Abstract
PECAM-1 (CD31) knockout (KO) mice exhibit excessive megakaryocytopoiesis accompanied by increased numbers of megakaryocytes associated with the stromal niche rather than the vascular niche. During earlier stages of megakaryocytopoiesis in KO marrow, an expanded Lin−Sca-1+ c-kit+ hematopoietic stem cell (HSC) population and increased quiescent Lin− progenitor pool were identified. During the later stages of megakaryocytopoiesis, CD31KO megakaryocytes exhibited abnormal adhesion/transmigration behaviors. Lastly, KO animals exhibited excessive splenic extramedullary megakaryocytopoiesis, which likely compensates for the impaired marrow megakaryocytopoiesis, resulting in normal peripheral platelet number. Thus, PECAM-1 modulates megakaryocytopoiesis in a hierarchic manner, functioning as a thermostat to “fine-tune” megakaryocytopoiesis.
Introduction
Megakaryocytopoiesis is regulated by cell-cell and cell-matrix interactions, stimulatory/inhibitory cytokines, and expression of transcription factors seamlessly in a tempospatial fashion. Platelet endothelial cell adhesion molecule-1 (PECAM-1, or CD31), a member of the immunoglobulin superfamily, is a 130 kDa glycoprotein present on endothelial cells and immature and mature circulating hematopoietic cells. It is known to be a modulator of vasculogenesis, angiogenesis, endothelial cell-hematopoietic cell adhesion and signaling, bleeding time, platelet-collagen interactions, lymphocyte signaling and activation, vascular permeability, and directed migration.1–9 PECAM-1 functions as a scaffolding for a number of adaptor, signaling, and structural proteins, including SHP-1, SHP-2, Src family kinases, STAT3 and STAT5, and β- and γ-catenin.10–17
Other than exhibiting smaller than normal litter sizes, PECAM-1 null animals appear to develop normally and do not exhibit any evidence of abnormal physiology under normal baseline conditions. However, as the animals age they develop an autoimmune lupuslike syndrome18 and, when stressed, a variety of abnormal responses are noted. Specifically, PECAM-1 null animals exhibit a prolonged bleeding time; delays in reestablishing vascular permeability barriers when challenged; persistent, robust cytokine expression following challenge; blunted angiogenesis; altered leukocyte responsiveness to selected cytokines; blunted directed migration of polymorphonuclear leukocytes; altered conductive vasodilation and dysregulation of matrix metalloprotease (MMP) expression; and impaired recovery of peripheral platelet count in immune-induced thrombocytopenia.2,7,9,13,19–22 Many of these observations, when modeled and tested in vitro, were shown to be mediated by alterations in the localizations and/or functions of selected adaptor, signaling, or cytoskeletal proteins that are known to interact with PECAM-1.2,8,9,13,16,20,21,23
Of interest is the finding that despite PECAM-1's presence in hematopoietic cells and endothelial cells, peripheral blood counts revealed normal numbers of all the mature circulating blood elements in PECAM-1 null mice.7 However, in this report, upon examination of the bone marrow of PECAM-1 null animals we observed that CD31KO marrow was hypercellular, with excessive megakaryocytopoiesis and altered localizations of polyploid megakaryocytes. Further examination of CD31KO marrow revealed abnormal characteristics of megakaryocytic progenitors and mature CD31KO megakaryocytes, including altered megakaryocyte adhesion/migratory properties. In this report we attributed the impaired CD31KO marrow megakaryocytopoiesis to an expanded Lin−Sca-1+c-kit+ (LSK) hematopoietic stem cell (HSC) population, increased quiescent G0 pool of Lin− cells, and abnormal adhesion/transmigration behaviors of mature megakaryocytes. We also present data supporting the concept that increased splenic extramedullary megakaryocytopoiesis compensates for the dysregulated bone marrow megakaryocytopoiesis in CD31KO mice, resulting in normal peripheral platelet counts.
Materials and methods
Mice and bone marrow sampling
Age- and gender-matched wild-type (WT), heterozygous (Het), and CD31KO littermates and/or C57BL/6 and CD31KO mice were used in these studies. Following anesthesia and humane killing according to Yale University Animal Care–approved protocols, femurs and tibias were excised. Bone marrow (BM) cell suspensions were harvested from the diaphyses by flushing and from the epiphyses by bone crushing and mincing in PBS/2% FBS followed by filtering through a 40-μm nylon strainer to remove bone debris.
