Abstract
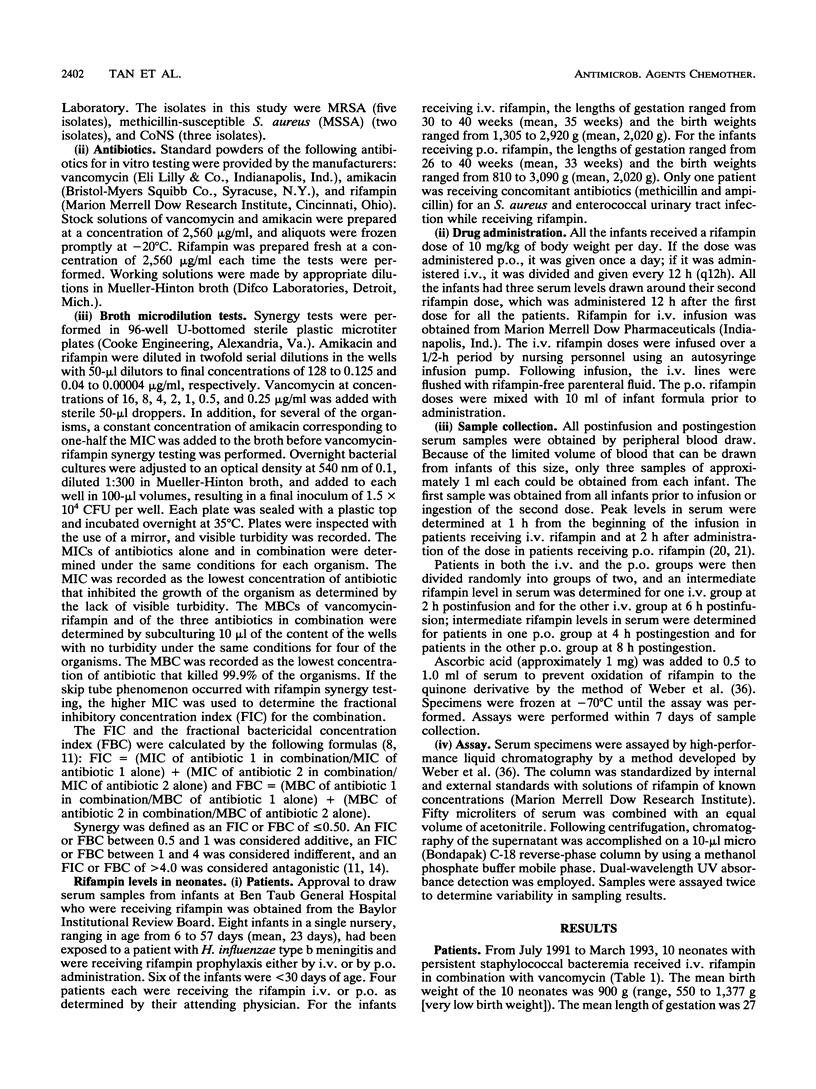
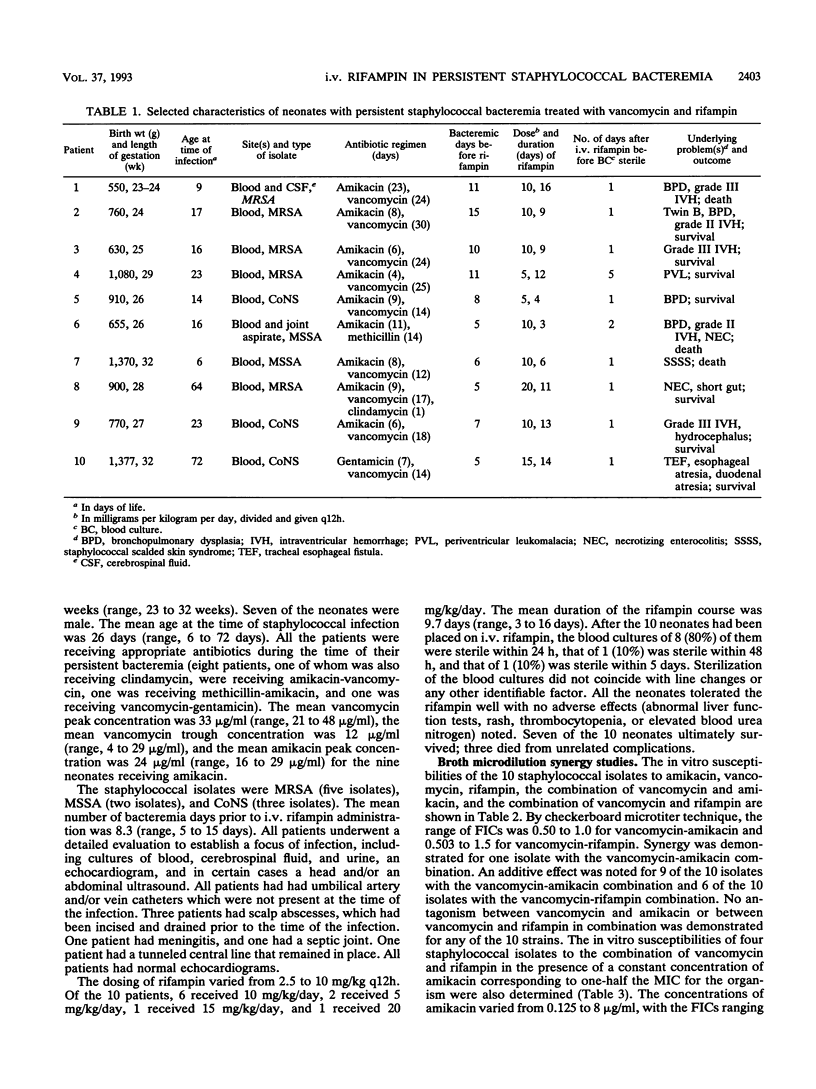
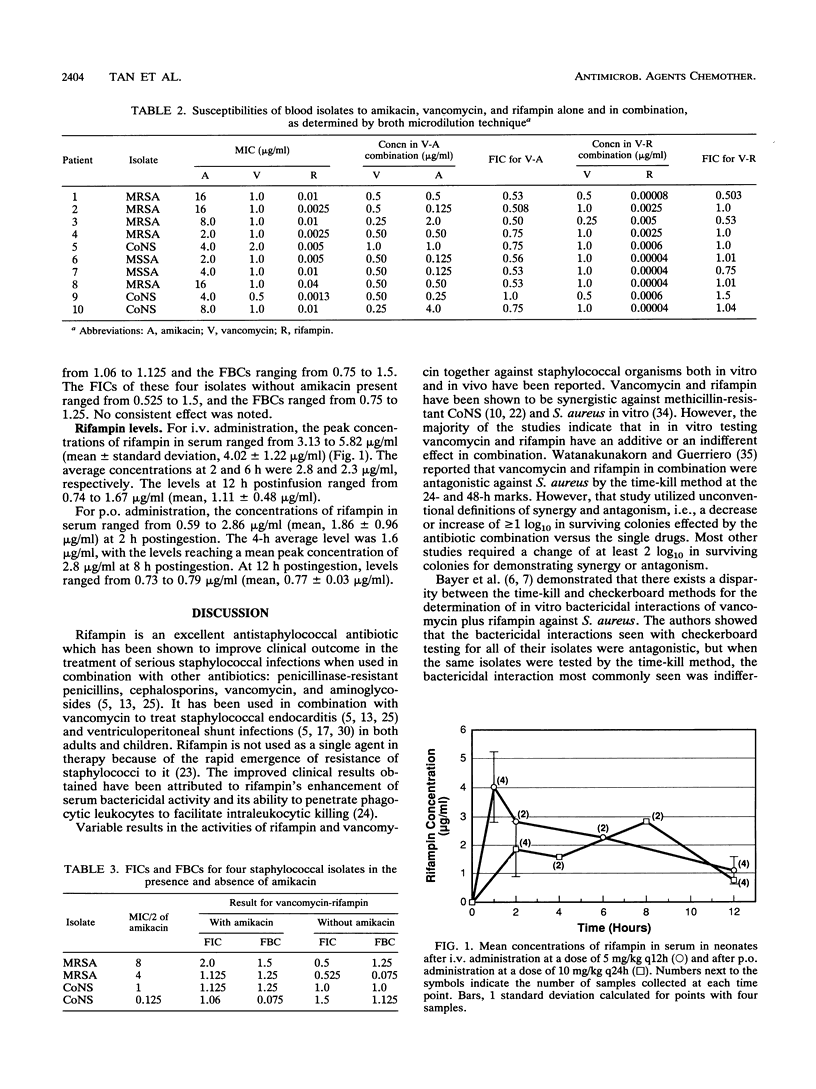
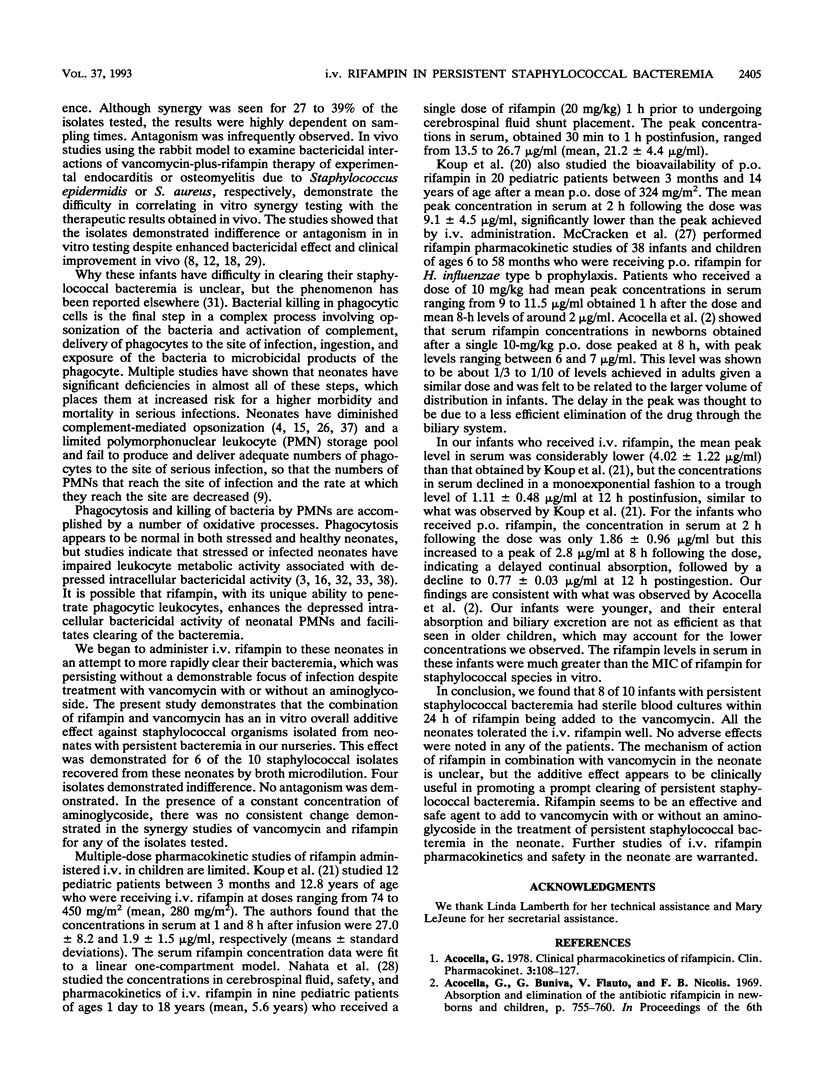
Ten neonates with persistent staphylococcal bacteremia (positive blood cultures for > or = 5 days despite appropriate antibiotic therapy) received intravenous (i.v.) rifampin in combination with vancomycin with or without aminoglycoside. Their mean birth weight and length of gestation were 900 g and 27 weeks, respectively. Their ages at the time of infection ranged from 6 to 64 days (mean, 26 days). The staphylococcal isolates were methicillin-resistant Staphylococcus aureus (five isolates), methicillin-susceptible S. aureus (two isolates), and coagulase-negative staphylococci (three isolates). The mean number of bacteremia days prior to administration of i.v. rifampin was 8.3 (range, 5 to 15 days), despite a mean peak vancomycin concentration of 33 micrograms/ml. The dosing of rifampin varied from 2.5 to 10 mg/kg of body weight every 12 h. The mean duration of the rifampin course was 9.7 days (range, 3 to 16 days). Of the 10 neonates, 8 (80%) had sterile blood cultures within 24 h, 1 (10%) had a sterile blood culture within 48 h, and 1 (10%) had a sterile blood culture within 5 days of being placed on i.v. rifampin. No adverse effects were noted in this small group of infants. Seven of the 10 neonates survived; three died from unrelated complications. The MIC ranges of amikacin, vancomycin, and rifampin for the isolates were 2.0 to 16, 0.5 to 2.0, and 0.0013 to 0.04 micrograms/ml, respectively. We also studied eight infants, with a mean age of 23 days, who were receiving i.v. or oral rifampin at a dose of 10 mg/kg/day. For i.v. administration, the peak serum concentration