Abstract
Background
A new primary care model for stroke aftercare has been developed to address the longer-term needs of patients who have had a stroke and their families.
Aim
To test the feasibility and acceptability of the new model on patients who have had a stroke and their carers.
Design of study
An observational feasibility study.
Setting
Patient and carer assessments and interviews conducted in patients' homes.
Method
Patients who have had a stroke and their carers were assessed using a purposely developed primary care stroke model. Qualified health- and social-care professionals acted as stroke care coordinators and carried out the assessments. Four evaluations were undertaken as part of the study: analysis of care plans, a survey of unmet needs, focus group sessions for staff, and patient/carer interviews.
Results
Forty-seven patients and 21 carers were recruited to the study. Analysis of care plans indicated that the assessment process was successful in identifying patient and carer problems (n = 219). Actions were instigated against 190 of these problems and, at 3 months after the assessment, 75% of the problems had been resolved. Patients/carers thought that the review process would be more valuable if conducted sooner after hospital discharge.
Conclusion
The model was acceptable to professionals, encouraging them to work in a manner more consistent with the expressed needs of patients and carers who were adjusting to the longer-term impact of stroke. Essential aspects informing the care process were also identified. Further work is now required to investigate the effects of the intervention on patient and carer outcomes.
Keywords: patient care management, primary healthcare, stroke
INTRODUCTION
Patients who have had a stroke and their carers experience a diversity of longer-term problems1 that are not well addressed by existing services.2 Although the National Service Framework for Older People3 recognises the need for a longer-term perspective, with a central role for the primary healthcare team, it offers little by way of service model guidance. The National Clinical Guidelines for Stroke4 provides a short inventory of recommendations for longer-term stroke management but these are insufficient in content and detail for the development of a service that is systematic and replicable. Successful management of other chronic diseases, such as diabetes and asthma, is already well developed in primary care in the UK; further preparatory work is required before similar approaches can be successfully applied in stroke.
Previous studies undertaken by this team have investigated and described the longer-term problems experienced by people who have had a stroke and their carers.5,6 By consolidating this evidence, and using it as a framework, we aimed to develop a primary care-based model for stroke aftercare.
The proposed process of care is presented in a manual comprising 16 problem-specific reference guides with assessment questions and associated patient and carer care plans (Table 1). The problem-specific reference guides contain educational text with supporting assessment algorithms and checklists. The assessment questions were identified following a review of tools listed in guidance documents for the single assessment process for older people.7 The Camberwell Assessment of Need for the Elderly (CANE) tool8 provided the best selection of questions for the problem areas within the primary care model with a selection of questions also being derived from the EASYcare tool.9 Additional material regarding local and national service information, together with a selection of validated assessment scales for specific areas such as depression and cognitive impairment, are included as appendices. The aim was to create a system of care that is comprehensive (encompasses all areas of potential concern to patient and carer) but individualised (patient-specific care plans).
Table 1.
Content and structure of primary care stroke model.
| Problem areas included in the model | ||
|---|---|---|
| • Transfer of care | • Shopping and meal preparation | |
| • Communication | • House and home | |
| • Medicines and general health | • Finances and benefits | |
| • Pain | • Personal hygiene | |
| • Mobility/falls | • Memory | |
| • Driving and general transport | • Mood changes | |
| • Incontinence | • Social needs | |
| • Sexual relations | • Carer emotional/social needs | |
| Care plans (patient and carer) | Reference guides | Additional material |
| Assessment questions provided for each problem area as basis for care plans. Questions derived mainly from The Camberwell Assessment of Need for the Elderly (CANE)8 and EASYcare9 needs assessment tools. | 2–3 page guides for each problem area. Each guide includes:
|
|
How this fits in
The longer-term needs of patients who have had a stroke and their carers are not being met by existing services. A new model for stroke aftercare has been developed based on the expressed needs of patients and carers. Feasibility testing with community-based health- and social-care professionals demonstrated the acceptability and practical application of this model. This novel approach to longer-term stroke care now requires outcome evaluation.
