Abstract
OBJECTIVE
To evaluate whether training primary care clinicians in maintenance care for patients who have changed their drinking influences practice behavior.
DESIGN
We randomized 15 physician and 3 mid-level clinicians in 2 primary care offices in a 2:1 design. The 12 intervention clinicians received a total of 2 ¼ hours of training in the maintenance care of alcohol problems in remission, a booster session, study materials and chart-based prompts at eligible patients' visits. Six controls provided usual care. Screening forms in the waiting rooms identified eligible patients, defined as those who endorsed: 1 or more items on the CAGE questionnaire or that they had an alcohol problem in the past; that they have “made a change in their drinking and are trying to keep it that way”; and that they drank <15 (men) or <10 (women) drinks per week in the past month. Exit interviews with patients evaluated the clinician's actions during the visit.
RESULTS
Of the 164 patients, 62% saw intervention clinicians. Compared with patients of control clinicians, intervention patients were more likely to report that their clinician asked about their alcohol history (odds ratio, 2.8; 95% confidence interval, 1.3, 5.8). Intervention clinicians who asked about the alcohol history were more likely to assess prior and planned alcohol treatment, assist through offers for prescriptions and treatment referral, and receive higher satisfaction ratings for the visit.
CONCLUSIONS
Systemic prompts and training in the maintenance care of alcohol use disorders in remission might increase primary care clinicians' inquiries about the alcohol history as well as appropriate assessment and intervention after an initial inquiry.
Keywords: primary health care, alcohol-related disorders, recurrence/PC
In primary care settings, 20% of adults have a history of an alcohol use disorder, and 70% of such patients have made changes in their drinking.1–3 Although alcohol treatment effectively initiates recovery, approximately half of patients will return to the previous level of alcohol use.4,5 Alcohol use disorders are characterized by remission and relapse. Quality management of these chronic disorders requires both induction of behavioral change and long-term maintenance care—the latter to prevent recurrence of the previous pattern of problematic alcohol use. Ongoing brief contacts with a trained health professional can improve the timeliness of re-referral for needed treatment and reduce consumption and consequences among former problem drinkers.6–8
The primary care clinician, with a comprehensive, person-centered, and longitudinal approach, is well-positioned to provide maintenance care for alcohol disorders.9 In the United States, 80% of adults see a physician at least once per year, and two-thirds of problem drinkers see a physician during early remission.10 As with other chronic diseases, generalist physicians can monitor progress, provide continuity care, and coordinate referrals. Other skills required for relapse prevention, such as building a therapeutic relationship, taking a thorough history, maintaining a nonjudgmental attitude, communicating with empathy and working with families, are also akin to primary care.11 For patients with limited access to specialty care, physician counseling, even if minimal, and recovery group meetings are often the only options.
Unfortunately, primary care physicians are poorly prepared for the longitudinal management of alcohol use disorders. Existing practice guidelines and consensus statements provide recommendations about screening and brief interventions to motivate patients to recognize and address active alcohol problems,12–15 but these approaches provide little guidance about working with patients who have moderated or stopped their drinking.11 Therefore, this project examined whether a maintenance care intervention for primary care clinicians can influence practice behavior among patients with prior alcohol problems. We hypothesized that training in the intervention and clipping training materials to the charts of such patients (i.e., chart cues) would make clinicians more likely to ask about the alcohol history, and assess and assist patients to reduce relapse risks. We also presupposed that clinicians who ask about the alcohol history would be more likely to assess and assist with relapse risks.
METHODS
Development of the PRIMECare Model
A local development group at Brown Medical School included an addiction medicine physician (P. D. F.), a primary care and HIV physician (M. D. S.), an addiction educator (C. D.), and a clinical psychologist (D. H). This group reviewed relevant literature for effective specialty relapse prevention approaches that might be feasible in the primary care setting. The resultant PRIMECare (Promote Recovery in Medical Care) model gives primary care clinicians an approach to assessment and brief intervention for the maintenance care of patients who have moderated or stopped drinking in response to alcohol-related problems. Fashioned after the 5 “A”s for smoking counseling16 (Appendix available Online), the model focuses on individualized risk factors for relapse to heavy drinking using a mnemonic “P.R.E.C.U.R.S.O.R.S.,” and a menu of options (a “toolbox”) to help reduce these risk factors in order to prevent relapse. The major foci of the model are: (1) Identification of persons in recovery (ASK); (2) Assessment of individualized relapse risks (ASSESS); (3) Brief counseling to address relapse risks (including 12-step facilitation and cognitive behavioral approaches (ADVISE); (4) Developing a plan to manage high risk situations/moods, urges, and lapses; and pharmacotherapy to manage affective symptoms and craving (ASSIST); and (5) Setting follow-up (ARRANGE), including regular appointments and monitoring γ-glutamyl transpeptidase.17
The group developed materials to help clinicians with implementation of the PRIMECare model, including: a recovery workbook with take-home exercises to facilitate the development of plans for managing high-risk situations/moods and recovery group involvement18,19; a recovery pocketcard on which patients could record a telephone call list and reminders of their relapse prevention plan; a physician card with an abbreviated version of the model and a menu of ways to address specific relapse risks; a booklet of local recovery resources; a chart note with cues for the model; and detailing items (PRIMECare pens, post-it notes, and coffee mugs).