Tissue section preparation
Age-matched mice were anesthetized and humanely killed according to Yale University Animal Care-approved protocols, and femur bones were dissected and immersed in 4% paraformadehyde (pH 7.4) for fixation, followed by decalcification in a 14% EDTA (pH 7.2) solution. The bones were then soaked in 70% ethanol for dehydration and sent to the Bone Histology Facility at Yale Medical School Department of Orthopedics for paraffin sectioning at 5 μm thickness and hematoxylin and eosin staining performed. Spleens were fixed in 4% PFA and sent to the Research Histology Laboratory in the Department of Pathology, Yale University, for paraffin embedding, sectioning, and hematoxylin and eosin staining. The samples were then examined using a microscopy Olympus IX71 microscope equipped with objective lenses (20×/0.4, 10×/0.25, and 4×/0.43) and a 10× eyepiece, and an Optronics MicroFire camera (Olympus America, Melville, NY) and PictureFrame software (Muskogee, OK).
Quantification of megakaryocyte localization in bone marrow
Hematoxylin and eosin–stained paraffin sections were used for quantification. Observation fields with comparable densities of sinusoid vasculature (defined as sinusoidal structures with erythrocytes in their lumina) were selected from WT, Het, and CD31KO femur section slides. Total megakayocyte number was counted in each × 20 observation field, and then the sinusoid vasculature-associated megakaryocytes were counted, followed by calculation of percentage.
Flow cytometric analysis
An LSRII flow cytometer (BD Sciences, San Jose, CA) was used to quantify the cell populations, cell cycle profiles, and cell apoptosis. Bone marrow mononucleated cells were harvested using NycoPrep (1.077A) gradient. To measure LSK populations, the cells were labeled with biotinylated mouse lineage panel antibodies (BD Pharmingen, San Diego, CA) followed by PerCP-conjugated streptavidin (BD Pharmingen) and stem cell markers Sca-1 (PE conjugated) and c-kit (APC conjugated) (BD Pharmingen). A lineage-negative (Lin−) population was gated for further analysis of stem cell phenotype (Sca+, c-kit+, Lin−). To measure cell cycle profile, cells were stained with lineage panel antibodies, incubated with 5 μg/mL DNA dye Hoechst 33342 for exactly 90 minutes at 37°C and 1 μg/mL RNA dye Pyronin Y for 45 minutes. The gated Lin−/HoechstLow population was analyzed for the ratio of Pyronin Ylow (quiescent G0) versus Pyronin Yhigh (G1). To detect apoptotic cells, Lin−, c-kit+ cells were stained with annexin V (BD Pharmingen) and propidium iodide (BD Pharmingen). Cells excluding propidium iodide but binding annexin V were considered apoptotic. To analyze CD41a+ cell percentage, marrow cells, spleen cells, or peripheral blood cells were stained with PE-conjugated CD41a antibody (BD Pharmingen). For determination of integrin profiles and CXCR4 expression levels, marrow cells were stained with PE-conjugated CD41a antibody as well as FITC-conjugated antibodies to either integrin panels (β1, β 3, α5, or αV) or CXCR4 (BD Pharmingen). CD41a+ cells were then gated for expression levels of integrins or CXCR4. Isotype and unstained control antibodies were used in each experiment.
Short-term colony formation unit assay
Bone marrow cells were harvested from murine femurs and incubated with E-lyse buffer (8.3 g/L NH4Cl, 37 mg/L EDTA, 1 g/L KHCO3) at room temperature for 5 minutes to lyse erythrocytes. The cells were then washed once with PBS and resuspended in Iscove MDM (IMDM). A total of 5 × 104 cells were used in each colony-forming unit (CFU)/Meg-CFU assay. CFU and Meg-CFU assays were performed according to the manufacturer's protocols (MethoCult M3234 methylcellulose medium and MegaCult-C collagen medium; Stem Cell Technologies, Vancouver, BC, Canada). A total of 50 ng/mL Tpo (or 50 ng/mL SCF), 50 ng/mL IL-11, 10 ng/mL IL-3, and 20 ng/mL IL-6 (Peprotech, Rocky Hill, NJ) were used in these assays. The cultures were in 37°C incubator for 6 to 8 days. Colonies containing more than 10 cells under × 20 objective were scored as CFUs, and colonies containing more than 3 megakaryocytes under × 20 objective were considered Meg-CFUs (megakaryocytes were identified by acetylcholinesterase staining according to manufacturer's protocol). To confirm the effects of PECAM-1 deficiency on progenitor cell CFU capabilities WT mononuclear cell populations were stained with c-kit and CD31 antibodies and then fluorescence-activated cell sorter (FACS) sorted into WT CD31+, c-kit+ and WT CD31−, and c-kit+ subpopulations. Due to the low viability of sorted cells, 10 000 cells were used as input for CFU assays of WT CD31+, c-kit+, WT CD31−, c-kit+ cells, as well as FACS-sorted c-kit+ cells from CD31KO mice (CD31KO c-kit+).
