Abstract
BACKGROUND
Federal law obligates health care providers receiving federal funding to ensure language access to limited English-proficient (LEP) individuals who cannot communicate with their provider.
OBJECTIVE
To determine whether LEP individual awareness of this law improved language access through interpreter utilization.
DESIGN, SETTING, AND PARTICIPANTS
In June 2003, a telephone survey of 1,200 Californians was conducted in 11 non-English languages.
MEASUREMENTS
The survey included items on English proficiency, awareness of language law, health care utilization, and communication methods. Language access was defined as having a provider who speaks the individual's language (language-concordant) or utilizing an interpreter.
RESULTS
There were 1,000 LEP participants, of whom 371 (37%) were aware of the language law. Four hundred and ninety-one (49%) of LEP participants had a language-concordant provider. Of the remaining 509 LEP participants without a language-concordant provider, 111 (22%) reported interpreter utilization in the health care setting. After controlling for age, gender, education, income, insurance status, years in the United States, health care utilization, and level of English proficiency, awareness of law was not associated with interpreter utilization (odds ratio [OR] 0.66; 95% confidence interval [CI] 0.38, 1.17; P = 0.16), but was associated with having a language-concordant provider (OR 1.64; 95% CI 1.19, 2.26; P = 0.003).
CONCLUSION
Awareness of language law is not sufficient to resolve language barriers for LEP individuals. Provider and organization level barriers to language access must be addressed.
Keywords: limited English proficient, interpreter, health policy, language barrier
Several studies suggest that language barriers in the health care setting decrease access to primary and preventive care,1–10 impede patient comprehension,11,12 decrease patient adherence,13,14 and reduce patient satisfaction.15–19 As such, language barriers impose a significant and increasing threat to quality care for limited English proficient (LEP) individuals. According to the 2000 Census, more than 21 million Americans (8%) speak English less than “very well”—a 30% increase since the 1990 Census. In California, home to a third of the nation's LEP population, 1 in 5 people speak English less than “very well.”20
Although several studies have found that use of providers who can communicate directly with LEP patients in the patient's primary language (language-concordant) is associated with improved patient comprehension,11,12 self-reported health status,21 interpersonal processes of care,22 and patient recall,23 the limited bilingual provider supply falls short of LEP demand. Therefore, health care institutions have needed to rely on interpreters. While the use of untrained or ad hoc interpreters like family, friends, and bilingual administrative and custodial staff is common,24,25 several studies have shown that, as compared with trained medical interpreters, this practice leads to increased miscommunication and errors, often with clinically significant consequences.26–30 Given that trained medical interpreters have specialized training in medical terminology, interpretation accuracy, and confidentiality, advocates for LEP individuals have argued for the routine use of trained medical interpreters and have found support for this position in federal statute.
The legal basis for a patient's right to language access was established with Title VI of the 1964 Civil Rights Act, which states:
No person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving federal financial assistance.
Because the courts have interpreted “national origin” to include persons with limited English proficiency, recipients of federal funding may be found liable for discrimination for failing to provide access to language services.31
The right to language access was reinforced in 2000 by President Clinton's Executive Order 13,166, which required all federal agencies to review their own policies and procedures to ensure appropriate access for LEP persons. In response to the Executive Order, the U.S. Department of Health and Human Services' Office for Civil Rights (OCR) released guidelines for health care providers receiving federal funding (e.g., providers who accept Medicare or Medicaid patients) on how to ensure language access, including provision of competent (i.e., trained) interpreters at no cost to LEP patients who cannot communicate with their providers.32 The guidelines, however, afforded considerable flexibility to providers on how to meet the requirement and provided no additional resources, thus limiting the potential for effectively addressing the problem of language barriers in health care settings.