Usual Care and Intervention Clinicians
The study occurred in 2 administratively and clinically separate private offices near an academic medical center in Providence, RI. Only 1 physician refused to participate. We randomized the 15 general internal medicine physicians, 2 nurse practitioners, and 1 physician assistant (18 total) in a 2:1 design. Both sites included both intervention and control providers. The 12 intervention clinicians received:
An initial 2 ¼hours of training in the PRIMECare model;
An academic detailing luncheon 6 weeks later;
A 45-minute booster training session 6 months later; and
PRIMECare materials clipped to the charts of eligible patients at the index patient visit.
The initial training consisted of 3 45-minute lunch sessions that used lecture, video demonstration, and case-based role-play to rehearse new skills.20 The 3 training sessions occurred in consecutive weeks over a 1-month period in April 2001. Because of limited time, the training focused on 3 aspects: (1) assessment of relapse risks (ASSESS); (2) brief counseling regarding relapse risks (ADVISE) and (3) developing a plan to manage high risk situations/moods, urges, and lapses, including pharmacotherapy (ASSIST). A detailing luncheon in June 2001 provided individualized educational outreach (P. D. F.).21,22 A 45-minute booster session in December 2001 included a review of the model, a case-based exercise in assessing relapse risks, feedback, and questions. The 6 clinicians assigned to the control group received lunch only, and provided standard care without chart prompts.
Patient Recruitment
The Institutional Review Board at Rhode Island Hospital approved the evaluation. A self-administered questionnaire screened patients in the offices' waiting areas. Like other studies,15 this questionnaire included general health screening questions along with items to identify problem-drinking patients in remission. Eligible patients endorsed 1 or more affirmative responses to the CAGE questionnaire23,24 or that they had an alcohol problem; AND a maintenance item from the Readiness to Change Questionnaire: “I have made a change in my drinking and I am trying to keep it that way.”25 The protocol excluded current heavy drinkers, defined as 15 or more drinks per week on average in the past month for men14 or 10 or more drinks per week for women.26
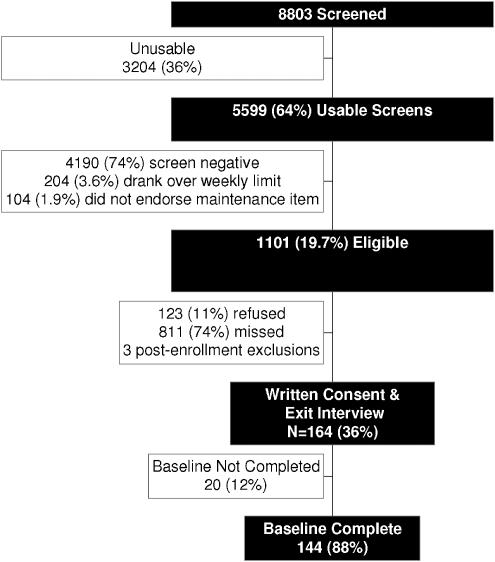
Research assistants approached 8,803 adults at the 2 offices on random days between May 2001 and April 2003 (Fig. 1). Of the 5,599 (64%) usable screens, 1,101 (19.7%) were eligible: 123 (11%) refused participation and 811 (74%) were missed for lack of research staff or an inability to obtain consent before the clinical visit. The remaining 167 individuals gave informed consent. Two subjects withdrew immediately and 1 patient was deemed ineligible following enrollment. This article reports on the 164 patients who completed the exit interview.
FIGURE 1.
Recruitment flowchart.
Based on the screener, eligible, nonenrolled individuals were older than the enrolled group (mean age between 41 and 50 years vs mean age between 31 and 40 years, P<.05). The nonenrolled group also included more women (60.6% vs 44.4%, P<.0001) than the enrolled group. These groups did not differ in education, drinking days per week, mean drinks per drinking day, or number of heavy drinking episodes in the prior month.
Exit Interviews
Research assistants administered exit interviews after the visit to all consenting patients to evaluate clinicians' adherence to the model. Exit interviews are a reliable and valid method to measure the implementation of practice-based behavioral interventions.27,28 Within the first week after the index visit, 144 of 164 subjects also completed a baseline interview that assessed alcohol abuse and dependence.