CD41a+ cell FACS sorting
Bone marrow mononucleated cells were stained with FITC-conjugated anti-CD41a (BD Pharmingen) followed by isolation of CD41a+ cells on a FACS sorter (BD FACSVantage SE, BD Sciences, San Jose, CA).
Cell adhesion and transmigration assays
The cell transmigration studies were performed according to published methods.24 Transwell chambers (5 μM pore size) were covered with a monolayer of murine lung microvascular endothelial cells9 or BM stromal cells (M2-10B4, ATCC cell lines; American Type Culture Collection, Manassas, VA). FACS-sorted CD41a+ cells were added to the upper chamber with SDF-1 at various dosage in serum-free IMDM placed in the lower chamber. After 4 hours, the CD41a+ cells were collected in the lower chamber (transmigrated cells) and upper chamber (unadhered cells) for quantification. The adherent cell number on endothelial cells was further determined by subtracting the transmigrated cell number and nonadherent cell number from total input cell number. For adhesion assays, the sorted CD41a+ cells were added to the multiwell plates coated with either fibronectin (10 μg/mL)24 or VCAM-1 (10 μg/mL)24 in the presence or absence of FGF4 (100 ng/mL). After 2 hours, the number of attached CD41a+ cells was counted.
Splenectomy
Splenectomy was performed on age-matched WT and CD31KO mice according to a published procedure.25
Serum and plasma Tpo concentration measurement
Quantikine Murine Tpo Immuonassay Kit (R&D Systems, Minneapolis, MN) was used to quantify Tpo concentration in harvested sera.
Peripheral murine blood platelet counting
Mice were anesthetized with ketamine/xylazine followed by retro-orbital sinus bleeding (approximately 200 μL) using heparinized 100λ Pasteur pipettes. The blood was evacuated into heparinized tubes and immediately mixed with 100 μL of 20 mM EDTA/PBS buffer to prevent clot formation. The blood sample was then incubated with 2 μL CD16/CD32 Fc blockers for 5 minutes on ice, followed by staining with PE-conjugated CD41a and FITC-conjugated CD42d antibodies for 20 minutes. After 2 washes and spins (7500 rpm [5900g] for 10 minutes), the samples were fixed with 1% PFA and used for FACS analyses. Logarithmic amplifications for forward scatter (FSC) and side scatter (SSC) gains were selected to identify a CD41a+, CD42d+ population. Gated CD41a+, CD42d+ population events were recorded.
Bleeding time
Bleeding times were assessed as described.7 Deep anesthesia was induced with Ketaset. The mice were then secured into a tabletop holder with their tails taped downward and perpendicular to their bodies. After being pulled through a 1.5-mm-diameter template, the tails were transected with ascalpel blade and bled onto a Whatman filter paper. The filter was dabbed to the wound every 30 seconds without disrupting the forming clot. Any blood dripping during the 30-second intervals was allowed to drop freely onto the filter. The experiment was continued until bleeding stopped completely (wild type). The bleeding of PECAM-1-deficient animals was stopped by cauterization at 20 minutes to prevent hypovolemic shock.
Statistics
Statistical significance was determined by 1-way analysis of variance (ANOVA) with the Fisher multiple comparison test and N-way ANOVA using Statview (Cary, NC). All data are expressed as mean SD, and differences are considered significant at a value of P less than .05.
