettes a day and the average smoking period was 20 years (range = 1–55 years). The average score in Fagerström's test was 4.04. The level of CO in expired air at the start of the study was 15.27 ppm.
Regarding the degree of motivation according to the classification of stages of change, 63.5% of smokers were in a precontemplative stage at the start of the study, 32.4% in a contemplative stage and 4.1% had taken the decision to give up smoking. In patients assigned to advice, 70.9, 27.9 and 1.2% were in the precontemplative, contemplative and determined stages, respectively, with P = 0.04. In the MI group, 56.1, 36.8 and 7% were in the above-mentioned stages, respectively.
Patients in this study with high physical dependency levels (that is; Fagerström's test scores of ≥7) were offered the possibility of using bupropion as an adjunct medical treatment. This medication was to be self-financed by the patient. Only 2.5% (five patients) began bupropion use; these five patients were assigned to the MI intervention.
Patient adherence to the MI intervention was as follows: 26 (22.8%) smokers attended the first interviewing only, 50 (43.9%) attended two interviews and 38 (33.3%) patients kept all three appointments.
Effectiveness
The measure of effectiveness of smoking cessation treatment at both 6 and 12 months post intervention showed that the action based on MI was 5.28 times more successful than anti-smoking advice (Table 2; odds ratio [OR] = 6.25, 95% CI = 1.8 to 21.7 at both 6 and 12 months). The fact that identical abstinence figures were obtained at 6 and 12 months in both patient groups was purely coincidental, given that some patients who did not respond at 6 months to confirm abstinence, did so at 12 months and vice versa.
Table 2.
Effectiveness of actions to give up smoking after 6 and 12 months.
| Advice n = 86 | Motivational Interviewing n = 114 | P | OR | 95% CI | NNT | |
|---|---|---|---|---|---|---|
| Abstinence after 6 months (%)a | 3 (3.5) | 21(18.4) | 0.00 | 6.25 | 1.8–21.71 | 7 |
| Abstinence after 12 months (%)a | 3 (3.5) | 21(18.4) | 0.001 | 6.25 | 1.8–21.71 | 7 |
The fact that identical abstinence figures were obtained at 6 and 12 months in both groups was purely coincidental.
NNT = number needed to treat.
OR = odds ratio.
The absolute increase in benefit was 14.9% (95% CI = 6.8 to 23%) and the number of smokers necessary to treat was 7 (95% CI = 5 to 15).
Regarding attendance of follow-up, 12 patients from the advice group and 27 patients from the MI group did not attend the first follow-up at 6 months post intervention. At 12 months, nine advice and 17 MI subjects did not attend appointments. In the logistic regression model, after both 6 and 12 months, the action appeared as a variable independently associated with smoking cessation. No confusion factors or effect-modifying variables were found. The probability of giving up the habit was 7.6 times greater in the MI group after 6 months (OR = 7.65, 95% CI = 2.18 to 26.84) and 6.9 times greater after 12 months (OR = 6.91, 95% CI = 1.98 to 24.15).
DISCUSSION
Summary of main findings
The primary objective of this study was to determine whether MI was a more effective anti-smoking intervention than brief advice. Our results show that MI is more effective than brief advice for smoking cessation in a primary care setting. Higher levels of abstinence in the MI group may be attributed, in part, to the patient-centred nature of the stage based intervention, where smokers actively involve themselves in making habit changes, without imposition or blame by the physician. Repeated advice, on the other hand, may be perceived as preaching, with subsequent risk of damaging the doctor–patient relationship and producing contrary behaviour.18
Comparison with existing literature
Until now, there has been limited evidence that MI and stage-of-change based interventions are effective for smoking cessation.19 The use of these methods has therefore not been justified in routine care by family physicians. Brief advice, however, about which more has been published, has been more extensively employed in clinical practice.6
A previous study conducted in a primary care setting by Butler et al12 comparing effectiveness of MI versus brief advice for smoking cessation in 536 smokers not selected for any other pathology, showed moderately higher success for the stage-based intervention. At 6 months post intervention, significant differences between groups in scores on self-reported abstinence in the previous 24 hours were found (OR = 2.86, 95% CI = 1.21 to 6.76). However, the odds of abandonment of the smoking habit at 6 months were considerably higher in our study for the MI group (OR = 7.65, 95% CI = 2.18 to 26.84) than in the Butler trial.12
Our relatively high abstinence levels for the MI intervention may be partly attributed to the fact that the GPs conducting the interviews in our study were the patients' regular family physicians. The GP registrars in the Butler et al study12 (resident doctors) trained in MI techniques were not the patients' habitual physicians; thus, although perhaps more enthusiastic, their experience and knowledge of the study subjects would have been more limited. Moreover, patients tend to respond more positively to doctors with whom they have maintained enduring doctor–patient relationships. Another difference between the current study and the Butler trial lies in the intensity of the MI intervention. Our patients were scheduled for three MI consultations, whereas in the Butler study, they were exposed to only one interview. Therefore, repeated stage of change based interventions may be more effective than a single consultation.
