Abstract
Background/aim: The “compact reduced logMAR” (cRLM) chart is being developed as a logMAR alternative to the Snellen chart. It is closer spaced and has fewer letters per line than conventional logMAR charts. Information regarding the performance of such a chart in amblyopes and children is therefore required. This study aimed to investigate the performance of the cRLM chart in amblyopic children.
Methods: Timed test and retest measurements using two versions of each chart design were obtained on the amblyopic eye of 43 children. Using the methods of Bland and Altman the agreement, test-retest variability (95% confidence limits for agreement, TRV) and test time of the cRLM and the current clinical standard Snellen chart were compared to the gold standard ETDRS logMAR chart.
Results: No systematic bias between chart designs was found. For line assignment scoring the respective TRVs were 0.20 logMAR, 0.20 logMAR, and 0.30 logMAR. Single letter scoring TRVs were cRLM (95% CL 0.17) logMAR, ETDRS (95% CL 0.14) logMAR, and Snellen (95% CL 0.29) logMAR. Median testing times were ETDRS 60 seconds, cRLM 40 seconds, Snellen 30 seconds.
Conclusion: The sensitivity to change of the cRLM equalled or approached that of the gold standard ETDRS and was at least 50% better than that of Snellen. This enhanced sensitivity to change was at the cost of only a 10 second time penalty compared to Snellen. The cRLM chart was approximately half the width of the ETDRS chart. The cRLM chart may represent a clinically acceptable compromise between the desire to obtain logMAR acuities of reasonable and known sensitivity to change, chart size, and testing time.
Keywords: visual acuity, vision test, amblyopia
The design flaws inherent in Snellen visual acuity and the advantages of logMAR format charts are well recognised.1–6 We aim to develop a chart for widespread ophthalmic use which will offer a clinically acceptable compromise between the sensitivity to change of current logMAR charts and the size and speed of use of Snellen optotypes. The “compact reduced logMAR” (cRLM) chart, which is described here is a development of the RLM chart that we have previously described.5 The cRLM chart is closer spaced than both the RLM and other logMAR charts and does not have the crowding bars which were present on the RLM chart. These changes might affect its performance in amblyopes. This study aimed to compare the performance of the cRLM chart in amblyopic children with that of the gold standard ETDRS and the current clinical standard Snellen charts.
PATIENTS AND METHODS
Forty three children (19 male) aged 5–9 years (mean 6.7 years) who were receiving orthoptic treatment for amblyopia participated in this study; 17 children had anisometropic amblyopia, in the remaining 26 the amblyopia was strabismic. The visual acuity of their amblyopic eyes ranged from −0.11 to 0.82 logMAR (mean 0.38 logMAR (95% CL 0.24) logMAR, Snellen equivalents 6/5 to 6/39). Ethical approval and informed consent were obtained.