Results
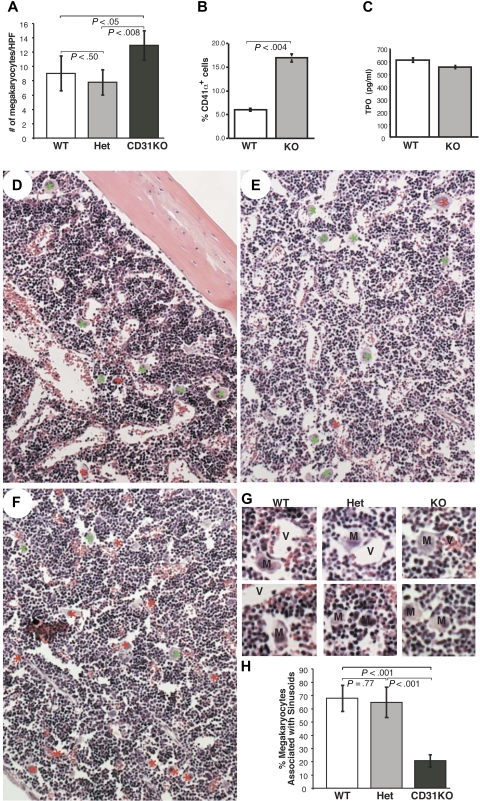
Bone marrow of PECAM-1 null mice exhibits increased megakaryocyte numbers and altered marrow localizations
Counting femoral bone marrow megakaryocytes from CD31KO, Het, and wild-type (WT) littermates revealed significant increases in CD31KO megakaryocyte numbers compared with WT and Het littermates (Figure 1A). In addition, the percent of CD41a+ cells was increased in BM harvested from CD31KO femurs compared with WT specimens (Figure 1B) despite essentially identical plasma and serum TPO levels (Figure 1C). This was confirmed using the offspring of Het × Het litters, with CD31KO offspring exhibiting 19.3% ± 1.6% CD41a+ cells, while Het and WT littermates exhibited 8.4% ± 0.9% and 9.8% ± 1.6% CD41a+ cells, respectively. Further, in additional littermate studies, the ratios of megakaryocytes associated with marrow sinusoid microvasculature and stromal compartments were noted to be distinct in CD31KO femurs when compared with WT and Het marrows, exhibiting a 1:4 vascular-stromal compartment prevalence, while the Het and WT marrows exhibited a 2:1 vascular-stromal compartment prevalence (Figure 1D-H).
Figure 1.
PECAM-1 null marrow exhibits excessive megakaryocytopoiesis and altered megakaryocyte localization. (A) Comparison of the numbers of megakaryocytes per high-power field in the femurs of WT, Het, and CD31KO littermates (n = 12). (B) Comparison of percentage of CD41a+ cells in WT and CD31KO BM (n = 11). (C) Comparison of Tpo concentration in WT and CD31KO peripheral blood serum (n = 3). (D-F) Representative low-power (10×) micrographs of hematoxylin and easin staining of WT, Het, and CD31KO femoral bone marrow sections. In WT (panel D) and Het (panel E) marrow, many WT megakaryocytes were shown to be associated with the sinusoidal vasculature (green asterisks), while most CD31KO megakaryocytes (F) were resident in the stromal compartment (red asterisks). (G) Representative high-power (20×) micrographs of WT, Het, and CD31KO marrow sections illustrating megakaryocytes (M) intimately associated with marrow vessels (V) in the top panels and megakaryocytes in the stromal compartment of the marrow in the bottom panels. (H) Quantification of megakaryocyte cell numbers in each × 20 high-power-field revealed significantly more megakaryocytes associated with sinusoidal vessels in the WT and Het marrows, while most CD31 KO megakaryocytes were observed to be resident in the stromal areas. Specifically, quantitation revealed a ratio of megakaryocyte localization in vasculture to stromal niches of 2:1 in WT and Het BMs and 1:4 in CD31KO BMs (n = 12). Vertical lines in the bar graphs represent standard deviations.
