Abstract
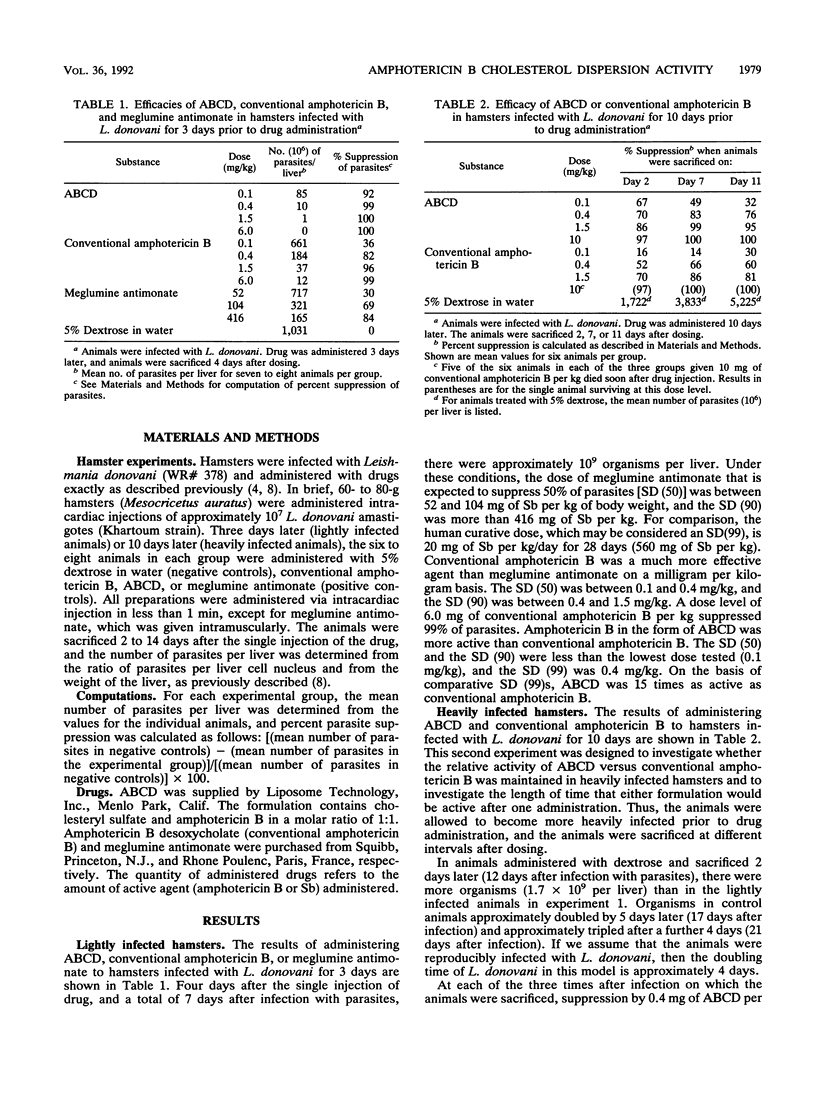
Standard therapy of human visceral leishmaniasis with parenteral pentavalent antimonial agents is generally curative but has the disadvantages of a 28-day treatment course, occasional treatment failures, and toxicity. The antifungal and antileishmanial agent amphotericin B has been complexed with lipids to develop a less toxic formulation of amphotericin B. Because lipid particles are phagocytized by the reticuloendothelial system, lipid-associated amphotericin B should be concentrated in infected macrophages and be very effective against visceral leishmaniasis. One formulation, amphotericin B cholesterol dispersion (ABCD) (Amphocil), was tested for antileishmanial activity in Leishmania donovani-infected hamsters. In the first experiment, hamsters were infected, administered with the drug 3 days later, and then sacrificed after a further 4 days. ABCD (dose needed to suppress 99% of hepatic parasites compared with controls [SD (99)], 0.4 mg/kg of body weight) was 15 times as effective as conventional amphotericin B [SD (99), 6.0 mg/kg]. Pentavalent antimony in the form of meglumine antimonate had an SD (84) of 416 mg/kg. In a second experiment in which animals were allowed to become more heavily infected, the drug was administered 10 days after infection and the animals were sacrificed after a further 2, 7, or 11 days. ABCD was approximately four times as active as conventional amphotericin B. These experiments suggest that ABCD is at least four times as active as conventional amphotericin B against visceral leishmaniasis and that clinical trials are warranted.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berman J. D., Goad L. J., Beach D. H., Holz G. G., Jr Effects of ketoconazole on sterol biosynthesis by Leishmania mexicana mexicana amastigotes in murine macrophage tumor cells. Mol Biochem Parasitol. 1986 Jul;20(1):85–92. doi: 10.1016/0166-6851(86)90145-3. [DOI] [PubMed] [Google Scholar]
- Berman J. D., Grogl M. Leishmania mexicana: chemistry and biochemistry of sodium stibogluconate (Pentostam). Exp Parasitol. 1988 Oct;67(1):96–103. doi: 10.1016/0014-4894(88)90012-4. [DOI] [PubMed] [Google Scholar]
- Berman J. D., Hanson W. L., Chapman W. L., Alving C. R., Lopez-Berestein G. Antileishmanial activity of liposome-encapsulated amphotericin B in hamsters and monkeys. Antimicrob Agents Chemother. 1986 Dec;30(6):847–851. doi: 10.1128/aac.30.6.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft S. L., Davidson R. N., Thornton E. A. Liposomal amphotericin B in the treatment of visceral leishmaniasis. J Antimicrob Chemother. 1991 Oct;28 (Suppl B):111–118. doi: 10.1093/jac/28.suppl_b.111. [DOI] [PubMed] [Google Scholar]
- Davidson R. N., Croft S. L., Scott A., Maini M., Moody A. H., Bryceson A. D. Liposomal amphotericin B in drug-resistant visceral leishmaniasis. Lancet. 1991 May 4;337(8749):1061–1062. doi: 10.1016/0140-6736(91)91708-3. [DOI] [PubMed] [Google Scholar]
- Fielding R. M., Singer A. W., Wang L. H., Babbar S., Guo L. S. Relationship of pharmacokinetics and drug distribution in tissue to increased safety of amphotericin B colloidal dispersion in dogs. Antimicrob Agents Chemother. 1992 Feb;36(2):299–307. doi: 10.1128/aac.36.2.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson W. L., Chapman W. L., Jr, Kinnamon K. E. Testing of drugs for antileishmanial activity in golden hamsters infected with Leishmania donovani. Int J Parasitol. 1977 Dec;7(6):443–447. doi: 10.1016/0020-7519(77)90004-2. [DOI] [PubMed] [Google Scholar]
- Hart D. T., Lauwers W. J., Willemsens G., Vanden Bossche H., Opperdoes F. R. Perturbation of sterol biosynthesis by itraconazole and ketoconazole in Leishmania mexicana mexicana infected macrophages. Mol Biochem Parasitol. 1989 Mar 1;33(2):123–134. doi: 10.1016/0166-6851(89)90026-1. [DOI] [PubMed] [Google Scholar]
- Herwaldt B. L., Berman J. D. Recommendations for treating leishmaniasis with sodium stibogluconate (Pentostam) and review of pertinent clinical studies. Am J Trop Med Hyg. 1992 Mar;46(3):296–306. doi: 10.4269/ajtmh.1992.46.296. [DOI] [PubMed] [Google Scholar]