To increase the effectiveness of this policy, advocacy groups have focused considerable efforts on public campaigns designed to increase consumer awareness of the right to language access afforded by federal statute. New California Media's statewide “Does Anyone Here Speak My Language?” campaign using ethnic media outlets is a prominent example of an educational campaign to inform LEP individuals of their language rights in the health care setting. This strategy of empowering individuals is based upon a bottom-up model of change that recognizes individual capacity for self-representation, health decision making, and health care participation, and has been used with success by advocates for the deaf community after passage of the Americans with Disabilities Act.33 In this model, increased individual awareness of the legal right to communicate with providers empowers individuals to request or insist on these legally mandated services. This cumulative individual pressure on health care institutions, reinforced by the OCR, ideally results in improved availability of language assistance services. In fact, this approach has created significant gains across a variety of health care settings.34 For example, 1 of Northern California's most comprehensive Interpreter Services was borne out of an OCR complaint against Oakland's Highland Hospital in 1980. However, no study to date has examined whether or not efforts to increase LEP individuals' awareness of language laws translate into improved language access for LEP individuals at the health care encounter. The goal of our study was to determine the extent of LEP individual awareness of language law and to investigate the impact of this awareness on language access as measured by interpreter utilization among a multilingual sample of LEP individuals in California. We hypothesized that individuals with awareness of language law would be more likely to report interpreter utilization in the health care setting.
METHODS
A statewide telephone survey was conducted in 11 non-English languages by Bendixen & Associates on behalf of New California Media in June 2003. The survey, part of an initiative to raise awareness of language barriers in health care settings, was designed to assess ethnic Californians' awareness, attitudes, and experiences with the health care setting.35
Participant telephone numbers were chosen by a probability sampling method that used information from the U.S. Census on the geographic distribution of ethnic groups to intentionally and efficiently oversample smaller ethnic groups. Participants were included in the survey if they were at least 18 years of age, self-identified as a member of 1 of the survey's targeted ethnic groups, and indicated a preference for being interviewed in a survey language. A target sample of 1,200 was chosen to allow for a 3% sampling error in poll results. Sampling was concluded when 1,200 consecutive participants who met inclusion criterion had been interviewed in the following languages: 100 in Armenian, 100 in Cambodian, 100 in Cantonese/Mandarin, 100 in Farsi, 100 in Mien, 100 in Korean, 100 in Russian, 100 in Tagalog, 100 in Vietnamese, and 300 in Spanish. Survey languages represent those served by New California Media and most commonly spoken in California. Interviews were conducted with 74% of those contacted who met inclusion criteria. No further information was collected on those who declined to participate.
A member of the study team (AC), the executive director of New California Media, and Bendixen & Associates developed the survey questions through expert opinion and previous survey review. Survey questions were translated using a 2-step process whereby after initial translation, a second, independent translator reviewed the questions to ensure completeness, accuracy, and cultural appropriateness. The telephone survey was pretested by using an identified sample who met study inclusion criteria. For each of the 11 languages, 10 pretest interviews were conducted.
The final survey contained 48 questions addressing issues of health care access, satisfaction, understanding, and knowledge. The survey assessed English proficiency using the U.S. Census question “How well do you speak English?” scored on a 4-point scale. The U.S. Census Bureau defines individuals as LEP if they respond “well,” “not well,” or “not at all” to this question, while those who respond “very well” are considered English proficient. We chose to apply the Census Bureau definition of LEP to our study, reasoning that a high level of fluency is required for health care settings given the risks for miscommunication even when language is not an issue.36 Only LEP participants were included in the analysis.
We considered participants to be aware of the language law if they answered “yes” to the question “Did you know the law in the United States gives you the right to a [participant language] interpreter when you visit a clinic or hospital?” Those who answered “no” were considered not aware of the language law. Those who answered “don't know” were not included in the final analysis.
