Abstract
BACKGROUND
Disclosure of medical errors is encouraged, but research on how patients respond to specific practices is limited.
OBJECTIVE
This study sought to determine whether full disclosure, an existing positive physician-patient relationship, an offer to waive associated costs, and the severity of the clinical outcome influenced patients' responses to medical errors.
PARTICIPANTS
Four hundred and seven health plan members participated in a randomized experiment in which they viewed video depictions of medical error and disclosure.
DESIGN
Subjects were randomly assigned to experimental condition. Conditions varied in type of medication error, level of disclosure, reference to a prior positive physician-patient relationship, an offer to waive costs, and clinical outcome.
MEASURES
Self-reported likelihood of changing physicians and of seeking legal advice; satisfaction, trust, and emotional response.
RESULTS
Nondisclosure increased the likelihood of changing physicians, and reduced satisfaction and trust in both error conditions. Nondisclosure increased the likelihood of seeking legal advice and was associated with a more negative emotional response in the missed allergy error condition, but did not have a statistically significant impact on seeking legal advice or emotional response in the monitoring error condition. Neither the existence of a positive relationship nor an offer to waive costs had a statistically significant impact.
CONCLUSIONS
This study provides evidence that full disclosure is likely to have a positive effect or no effect on how patients respond to medical errors. The clinical outcome also influences patients' responses. The impact of an existing positive physician-patient relationship, or of waiving costs associated with the error remains uncertain.
Keywords: medical error, disclosure, physician, patient relationship, compensation and redress
It is well established that medical errors occur at alarmingly high rates.1 Patients and the public strongly favor disclosure of medical errors,2–6 but physicians often do not disclose.3,7–10 Physicians' concerns about damage to the physician-patient relationship and about legal risk are 2 major barriers to full disclosure. While experts have suggested that full disclosure is both ethically correct and likely to result in better outcomes for physicians and patients,11–25 there has been limited empirical research into the specific factors that influence patients' responses. Recent findings suggest that patients are likely to respond favorably to full disclosure, with full disclosure associated with lower likelihood of changing physicians, higher satisfaction, greater trust, a more positive emotional response, and less support for sanctions against the physician.2,26 The purpose of the present study was to further examine the factors that influence patients' responses to errors. Specifically, we sought to examine the impact of 4 factors: a positive physician-patient relationship before the occurrence of the error, the clinical outcome of the error, the level of disclosure following the error, and an offer to waive costs associated with the error. We measured 5 patient responses: likelihood of changing physicians, likelihood of seeking legal advice, satisfaction, trust, and emotional response. We used a randomized experimental design, and recruited study subjects to view videos of simulated physician-patient encounters, and to report their responses as if they were the patient or family member involved.
METHODS
Study Subjects
Four hundred and seven members of a large New England–based health maintenance organization were recruited. Letters of invitation were sent to 7,600 members, randomly sampled from a master list of all members age 21–85 years (N = 128,615). Letters described the study as focusing on doctor-patient communication about medical errors, stressed that participation was voluntary, and offered a $25 incentive. Subjects were randomly assigned to experimental condition upon arrival at the study session. Each subject viewed the video and completed the questionnaire alone.