Measures
Demographics
Demographic measures on the screener included single items assessing age, gender, race (Caucasian vs non-Caucasian), education (high school education or less vs any post high school education) and patients' rating of their own general health status from 1=poor to 5=excellent.
Patient Satisfaction
Three items assessed patients' level of satisfaction with the clinician's thoroughness, carefulness, and competence; personal manner; and overall satisfaction. A composite score was created from the mean of these 3 items (coefficient α=0.87).
CAGE Score
The CAGE Score was included as a marker of the likelihood of alcohol dependence.29 Scores ranged from 0 to 4 with a mean of 2.04 (SD, 1.07).
Clinician Adherence
The exit interview included a single item that asked participants if the clinician inquired about their alcohol history. Sixteen ASSESS items, with response options ranging from 1—“We have never discussed it” to 4—“We did discuss it today,” measured assessment of relapse risks (e.g., “At today's visit did you and your medical provider discuss … whether you have family and friends who support the changes you have made in your drinking?”). Sixteen ASSIST items measured the extent to which the clinician offered interventions or referral to support abstinence (e.g., “At this visit did your medical provider offer … suggestions about ways to improve your coping with risky or difficult situations or moods”), with responses ranging from 1—“He/She never offered it” to 4—“He/She did offer it today.”
Principal component analysis (PCA) indicated that 12 of the ASSESS items loaded on 1 of 3 components: relapse risk factors (7 items, e.g., family stress, mood, urges and cravings; coefficient α=0.84), prior treatment and treatment intention (3 items: attended prior detox or treatment for drinking, completed prior treatment program, and any plan for future treatment; coefficient α=0.86), and general health (2 items: physical pain or discomfort, daily activities; coefficient α=0.44). These 3 components explained 57% of the variance in the ASSESS items.
Eleven of the ASSIST items loaded on 1 of 3 components describing offers for prescriptions and treatment referrals (5 items, e.g., prescription for disulfiram, prescription to relieve depression, referrals to alcohol specific treatment program or mental health professionals; coefficient α=0.73); provision of study materials (4 items: log to record craving and coping, log to record AA meetings, recovery workbook and pocket card; coefficient α=0.84); and information about smoking cessation (2 items: suggestions for ways to stop smoking, prescription to aid smoking cessation; coefficient α=0.82). These 3 components explained 56% of the variance in the ASSIST items.
Patients were also asked how many minutes they spent with their clinician during the visit and whether or not the clinician was aware of their alcohol history before the visit.
Clinician Confidence
Before randomization all clinicians completed surveys rating their confidence and experience with alcohol-using patients on 10-point scales. For example, confidence in assessing and counseling patients in remission or recovery from alcohol abuse or dependence was anchored from 1=definitely not confident to 10=definitely confident. Similar questionnaires were administered to all clinicians 1 month after the training. Intervention clinicians rated the helpfulness of the training on a similar 10-point scale.
Statistical Methods
Most of the adherence outcome variables were continuous and modeled using linear regression estimation methods. The exception was a dichotomous inquiry about the patient's history of alcohol-related issues (ASK), which was modeled using logistic regression. Univariate analyses evaluated the distribution of the outcomes. Four of them (ASSESS—prior and planned treatment, ASSIST—offer prescription or treatment referral, visit satisfaction, and visit time) exhibited nonnormality. These variables normalized after logarithmic transformation.
As a first step in testing the multivariate models, mixed linear models identified the extent to which the outcome variables clustered within clinics and clinicians. The intraclass correlation coefficient (ICC) within clinics was not significant (P>.10), and the ICC within clinician was negligible (ranging from <0.01 to 0.03; P>.10) for most of the clinician adherence outcomes, allowing the predominant use of fixed effect regression models. Exceptions included ASSESS-relapse risk (ICC for clinician, 0.17; P=.049) and ASSIST-provision of study materials (ICC for clinician, 0.12; P=.043) whose mixed linear models required a random effect for clinician. For all analyses, a main effects model first evaluated differences between the groups on the adherence outcomes controlling for age, CAGE score, and visit time. Next, a model tested main effects and interactions of intervention with CAGE score and clinician asking about the alcohol history. Main effects only models were interpreted when no interaction effects were significant.
RESULTS
Clinician Characteristics
All but one of the clinicians was white and half were female (Table 1). All physicians were board-certified in internal medicine. More intervention clinicians reported having attended a lecture or seminar on substance use problems in the past year, although they reported spending only 1 to 2 hours at such seminars. Intervention and control clinicians did not differ in the amount of prior supervised clinical experience they had in treating patients with alcohol problems, in the number of outpatients or practice hours per week, or in their baseline level of confidence in assessing and counseling patients in remission or recovery from alcohol problems. In the month after the training, intervention clinicians reported significantly greater confidence in assessing and counseling alcohol patients in recovery after controlling for baseline confidence. Virtually all intervention clinicians found the intervention to be helpful: on a 1 to 10 rating scale from 1=definitely not helpful to 10=definitely helpful, responses ranged from 6 to 10, with an average rating of 8.03.