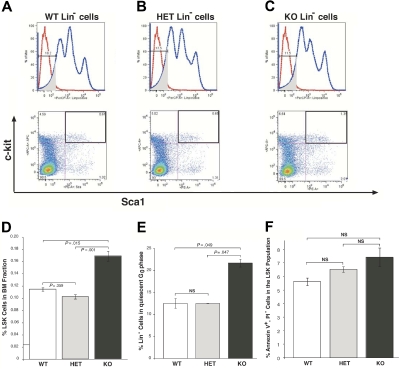
PECAM-1 null early hematopoietic precursors exhibit increased numbers and more cells in quiescent G0 phase
FACS analyses of CD31KO marrow progenitor cells revealed increases in the percentage of Lin−, Sca-1+, c-kit+ (LSK) cells compared with WT and Het LSK cells (Figure 2A-D); and more CD31KO Lin− cells arrested in quiescent PyroninlowHoechstlow G0 phase compared with WT and Het Lin− cells (Figure 2E). However, cell apoptosis was not affected, as evidenced by annexin V staining (Figure 2F), and cell cycle kinetics were not perturbed, because percent BrdU incorporation kinetics in WT and CD31KO LSK cells was similar when assessed at 3 hours (WT, 2.54%, versus CD31KO, 3.05%; P = .12, n = 3) and 6 days (WT, 57.1%, versus CD31KO, 55.2%; P = .29, n = 3) after BrdU in vivo injection.
Figure 2.
PECAM-1 null marrow exhibited an expanded hematopoietic stem cell population and increased quiescent G0 phase cells. (A-C) Representative graphs of flow cytometric assays on the hematopoietic stem cell populations of WT, Het, and CD31KO cells (Lin−, Sca-1+, c-kit+ cells [LSK]). The same number of BM mononuclear cells (250 000) was used in each FACS assay. The top panels are representative FACS plots of Lin− population gating. The shaded areas of these graphs represent gated Lin− areas, which exclude high-intensity, intermediate-intensity, and low-intensity PerCP-positive populations. Nonstained controls (red lines) were included in these graphs. The bottom panels are corresponding representative graphs of the percentages of Sca-1+, c-kit+ cells in gated Lin− populations of WT, Het, and CD31 KO littermates. (D) The percentage of LSK cells in BM fraction (LSK cell number divided by BM cell fraction number) was significantly increased in KO marrow (denoted in the heavy outlined quadrants in panels A-C and quantitated in panel D; n = 3). (E) Distribution of cells in G0 versus G1 in the Lin− BM mononuclear WT, Het, and CD31KO cell populations indicates increased CD31KO hematopoietic progenitor cells were arrested in quiescent G0 phase (n = 3). Marrow cells were stained with lineage antibodies, Pyronin Y(RNA dye), and Hoechst 33342 (DNA dye). Lin− cells that had low Hoechst staining (cells in G0/G1 phase) were gated for analyses. The average G0 percentage in Lin−Hoechstlow cells from CD31KO marrow is significantly increased compared with that of WT and Het marrows (n = 3). (F) The mean percentages of annexin V-positive, PI-negative cells representing apoptotic cells were not significantly different in WT, Het, and CD31KO Lin−, c-kit+ populations (n = 3). Vertical lines represent standard deviations.
PECAM-1 null marrow exhibits fewer functional megakaryocytic progenitor colonies in short-term CFU assay
To quantitate the functional progenitor cells, methylcellulose CFU assays for total marrow progenitors and acetylcholine esterase-positive colony-forming unit (CFU-MK) assays for megakaryocytic progenitors were performed. Significantly lower numbers of CFUs (Figure 3A) and Meg-CFUs (Figure 3B) derived from whole marrow cells were observed in CD31KO marrow compared with cells derived from WT or Het animals.
Figure 3.
PECAM-1 null marrow exhibits fewer functional megakaryocytic progenitors in short-term colony formation assay. (A) CFU assay comparing the number of functional hematopoietic stem cells (HSCs) between WT, Het, and CD31KO littermate BMs. Input cells (5 × 104) for CFU assays were erythrocyte-depleted whole BM cells (n = 3). (B) CFU-MK assay comparing the functional megakaryocytic progenitor cell numbers between WT, Het, and CD31KO marrow. The 5 × 104 input cells were erythrocyte-depleted whole BM cells. The megakaryocytic colonies were identified using acetylcholine esterase assays (n = 3). (C) The presence of CD31 on HSCs affects their function. The Lin− c-kit+ WT cells were sorted into 2 populations: Lin−, c-kit+, CD31+ and Lin−, c-kit+, CD31−, followed by CFU assays using 10 000 sorted cells as inputs. The sorted Lin− c-kit+ population from CD31KO mouse marrow was used as a control. In the absence of CD31, WT hematopoietic progenitor cells were less functional in terms of CFU capability (n = 3). Vertical lines represent standard deviations.