Experimental Conditions
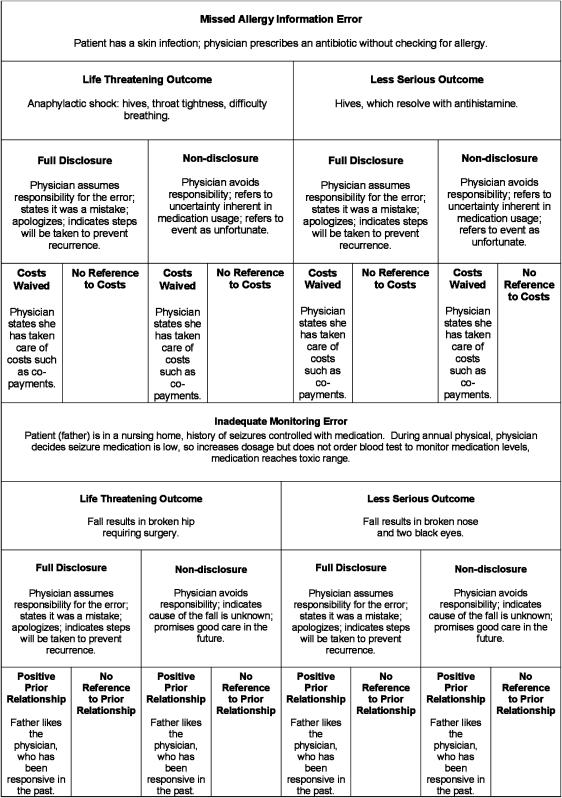
Sixteen versions of the video were produced. The vignette/dialogue combinations comprising each condition are summarized in Figure 1. Two different medication errors were used: inadequate monitoring of antiepileptic medication and prescribing a penicillin-type antibiotic in the presence of a documented penicillin allergy. For each of these errors, the clinical outcome of the error was varied (life-threatening outcome vs less serious outcome), as was the level of physician disclosure about the error (nondisclosure, with limited information and avoidance of responsibility vs full disclosure, with high information, an explicit acknowledgement of responsibility, and a promise to prevent recurrences). Within the inadequate monitoring error situation, a prior positive relationship was conveyed through additional background information presented in text and voiceover indicating that the physician was pleasant, responded promptly to questions, was knowledgeable about the patient, and was well-liked by the patient. The alternative contained no reference to prior interactions with the physician. Within the missed allergy error, an offer to waive costs condition was simulated by the physician informing the patient that she had arranged for patient-incurred costs associated with the error, such as co-payments for visits or medications, to be “taken care of.” The alternative contained no reference to costs.
FIGURE 1.
Description of study conditions.
The description of the error and clinical outcome was presented in text with voiceover. The physician–patient dialogues were enacted. The actors were the same for all versions; where the dialogue was the same across conditions, the same footage was used. Each subject viewed 1 version of the video; assignment was randomized.
Dependent Measures
Subjects were instructed to imagine themselves in the place of the patient or family member in the video when responding. Three items assessed whether the vignettes were effective in communicating as intended; specifically whether subjects perceived that an error had been made, whether the physician was perceived as responsible, and whether the error was perceived as preventable. Five response options were provided: Strongly Disagree, Disagree, Agree, Strongly Agree, and Don't Know.
Subjects responded whether they would change physicians or seek legal advice. For the analysis, responses were dichotomized, with Agree/Strongly Agree responses compared with Strongly Disagree/Disagree/Don't Know. Patient satisfaction was assessed using 5 items drawn from an established scale.27 Trust was assessed using 8 items drawn from the Trust in Physician Scale,28 plus a supplemental item (“This doctor seemed to be withholding important information”). Satisfaction and trust items were modified to refer to the vignette, rather than a real encounter. Emotional response was computed as the mean across 5 semantic differential items drawn from a prior study2; higher scores indicated a more positive emotional response.
Background and Demographic Items
Final items queried personal experience with medical error or injury, history of having filed a complaint or malpractice suit against a doctor or other health care provider, experience working in health care, relationship with current or most recent provider, gender, education, age, and race/ethnicity.
ANALYSIS
Responses to the missed allergy error and the monitoring error were analyzed separately. Logistic regression was used to evaluate associations between the 4 design variables (existence of a positive prior relationship, severity of clinical outcome, level of disclosure, and an offer to waive costs) and the dichotomously coded dependent variables (likelihood of changing physicians and likelihood of seeking legal advice). Odds ratios (OR) and 95% confidence intervals (CIs) were estimated. Linear regression was used to evaluate the association between the design variables and the dependent variables patient satisfaction, trust, and emotional response. Linear regression coefficients and 95% CIs were estimated. For each dependent variable, a series of regression analyses were conducted. In order to determine which covariates should be included in the final models, we first evaluated models which adjusted for age, gender, education, race/ethnicity, experience working in health care, current relationship with provider, personal experience with errors and personal suffering, in addition to the design variables. Final models included the design variables and all covariates found to be statistically significant in at least one analysis (using the criterion of P < 0.05). Results reported in Tables 2 and 3 are from these adjusted final models. Model based means and percentages were estimated by setting other variables in the model to their mean values. Interactions were evaluated by analyzing models that included the design variables and all possible 2-way interactions; models including the design variables and all possible 3-way interactions were also analyzed. Significant interactions are reported (using the criterion of P < 0.05). Statistical analyses were performed using Stata software, version 8 (Stata Corporation, College Station, TX) and SPSS software, version 11.5 (SPSS, Inc., Chicago, IL).