Table 1.
Clinician Characteristics
| Intervention (N=12) | Control (N=6) | P Value | |
|---|---|---|---|
| % Female | 58.3 | 33.3 | .620 |
| % Caucasian | 91.7 | 100.0 | .467 |
| % Attended alcohol/substance seminars past year | 66.7 | 16.7 | .046 |
| % With 4 or more weeks of supervised clinical experience treating alcohol problems | 91.7 | 100.0 | .572 |
| Hours of scheduled outpatients per week (SD) | 30.3 (5.28) | 26.2 (8.91) | .236 |
| Number of outpatients seen per week (SD) | 75.5 (13.87) | 67.5 (18.37) | .315 |
| Confidence in assessing and counseling patients in remission/recovery from alcohol abuse/dependence* | |||
| Before training (SD) | 4.88 (1.51) | 4.69 (1.90) | .829 |
| Within 1 month after training (SD) | 7.36 (1.37) | 4.89 (1.59) | .037 |
| Overall helpfulness of the training (SD)† | 8.03 (1.00) | NA | NA |
On a 10-point scale anchored from 1=definitely not confident to 10=definitely confident.
On a 10-point scale anchored from 1=definitely not helpful to 10=definitely helpful.
Patient Characteristics
Patients who saw intervention clinicians tended to be older than those who saw control clinicians, but they did not differ on gender, race, education, alcohol use, CAGE score, or rating of their own general health (Table 2). Patients reported that they spent a median of 15 minutes with the clinician during the visit, 54.6% indicated that the clinician was previously aware of their alcohol abuse history, and 59.5% indicated that the clinician inquired about their alcohol history during the current visit.
Table 2.
Demographic Characteristics and Alcohol Use of Eligible Participants by Physician Seen
| Intervention (N=101) | Control (N=63) | P Value | |
|---|---|---|---|
| Age (SD) | 48 (13.9) | 42 (13.0) | .017 |
| % Female | 40.6 | 53.9 | .096 |
| % Caucasian | 73.3 | 81.0 | .261 |
| % Completed high school | 92.7 | 100.0 | .089 |
| % 1 or more symptom of past year alcohol abuse* | 25.8 | 30.8 | .528 |
| % 1 or more symptom of past year alcohol dependence* | 51.7 | 44.2 | .393 |
| % Complete abstinence past 90 days* | 27.0 | 28.3 | .863 |
| Past month drinking | |||
| Drinking days per week (SD) | 2.03 (2.15) | 1.40 (1.41) | .152 |
| Mean drinks per drinking day (SD) | 1.72 (1.57) | 1.85 (1.72) | .618 |
| Number of heavy drinking episodes (SD) | 0.78 (1.36) | 1.00 (1.55) | .365 |
| CAGE score | 2.07 (1.05) | 1.98 (1.10) | .621 |
| General health perception | 2.63 (0.85) | 2.52 (0.94) | .409 |
| Visit time (min) | 19.5 (12.8) | 20.5 (13.7) | .710 |
| Physician was previously aware of alcohol history | 50.0% | 62.1% | .145 |
| Clinician asked about alcohol history during current visit | 67.7% | 45.8% | .007 |
Assessed in baseline interview (N=144).
Multivariate Results
Intervention's Effect on Clinicians' Practice Behavior
Intervention clinicians were more likely to ask about the patient's history of alcohol issues during the visit (odds ratio [OR], 2.8; 95% confidence interval [CI], 1.3, 5.8), after controlling for age and CAGE score (Table 3). The intervention did not increase assessment of relapse risk, general health, or assistance with smoking cessation (not shown). However, we detected significant interactions of asking about alcohol history with the intervention (Table 3). Intervention clinicians were significantly more likely to discuss prior and planned treatment (ASSESS) and make offers of prescriptions and/or referrals (ASSIST) among patients who were asked their alcohol history at the visit. In addition, patients who were asked their alcohol history by an intervention clinician reported the greatest satisfaction with the visit.
Table 3.