To determine whether the presence of CD31 on hematopoietic progenitor cells affects cell functions, WT bone marrow cells were used as a source to isolate PECAM-1+ (CD31+ c-kit+ WT cells) and PECAM-1− (CD31− c-kit+ WT cells) progenitor populations for CFU assays. FACS-sorted CD31− c-kit+ WT cells demonstrated significantly fewer CFUs compared with that of CD31+ c-kit+ WT progenitors (Figure 3C). The significant CFU number difference noted between CD31− c-kit+ WT progenitors and c-kit+ progenitors derived from CD31KO marrow (c-kit+ CD31KO cells) was due to the unequivalent progenitor pool sizes (Figure 3C).
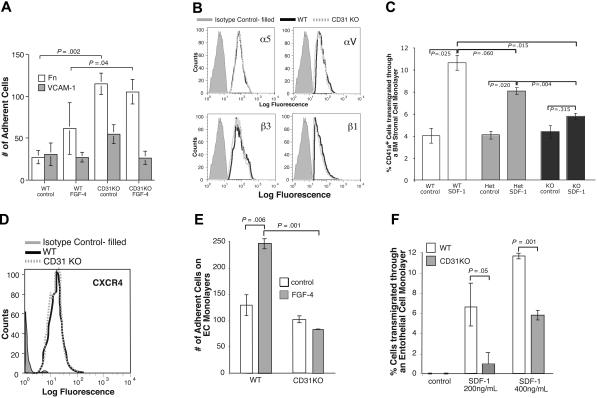
PECAM-1 null megakaryocytes exhibit abnormal adherence behavior and decreased motility
Because the homing/residency/migration of megakaryocyte progenitors is essential for marrow megakaryocytopoiesis, we examined the adhesive and migratory behaviors of CD41a+ cells derived from WT and CD31KO marrow in vitro. Adherence to fibronectin and VCAM-1 was assessed in the absence and presence of FGF4, a chemokine known to induce megakaryocyte adhesion.26 The CD31KO CD41a+ cells showed a significantly increased basal level of adherence to fibronectin, exhibiting a 5-fold increase compared with WT control and 2-fold increase compared with FGF4-induced WT adherence. This adherence was FGF4 noninducible in the CD31KO cells (Figure 4A). The integrin expression profiles of WT and CD31KO CD41a+ cells were compared. As illustrated in Figure 4B, the expression profiles of β1, β3, α5, and αV integrins of WT and CD31KO megakaryocytes were essentially superimposable.
Figure 4.
PECAM-1 null CD41a+ cells showed abnormal adherence and transmigration behavior. (A) Adherence of WT and CD31KO CD41a+ cells on fibronectin- or VCAM-1-coated multiwell plates in the presence or absence of FGF4 (n = 3; P > .04). (B) Integrin α5, αV, β1, and β3 expression profiles were near identical between WT and KO CD41a+ cells. Bone marrow cells were harvested for FACS analyses, and only CD41a+ cells were gated for integrin expression level quantitation (control = isotype control antibody). (C) Transmigration of WT, Het, and KO littermate CD41a+ cells through stromal cell monolayers in response to SDF-1 (400 ng/mL) stimulation (n = 3). (D) CD31KO CD41a+ cells showed no defects in CXCR4 expression level. WT and CD31KO bone marrow cells were harvested and cultured for 3 days in Tpo-containing medium. The cells were then analyzed by flow cytometry for CXCR4 expression level on a gated CD41a+ cell population. (E) The adherence of WT and CD31KO CD41a+ cells on endothelial cell monolayers (n = 3). (F) Transendothelial migration of WT and CD31KO CD41a+ cells in response to different dosages of SDF-1 stimulation (n = 3). Vertical lines represent standard deviations.
SDF-1 is a chemokine used to induce megakaryocyte motility.26 In studies using littermates, CD31KO CD41a+ cells showed no appreciable SDF-1-induced transmigration through stromal cell monolayers in contrast with the increased transmigration observed in WT and Het littermate-derived cells driven by SDF-1 (Figure 4C). The impaired migration of CD41a+ cells appears not to be due to altered CXCR4 (SDF-1 receptor) expression levels. As illustrated in Figure 4D, the CXCR4 expression profiles of WT CD41+ and CD31KO CD41a+ cells were found to be essentially superimposable when examined by FACS analysis (Figure 4D).