Table 2.
Predictors of Changing Physicians and Seeking Legal Advice
| Would Probably Change Physicians | Would Probably Seek Legal Advice | |||
|---|---|---|---|---|
| Agreement* (%) | Odds Ratio (95% CI) | Agreement* (%) | Odds Ratio (95% CI) | |
| Missed allergy error | ||||
| Full disclosure | 19.1 | 1 (reference) | 3.8 | 1 (reference) |
| Nondisclosure | 46.7 | 3.70 (1.86,7.35) | 10.9 | 3.12 (1.11,8.75) |
| No mention of costs | 27.0 | 1 (reference) | 4.2 | 1 (reference) |
| Offer to waive costs | 36.9 | 1.53 (0.80,2.94) | 9.8 | 2.49 (0.94,6.61) |
| Less serious outcome | 20.0 | 1 (reference) | 2.4 | 1 (reference) |
| Life threatening outcome | 45.5 | 3.33 (1.71,6.47) | 16.3 | 7.87 (2.39,25.9) |
| Monitoring error | ||||
| Full disclosure | 44.5 | 1 (reference) | 21.8 | 1 (reference) |
| Nondisclosure | 64.7 | 2.29 (1.25,4.21) | 21.4 | 0.98 (0.49,1.96) |
| No mention of prior relationship | 58.9 | 1 (reference) | 23.4 | 1 (reference) |
| Positive prior relationship | 50.3 | 0.70 (0.38,1.29) | 19.9 | 0.81 (0.41,1.62) |
| Less serious outcome | 43.8 | 1 (reference) | 12.7 | 1 (reference) |
| Life threatening outcome | 65.6 | 2.45 (1.33,4.52) | 35.0 | 3.68 (1.79,7.59) |
Adjusted for current relationship with provider, gender, race/ethnicity, and age.
Older subjects were less likely to seek legal advice (OR 0.19; 95% CI 0.05, 0.78; P = 0.02) in the missed allergy error condition.
Older subjects were less likely to change doctors (OR 0.46; 95% CI 0.23, 0.92; P = 0.03) or seek legal advice (OR 0.40, 95% CI 0.17,0.89; P = 0.04) in the monitoring error condition.
CI, confidence interval; OR, odds ratio.
Table 3.
Predictors of Satisfaction, Trust and Emotional Response: Each Error Modeled Separately
| Patient Satisfaction* | Trust in Physician* | Patient Emotional Response* | ||||
|---|---|---|---|---|---|---|
| Mean† | Difference (95% CI) | Mean† | Difference (95% CI) | Mean† | Difference (95% CI) | |
| Missed allergy error | ||||||
| Full disclosure | 3.72 | −1.79 | 3.46 | −1.11 | 2.92 | −0.74 |
| Nondisclosure | 1.93 | (−2.02,−1.55) | 2.35 | (−1.31,−0.90) | 2.18 | (−1.01,−0.47) |
| No mention of reimbursement | 2.84 | −0.04 | 2.93 | −0.06 | 2.50 | 0.09 |
| Offer to reimburse costs | 2.80 | (−0.27,0.19) | 2.87 | (−0.26,0.14) | 2.59 | (−0.17,0.35) |
| Less serious outcome | 2.84 | −0.06 | 2.97 | −0.15 | 2.81 | −0.53 |
| Life threatening outcome | 2.79 | (−0.29,0.18) | 2.82 | (−0.35,0.05) | 2.28 | (−0.79,−0.26) |
| Monitoring error | ||||||
| Full disclosure | 3.59 | −1.75 | 3.11 | −0.89 | 2.53 | −0.55 |
| Nondisclosure | 1.84 | (−1.98,−1.52) | 2.23 | (−1.08,−0.70) | 1.98 | (−0.79,0.30) |
| No mention of prior relationship | 2.63 | 0.20 | 2.64 | 0.08 | 2.19 | 0.13 |
| Positive prior relationship | 2.83 | (−0.03,0.43) | 2.72 | (−0.11,0.27) | 2.32 | (−0.12,0.37) |
| Less serious outcome | 2.66 | 0.14 | 2.64 | 0.07 | 2.37 | −0.24 |
| Life threatening outcome | 2.80 | (−0.09,0.36) | 2.71 | (−0.12,0.26) | 2.13 | (−0.48,0.00) |
Higher scores indicate a more positive response.