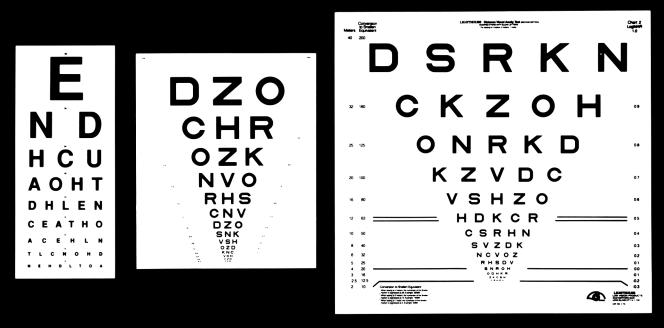
The cRLM, ETDRS and Snellen charts are illustrated in Figure 1. The ETDRS and Snellen charts, testing protocol, scoring and methods of analysis employed have been described in detail in a previous paper5 and will only be summarised here. A testing distance of 6 metres was used for all tests and logMAR scores adjusted accordingly. Timing was to the nearest 10 seconds. The ETDRS chart has a visible area of 64×59 cm., the cRLM 36×45 cm, and the Snellen chart 20×48 cm. In common with ETDRS charts the cRLM chart has 14 lines and a 0.1 logMAR line size progression. It differs in having three rather than five letters per line and letter and line spacing of half rather than a whole letter width/height. The single letter scoring value of each cRLM letter is therefore 0.033 logMAR as opposed to 0.02 logMAR on an ETDRS chart. Each of these design parameters is very variable on a Snellen chart. From 4 metres both ETDRS and cRLM charts measure a Snellen equivalent acuity range of 6/60 (20/200) to 6/3 (20/10). Timed test and retest measurements of acuity were obtained in random order using two versions of each chart design on the amblyopic eye of every subject by one examiner. The tests were performed at one sitting with breaks as required. A single letter scoring algorithm, which gives credit for each letter on the chart that is correctly identified, was employed. In this the subject is required to read each letter on the chart until an entire line of letters has been incorrectly identified. This method has been shown to be associated with less test-retest variability (TRV) than the “line assignment” method commonly used with the Snellen chart.7–9 A “line assignment” scoring algorithm (which identifies the lowest line upon which half or more of the letters have been correctly read) was retrospectively applied to the test results.
Figure 1.
The Snellen, cRLM, and ETDRS charts (to scale).
The objectives were to determine for each chart:
The level of agreement with the gold standard ETDRS
The TRV of single letter and line scoring acuity measurements. TRV was defined as 95% confidence limits of agreement.
The time taken to perform a “single letter scoring” acuity measurement.
The methods of Bland and Altman were employed.10
RESULTS
Examination of the distribution of data sets suggested that the parametric methods of Bland and Altman might reasonably be applied.10 Performance data for each chart are presented in Table 1. The median and range of testing times for the single letter scoring algorithm were: ETDRS 60 (30–300) seconds, cRLM 40 (20–140) seconds, Snellen 30 (20–100) seconds.
Table 1.
Performance data for each chart
| Single letter scoring | ||||
| Mean difference (95% CI) logMAR | Min/max difference logMAR | TRV (95% CLA) logMAR | Line scoring TRV (95% CLA) logMAR | |
| ETDRS-ETDRS | 0.00 (0.02) | −0.16, 0.17 | ±0.14 (7 ETDRS letters) | ±0.20 (2 ETDRS lines) |
| cRLM-cRLM | 0.00 (0.02) | −0.22, 0.23 | ±0.17 (5 cRLM letters) | ±0.20 (2 cRLM lines) |
| Snellen-Snellen | 0.03 (−0.01, 0.06) | −0.36, 0.16 | ±0.29 (variable number of Snellen letters) | ±0.30 (variable number of Snellen lines) |
| ETDRS-cRLM | 0.01 (−0.01, 0.03) | −0.13, 0.20 | - | - |
| ETDRS-Snellen | 0.02 (−0.02, 0.06) | −0.26, 0.27 | - | - |
DISCUSSION
Visual acuity is used as a measure of both disease severity and change. logMAR format tests offer the advantage of consistent test-retest variability across the acuity range. This means that one can identify in terms of numbers of letters or lines, a minimum change which might be considered significant and which might be applied regardless of the underlying acuity. Scaling and other factors mean that this is not possible with Snellen acuity measurements. The use of Snellen charts therefore compromises clinical sensitivity to change. The Snellen fraction is also very difficult to analyse which unnecessarily compromises both research and audit. A logMAR score can be regarded as interval data and analysed using parametric tests.
While standard in prospective research,6,11 logMAR charts have not widely replaced Snellen charts in clinical practice. Reasons for this may include the large size and number of letters on each chart, the unfamiliar scoring system, and the perception that logMAR tests are time consuming. We therefore aim to develop a chart for general ophthalmic use which will offer a clinically acceptable compromise between the desire to measure logMAR acuities and the size, ease of use, and testing time of the Snellen chart. The cRLM chart that is described here is an iterative development of the RLM chart which we have previously described.5 It is closer spaced and has fewer letters per line than conventional logMAR charts. It also differs from the preceding RLM chart in having no crowding bars. Both these design changes and the desire for general acceptability mean that information regarding the performance of the chart in amblyopes and children is required. This study therefore aimed to compare the performance of the cRLM chart in amblyopic children with that of the gold standard ETDRS and the current clinical standard Snellen charts.