Interestingly, the enhanced adherence noted in CD31KO CD41a+ cells when plated on a fibronectin substratum (Figure 4A) was not observed when CD31KO CD41a+ cells were incubated with endothelial cell monolayers. Further, FGF4-induced adherence of WT CD41a+ cells to endothelial cell monolayers was impaired in CD31KO CD41a+ cells (Figure 4E). Additionally, while both CD31KO and WT CD41a+ cells exhibited SDF-1-induced transmigration through endothelial cell monolayers, the CD31KO CD41a+ cells exhibited an overall attenuated transmigration at the higher SDF-1 dosage (400 ng/mL) (Figure 4F).
Excessive splenic extramedullary megakaryocytopoiesis compensates for impaired bone marrow megakaryocytopoiesis, resulting in normal peripheral platelet number
In previous studies we demonstrated that the peripheral platelet counts of CD31KO mice were indistinguishable from those of WT C57BL6 mice.7 To address this apparent discrepancy between peripheral platelet counts and megakaryocyte behaviors, we assessed the potential contributions of splenic megakaryocytopoiesis in WT, Het, and CD31KO littermates (Figure 5). Histologic analyses demonstrated that in WT spleen sections only an occasional (approximately 1) morphologically mature megakaryocyte was identified in each × 20 observation field while in knockout (KO) spleens appreciably more (5 or 6) megakaryocytes were observed in each field (Figure 5A-D). The percentage of splenic megakaryocytic CD41a+ cells identified by FACS analyses was significantly increased in CD31KO spleens compared with that found in Het and WT littermate spleens (Figure 5E).
Figure 5.
Increased extramedullary splenic megakaryocytopoieis in PECAM-1 null spleens. (A,C) Low-power (5×) hematoxylin and eosin analyses of WT and CD31KO spleen sections. Circled are megakaryocytes identified by their morphologies. (B) Higher-power (20×) magnification of panel A. (D) Higher power (20×) magnifications of panel C. (E) The percentage of splenic megakaryocytic CD41a+ cells identified by FACS analyses was found to be increased in CD31KO spleens compared with that found in Het and WT littermate spleens (n = 2). (F) Splenectomies on WT and CD31KO mice were performed, and peripheral platelet counts were determined over a 70-day period (WT, n = 4; CD31KO, n = 3). (G) Representative bleeding time assay of age-matched splenectomized CD31KO (top panel) and WT mice (bottom panel) illustrating the increased volume of blood lost over time in the CD31KO animals. Numbers 1 through 5 denote consecutive 30-second intervals following tail clip starting at time 0 (arrowheads). Vertical lines in the bar graphs represent standard deviations.
Splenectomy of WT and CD31 KO mice reveals the spleen as an important contributor of megakaryocytopoiesis in CD31KO mice
The increased number of CD41a+ cells in the CD31KO spleens is consistent with the notion that the CD31KO spleens are functioning as a major site of megakaryocytopoiesis. To test this hypothesis we performed splenectomies on WT and CD31KO mice and determined peripheral platelet counts over a 70-day period. As illustrated in Figure 5F, WT and CD31KO peripheral blood showed similar platelet numbers prior to splenectomy. Following splenectomy, WT platelet counts were observed to increase at day 5, followed by a slight decrease between days 12 and 26 and subsequently increase until sacrifice at day 70, with platelet number exceeding that prior to splenectomy. In contrast, at days 12 through 70 following splenectomy the CD31KO mice exhibited significantly decreased platelet counts, and the platelet number never recovered to presplenectomy levels or the levels in their WT counterparts (Figure 5F). In addition, hematoxylin and eosin staining of liver sections harvested from postsplenectomized WT and CD31KO mice showed no appreciable extramedullary hematopoiesis throughout the course of the study (data not shown).
Bleeding times of splenectomized CD31KO mice were prolonged compared with those of splenectomized WT mice
Forty days after splenectomy the bleeding times of age-matched WT and CD31KO mice were assessed. As observed in our previous study,7 the bleeding times of the CD31KO mice were similarly prolonged compared with the WT mice (data not shown). Moreover, the bleeding time of postsplenectomy mice was prolonged compared with that of unsplenectomized control KO mice (810 seconds versus 600 seconds). In addition, the CD31KO mice exhibited significantly more blood loss during each time point taken compared with the WT mice (Figure 5G).