Model-based means adjusted for current relationship with provider, gender, race/ethnicity, and age.
In the monitoring error condition, white subjects tended to report greater satisfaction (difference = 0.69; 95% CI 0.07,1.31; P = 0.03).
In the missed allergy condition, subjects who rated their relationship with their own physician as excellent or very good tended to report greater trust (difference 0.249; 95% CI 0.03,0.47; P = 0.03), as did older subjects (difference 0.26; 95% CI 0.04,0.48; P = 0.02). In the monitoring error condition, female subjects tended to report less trust (difference = −0.21;95% CI–0.41, −0.00; P = 0.05).
In the missed allergy condition, subjects who rated their relationship with their own physician as excellent or very good tended to report a more positive emotional response (difference = 0.32; 95% CI 0.02,0.61; P = 0.04).
CI, confidence interval; OR, odds ratio.
The study protocol was approved by the Institutional Review Boards of the participating health plan and the University of Massachusetts Medical School.
RESULTS
Random assignment resulted in groups balanced in terms of age, gender, education, personal experience with errors, personal suffering because of errors, and experience working in health care. Randomization did not result in groups balanced with regard to race/ethnicity; however, all analyses included race/ethnicity to control for this.
Table 1 presents subjects' characteristics. Women were overrepresented in the sample (63.7% compared with 52.5% of the population from which our sample was drawn). The majority of subjects self-identified as white (92.6%), consistent with the U.S. census statistics for this area, where 89.6% of respondents self-identified as white (29); 34.7% of study subjects age 25 or older reported a 4-year college degree or higher, compared with 27% of census respondents age 25 or older.29 Almost one quarter of study subjects (22.7%) reported ever having worked in health care; 44.7% reported personal experience of a medical error in their own treatment or in the treatment of a close family member; 20.7% reported having personally suffered an injury or harm as the result of a medical error. Very few (0.5%) had ever filed a claim or lawsuit against a physician or other health care provider; 8.1% reported having filed a complaint against a provider. Most subjects (71.2%) reported an excellent or very good relationship with their provider.
Table 1.
Characteristics of Subjects
| Characteristic | n | % |
|---|---|---|
| Age | ||
| 21 to 24 | 10 | 2.5 |
| 25 to 34 | 34 | 8.4 |
| 35 to 44 | 59 | 14.5 |
| 45 to 54 | 87 | 21.4 |
| 55 to 64 | 91 | 22.4 |
| 65 to 74 | 81 | 19.9 |
| 75 or older | 43 | 10.6 |
| Missing data | 2 | 0.5 |
| Sex | ||
| Men | 147 | 36.3 |
| Women | 258 | 63.7 |
| Missing data | 2 | 0.5 |
| Race/ethnicity | ||
| American Indian or Alaska Native | 3 | 0.7 |
| Asian | 2 | 0.5 |
| Black or African American | 6 | 1.5 |
| Hispanic or Latino | 7 | 1.7 |
| White | 377 | 92.6 |
| Other | 7 | 1.7 |
| Multi-racial | 1 | 0.2 |
| Missing data | 4 | 1.0 |
| Education | ||
| Eighth grade or less | 3 | 0.7 |
| Some high school | 19 | 4.7 |
| High school graduate or GED | 92 | 22.6 |
| Some college or 2 y degree | 149 | 36.6 |
| 4 y college graduate | 65 | 16.0 |
| 4 y college graduate | 77 | 18.9 |
| Missing data | 2 | 0.5 |
Validation of Error Vignettes
The majority of subjects in all conditions agreed the doctor had made an error (96.0%), that the doctor was at fault (93.7%), and that the incident could have been prevented (95.3%).