Other interventions reviewed by Lancaster and Stead20 of a similar nature to MI, such as individual behavioural counselling, have shown a certain efficacy, with a reported OR of abandonment of the smoking habit of 1.56 (95% CI = 1.32 to 1.84). Once again, however, the OR we report are considerably higher. These differences in results may be due to the nature of stage-based interventions, as previously described, and/or to the fact that in the behavioural counselling studies reviewed, sessions were administered by a trained therapist unknown to the patient.
Strengths and limitations of the study
This is a study of the development and evaluation of a motivational interviewing intervention for primary care use only. In our trial, patients were recruited during a regular visit to their GP for whatever reason and were not selected for any type of disease. No prior advertisements were issued regarding the trial and subjects had not received pre-selections cards. Therefore a more realistic assessment of the effectiveness of the intervention variable could be made under normal conditions experienced by GPs and their patients on a daily basis.
The design of our study presents several limitations. As part of our efforts to evaluate the efficacy of MI in the normal course of a GP's daily practice, adolescents as young as 15 years of age were included in the trial, given the reality that family physicians in Spain attend patients over the age of 14 years (minors of 14 years and younger are treated by paediatricians). The drawback to the admittance of young adolescent smokers in the study lies with the fact that they have not had sufficient time to develop established nicotine dependency, thus increasing their chances of successful quitting.
For ethical reasons, patients in our study with high nicotine dependency were offered bupropion as adjunct therapy (five patients from the MI group accepted). It is well-demonstrated that this therapy is effective for smoking cessation, increasing quitting odds by 1.5–2 times, independent of setting.17 Therefore, these patients should probably have been excluded from the trial, as they may potentially have skewed results in favour of the MI intervention.
Regarding patient characteristics at the outset of the study, the two groups were not homogeneous with respect to the variable ‘stage of change.’ A greater number of MI patients than advice patients were classified as belonging to a contemplative or decision stage (Table 1), thus favouring more successful outcomes in the MI group. However, it is also possible that since stage of change was determined following group assignation of subjects, GPs tended to overestimate the motivation of patients belonging to the MI group. Ideally, data collection from smokers and classification of stage of change should have been performed by an independent investigator before randomisation and group assignation of patients. However, our wish to be pragmatic and produce minimal alterations in the course of our consultations did not allow us to proceed in this way.
Lastly, patient randomisation was achieved by applying a non-block table of random numbers as opposed to a block table, resulting in unbalanced group sizes of 114 MI patients and 86 belonging to the advice group.
Implications for future research
The unusually high OR of abandonment of the smoking habit obtained in our study by the MI intervention, raises several questions for future research. Since the current study was conducted in a general practice setting with GPs familiar to patients, comparisons should be made with stage-based techniques carried out by therapists unconnected to subjects, in specific tobacco addiction treatment consultations.
The MI group in our study received three treatment sessions, whereas patients in the advice group were exposed to only one consultation with the GP, suggesting that intensity of the intervention, rather than efficacy of stage-based therapy and MI, may be responsible for higher abstinence levels. Further investigations are needed to compare effectiveness of more brief tailored MI interventions with brief advice and to evaluate whether single session MI interventions are as effective as repeated ones.
It may also be of interest to ascertain from which stage of change anti-smoking therapy is most likely to be successful. The cost-effectiveness of MI compared to other interventions should also be investigated, since application of the method requires training of physicians and extra consultation time.
Acknowledgments
We wish to thank all the patients who worked with us and were involved in the project. Special thanks go to Dr. López Torres for his impartial cooperation as scientific advisor.