The aim of the current study was to test the feasibility of the primary care stroke model in practice. We wished to learn about:
the practical implications of its use;
its acceptability to patients and carers, and;
the extent to which it identified and addressed patients' and carers' stroke-related problems.
METHOD
Participants
Patients were identified from a hospital-based stroke register and approached for inclusion into the study. The initial contact was by letter, followed by a telephone call; consent was obtained during home visits by the research staff. The patients were between 4 months and 18 months post stroke onset. The study was widely advertised to community staff including social service offices, district nursing teams, community therapists, and general practices.
Permission to approach existing community-based staff was obtained from the relevant service managers. Eight nurses, two therapists and five social workers were recruited to become stroke coordinators as an extension of their usual work. In addition, one community nurse was funded to have sessional time dedicated to the role of stroke coordinator. All staff members recruited to the study agreed to conduct patient assessments using the new model of stroke care and coordinate any service responses identified, including liaising with the patient's primary healthcare team.
All staff except the funded post received a half-day induction programme to introduce them to the assessment system. This was followed by a series of training sessions provided in four key areas jointly identified by the community staff:
mood;
cognitive impairment;
benefits, and;
post-stroke sexual relations.
The funded nurse received the training material and was given professional support and informal education through an existing multidisciplinary stroke team comprising two stroke physicians, two physiotherapists, and two occupational therapists. The team met with the nurse approximately monthly to assist her in resolving identified problems.
Evaluations conducted
Analysis of care plans
Care plans, completed by staff during the assessments, recorded the types of patient and carer problems identified and the actions instigated. Each care plan was anonymised, and independently reviewed and summarised by two members of the research team using a data extraction form. As all patients were recruited some time after hospital discharge, the problem area of transfer of care was not included in the analysis. Agreement between reviewers was examined and discordance explored by group discussion to reach consensus.
Survey of unmet needs
Patients and carers were questioned about areas of unmet need using a purposely designed structured questionnaire based on the 15 problem areas incorporated in the stroke care model (transfer of care was excluded). The questionnaire comprised 40 questions for patients and six for carers. For each question, possible responses were ‘don't need help’ (that is, independent), ‘need help and support not sufficient’ (that is, unmet need), and ‘need help but receiving sufficient support’ (that is, met need). The questionnaire was administered by a researcher visiting the patient at home 3 months after first contact with the volunteer stroke care coordinators.
Views of the participating staff
Staff members were asked to complete a structured questionnaire after each patient had been assessed. These questionnaires comprised closed and open-ended questions designed to elicit views on the usefulness and ease of use of the manual and individual reference guides, time taken to complete an assessment and acceptability of this, and difficulties encountered. In addition, debriefing sessions were organised and facilitated by the research staff at various times during the study. Contemporaneous and observational notes that were taken during these sessions were later reviewed for completeness and accuracy by the facilitators. A summary of the main findings was prepared and circulated among the researchers to check for agreement.
Patient and carer interviews
Semi-structured interviews were undertaken with a purposeful sample of patients and carers. Patients were selected according to a range of personal variables relating to their stroke, age, and whether or not they had a carer. The researcher carrying out the interviews was aware of the findings of the assessment in each case and this information guided the format of the discussion. The interviews were tape-recorded and, following transcription, the data was coded into broadly negative and positive experiences related to the assessment process.
RESULTS
Forty-seven patients and 21 carers were recruited to the study. The average age of patients at the time of stroke was 72 years. Patients were, on average, 7–8 months post stroke at the time of assessment. Of the original 16 members of staff recruited to the study, 12 completed at least one assessment. Four were unable to carry out an assessment due to time constraints. Patients waited, on average, 37 days from recruitment to assessment; six patients waited more than 100 days.
Analysis of care plans
For each of the 47 patients assessed, a 16-item care plan had been completed. This included all problem areas except carer social/emotional needs. An ‘other’ section was included on the care plan. A total of 201 problems had been identified (an average of four stroke-related problems per patient) and an associated 175 actions recorded. The most commonly identified problems were in the areas of mobility/falls and personal hygiene (Figure 1). The largest discrepancies between problems identified and responses recorded occurred in the problem areas of pain (67% response) and cognition (33% response).