Multivariate Results
Results of the logistic regression analyses predicting intent to change physicians and intent to seek legal advice are presented in Table 2. Odds ratios are adjusted for relationship with current provider, gender, race/ethnicity, and age. The top portion of the table contains results for the missed allergy error conditions, the bottom portion contains results for the monitoring error conditions.
Considering first intent to change physicians, the results in Table 2 indicate that for both error conditions, subjects were more likely to change physicians when the physician failed to fully disclose, and when the outcome of the error was life threatening. The ORs associated with offering to waive costs and a prior positive relationship for changing physicians were not statistically significant. However for the missed allergy error, there was a statistically significant interaction between the clinical outcome of the error and offering to waive costs. When the outcome was serious and the physician offered to waive costs, subjects were more likely to report that they would change physicians. When the physician did not mention costs, 12% of subjects would change physicians; when she did offer to waive costs, this increased to 32.7% (OR = 0.23, 95% CI: 0.06,0.92, P = 0.04).
Considering intent to seek legal advice, nondisclosure resulted in an increased likelihood of seeking legal advice in the missed allergy error condition, but did not have a statistically significant impact on seeking legal advice in the monitoring error condition. The ORs for offering to waive costs and for a prior positive relationship were not statistically significant. For both error conditions, subjects were more likely to report that they would seek legal advice when the outcome of the error was life threatening.
Results of the linear regression analyses predicting satisfaction, trust, and emotional response are presented in Table 3. Again, the top portion of the table contains results for the missed allergy error, and the bottom portion contains results for the monitoring error. All means are adjusted for relationship with current provider, gender, race/ethnicity, and age.
The results reported in Table 3 indicate that in both error conditions, subjects provided significantly lower satisfaction ratings when the physician did not fully disclose. Neither the existence of a prior positive relationship, offering to waive costs, nor the clinical outcome of the error had a statistically significant impact on satisfaction. However, a statistically significant interaction related to satisfaction was noted; in the monitoring error condition, the life-threatening outcome reduced the impact of nondisclosure by an additional decrease in satisfaction of 0.56 (95% CI: −1.01,−0.11; P = 0.02) compared with the impact of nondisclosure in the serious outcome condition.
Subjects reported less trust in the physician when she did not disclose in both error conditions. Neither the offer to waive costs nor reference to a prior positive relationship had a statistically significant impact on trust. The clinical outcome of the error also had no statistically significant impact on trust in either error condition.
Nondisclosure was also associated with a more negative emotional response in the missed allergy error, but this relationship was not statistically significant in the monitoring error condition. Neither the offer to waive costs nor the existence of a prior positive relationship had a statistically significant impact on emotional response. Subjects reported a more negative emotional response when the clinical outcome was life threatening in the missed allergy error; for the monitoring error the difference in emotional response associated with clinical outcome was slightly above the criterion for statistical significance (P = 0.053).
DISCUSSION
This study confirms earlier findings that full disclosure results in a more positive response on the part of the patient or family member in terms of satisfaction and trust, and reduces the likelihood of changing physicians.2,26 The impact of disclosure on seeking legal advice varied across the 2 error conditions; full disclosure reduced the likelihood of seeking legal advice in the missed allergy error situation, but had no detectable impact in the inadequate monitoring error situation. This is consistent with findings from a prior study,2 which also found no statistically significant association between disclosure and seeking legal advice in the monitoring error condition. Overall, our results suggest that full disclosure is likely to have either a positive impact or no impact on patients and family members; we found no evidence that full disclosure increases the risk of negative consequences for physicians.