Effect of Intervention and Other Covariates on Adherence to Components of the PRIMECare Model As Assessed from Exit Interviews
| PRIMECare Component, Unstandardized Parameter Estimate (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Predictor Variables | ASK—Alcohol History* | ASSESS—Relapse Risks† | ASSESS—Prior & Planned Treatment†‡ | ASSESS—General Health† | ASSIST—Offer Prescription or Referral†‡ | Visit Satisfaction†‡ |
| Intervention | 1.17 (0.47, 1.88)§ | 0.07 (−0.39, 0.52) | −0.10 (−0.26, 0.06) | −0.22 (−0.54, 0.10) | −0.15 (−0.26, −0.06)§ | −0.03 (−0.07, 0.01) |
| Asked about alcohol history | … | 0.73 (0.47, 1.00)∥ | 0.07 (−0.02, 0.16) | 0.37 (0.05, 0.69)§ | — | 0.03 (0.01, 0.05)§ |
| Asked about alcohol history × intervention | … | — | 0.15 (0.01, 0.29)§ | — | 0.09 (0.01, 0.18)§ | 0.03 (0.00, 0.06)§ |
| CAGE score | — | — | — | — | 0.02 (−0.01, 0.04) | 0.005 (−0.005, 0.01) |
| CAGE score × intervention | — | — | — | — | 0.04 (0.00, 0.08)∥ | 0.02 (0.00, 0.04)§ |
| Age | — | — | — | — | — | 0.01 (0.005, 0.02)§ |
| Model R2 | 0.10 | 0.22 | 0.15 | 0.06 | 0.10 | 0.09 |
| Range of outcome values | Yes/No | 1 to 4 | 0 to 0.60 | 1 to 4 | 0 to 0.60 | 0 to 0.70 |
Multivariate logistic regression model that examined main effects of age, CAGE score, visit time, and intervention. Parameter estimate presented in table (odds ratio presented in text). Only significant variables are shown. Ellipses indicate variables not able to be tested. Nagelkerke R2 for the logistic model is presented.
Multivariate linear regression model that examined main effects of age, CAGE score, visit time, asked about alcohol history, and intervention, as well as interactions of intervention with CAGE score and clinician asked about alcohol history. Only significant variables and components of displayed interaction terms are shown.
Log-transformed outcome variable.
P<.05.
P<.10.
Asking about the patient's alcohol history exerted main effects on adherence outcomes independent of intervention status. Patients whose clinician asked the alcohol history reported that their clinicians also spent more time with them (21 and 17 total minutes for taking vs not taking an alcohol history; unstandardized coefficient=0.11, P<.05; 95% CI=0.03, 0.19; R2=0.06) and were more likely to assess relapse risks and general health issues compared with patients whose clinicians did not take an alcohol history (Table 3). Effect sizes were small, ranging from R2=0.22 for assessment of relapse risk to R2=0.06 for assessment of general health. Visit time was not related to any of the clinician adherence outcomes, nor was age, although older patients reported greater satisfaction with the visit. CAGE score exerted no significant main effects, but it tended to produce 2 interactions with the intervention: patients with higher CAGE scores seen by intervention clinicians tended to report more offers of prescriptions or treatment referrals (P=.10) and patients with higher CAGE scores who saw control clinicians were least satisfied. Intervention clinicians did not appear to spend more time with the patient than control clinicians, nor were they more likely to be more aware of their patients' alcohol histories before the visit.
We examined correlations between the adherence outcomes and the number of days elapsed between the clinician training and the visit. Most correlations were nonsignificant, ranging from r=−0.03 for asking the alcohol history to r=−0.17 for assessment of general health. The amount of time patients reported spending with the clinician decreased as more time elapsed between clinician training and the index visit (r=−0.21, P=.041).
DISCUSSION
Despite belief in a responsibility to help their patients with alcohol problems, primary care physicians are often hesitant to accept responsibility for the management of these disorders.30,31 This pilot study suggests that training and chart-based prompting can increase by nearly 3-fold the likelihood that clinicians will inquire about the alcohol history with patients who have changed their drinking behavior. The magnitude of our findings is similar to that of a primary care study of brief counseling for patients with current hazardous drinking in which providers who received 2.5 hours of training and were prompted to intervene were twice as likely as usual care providers to discuss alcohol use.27 The current study differed from prior studies in its exclusive focus on maintenance care for patients who have already made changes in their alcohol use (who are the majority of patients with alcohol issues in primary care),3,32 and we did not provide the clinicians with specific therapeutic recommendations.
