Since the clinical entity of acute zonal occult outer retinopathy (AZOOR) was initially proposed,1 it has been noted that the visual loss may be misattributed to lesions in the optic nerve or central nervous system. Even with a likely visual field defect for those diseases—an afferent pupillary defect and reduced subjective central flicker fusion threshold—clinicians should be always aware of the possibility of AZOOR.
Case report
A 32 year old woman noticed a large scotoma in her right eye. She was examined by an ophthalmologist who found her corrected visual acuity to be 0.4 in the right eye and 1.0 in the left eye. She also had an afferent pupillary defect in the right eye. Goldmann perimetry showed a superior altitudinal hemianopic defect in the right eye (fig 1). Subjective central flicker fusion threshold was reduced in the right eye (18 Hz) and normal in the left eye (35 Hz). Ophthalmoscopic examination, fluorescein angiography, blood screening, and computed tomography were normal. Suspecting ischaemic optic neuropathy (ION), a 5 day course of intravenous succinic hydrocortisone, 100 mg/day, was used but this treatment was not effective. The patient was then referred to us for further examination. Full field rod and cone electroretinograms (ERGs) were reduced in her right eye (about 50% of those in the left eye). Multifocal ERGs (mfERGs) recorded with the VERIS Science 4.0 system (Electro-Diagnostic Imaging, San Mateo, CA, USA) revealed reduced responses in areas corresponding to the visual field defect (fig 2). These findings led us to presume the diagnosis to be AZOOR.1 While we have followed her for approximately a year, no retinal finding has been observed and the visual defect has not changed.
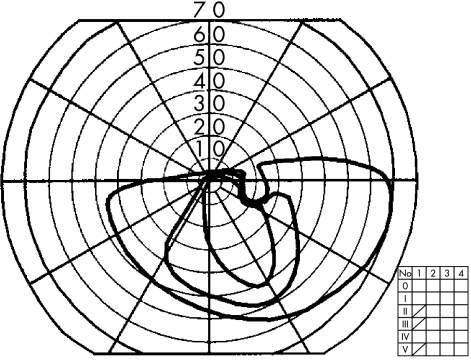
Figure 1.
Goldmann visual field of the right eye showing superior altitudinal hemianopic depression including the blind spot. The field for the left eye was normal (not shown).
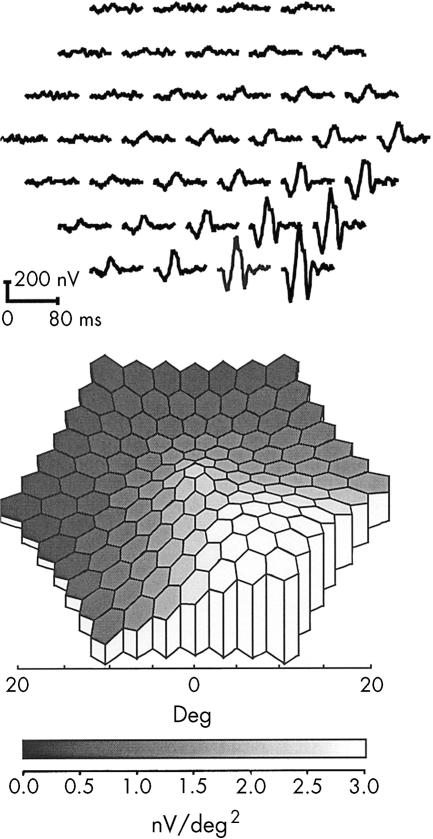
Figure 2.
(Upper panel) Trace array of multifocal ERGs (mfERGs) of the right eye showing marked depression in the superior retinal areas. Waveforms that are close to “extinguished” within the lesion are one of the characteristics of mfERGs in AZOOR. Recorded with: length of m-sequence, 214–1; base rate, 75 Hz; flash intensity, 2.67 cd/s/m2; band pass filter, 10–300 Hz; and artefact removal procedure, one iteration (0–80 ms on the first order kernel). (Lower panel) The 3D topographic plot translated from the trace array shown above showing functional distribution of the retina corresponding to the visual field defect.
Comment
Although altitudinal hemianopsia is found in many optic nerve disorders—for example, as meningioma, optic neuritis, ION, sinuses or intracranial artery disorders, and congenital abnormalities of the optic nerve head,2 this type of field defect had been rarely reported in AZOOR.3 The visual field abnormality in AZOOR varies from case to case,1 but central or paracentral scotoma is most common. When the clinical entity of AZOOR was initially proposed,1 the visual loss was attributed to retrobulbar neuritis, a pituitary adenoma, or other intracranial lesions during the early stages of this disease. Normal fundus and fluorescein angiographic findings with dense scotoma led ophthalmologists to suspect optic nerve or intracranial diseases. In addition, the afferent pupillary defect and disc swelling in AZOOR1 were very misleading. Our patient had a superior altitudinal hemianopic defect, an afferent pupillary defect, the reduced subjective central flicker fusion threshold and no disc swelling, and thus, had to be differentiated from ION or posterior ION (PION) without optic disc involvement. PION is an unusual subset of ION and frequently related to arteritis. ERG observations may be critical for the differential diagnosis of cases with visual field defect without observable retinal lesions that are usually attributed to optic nerve or intracranial diseases. While the full field ERG may be sufficient to make the diagnosis,4 in many of the cases, focal ERG1,5 or mfERG6–8 can show the correspondence of the retinal dysfunction to the visual field defect which strongly reinforce the diagnosis of AZOOR.
Grant support: Grant No 13877293 from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
References
- 1.Gass JD. Acute zonal occult outer retinopathy. J Clin Neuro Ophthalmol 1993;13:79–97. [PubMed] [Google Scholar]
- 2.Herse PR. Altitudal hemianopsia: a case report and mini-review. Optom Vis Sci 1991;68:314–17. [DOI] [PubMed] [Google Scholar]
- 3.Saito K, Ishibashi K, Nakamura M, et al. AZOOR with ischemic optic neuropathy-like visual field. Jpn Rev Clin Ophthalmol 1999;93:319–22. [Google Scholar]
- 4.Jacobson SG, Morales DS, Sun XK, et al. Pattern of retinal dysfunction in acute zonal occult outer retinopathy. Ophthalmology 1995;102:1187–98. [DOI] [PubMed] [Google Scholar]
- 5.Horiguchi M, Miyake Y, Nakamura M, et al. Focal electroretinogram and visual field defect in multiple evanescent white dot syndrome. Br J Ophthalmol 1993;77:452–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arai M, Nao-i N, Sawada A, et al. Multifocal electroretinogram indicates visual field loss in acute zonal occult outer retinopathy. Am J Ophthalmol 1998;126:466–9. [DOI] [PubMed] [Google Scholar]
- 7.Yasuda K, Shimura M, Noro M, et al. Clinical course of acute retinal zonal occult outer retinopathy in visual field and multifocal electroretinogram. Br J Ophthalmol 1999;83:1089–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Yousuf N, Parks S, Dhillon B, et al. Acute zonal occult outer retinopathy. Br J Ophthalmol 2000;84:118–19. [DOI] [PMC free article] [PubMed] [Google Scholar]