The relationship between disclosure and legal repercussions is a particular concern to physicians. Patient safety experts and ethicists advise physicians to be forthcoming to patients when errors occur, but empirical evidence on the relationship between disclosure and legal consequences is limited.30,31 Studies have found that patients and family members pursuing legal action subsequent to an error are often motivated by the desire for explanations and apologies32–35; however, such studies do not provide evidence that full disclosure can prevent legal action.30,31
We anticipated that a positive relationship with the physician before the error incident could have a protective effect, mitigating negative feelings, and actions on the part of the patient or family. While we detected no statistically significant beneficial effect of a prior positive relationship, our inability to detect an impact should not be construed as evidence of no effect. First, we may not have had sufficient statistical power to detect an impact. Alternatively, our effort to simulate a prior positive relationship may have been unsuccessful. It also is possible that subjects' relationship with their own providers influenced their perceptions of the physician in the vignette. Although we included ratings of subjects' relationship with their current provider in the regression models, our models do not fully evaluate the extent to which subjects' prior experiences may have influenced responding. Our nonsignificant results are in contrast to findings suggesting that how providers communicate with patients in routine encounters is predictive of the provider malpractice status.36,37 However, we note that findings from earlier studies of the importance of communication behaviors in predicting malpractice focused on routine encounters and physician-patient relationships, not on the question of whether a positive relationship was influential once an error occurred. Future research should explore this issue more fully.
Our findings call into question the assumption that patients will necessarily respond positively to an offer to waive the costs associated with a medical error. While the vast majority of patients would want the medical fees related to an error waived,2 with one exception, we failed to detect a statistically significant association between offering to waive costs and patients' responses. The exception was the finding of a statistically significant interaction between the clinical outcome of the error and offering to waive costs: when the clinical outcome was less serious, offering to waive costs was associated with higher rates of intent to change physician (compared with no reference to waiving costs). It is noteworthy that in this instance the impact of offering to waive costs was negative rather than positive. The interaction effect also suggests that how patients respond to an offer to waive costs may depend on other aspects of the error situation. The finding of no effect or a negative effect of waiving costs may appear to contradict the work of Kraman and Hamm,25 who reported that full disclosure and assistance in obtaining financial compensation may reduce the amount, if not the number of claims. However, that study was conducted in the context of the Veteran's Administration (VA), an atypical system, whose providers are protected from malpractice litigation. Further, it was an institutional case study of the impact of the “extreme honesty” policy, which entailed providing information about what had occurred, an apology, and assistance in obtaining financial compensation. Thus, it was not possible to evaluate the independent effect of financial assistance, or to consider how other factors may have influenced such an effect. Finally, while introduction of the extreme honesty policy appeared to reduce the amount paid out in claims, it is less clear that it reduced the number of claims, and data on other patient outcomes were not reported.
The finding that the clinical outcome of the error has a significant impact on how patients and families respond is consistent with prior findings.2,26 It not surprising that patients and family members are likely to be more distressed by a life threatening error, as well as more likely to change providers and seek legal advice.
Using an experimental design, we were able to overcome a number of limitations inherent in observational survey studies; however, this study does have limitations. Because participants were drawn from a single geographic area, and were predominantly white, the extent to which these findings are generalizable to other geographic areas and other racial/ethnic groups is not known. Further, we are unable to assess whether the relatively high percentage of female participants biased the results. As participation required coming to a central study location, subjects were necessarily those with the ability, time, and motivation to do so. Both of these factors may have limited the extent to which those who participated are representative of the general population, even in this geographic area. The fact that subjects were recruited from the membership of an HMO may also have had an impact on generalizability; for instance, trust level may differ as a function of insurance type. Finally, we note that we did not have sufficient power to fully test interactions between design variables.
The findings from this study underscore the need for additional research, particularly into the determinants of seeking legal advice and the effects of discussions of patient-incurred costs. While simulation studies such as this are valuable in that they allow systematic manipulation of key variables, research into the content and impact of what practicing physicians actually say following medical errors is needed. It would also be informative to query patients who believe they have been harmed as a result of a medical error, but who decide not to take legal action. Over 20% of the subjects in this study reported having personally suffered an injury or harm as the result of a medical error, but less than half of 1% reported filing a malpractice suit against a provider. These findings are consistent with findings from national surveys in the United States, where 34%10 or 42%4 of the public report personal experience with an error in their own care or the care of a family member, and in Germany, where 30% report an error in their own care.26 While several studies have focused on patients involved in or considering legal action,32–35 to our knowledge, there have been no studies of patients who believe they have been injured, but did not pursue legal action. This may be a promising direction for future research.