Figure 2.
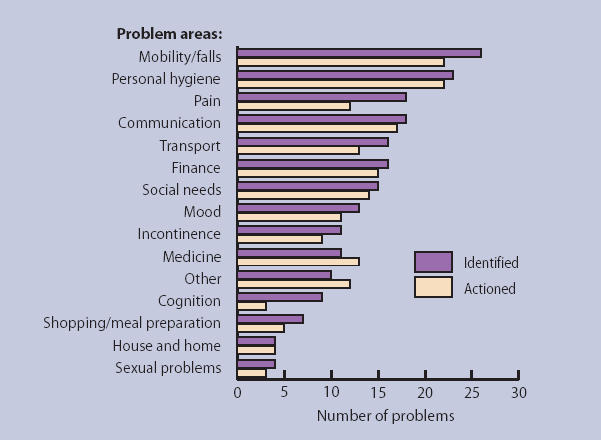
Number of patient problems identified and actioned.
Nineteen carers were assessed using an 11-item care plan. Two carers were not present at the time of assessment. In total, 18 carer-specific problems were identified and 15 actions recorded. Carers most commonly reported problems related to mood and social life, patient handling, and falls management (general health [n = 1]; transport [n = 1]; house and home [n = 1]; mobility and falls [n = 5]; personal hygiene [n = 3]; carer emotional/social needs [n = 7].
Survey of unmet needs
The 3-month follow-up survey found that of the 219 patient and carer problems identified at assessment, 54 (25%) problems still existed. The majority of these persisting problems (39/54) had actions recorded against them. Those that did not have a recorded action were twice as likely to persist 3 months after the assessment compared with problems that were acted upon (52 versus 21% of remaining problems). A further 97 new areas of unmet need were also identified but no action was taken regarding these.
Views of participating staff
The questionnaire was completed after 23 assessments. The average time to complete an assessment was 1 hour and 45 minutes (range = 1–4 hours). This was regarded as acceptable, although one staff member did remark that this was only because it was a ‘one-off’.
All responders who completed a questionnaire reported that the time taken to do follow-up work was acceptable. Two people reported that they found the manual difficult to use, mainly due to their unfamiliarity with the document. The reference guides were, in general, regarded as useful, however one person found them difficult to use. In seven assessments, staff members indicated that they were unsure about the adequacy of their skills.
The debriefing sessions provided a more informal forum, enabling staff to discuss their experiences and voice their opinions on the care model. The most prominent observation from the sessions was the attitudinal shift among staff that occurred during the period of study. Initial scepticism regarding the added value of the model over existing assessments was replaced with a general appreciation of the need for a systematic approach to the long-term management of patients who had had a stroke.
As anticipated, there was a general tendency for professional background to influence the approach to delivering the model. Not all staff members worked outside their usual skill base and in feedback sessions there was debate over the different approaches that could have been taken to specific problems. All staff members acknowledged specific gaps in their skill base and appreciated the training provided. The general perception among them was that patients and carers valued their assessments.
An additional development to the model was the construction of a patient and carer checklist. This was given to the patients and carers before, or at, their appointment. Staff members, patients, and carers all found this useful.
Patient and carer interviews
Seven patient/carer qualitative interviews were conducted. The patients were, on average, 7–8 months post-stroke at the time of assessment. The main view expressed was that the assessments had been of limited value and the interviews were used as an opportunity for the patients and carers to expound on ongoing problems. Patients had varying expectations about how the service might have helped them; three reported that they had expected more from the service in terms of providing reassurance and aiding coping, while a fourth patient envisaged little benefit.
Negative experiences
The general consensus among the limited number of patients and carers interviewed was that the assessment might have been more beneficial had it been conducted sooner after discharge from hospital. The need for more contact and continuity was an issue.
One assessment question, on sexual problems, had been embarrassing to two patients. In addition, there was evidence from three interviews that advice and information provided by the assessor for particular problems had not been utilised by the patient or carer, such that these problems had not been resolved. No reason was given for their rejection of the advice.