of rifampin (mean +/- standard deviation) was 4.02 +/- 1.22 microgram/ml. The mean trough level at 12 h postifution was 1.11 +/- 0.48 micrograms/ml. For oral administration, the concentrations of rifampin in serum ranged from 0.59 to 2.86 micrograms/ml (mean, 1.86 +/- 0.96 microgram/ml) at 2 h postingestion, increasing to a peak concentration of 2.8 micrograms/ml at 8 h postingestion. The mean 12-h postingestion level was 0.77 +/- 0.03 microgram/ml. From the study of this limited series of neonates, rifampin appears to be a safe and effective addition to therapy when staphylococcal bacteremia is persistent despite vancomycin treatment.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Acocella G. Clinical pharmacokinetics of rifampicin. Clin Pharmacokinet. 1978 Mar-Apr;3(2):108–127. doi: 10.2165/00003088-197803020-00002. [DOI] [PubMed] [Google Scholar]
- Ambruso D. R., Altenburger K. M., Johnston R. B., Jr Defective oxidative metabolism in newborn neutrophils: discrepancy between superoxide anion and hydroxyl radical generation. Pediatrics. 1979 Nov;64(5 Pt 2 Suppl):722–725. [PubMed] [Google Scholar]
- Anderson D. C., Hughes B. J., Edwards M. S., Buffone G. J., Baker C. J. Impaired chemotaxigenesis by type III group B streptococci in neonatal sera: relationship to diminished concentration of specific anticapsular antibody and abnormalities of serum complement. Pediatr Res. 1983 Jun;17(6):496–502. doi: 10.1203/00006450-198306000-00015. [DOI] [PubMed] [Google Scholar]
- Archer G. L., Tenenbaum M. J., Haywood H. B., 3rd Rifampin therapy of Staphylococcus epidermidis. Use in infections from indwelling artificial devices. JAMA. 1978 Aug 25;240(8):751–753. [PubMed] [Google Scholar]