While participants were not asked how many different providers they saw or the number of times they interacted with the health care system, they were asked, “Is there a particular doctor's office, clinic, or health care center that you usually go to if you are sick or need advice about your health?” to assess an individual's usual communication experience with her/his primary provider. In an effort to control for health care utilization in our analyses, we considered participants to have a usual source of care if they answered “yes” to this question under the assumption that those with a usual source of care would be more likely than those without to use language services. For those who responded “no,” the primary reason for not having a usual source of care was elicited. Only those participants who reported having a usual source of care were questioned about provider language concordance.
Language access was defined as either having a language-concordant provider or utilizing an interpreter in the health care setting. We considered participants who responded “yes” to the question “Does your doctor speak [respondent language]?” to have a language-concordant provider. Only those who reported not having a language-concordant provider were asked, “Who helps you communicate with your doctor—a professional interpreter, a staff person at your doctor's office, a family member, a friend, or do you do the best that you can in English?” The survey design allowed multiple responses. Although the use of untrained bilingual clinical or clerical staff as ad hoc interpreters may compromise health care quality, we considered participants to have utilized an interpreter if their response included “professional interpreter” (i.e., trained, with primary job role as medical interpreter) or “staff member” as it is often difficult for lay persons to distinguish between the 2. Those whose responses only included “family/friend” or “do the best I can in English” were considered to not have utilized an interpreter.
“Don't know/not applicable” and missing responses to study variables accounted for less than 4% of total responses and were excluded from the analysis. Approximately 25% declined to report income. This missing response was maintained as an income category.
Data for age, income, years in the United States, and insurance were collected within detailed strata. We collapsed strata into categories after verifying no differences in association with outcome variables between contiguous strata.
We hypothesized that awareness of language law would be associated with improved language access through increased interpreter utilization. To test our hypothesis, we used multivariate logistic modeling to estimate the independent effect of awareness on interpreter utilization after controlling for age, gender, education, insurance, income, years in the United States, and level of English proficiency. Because having a language-concordant provider also constitutes language access and participants with a language-concordant provider were not asked about interpreter utilization, we conducted a separate analysis to assess the independent association of awareness of language law with having a language-concordant provider. We also conducted an analysis to assess the association of awareness of language law with language access overall (interpreter or language-concordant provider). To assess the potential bias introduced by excluding “don't know” responses to the question “Who helps you communicate with your doctor?” we repeated the analyses, recoding “don't know” responses as utilizing an interpreter. To assess the potential bias introduced by lack of health care utilization, we repeated the analyses excluding those participants who reported having no usual source for health care. Finally, we checked for differences in the effect of awareness of language law across demographic and socioeconomic subgroups.
RESULTS
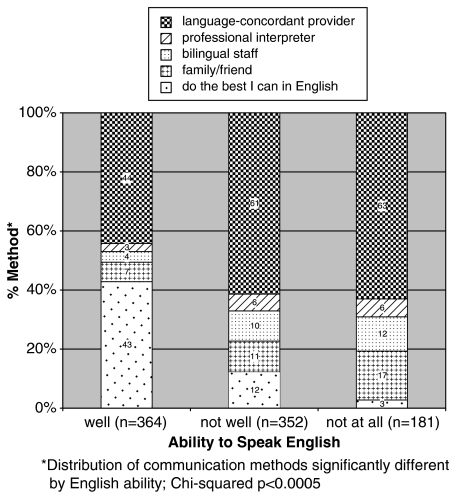
Of the 1,200 survey participants, 1,000 (83%) were LEP. As compared with their non-LEP counterparts, LEP participants tended to be less educated (54% vs 84% with high school equivalent), more recent immigrants (33% vs 13% in the United States less than 10 years), and more likely to be uninsured (23% vs 12%). Limited English proficient patients used various methods through which to communicate with their providers. Figure 1 illustrates the percentage of participants at each level of English proficiency who used each communication method. Of note, among those rating their ability to speak English as “not well” or “not at all,” 12% and 3%, respectively, relied upon their own English skills when communicating with their health care provider. Overall, 60% of the LEP patients in our study reported utilizing either an interpreter (professional interpreter or bilingual staff) or a language-concordant provider.