Positive experiences
Three patients stated that they had appreciated having someone to visit who showed interest in their problems. One found the contact helpful in a ‘supportive way’, while another described satisfaction associated with information provision, benefits advice, and support in liaising with the GP.
DISCUSSION
Summary of main findings
The main finding from our study is that a systematic and comprehensive assessment approach to post-acute stroke care proved feasible to implement and was successful in prompting the engagement of a range of community-based staff members who, in the main, were sufficiently confident to instigate actions against identified problems. The new care process under investigation encouraged professionals to work outside of their usual skill base in a manner more consistent with the expressed needs of patients and carers adjusting to the longer-term impact of stroke.5 In general, staff found the model acceptable and deliverable, although their commitment to the work was limited by existing workloads. Patients and carers, however, appeared to place less value on the assessments than the participating staff, indicating that they would have preferred an assessment earlier after discharge from hospital.
The follow-up survey at 3 months revealed that most of the identified problems that had a response recorded against them had been resolved. This is encouraging in terms of possible efficacy of the intervention and represents an improvement from the findings of a previous stroke aftercare study, based on a less structured approach involving routine hospital outreach nurse visits.10
A quarter of the initially identified problems remained at 3 months, however. The qualitative interviews revealed that some patients chose not to follow specific recommendations or advice. The reasons for this are not known.
Our feasibility study also revealed, at an early stage, that actions considered necessary after the assessment — particularly if they required input from other people, such as ordering equipment — might be overlooked or had long response times. This observation led us to instigate a monitoring process whereby all patients and carers were telephoned routinely by the stroke coordinator 3 months after the initial assessment to check progress. The monitoring process only related to the problems that had been identified initially; the survey of unmet need at 3 months revealed a large number of apparently new stroke-related problems. This is consistent with the previous literature10 and strongly implies that there is a need for ongoing contact with patients and carers after stroke, rather than the single point of contact adopted in this feasibility study.
Strengths and limitations of the study
One explanation for the less favourable comments from the patients and carers might relate to the timing of the intervention. The assessments were conducted an average 7–8 months post-stroke onset and patients and carers suggested that an earlier assessment would have been more valuable. The timing of the assessments was dictated by the short timescale of the study and the need to identify patients of relevance to the participating community staff, who worked in geographically defined locations. For these reasons, patients had to be identified retrospectively from an existing stroke register.
A further weakness was that, apart from the specifically funded sessional time of one community nurse, the participating community staff, by necessity, needed to include the work of the stroke assessments within their usual workload. This also contributed to delays in timely patient assessment.
The main strength of the study was the overlapping methods that allowed the implications of the new service model to be investigated from several perspectives, including that of the patients and carers.
Comparison with existing literature
The traditional approach to stroke has adopted a predominantly physical rehabilitation model.11 Physical losses are, however, only part of the longer-term issues facing patients who have had a stroke;1 psychosocial and adjustment issues become more intrusive with time.10 This may be an important reason why continuing physical therapy in the post-discharge period, although undoubtedly of value,12 has limited effectiveness and does not appear to positively impact on patient and carer well-being.
The existing approaches to longer-term stroke care that have incorporated a psychosocial component have proved disappointing.13 One common weakness in these previous studies is their lack of focus on the expressed needs of patients who have had a stroke and their carers. We know of one American study that evaluated a post-discharge stroke management model similar to our own.14 This was a small randomised controlled trial (n = 96) of carefully selected patients who had had a stroke; improved outcomes were reported at a 3-months follow up.
Implication for future research and clinical practice
There are persuasive arguments for embedding longer-term management of stroke in primary care:
to enhance continuity of care;
to improve access to community services;
to offer a coordinated approach, and;
to undertake regular reviews.
A recent national report, highly critical of current stroke care in the UK, has also emphasised these issues.15 Exactly how this might be achieved, however, is uncertain but a defined care structure and specified staff skills are likely to be the essential first steps to an effective service.