The size and results of this study in terms of agreement and TRV scores are in keeping with previously published data and with the results of testing of the preceding RLM chart design.2,5,8,9,12–14
It is a principle of method comparison studies that a lack of bias between the index and gold standard tests implies that the index test(s) is/are measuring the same thing in a similar way.15 No systematic bias was found between measurements made with the cRLM or Snellen chart when compared to the gold standard ETDRS chart (Table 1: the 95% confidence interval for the mean difference include 0 in each case). Contour interaction (crowding) is a complex and poorly understood but potentially important aspect of chart design, particularly in amblyopes.16–19 In brief the presence of adjacent contours is known to influence the legibility of letters and this effect is greatest in amblyopes. The effect of number, positioning, and horizontal or vertical spacing of such “crowding” contours (which are usually letters but sometimes bars) is far from clear. Each letter on the cRLM has between two and four adjacent letters. The lack of bias between the cRLM and ETDRS charts in this paediatric amblyopic population suggests that the letter stimuli on the two charts are subject to comparable degrees of contour interaction. If the letters on the cRLM chart were less crowded than the ETDRS chart then systematically better acuity measurements would have been expected. This conclusion might also reasonably be applied to the Snellen chart.
Using the clinically usual line assignment scoring method the cRLM chart was as reliable as the gold standard ETDRS chart (TRVs±0.20 logMAR (or two lines) in either direction). The corresponding value for the Snellen chart was ±0.30 logMAR. A change of three lines in either direction on the cRLM and ETDRS is therefore required before the result exceeds the upper limit of normal test-retest variability for the tested population and can be considered significant. One in 20 subjects would also be expected to show greater TRV. Scaling factors mean that the minimum clinically significant change on a Snellen chart, while 50% greater, cannot be defined in terms of a consistent number of letters or lines, thereby further compromising its sensitivity as a clinical tool. These data underline the “noisiness” of clinical acuity tests and provide a basis for the need for the test methodology to be optimised. A prerequisite for a Bland and Altman10 analysis is an examination of the test-retest variability data to ensure that the TRV is not dependent on the magnitude of the quantity being measured. The results of this analysis suggest that the up to two lines in either direction test-retest variability of acuity measurements might be consistently applied across the observed range.
The desire to increase the precision of acuity scores beyond single line values is reflected in notations such as 6/9-3. The single letter scoring algorithm addresses this and is associated with both the greatest precision and the lowest TRV of all current clinical chart scoring methods.7,8 The single letter scoring TRV of the cRLM chart was only slightly greater than that of the ETDRS chart (95% confidence limit for agreement ±0.17 and ±0.14 logMAR respectively). The Snellen chart demonstrated nearly twice this level of test-retest variability (±0.29 logMAR). An acuity change in either direction of eight ETDRS letters (0.16 logMAR) or six cRLM letters (0.20 logMAR) might therefore be considered significant with 95% confidence. Changes of less than this might arise because of either measurement error or change. Because of the irregular scaling on Snellen charts the minimum clinically significant change varies from line to line and cannot be consistently expressed in terms of a number of letters of change. The sensitivity to change advantage of employing a single letter as opposed to a line by line scoring algorithm is illustrated by these data.
When the method of single letter scoring was employed the median cRLM measurement time of 40 seconds was 10 seconds slower than that of Snellen charts and 20 seconds faster to use than ETDRS. Line by line scoring would be expected to be quicker using each chart design. The difficulty and time involved in calculating single letter scores for any chart design is being addressed with the development of an automated scoring device. The advantages of a single letter score in terms of sensitivity to change mean that the clinical adoption of this technique is worthwhile.