FIGURE 1.
Method of communication by ability to speak English. (Because of rounding, totals may not equal 100%. Only those asked about communicating with provider included, n = 897).
Three hundred and seventy-one (37%) LEP participants were aware of the language law. The demographic and socioeconomic characteristics of LEP participants by awareness of language law are shown in Table 1. Limited English proficient participants who were aware of the language law were significantly more likely to be over the age of 65 (17% vs 11%, P = 0.01) and marginally more likely to be publicly insured (38% vs 32%, P = 0.06) than those who were not aware of the language law.
Table 1.
| LEP Participant Characteristics (n = 1,000) | Percentage of Participants Aware of Language Law (n = 371) (37%) | Percentage of Participants Not Aware of Language Law (n = 598) (60%) | P Value |
|---|---|---|---|
| Age (%≤65 y) | 83 | 89 | .01 |
| Female (%) | 60 | 60 | 1.00 |
| English proficiency (%) | .42 | ||
| Well | 39 | 42 | |
| Not well | 41 | 37 | |
| Not at all | 20 | 20 | |
| High school education or equivalent (%) | 53 | 54 | .69 |
| Income (%) | |||
| < $25,000 | 29 | 35 | .14 |
| ≥$25,000 | 45 | 43 | |
| Refused | 26 | 22 | |
| Insurance (%) | .06 | ||
| No insurance | 20 | 25 | |
| Public | 38 | 32 | |
| Private | 42 | 43 | |
| Years in United States (% < 10 y) | 32 | 34 | .69 |
| Usual source of care (%) | 83 | 83 | .93 |
Missing data and “don't know” responses are not included in the table (or in analysis).
Because of rounding, total may not equal 100%.
English proficiency includes LEP only (English less than “very well”).
LEP, limited English proficient.
After adjusting for age, gender, education, income, insurance, years in the United States, and level of English proficiency, we found no association between awareness of language law and interpreter utilization (adjusted odds ratio [OR] 0.66; 95% confidence interval [CI] 0.38, 1.17; P = 0.16). However, awareness of language law was significantly associated with having a language-concordant provider (adjusted OR 1.64; 95% CI 1.19, 2.26; P = 0.003). There was no association between awareness of language law and language access overall (interpreter utilization or having a language-concordant provider) (adjusted OR 1.17; 95% CI 0.88, 1.57; P = 0.28). When we repeated the analysis using a more conservative definition of LEP to include only those who self-rated their English ability as “not well” and “not at all” only, awareness of language law remained unassociated with interpreter utilization and weakened its association having a language-concordant provider (adjusted OR 1.56; 95% CI 1.00, 2.42; P = 0.05).
When we repeated the analyses recoding “don't know” responses as utilizing an interpreter, we observed no significant change in the results. To estimate the impact of health care utilization on our results, we also repeated the analysis excluding those without a usual source for health care. There was no significant change in the results. Of note, those who reported that they spoke English not well or not at all as compared with those who said they spoke English well were more likely to have language access (overall adjusted OR 2.91 and 3.30, respectively; P < 0.0005). We found no differences in the effect of awareness of language law across demographic and socioeconomic subgroups.
DISCUSSION
Previous research has focused primarily on documenting the existence of and adverse effects of language barriers on health care. Few studies have solicited LEP individual knowledge or perspectives on the issue, and none across so many languages. To our knowledge, this is the first multilingual study to focus on the extent of individual awareness of language law and its association with language access. We found that only 38% of our survey participants reported awareness of the language law affording LEP individuals the right to an interpreter in the health care setting.
We expected that LEP individuals who were aware of the language law and did not have a provider who spoke their language would be more empowered to self-advocate for language services and therefore more likely to report interpreter utilization than their counterparts who were not aware of the language law. We found that awareness of language law was not associated with interpreter utilization, but was associated with having a language-concordant provider. These findings persisted after adjusting for demographic and socioeconomic characteristics and having a usual source of care.