The comprehensive stroke assessment process we have developed appears to be a practical way forward. The participating staff in our study expressed a need for training in four specific areas: benefits, sexual problems, mood/depression, and cognition. Although these are likely to be particular to these staff, they give an indication of the diversity of the training requirements in the special context of post-acute stroke care. This conclusion is supported by an earlier survey of community nurses who reported a considerable perceived knowledge gap in relation to stroke.16 Having demonstrated the feasibility and acceptability of this novel system of stroke care, the intervention now requires a robust evaluation before it can be recommended for routine clinical use.
Acknowledgments
We wish to thank our acting Stroke Care Coordinators and members of the multidisciplinary team for their commitment to the study. We also thank Nick Hodgkinson (Welfare Rights & Debt Advice Development Worker), and Gill Croft and Michelle Shively-Harris (Bradford Relate Therapists) for providing educational sessions to our coordinators. We pass on our gratitude to the long list of people who provided us with information aiding the development of the model.
Funding body
The Stroke Association TSA 01/00
Ethics committee
Bradford Local Ethics Committee 20/09/230
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Young J, Murray J, Forster A. Review of longer-term problems after disabling stroke. Reviews in Clinical Gerontology. 2003;13:55–65. [Google Scholar]
- 2.Young JB. The primary care stroke gap. Br J Gen Pract. 2001;51:787–788. [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health. National service framework for older people. London: Department of Health; 2001. [Google Scholar]
- 4.Intercollegiate Working Party for Stroke. National clinical guidelines for stroke. London: Royal College of Physicians; 2002. [Google Scholar]
- 5.Murray J, Ashworth R, Forster A, Young J. Developing a primary care-based stroke service: a review of the qualitative literature. Br J Gen Pract. 2003;53:137–142. [PMC free article] [PubMed] [Google Scholar]
- 6.Murray J, Young J, Forster A, Ashworth R. Developing a primary care-based stroke model: the prevalence of longer-term problems experienced by patients and carers. Br J Gen Pract. 2003;53:803–807. [PMC free article] [PubMed] [Google Scholar]
- 7.Department of Health. Guidance on the single assessment process for older people. HSC2002/001; LAC (2002)1. London: Department of Health; 2002. [Google Scholar]
- 8.Orrell M, Hancock G. The Camberwell Assessment of Need for the Elderly. London: Gaskell; 2004. [Google Scholar]
- 9.Philp I. EASY-Care: A systematic approach to the assessment of older people. Geriatric Medicine. 2000;30(5):15–19. [Google Scholar]
- 10.Dowswell G, Lawler J, Young J. Unpacking the ‘black-box’ of nurse-led stroke support service. Clin Rehabil. 2000;14(2):160–171. doi: 10.1191/026921500672130349. [DOI] [PubMed] [Google Scholar]
- 11.Forster A, Young J. Stroke rehabilitation: can we do better? BMJ. 1992;305:1446–1447. doi: 10.1136/bmj.305.6867.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Outpatient Service Trialists. Rehabilitation therapy services for stroke patients living at home: systematic review of randomised trials. Lancet. 2004;363:352–356. doi: 10.1016/S0140-6736(04)15434-2. [DOI] [PubMed] [Google Scholar]
- 13.Knapp P, House A, Forster A, Young J. Review of non-drug strategies to address psycho-social difficulties after stroke. Age and Ageing. 2000;29:23–30. doi: 10.1093/ageing/29.1.23. [DOI] [PubMed] [Google Scholar]
- 14.Allen KR, Hazelett S, Jarjoura D, et al. Effectiveness of a post-discharge care management model for stroke and transient ischemic attack: a randomised trial. J Stroke Cerebrovasc Dis. 2002;11(2):88–98. doi: 10.1053/jscd.2002.127106. [DOI] [PubMed] [Google Scholar]
- 15.National Audit Office. Reducing brain injury: faster access to better stroke care. HC 452. London: Department of Health; 2005. [Google Scholar]
- 16.Murray J, Young J, Forster A, Ashworth R. A survey to investigate the role of the district nurse in stroke care. Br J Community Nurs. 2004;9(8):318–324. doi: 10.12968/bjcn.2004.9.8.15352. [DOI] [PubMed] [Google Scholar]