For patients who were asked an alcohol history, the intervention also increased assessment of prior and planned alcohol treatment, and offers of prescriptions and/or referrals. These findings suggest that the intervention improved the appropriate content of alcohol-related discussions when they occurred. The greater satisfaction among patients of intervention clinicians who took an alcohol history bolsters this supposition. Other studies suggest that satisfied patients are more likely to return for follow-up and adhere to therapy.33,34 Patient satisfaction here might be a proxy for the quality of the therapeutic alliance, an important process marker and harbinger of better substance use outcomes.35 The intervention also tended to increase provider assistance through offers of prescriptions and/or referrals among patients with greater CAGE scores. This finding suggests that the intervention increased the appropriate counseling of patients with more severe alcohol histories.10
We cannot discern the independent contribution of training versus prompting. A randomized trial in a primary care setting found that prompting with alcohol screening results and individualized recommendations increased faculty physicians' alcohol-related discussions by 1.5-fold.36 In the current study, the prompt did not include screening results or recommendations. We sought to simulate the situation where a nurse or assistant might prescreen a patient then clip materials to the chart for the clinician. We decided to include such a cue because prompts are effective and educational interventions alone have limited effect on practice behaviors.27,36,37 The clipped materials appear to have piqued providers' interest in the alcohol history, and the limited decay in relation to the time since the training suggests the importance of an ongoing system of prompts. However, chart cues alone would be unlikely to induce medical clinicians to assess appropriately the patient's plans for treatment or to offer prescriptions and referrals. One can speculate that the latter findings represent an effect of the training, though further research is needed to discern these relationships.
Clinicians' confidence in managing problematic alcohol use influences whether they elicit an alcohol history.31,38 Clinicians' increased confidence might explain the findings, though small numbers of clinicians prevented detection of a direct effect. Patients did not report that intervention clinicians spent more time with them, though they did perceive that clinicians who inquired about the alcohol history spent on average 4 more minutes at the index visit. Although uncorroborated patient perceptions of time warrant caution, these findings suggest that training and prompting might not be enough to motivate clinicians to provide the 5 to 15 minutes of most brief counseling interventions without special visits.
This study has further limitations. Studies of unhealthy drinking in primary care commonly lose 45% to 75% of eligible subjects for logistical reasons or refusal.36,39 In the current study only 11% of patients refused participation, but a large proportion of those eligible could not be approached for logistical reasons. The arrangement with these busy private offices prohibited research staff from disrupting patient flow. Patients often completed the screener in the waiting room, but were commonly called for their medical appointment before study enrollment. Eligible persons were also missed while the research assistant was interviewing another subject. Although research staff screened individuals without regard to age or gender, the nonenrollee group was older and had more women than the enrolled group. We can speculate that older patients or women might have been more likely to have come for a sick visit, rather than a routine appointment, and were taken into the office more quickly. Selection bias, e.g., a healthy volunteer effect, might mean that the intervention would work more or less well if implemented for all patients with prior alcohol problems.
Exit interviews with the patients assessed the primary outcomes. Previous studies suggest that patients can provide valid reports of the content of clinical encounters.27,28,40,41 Despite their face validity, the current measures have not been validated against objective indicators or corroborative clinician reports. Resource limitations also prevented blinding of research interviewers to study condition. The study also examines a single visit with a single provider. “Cross-overs” to other clinicians over time limit our ability to detect small changes in practice behaviors. More definitive studies should consider randomization by natural practice groupings to minimize contamination across groups.
Despite these limitations, we conclude that training and prompting primary care clinicians in the maintenance care of patients with prior alcohol problems can modestly increase inquiry about the alcohol history and appropriate actions after elicitation of a suggestive history. These effects might last for a minimum of 18 months after the training. Alcohol dependent patients in primary care settings often have less severe alcohol problems than formal treatment populations.42 Many have remitted in response to medical problems or family concerns without formal treatment, and they commonly continue controlled drinking.32,43–45 Such patients, as well as those with treated alcohol use disorders no longer in treatment aftercare and those with less severe alcohol histories in remission, deserve monitoring, support and follow-up. With proper training, tools and logistical support, primary care clinicians might fulfill this role for alcohol use disorders as they do for other chronic disorders. Future research should determine whether primary care clinicians could effectively deliver maintenance care longitudinally and reduce relapse.
Acknowledgments
Supported by the Robert Wood Johnson Foundation Generalist Physician Faculty Scholar Program (7621-01-00). Dr. Friedmann directs the Program to Integrate Psychosocial and Health Services, a Targeted Research Enhancement Program (TRP 04-179) of the VA Health Services Research & Development Service, at the Providence Veterans Affairs Medical Center (Rhode Island). Dr. Stein is a recipient of a Mid-Career Investigator Award from the National Institute on Drug Abuse. The views expressed in this article are the authors' and not necessarily those of the Robert Wood Johnson Foundation, Department of Veterans Affairs, or National Institute on Drug Abuse.