- Bayer A. S., Lam K. Efficacy of vancomycin plus rifampin in experimental aortic-valve endocarditis due to methicillin-resistant Staphylococcus aureus: in vitro-in vivo correlations. J Infect Dis. 1985 Jan;151(1):157–165. doi: 10.1093/infdis/151.1.157. [DOI] [PubMed] [Google Scholar]
- Bayer A. S., Morrison J. O. Disparity between timed-kill and checkerboard methods for determination of in vitro bactericidal interactions of vancomycin plus rifampin versus methicillin-susceptible and -resistant Staphylococcus aureus. Antimicrob Agents Chemother. 1984 Aug;26(2):220–223. doi: 10.1128/aac.26.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenbaum M. C. A method for testing for synergy with any number of agents. J Infect Dis. 1978 Feb;137(2):122–130. doi: 10.1093/infdis/137.2.122. [DOI] [PubMed] [Google Scholar]
- Christensen R. D., Rothstein G. Exhaustion of mature marrow neutrophils in neonates with sepsis. J Pediatr. 1980 Feb;96(2):316–318. doi: 10.1016/s0022-3476(80)80837-7. [DOI] [PubMed] [Google Scholar]
- Ein M. E., Smith N. J., Aruffo J. F., Heerema M. S., Bradshaw M. W., Williams T. W., Jr Susceptibility and synergy studies of methicillin-resistant Staphylococcus epidermidis. Antimicrob Agents Chemother. 1979 Nov;16(5):655–659. doi: 10.1128/aac.16.5.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantin B., Carbon C. In vivo antibiotic synergism: contribution of animal models. Antimicrob Agents Chemother. 1992 May;36(5):907–912. doi: 10.1128/aac.36.5.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faville R. J., Jr, Zaske D. E., Kaplan E. L., Crossley K., Sabath L. D., Quie P. G. Staphylococcus aureus endocarditis. Combined therapy with vancomycin and rifampin. JAMA. 1978 Oct 27;240(18):1963–1965. doi: 10.1001/jama.240.18.1963. [DOI] [PubMed] [Google Scholar]