Full disclosure may seem risky to a physician faced with a patient who has experienced a medical error, but the results presented here suggest that full disclosure is likely to have either a positive impact or no impact on patients and family members; we found no evidence that full disclosure increases the risk of negative consequences for physicians. Further work is needed to clarify the impact of an existing positive physician-patient relationship, and of waiving costs associated with the error.
Acknowledgments
Funding/Support: This study was supported by a grant from the National Patient Safety Foundation and the Commonwealth Fund (20030288).
REFERENCES
- 1.Kohn LT, Corrigan JM, Donaldson M. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Mazor KM, Simon SR, Yood RA, et al. Health plan members' views about disclosure of medical errors. Ann Intern Med. 2004;140:409–18. doi: 10.7326/0003-4819-140-6-200403160-00006. [DOI] [PubMed] [Google Scholar]
- 3.Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients and physicians attitudes regarding the disclosure of medical errors. JAMA. 2003;289:1001–7. doi: 10.1001/jama.289.8.1001. [DOI] [PubMed] [Google Scholar]
- 4.Blendon R, DesRoches CM, Brodie M, et al. Views of practicing physicians and the public on medical errors. N Engl J Med. 2002;347:1933–40. doi: 10.1056/NEJMsa022151. [DOI] [PubMed] [Google Scholar]
- 5.Hobgood C, Peck CR, Gilbert B, Chappell K, Zou B. Medical errors–what and when: what do patients want to know? Acad Emerg Med. 2002;9:1156–61. doi: 10.1197/aemj.9.11.1156. [DOI] [PubMed] [Google Scholar]
- 6.Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156:2565–9. [PubMed] [Google Scholar]
- 7.Mizrahi T. Managing medical mistakes: ideology, insularity and accountability among internists-in-training. Soc Sci Med. 1984;19:135–46. doi: 10.1016/0277-9536(84)90280-6. [DOI] [PubMed] [Google Scholar]
- 8.Wu AW, Folkman S, McPhee SJ, Lo B. Do house officers learn from their mistakes? JAMA. 1991;265:2089–94. [PubMed] [Google Scholar]
- 9.Lamb RM, Studdert DM, Bohmer RMJ, Berwick D, Brennan TA. Hospital disclosure practices: results of a national survey. Health Aff. 2003;22:73–83. doi: 10.1377/hlthaff.22.2.73. [DOI] [PubMed] [Google Scholar]
- 10.The Kaiser Family Foundation, Agency for Healthcare Research and Quality, Harvard School of Public Health. National Survey on Consumers' Experiences with patient Safety and Quality Information. Summary and Chartpack. [December 2, 2004]; Available at http://www.kff.org/kaiserpolls/7209.cfm.