At its standard test distance of 4 metres the cRLM chart does not fit into a Snellen light box, the required width is however only just over half that of the ETDRS light box which means that a rotating box design is potentially feasible.
REFERENCES
- 1.Bailey I, Lovie J. New design principles for visual acuity letter charts. Am J Optom Physiol Opt 1976;53:740–5. [DOI] [PubMed] [Google Scholar]
- 2.Elliott DB, Sheridan M. The use of accurate visual acuity measurements in clinical anti-cataract formulation trials. Ophthalmic Physiol Opt 1988;8:397–401. [DOI] [PubMed] [Google Scholar]
- 3.Ferris FL, Kassoff A, Bresnick GH, et al. New visual acuity charts for clinical research. Am J Ophthalmol 1982;94:91–6. [PubMed] [Google Scholar]
- 4.Sloan LL. New test charts for the measurement of visual acuity at near and far distances. Am J Ophthalmol 1959;48:807–13. [DOI] [PubMed] [Google Scholar]
- 5.Rosser DA, Laidlaw DA, Murdoch IE. The development of a “reduced logMAR” visual acuity chart for use in routine clinical practice. Br J Ophthalmol 2001;85:432–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Acadamy of Sciences-National Research Council Committee on Vision. Report of working group 39: recommended standard procedures for the clinical measurement and specification of visual acuity. Adv Ophthalmol 1980;41:103. [PubMed] [Google Scholar]
- 7.Vanden Bosch ME, Wall M. Visual acuity scored by the letter-by-letter or probit methods has lower retest variability than the line assignment method. Eye 1997;11:411–17. [DOI] [PubMed] [Google Scholar]
- 8.Bailey IL, Bullimore MA, Raasch TW, et al. Clinical grading and the effects of scaling. Invest Ophthalmol Vis Sci 1991;32:422–32. [PubMed] [Google Scholar]
- 9.Arditi A, Cagenello R. On the statistical reliability of letter-chart visual acuity measurements. Invest Ophthalmol Vis Sci 1993;34:120–9. [PubMed] [Google Scholar]
- 10.Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;i:307–10. [PubMed] [Google Scholar]
- 11.Ferris FL, Bailey I. Standardizing the measurement of visual acuity for clinical research studies: Guidelines from the Eye Care Technology Forum. Ophthalmology 1996;103:181–2. [DOI] [PubMed] [Google Scholar]
- 12.Lovie Kitchin JE. Validity and reliability of visual acuity measurements. Ophthalmic Physiol Opt 1988;8:363–70. [DOI] [PubMed] [Google Scholar]
- 13.Reeves B, Wood J, Hill A. Vistech VCTS 6500 charts, within- and between-session reliability. Optom Vis Sci 1991;68:728–37. [DOI] [PubMed] [Google Scholar]
- 14.Siderov J, Tiu AL. Variability of measurements of visual acuity in a large eye clinic. Acta Ophthalmol Scand 1999;77:673–6. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135–60. [DOI] [PubMed] [Google Scholar]
- 16.Fern KD, Manny RE, Davis JR, et al. Contour interaction in the preschool child. Am J Optom Physiol Opt 1986;63:313–8. [DOI] [PubMed] [Google Scholar]
- 17.Simmers AJ, Gray LS, McGraw PV, et al. Contour interaction for high and low contrast optotypes in normal and amblyopic observers. Ophthalmic Physiol Opt 1999;19:253–60. [PubMed] [Google Scholar]
- 18.Stager DR, Everett ME, Birch EE. Comparison of linear and optotype acuity in amblyopia. Am Orthopt J 1990;40:51–6. [Google Scholar]
- 19.McGraw PV, Winn B, Gray LS, et al. Improving the reliability of visual acuity measures in young children. Ophthalmic Physiol Opt 2000;20:173–84. [PubMed] [Google Scholar]