Supplementary Material
The following supplementary material is available for this article online at www.blackwell-synergy.com
The PRIMECare Model of Maintenance Care for Moderated Alcohol Use
REFERENCES
- 1.Buchsbaum DG, Buchanan RG, Lawton MJ, Elswick RK, Jr, Schnoll SH. A program of screening and prompting improves short-term physician counseling of dependent and nondependent harmful drinkers. Arch Intern Med. 1993;153:1573–7. [PubMed] [Google Scholar]
- 2.Barnes HN, Samet JH. Brief interventions with substance-abusing patients. Med Clin North Am. 1997;81:867–79. doi: 10.1016/s0025-7125(05)70553-8. [DOI] [PubMed] [Google Scholar]
- 3.Samet JH, O'Connor PG. Alcohol abusers in primary care: readiness to change behavior. Am J Med. 1998;105:302–6. doi: 10.1016/s0002-9343(98)00258-7. [DOI] [PubMed] [Google Scholar]
- 4.Pickens RW, Hatsukami DK, Spicer JW, Svikis DS. Relapse by alcohol abusers. Alcohol Clin Exp Res. 1985;9:244–7. doi: 10.1111/j.1530-0277.1985.tb05744.x. [DOI] [PubMed] [Google Scholar]
- 5.Hunt WA, Barnett W, Branch LG. Relapse rates in addiction programs. J Clin Psychiatry. 1971;27:455–6. doi: 10.1002/1097-4679(197110)27:4<455::aid-jclp2270270412>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 6.Weisner C, Delucchi K, Matzger H, Schmidt L. The role of community services and informal support on five-year drinking trajectories of alcohol dependent and problem drinkers. J Stud Alcohol. 2003;64:862–73. doi: 10.15288/jsa.2003.64.862. [DOI] [PubMed] [Google Scholar]
- 7.Stout RL, Rubin A, Zwick W, Zywiak W, Bellino L. Optimizing the cost-effectiveness of alcohol treatment: a rationale for extended case monitoring. Addict Behav. 1999;24:17–35. doi: 10.1016/s0306-4603(98)00029-x. [DOI] [PubMed] [Google Scholar]
- 8.Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug Alcohol Depend. 2005;78:325–38. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kimball HR, Young PR. Statement on the generalist physician from the American Boards of Family Practice and internal medicine. JAMA. 1994;271:315–6. [PubMed] [Google Scholar]
- 10.Weisner C, Matzger H. Missed opportunities in addressing drinking behavior in medical and mental health services. Alcohol Clin Exp Res. 2003;27:1132–41. doi: 10.1097/01.ALC.0000075546.38349.69. [DOI] [PubMed] [Google Scholar]
- 11.Friedmann PD, Saitz R, Samet JH. Management of adults recovering from alcohol or other drug problems: relapse prevention in primary care. JAMA. 1998;279:1227–31. doi: 10.1001/jama.279.15.1227. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2. Alexandria, VA: International Medical Publishing; 1998. [Google Scholar]
- 13.Samet JH, Rollnick S, Barnes H. A brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287–93. doi: 10.1001/archinte.156.20.2287. [DOI] [PubMed] [Google Scholar]
- 14.National Institute on Alcohol Abuse and Alcoholism. The Physician's Guide to Helping Patients with Alcohol Problems. Washington, DC: NIH Publication No. 95-3769. National Institutes of Health; 1995. [Google Scholar]
- 15.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 16.Fiore MC, Bailey WC, Cohen SJ, et al. A clinical practice guideline for treating tobacco use and dependence: a US Public Health Service report. The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. JAMA. 2000;283:3244–54. [PubMed] [Google Scholar]
- 17.Kristenson H, Ohlin H, Hulten-Nosslin MB, Trell E, Hood B. Identification and intervention of heavy drinking in middle-aged men: results and follow-up of 24–60 months of long-term study with randomized controls. Alcohol Clin Exp Res. 1983;7:203–9. doi: 10.1111/j.1530-0277.1983.tb05441.x. [DOI] [PubMed] [Google Scholar]
- 18.Kadden R, Carroll K, Donovan D, et al. Project MATCH monograph series. National Institute on Alcohol Abuse and Alcoholism. Washington, DC: DHHS publication no. (ADM)94-3724[3]. Superintendent of Documents, US Government Printing Office; 1995. Cognitive-Behavioral Coping Skills Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- 19.Nowinski J, Baker S, Carroll K. Project MATCH monograph series. National Institute on Alcohol Abuse and Alcoholism. Washington, DC: DHHS publication no. (ADM)94-3724[1]. Superintendent of Documents, US Government Printing Office; 1995. Twelve Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse or Dependence. [Google Scholar]
- 20.Levinson W, Roter D. Can educational programs change the actual communication skills of practicing primary care physicians? The results of two types of continuing medical education programs. J Gen Intern Med. 1993;8:318–24. doi: 10.1007/BF02600146. [DOI] [PubMed] [Google Scholar]
- 21.Greco PJ, Eisenberg JM. Changing physicians' practices. N Engl J Med. 1993;329:1271–3. doi: 10.1056/NEJM199310213291714. [DOI] [PubMed] [Google Scholar]