Our unexpected findings suggest several possible explanations. Health care organizations and providers may not be aware of their legal obligation to provide language access services for LEP individuals. Alternatively, individual requests for professional interpreters may not be effective at overcoming provider and organizational-level barriers until the collective impact of such requests reaches some threshold or triggers an OCR complaint. For example, organizations may not respond to requests for trained interpreters if they perceive LEP individuals to constitute too small a market share to merit hiring new staff. On a provider level, clinicians may harbor strong feelings about LEP individuals' obligation to bring their own interpreters, or may not be aware that untrained interpreters such as family and friends frequently make significant errors and omissions in interpreting and therefore consider using untrained interpreters appropriate language access. For LEP individuals who want to realize their language rights, such barriers may leave finding a provider who speaks their language the only option at hand.
Our study had several limitations. First, cross-sectional, self-reported data are subject to the inherent limitations of recall and comprehension. Second, the survey does not elicit how many times individual participants encountered the health care system. It is likely that the more health care interactions a given individual has, the more likely s/he will encounter an interpreter at least once. Instead, the survey attempted to elicit the individual's usual communication experience with his or her provider. Further, when we excluded participants without a usual source of care, our results did not change.
A third limitation is that because so few participants reported receiving “professional” interpretation (41 of 424 responses), we expanded our definition of interpreter utilization to include bilingual staff. This analytic approach likely led us to overestimate the extent of language access for the participants as measured by interpreter use. However, this only reinforces our findings that awareness of language law in this cohort was not predictive of increased access to trained interpreters.
Fourth, the survey was not able to provide an objective metric of participants' English proficiency, instead relying on self-reported proficiency. However, we are not aware of any currently available validated assessment tool to gauge English proficiency (akin to the TOFHL for health literacy). We chose to use the standard and widely accepted U.S. Census Bureau definition of “LEP.” Further supporting our choice was the survey design, which used non-English language preference as an inclusion criteria for participation, suggesting a lower comfort level for communicating in English, even among those who reported speaking English “well” or “very well.” Nevertheless, when we repeated the analysis excluding those who self-rated their English ability as “very well” and “well,” awareness of language law remained unassociated with interpreter utilization and weakened its association with having a language-concordant provider, suggesting that the most LEP individuals are least able to overcome language barriers.
Fifth, the clustered sampling method may have resulted in participants with higher levels of awareness of language law and access to language-concordant providers than may exist in more geographically dispersed LEP communities. As such, our findings may overestimate language access and be less generalizable to more isolated LEP individuals.
A final limitation particular to this California study of language access is the existence of state laws (California Dymally-Alatorre Bilingual Services Act and the Kopp Act), which require language access services only if at least 5% of people served speak a specific language.37,38 We were unable to contextualize the impact of this threshold, as we had no measure of community language prevalence with which to match with individual respondent language. However, when we examined awareness of language law among LEP participants who spoke Spanish, the second most common language spoken in both California and the United States, there remained no association between awareness of language law and interpreter utilization or having a language-concordant provider.
Despite these limitations, our findings highlight several disconcerting realities. While federal policy has mandated that health care providers receiving federal funding provide meaningful language access to LEP patients for over 4 decades, 2 of every 5 LEP participants in our study reported having no language access in the health care setting irrespective of their awareness of language law. This finding illustrates how policy lacking rigorous guidelines, enforcement, and resources often fails to adequately address the problems prompting their creation, and emphasizes the need for effective advocacy for LEP individuals. Further, while it is reassuring that individuals with minimal English ability who arguably may have the most difficult time accessing and navigating the U.S. health care system are most likely to utilize an interpreter, it is of concern that 12% of patients who self-rate their ability to speak English as “not well”—and 3% of patients who report speaking English “not at all”—are communicating with their providers by “doing the best they can in English.” This suggests that those who speak just enough English to “get by” are at greatest risk for negative outcomes associated with miscommunication.