- Feldman W. E. Effect of ampicillin and chloramphenicol against Haemophilus influenzae. Pediatrics. 1978 Mar;61(3):406–409. doi: 10.1542/peds.61.3.406. [DOI] [PubMed] [Google Scholar]
- Fleer A., Gerards L. J., Aerts P., Westerdaal N. A., Senders R. C., van Dijk H., Verhoef J. Opsonic defense to Staphylococcus epidermidis in the premature neonate. J Infect Dis. 1985 Nov;152(5):930–937. doi: 10.1093/infdis/152.5.930. [DOI] [PubMed] [Google Scholar]
- Gopal V., Bisno A. L., Silverblatt F. J. Failure of vancomycin treatment in Staphylococcus aureus endocarditis. In vivo and in vitro observations. JAMA. 1976 Oct 4;236(14):1604–1606. [PubMed] [Google Scholar]
- Kapusnik J. E., Parenti F., Sande M. A. The use of rifampicin in staphylococcal infections--a review. J Antimicrob Chemother. 1984 Jun;13 (Suppl 100):61–66. doi: 10.1093/jac/13.suppl_c.61. [DOI] [PubMed] [Google Scholar]
- Kobasa W. D., Kaye K. L., Shapiro T., Kaye D. Therapy for experimental endocarditis due to Staphylococcus epidermidis. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S533–S537. doi: 10.1093/clinids/5.supplement_3.s533. [DOI] [PubMed] [Google Scholar]
- Koup J. R., Williams-Warren J., Viswanathan C. T., Weber A., Smith A. L. Pharmacokinetics of rifampin in children. II. Oral bioavailability. Ther Drug Monit. 1986;8(1):17–22. doi: 10.1097/00007691-198603000-00004. [DOI] [PubMed] [Google Scholar]
- Koup J. R., Williams-Warren J., Weber A., Smith A. L. Pharmacokinetics of rifampin in children. I. Multiple dose intravenous infusion. Ther Drug Monit. 1986;8(1):11–16. doi: 10.1097/00007691-198603000-00003. [DOI] [PubMed] [Google Scholar]