Funding body
Research project financed by the Department of Health, Health Science Institute of the Government of the Autonomous Communities of Castille – La Mancha,(Spain) according to the decision taken at the meeting of 19 February 2003 (D. O. C. M. number 21)
Ethics committee
Project approved by the Medical Research Ethics Committee of the Albacete Health Service,(Spain) taking into consideration that the aforesaid project was in accordance with the essential ethical standards used in this field, as recorded in minutes no. 05/03 of the Medical Research Ethics Committee meeting in Albacete held on 3 April 2003
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Peto R, López AD, Boreham J, et al. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 2.Banegas Banegas JR, Diez Gañan L, Rodríguez-Artalejo F, et al. Mortalidad atribuible al tabaquismo en España en 1998. (Smoking-attributable deaths in Spain in 1998) Med Clin (Barc) 2001;117:692–694. doi: 10.1016/s0025-7753(01)72226-9. [DOI] [PubMed] [Google Scholar]
- 3.Ministerio de Sanidad y Consumo. Encuesta Nacional de Salud de España 1997. Madrid: Ministerio de Sanidad y Consumo; 1999. [Google Scholar]
- 4.Alonso JM, Magro R, Martínez JA, Sanz N. Comité Nacional para la Prevención del Tabaquismo. El Libro Blanco sobre el tabaquismo en España. [National Committee Smoking Prevention. White Paper about Smoking in Spain]. Barcelona: Glosa SL; 1998. Tabaco y atención primaria. [Google Scholar]
- 5.Lancaster T, Stead L, Silagy C, Sowden A. Effectiveness of actions to help people stop smoking: findings from the Cochrane Library. BMJ. 2000;321:355–358. doi: 10.1136/bmj.321.7257.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lancaster T, Stead LF. Physician advice for smoking cessation [review] Cochrane Database Syst Rev. 2004;(Issue 4):CD000165. doi: 10.1002/14651858.CD000165.pub3. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organisation. Evidence-based recommendations on the treatment of tobacco dependency. Copenhagen: WHO; 2001. [Google Scholar]
- 8.Centres for Disease Control and Prevention. Strategies for reducing exposure to environmental tobacco smoke, increasing tobacco-use cessation and reducing initiation in communities and health-care systems. A report on recommendations of the Task Force on Community Preventive Services. MMWR. 2000;49(RR-12):1–11. [PubMed] [Google Scholar]
- 9.Miller WR. Motivational interviewing with problem drinkers. Behavioural Psychotherapy. 1983;11:147–172. [Google Scholar]
- 10.Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behaviour. Barcelona: Ed Paidós; 1999. [Google Scholar]
- 11.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 12.Butler C, Rollnick S, Cohen D, et al. Motivational consulting versus brief advice for smokers in general practice: a randomised trial. Br J Gen Pract. 1999;49:611–616. [Google Scholar]
- 13.Fagerström KO, Schneider NG. Measuring nicotine dependence: a review of the Fagerström Tolerance Questionnaire. J Behav Med. 1989;12:159–182. doi: 10.1007/BF00846549. [DOI] [PubMed] [Google Scholar]
- 14.Jarvis M J, Russell MAH, Saloojee Y. Expired air carbon monoxide: a simple breath test of tobacco smoke intake. BMJ. 1980;281:484–485. doi: 10.1136/bmj.281.6238.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russell MAH, Merriman R, Stapleton J, Taylor W. Effect of nicotine chewing gum as an adjunct to general practitioner advice against smoking. BMJ. 1983;287:1782–1785. doi: 10.1136/bmj.287.6407.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiménez CA, Solano S, González de Vega JM, et al. Recomendaciones SEPAR. [SEPAR Recommendations]. Barcelona: Doyma; 1998. Tratamiento del tabaquismo; pp. 421–436. [Google Scholar]
- 17.Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2004;(Issue 4):CD000031. doi: 10.1002/14651858.CD000031. [DOI] [PubMed] [Google Scholar]
- 18.Butler CC, Pill R, Stott NC. Qualitative study of patients' perceptions of doctors' advice to give up smoking: implications for opportunistic health promotion. BMJ. 1998;316:1878–1881. doi: 10.1136/bmj.316.7148.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Riemsma RP, Pattenden J, Bridle C, et al. Systematic review of the effectiveness of stage based interventions to promote smoking cessation. BMJ. 2003;326:1175–1177. doi: 10.1136/bmj.326.7400.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005;(Issue 2):CD001292. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]