- 22.Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263:549–56. [PubMed] [Google Scholar]
- 23.Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 24.Mayfield D, McLeod G, Hall P. The CAGE questionnaire. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 25.Heather N, Luce A, Peck D, Dunbar B, James I. Development of a treatment version of the readiness to change questionnaire. Addict Res. 1999;7:63–83. [Google Scholar]
- 26.Sanchez-Craig M, Wilkinson DA, Davila R. Empirically based guidelines for moderate drinking: 1-year results from three studies with problem drinkers. Am J Public Health. 1995;85:823–8. doi: 10.2105/ajph.85.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adams A, Ockene JK, Wheeler EV, Hurley TG. Alcohol counseling: physicians will do it. J Gen Intern Med. 1998;13:692–8. doi: 10.1046/j.1525-1497.1998.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pbert L, Adams A, Quirk M, Hebert JR, Ockene JK, Luippold RS. The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol. 1999;18:183–8. doi: 10.1037//0278-6133.18.2.183. [DOI] [PubMed] [Google Scholar]
- 29.Buchsbaum DG, Buchanan RG, Centor RM, Schnoll SH, Lawton MJ. Screening for alcohol abuse using CAGE scores and likelihood ratios. Ann Intern Med. 1991;115:774–7. doi: 10.7326/0003-4819-115-10-774. [DOI] [PubMed] [Google Scholar]
- 30.Bradley KA, Curry SJ, Koepsell TD, Larson EB. Primary and secondary prevention of alcohol problems: U.S. internist attitudes and practice. J Gen Intern Med. 1995;10:67–72. doi: 10.1007/BF02600228. [DOI] [PubMed] [Google Scholar]
- 31.Friedmann PD, McCullough D, Chin MH, Saitz R. Screening and intervention for alcohol problems. A national survey of primary care physicians and psychiatrists. J Gen Intern Med. 2000;15:84–91. doi: 10.1046/j.1525-1497.2000.03379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown RL, Saunders LA, Bobula JA, Lauster MH. Remission of alcohol disorders in primary care patients. Does diagnosis matter? J Fam Pract. 2000;49:522–8. [PubMed] [Google Scholar]
- 33.Carlson MJ, Gabriel RM. Patient satisfaction, use of services, and one-year outcomes in publicly funded substance abuse treatment. Psychiatr Serv. 2001;52:1230–6. doi: 10.1176/appi.ps.52.9.1230. [DOI] [PubMed] [Google Scholar]
- 34.Druss BG, Rosenheck RA, Stolar M. Patient satisfaction and administrative measures as indicators of the quality of mental health care. Psychiatr Serv. 1999;50:1053–8. doi: 10.1176/ps.50.8.1053. [DOI] [PubMed] [Google Scholar]
- 35.Simpson DD. A conceptual framework for drug treatment process and outcomes. J Subst Abuse Treat. 2004;27:99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 36.Saitz R, Horton NJ, Sullivan LM, Moskowitz MA, Samet JH. Addressing alcohol problems in primary care: a cluster randomized, controlled trial of a systems intervention. The screening and intervention in primary care (SIP) study. Ann Intern Med. 2003;138:372–82. doi: 10.7326/0003-4819-138-5-200303040-00006. [DOI] [PubMed] [Google Scholar]
- 37.Davis DA, Thomson MA, Oxman AD, Haynes RB. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992;268:1111–7. [PubMed] [Google Scholar]
- 38.Saitz R, Friedmann PD, Sullivan LM, et al. Professional satisfaction experienced when caring for substance-abusing patients: faculty and resident physician perspectives. J Gen Intern Med. 2002;17:373–6. doi: 10.1046/j.1525-1497.2002.10520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. J Stud Alcohol. 2001;62:605–14. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- 40.Killeen TK, Brady KT, Gold PB, Tyson C, Simpson KN. Comparison of self-report versus agency records of service utilization in a community sample of individuals with alcohol use disorders. Drug Alcohol Depend. 2004;73:141–7. doi: 10.1016/j.drugalcdep.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 41.Brown JB, Adams ME. Patients as reliable reporters of medical care process. Recall of ambulatory encounter events. Med Care. 1992;30:400–11. doi: 10.1097/00005650-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Johnson JG, Spitzer RL, Williams JB, et al. Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: findings of the PRIME MD-1000 study. J Consult Clin Psychol. 1995;63:133–40. doi: 10.1037//0022-006x.63.1.133. [DOI] [PubMed] [Google Scholar]
- 43.Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cunningham JA, Breslin FC. Only one in three people with alcohol abuse or dependence ever seek treatment. Addict Behav. 2004;29:221–3. doi: 10.1016/s0306-4603(03)00077-7. [DOI] [PubMed] [Google Scholar]
- 45.Cunningham JA, Lin E, Ross HE, Walsh GW. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25:317–21. doi: 10.1016/s0306-4603(98)00130-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The PRIMECare Model of Maintenance Care for Moderated Alcohol Use