In summary, our findings illustrate that there is much room for raising awareness in LEP populations of their right to appropriate language access. However, even when individuals are aware of this right, it is often unrealized in the health care setting. While consumer engagement and education are important general principles that providers and advocates should continue to support, system and provider-level barriers to language access appear to override patient ability to self-advocate, particularly when policy mandates lack resources and enforcement. Although we do need stronger and more consistent efforts to increase the number of bilingual health care providers, our findings illustrate that we cannot depend upon bilingual providers to ensure language access in every setting or for every language. Further research is needed to define what factors and/or incentives influence providers and health care institutions to offer language services. Given that financial resources often limit interpreter services, research is also needed to investigate the feasibility and cost-effectiveness of sharing existing resources across multiple centers through recent technologic advances such as remote simultaneous interpretation and videoconferencing medical interpretation to improve access to trained interpreters. Finally, health care institutions should go beyond counting interpreter positions and logging interpreter requests to more accurate assessments of how well their efforts are meeting the needs of the LEP individuals they serve.
Acknowledgments
Funding: New California Media's project “Bridging Language Barriers in Health Care” was funded by The California Endowment. This study was funded in part by a Physician Faculty Development in Primary Care Grant (#D55 HP 05165-01-00) from Department of Health and Human Services. Dr. Fernandez's efforts were supported by an NIH Career Development Award (K23 832401).
Bendixen & Associates: a survey and communications consulting group that focuses on the characteristics of the Latino population and market in the United States and Latin America.
New California Media: a statewide multi-ethnic media association run by the nonprofit Pacific News Service.
REFERENCES
- 1.Facione NC. Breast cancer screening in relation to access to health services. Oncol Nurs Forum. 1999;26:689–96. [PubMed] [Google Scholar]
- 2.Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: findings from a national sample. Med Care. 2002;40:52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152:1119–25. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 4.Harlan LC, Bernstein AB, Kessler LG. Cervical cancer screening: who is not screened and why? Am J Public Health. 1991;81:885–91. doi: 10.2105/ajph.81.7.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu DJ, Covell RM. Health care usage by hispanic outpatients as function of primary language. West J Med. 1986;144:490–3. [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkman-Liff B, Mondragon D. Language of interview: relevance for research of southwest Hispanics. Am J Public Health. 1991;81:1399–404. doi: 10.2105/ajph.81.11.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pitkin Derose K, Baker DW. Limited English proficiency and Latino's use of physician services. Med Care Res Rev. 2000;57:76–91. doi: 10.1177/107755870005700105. [DOI] [PubMed] [Google Scholar]
- 8.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80:11–9. doi: 10.2105/ajph.80.suppl.11. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinick RM, Krauss NA. Racial/ethnic differences in children's access to care. Am J Public Health. 2000;90:1771–4. doi: 10.2105/ajph.90.11.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doty MM. Hispanic Patients' Double Burden: Lack of Health Insurance and Limited English. New York, NY: The Commonwealth Fund; 2003. [Google Scholar]
- 11.Crane JA. Patient comprehension of doctor-patient communication on discharge from the emergency department. J Emerg Med. 1997;15:1–7. doi: 10.1016/s0736-4679(96)00261-2. [DOI] [PubMed] [Google Scholar]
- 12.Lasater LM, Davidson AJ, Steiner JF, Mehler PS. Glycemic control in English- vs Spanish-speaking Hispanic patients with type 2 diabetes mellitus. Arch Intern Med. 2001;161:77–82. doi: 10.1001/archinte.161.1.77. [DOI] [PubMed] [Google Scholar]