- 11.Baylis F. Errors in medicine: nurturing truthfulness. J Clin Ethics. 1997;8:336–40. [PubMed] [Google Scholar]
- 12.Finkelstein D, Wu AW, Holtzman NA, Smith MK. When a physician harms a patient by a medical error: ethical, legal, and risk-management considerations. J Clin Ethics. 1997;8:330–5. [PubMed] [Google Scholar]
- 13.Hebert PC. Disclosure of adverse events and errors in healthcare: an ethical perspective. Drug Safety. 2001;24:1095–104. doi: 10.2165/00002018-200124150-00001. [DOI] [PubMed] [Google Scholar]
- 14.Hebert PC, Levin AV, Robertson G. Bioethics for clinicians: 23. Disclosure of medical error. Can Med Assoc J. 2001;164:509–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Kapp MB. Legal anxieties and medical mistakes: barriers and pretexts. J Gen Intern Med. 1997;12:787–8. doi: 10.1046/j.1525-1497.1997.07167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kapp MB. Medical mistakes and older patients: admitting errors and improving care. J Am Geriatr Soc. 2001;49:1361–5. doi: 10.1046/j.1532-5415.2001.49267.x. [DOI] [PubMed] [Google Scholar]
- 17.Liang BA. A system of medical error disclosure. Qual Safety Health Care. 2002;11:64–8. doi: 10.1136/qhc.11.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.May T, Aulisio MP. Medical malpractice, mistake prevention, and compensation. Kennedy Inst Ethics J. 2001;11:135–46. doi: 10.1353/ken.2001.0014. [DOI] [PubMed] [Google Scholar]
- 19.Peterson LM, Brennan T. Medical ethics and medical injuries; taking our duties seriously. J Clin Ethics. 1990;1:207–11. [PubMed] [Google Scholar]
- 20.Porto GG. Disclosure of medical errors: facts and fallacies. J Health Care Risk Manage. 2001;21:67–76. doi: 10.1002/jhrm.5600210411. [DOI] [PubMed] [Google Scholar]
- 21.Rosner F, Berger JT, Kark P, Potash J, Bennett AJ. Disclosure and prevention of medical errors. Committee on Bioethical issues of the medical society of the state of New York. Arch Intern Med. 2000;160:2089–92. doi: 10.1001/archinte.160.14.2089. [DOI] [PubMed] [Google Scholar]
- 22.Smith ML, Forster HP. Morally managing medical mistakes. Camb Q Health Care Ethics. 2000;9:38–53. doi: 10.1017/s0963180100901051. [DOI] [PubMed] [Google Scholar]
- 23.Thurman AE. Institutional responses to medical mistakes: ethical and legal perspectives. Kennedy Inst Ethics J. 2001;11:147–56. doi: 10.1353/ken.2001.0018. [DOI] [PubMed] [Google Scholar]
- 24.Wu AW, Cavanaugh TA, McPhee SJ, Lo B, Micco GP. To tell the truth: ethical and practical issues in disclosing medical mistakes to patients. J Gen Intern Med. 1997;12:770–5. doi: 10.1046/j.1525-1497.1997.07163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med. 1999;131:963–7. doi: 10.7326/0003-4819-131-12-199912210-00010. [DOI] [PubMed] [Google Scholar]
- 26.Schwappach DLB, Koek CM. What makes an error unacceptable? A factorial survey on the disclosure of medical errors. Int J Qual Health Care. 2004;16:317–26. doi: 10.1093/intqhc/mzh058. [DOI] [PubMed] [Google Scholar]
- 27.American Board of Internal Medicine. Washington, DC: American Board of Internal Medicine; 1989. Final Report on the Patient Satisfaction Questionnaire Project. [Google Scholar]
- 28.Anderson L, Dedrick R. Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67:1091–100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau, Census. Massachusetts: Worcester County; 2000. [January 31, 2005]. Table DP-1. Profile of General Demographic Characteristics. Available at http://censtats.census.gov/data/ma/05025027.pdf. [Google Scholar]
- 30.Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med. 2004;164:1690–7. doi: 10.1001/archinte.164.15.1690. [DOI] [PubMed] [Google Scholar]
- 31.Kachalia A, Shojania KG, Hofer TP, Piotrowski M, Saint S. Does full disclosure of medical errors affect malpractice liability? Jt Comm J Qual Improv. 2003;29:503–11. doi: 10.1016/s1549-3741(03)29060-2. [DOI] [PubMed] [Google Scholar]
- 32.Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992;267:1359–63. [PubMed] [Google Scholar]
- 33.Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154:1365–70. [PubMed] [Google Scholar]
- 34.Vincent CA, Pincus T, Scurr JH. Patients' experience of surgical accidents. Qual Health Care. 1993;2:77–82. doi: 10.1136/qshc.2.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vincent C, Young M, Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet. 1994;343:1609–13. doi: 10.1016/s0140-6736(94)93062-7. [DOI] [PubMed] [Google Scholar]
- 36.Levinson W, Roter DL, Mullooly JP, et al. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553–9. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 37.Ambady N, Laplante D, Nguyen T, Rosenthal R, Chaumeton N, Levinson W. Surgeons' tone of voice: a clue to malpractice history. Surgery. 2002;132:5–9. doi: 10.1067/msy.2002.124733. [DOI] [PubMed] [Google Scholar]