- Lowy F. D., Chang D. S., Lash P. R. Synergy of combinations of vancomycin, gentamicin, and rifampin against methicillin-resistant, coagulase-negative staphylococci. Antimicrob Agents Chemother. 1983 Jun;23(6):932–934. doi: 10.1128/aac.23.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell G. L., Vest T. K. Killing of intraleukocytic Staphylococcus aureus by rifampin: in-vitro and in-vivo studies. J Infect Dis. 1972 May;125(5):486–490. doi: 10.1093/infdis/125.5.486. [DOI] [PubMed] [Google Scholar]
- Massanari R. M., Donta S. T. The efficacy of rifampin as adjunctive therapy in selected cases of staphylococcal endocarditis. Chest. 1978 Mar;73(3):371–375. doi: 10.1378/chest.73.3.371. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr, Eichenwald H. F. Leukocyte function and the development of opsonic and complement activity in the neonate. Am J Dis Child. 1971 Feb;121(2):120–126. doi: 10.1001/archpedi.1971.02100130074008. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr, Ginsburg C. M., Zweighaft T. C., Clahsen J. Pharmacokinetics of rifampin in infants and children: relevance to prophylaxis against Haemophilus influenzae type b disease. Pediatrics. 1980 Jul;66(1):17–21. [PubMed] [Google Scholar]
- Nahata M. C., Fan-Havard P., Barson W. J., Bartkowski H. M., Kosnik E. J. Pharmacokinetics, cerebrospinal fluid concentration, and safety of intravenous rifampin in pediatric patients undergoing shunt placements. Eur J Clin Pharmacol. 1990;38(5):515–517. doi: 10.1007/BF02336694. [DOI] [PubMed] [Google Scholar]
- Norden C. W., Shaffer M. Treatment of experimental chronic osteomyelitis due to staphylococcus aureus with vancomycin and rifampin. J Infect Dis. 1983 Feb;147(2):352–357. doi: 10.1093/infdis/147.2.352. [DOI] [PubMed] [Google Scholar]
- Patrick C. C., Kaplan S. L., Baker C. J., Parisi J. T., Mason E. O., Jr Persistent bacteremia due to coagulase-negative staphylococci in low birth weight neonates. Pediatrics. 1989 Dec;84(6):977–985. [PubMed] [Google Scholar]