- 13.Ghandi TK, Burstin HR, Cook EF, et al. Drug complications in outpatients. J Gen Intern Med. 2000;15:149–54. doi: 10.1046/j.1525-1497.2000.04199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaw J, Hemming MP, Hobson JD, Nieman P, Naismith NW. Comprehension of therapy by non-English speaking hospital patients. Med J Aust. 1977;2:423–7. doi: 10.5694/j.1326-5377.1977.tb114593.x. [DOI] [PubMed] [Google Scholar]
- 15.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for spanish-speaking patients. Med Care. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–7. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 17.David RA, Rhee M. The impact of language as a barrier to effective health care in an underserved urban hispanic community. Mt Sinai J Med. 1998;65:393–7. [PubMed] [Google Scholar]
- 18.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14:409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weech-Maldonado R, Morales LS, Elliott M, Spritzer K, Marshall G, Hays RD. Race/ethnicity, language, and patients' assessments of care in medicaid managed care. Health Serv Res. Jun 2003;38:789–808. doi: 10.1111/1475-6773.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Census Bureau. QT-02, Profile of Selected Social Characteristics. 2000 [Google Scholar]
- 21.Perez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–9. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. J Gen Intern Med. 2004;19:167–74. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seijo R, Gomez J, Freidenberg J. Language as a communication barrier in medical care for hispanic patients. Hispanic J Behav Sci. 1991;13:363–75. [Google Scholar]
- 24.Hornberger J, Itakura H, Wilson SR. Bridging language and cultural barriers between physicians and patients. Public Health Rep. 1997;112:410–17. [PMC free article] [PubMed] [Google Scholar]
- 25.Ginsberg C, Martin V, Andrulis D, Shaw-Taylor Y, McGregor C. Interpretation and Translation Services in Health Care: A Survey of US Public and Private Teaching Hospitals. Washington, DC: National Public Health and Hospital Institute; 1995. pp. 1–49. [Google Scholar]
- 26.Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111:6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 27.Elderkin-Thompson V, Silver RC, Waitzkin H. When nurses double as interpreters: a study of Spanish-speaking patients in a U.S. primary care setting. Soc Sci Med. 2001;52:1343–58. doi: 10.1016/s0277-9536(00)00234-3. [DOI] [PubMed] [Google Scholar]
- 28.Launer J. Taking medical histories through interpreters: practice in a Nigerian outpatient department. Br Med J. 1978;2:934–5. doi: 10.1136/bmj.2.6142.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marcos LR. Effects of interpreters on the evaluation of psychopathology in non-english-speaking patients. Am J Psychiatry. 1979;136:171–4. doi: 10.1176/ajp.136.2.171. [DOI] [PubMed] [Google Scholar]
- 30.Rivadeneyra R, Elderkin-Thompson V, Silver RC, Waitzkin H. Patient centeredness in medical encounters requiring an interpreter. Am J Med. 2000;108:470–4. doi: 10.1016/s0002-9343(99)00445-3. [DOI] [PubMed] [Google Scholar]
- 31.San Francisco, CA: Grantmakers Health; 2003. In the Right Words: Addressing Language and Culture in Providing Health Care. Issue Brief No. 18 August. [PubMed] [Google Scholar]
- 32.San Francisco, CA: Grantmakers Health; In the Right Words; p. 10. [Google Scholar]
- 33.Munoz-Baell IM, Ruiz MT. Empowering the deaf. Let the deaf be deaf. J Epidemiol Commun Health. 2000;54:40–4. doi: 10.1136/jech.54.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perkins J, Youdelman M, Wong D. Ensuring Linguistic Access in Health Care Settings: Legal Rights and Responsibilities. 2. Los Angeles, CA: National Health Law Program; 2004. [Google Scholar]
- 35.New California Media. Bridging Language Barriers in Health Care. [January 10, 2005]; Available at: http://news.ncmonline.com/news/view_article.html?article_id=ac9fc71c53d1afbd8d928601e9c79685.
- 36.Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52:315–23. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 37.California Government Code §7290–7299.8 (Dymally-Alatorre Bilingual Services Act 1973).
- 38.California Health and Safety Code §1259 (Kopp Act 1983).