- Shigeoka A. O., Santos J. I., Hill H. R. Functional analysis of neutrophil granulocytes from healthy, infected, and stressed neonates. J Pediatr. 1979 Sep;95(3):454–460. doi: 10.1016/s0022-3476(79)80535-1. [DOI] [PubMed] [Google Scholar]
- Stoerner J. W., Pickering L. K., Adcock E. W., 3rd, Morriss F. H., Jr Polymorphonuclear leukocyte function in newborn infants. J Pediatr. 1978 Nov;93(5):862–864. doi: 10.1016/s0022-3476(78)81102-0. [DOI] [PubMed] [Google Scholar]
- Tuazon C. U., Lin M. Y., Sheagren J. N. In vitro activity of rifampin alone and in combination with nafcillin and Vancomycin against pathogenic strains of Staphylococcus aureus. Antimicrob Agents Chemother. 1978 May;13(5):759–761. doi: 10.1128/aac.13.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanakunakorn C., Guerriero J. C. Interaction between vancomycin and rifampin against Staphylococcus aureus. Antimicrob Agents Chemother. 1981 Jun;19(6):1089–1091. doi: 10.1128/aac.19.6.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber A., Opheim K. E., Smith A. L., Wong K. High-pressure liquid chromatographic quantitation of rifampin and its two major metabolites in urine and serum. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S433–S439. doi: 10.1093/clinids/5.supplement_3.s433. [DOI] [PubMed] [Google Scholar]
- Wilson C. B. Immunologic basis for increased susceptibility of the neonate to infection. J Pediatr. 1986 Jan;108(1):1–12. doi: 10.1016/s0022-3476(86)80761-2. [DOI] [PubMed] [Google Scholar]
- Wright W. C., Jr, Ank B. J., Herbert J., Stiehm E. R. Decreased bactericidal activity of leukocytes of stressed newborn infants. Pediatrics. 1975 Oct;56(4):579–584. [PubMed] [Google Scholar]