Discussion
The data presented here demonstrated novel roles of PECAM-1 (CD31) in regulating megakaryocytopoiesis. In addition to its effects on megakaryocytopoiesis, PECAM-1 deficiency has been found to also affect B lymphocyte development and is associated with reduced B lymphocyte numbers in the spleen, resulting in disordered lymphocyte function leading to the development of autoimmune disease.27 In this paper we focused on the impacts exerted by PECAM-1 deficiency on megakaryocytopoieis, which spans several developmental stages. Earlier at the progenitor stage, an expanded LSK population was observed in CD31KO BM littermates. Further, an increased fraction of the CD31KO Lin− population is arrested in quiescent G0 phase, which is consistent with decreased CFU colony number derived from short-term (6- to 8-day culture) assay of CD31KO marrow cells and the slower recovery rate of CD31KO bone marrow after 5-FU (Fluorouracil) treatment (a procedure to ablate proliferating cells and enrich progenitor cells). In addition, a similar cell apoptosis rate, as evidenced by annexin V-positive, Propidium Iodide (PI)-negative staining, was observed in both WT and CD31KO marrow Lin− cells. Thus, most likely the expanded LSK population in CD31KO marrow is due to increased G0 quiescent cell pool, in which most primitive hematopoietic progenitor cells remain.28,29 The abnormal characteristics of CD31KO stem cells, such as the increased G0 phase population and LSK population and decreased short-term colony-forming potential, may also be caused by a microenvironmental effect rather than only by a stem cell-autonomous effect, which will be pursued in future studies.
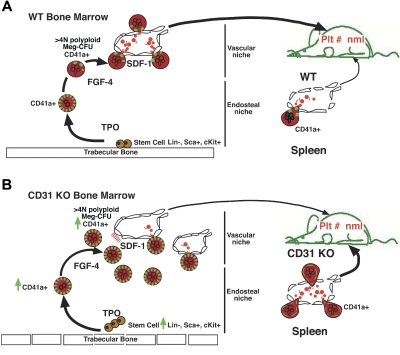
During megakaryocytopoiesis, the progenitors migrate from the stromal cell niche to sinusoidal vasculature accompanied by differentiation and maturation (Figure 6). This complex dynamic process involves multiple adhesion and transmigration events regulated by several chemokines, including Tpo and SDF-1. Our data suggest that CD31KO immature megakaryocytes have a greater basal level adhesion on fibronectin, which suggested that CD31KO cells may exhibit altered expression and/or activation levels of adhesion receptors (because CD31 is known to affect integrin behavior5,30). Our FACS analyses of integrin expression revealed near identical levels of β1, β 3, α5, and αV integrins of WT and CD31 KO megakaryocytes. Thus, while expression levels are similar, affinity, avidity, and downstream signaling may be different, causing the observed changes in adhesion/transmigration. This altered adhesion may affect the egress of CD31KO progenitor cells from the stromal cell niche to the vascular niche (Figure 5). Further, the impaired FGF4-induced adhesion of CD41a+ CD31KO cells with endothelial monolayers indicates that the CD31KO cells may have defects in maintaining vascular residency in marrow. Finally, the decreased CD31KO CD41a+ cell transmigration rates through stromal and endothelial cell monolayers may reflect the relative inability of CD31KO cells in leaving the stromal niche and homing to the marrow vasculature during differentiation and maturation. This suggests that CD31KO cells may exhibit altered expression and/or activation levels of CXCR4. However, similar to our integrin expression data, FACS analyses revealed CXCR4 levels to be near identical on WT and CD31KO megakaryocytes. Again, the differences in migration could be explained by differences in downstream signaling and/or differences in the cells' ability to organize their cytoskeletons. Ongoing biochemical studies reveal that the actin crosslinker moesin31 is not stabilized in the cytoskeleton pool in the absence of CD31 (unpublished observations, January 2006), which was similar to our findings in PECAM-1 null neutrophils.21
Figure 6.
Scheme summarizing the roles of CD31 in megakaryocytopoiesis. CD31 regulates megakaryocytopoiesis in a hierarchic manner (panel A). At a very early stage of megakaryocytopoiesis, CD31 deficiency affects the stem cell niche and subsequent stem cell characteristics (panel B). There is an expanded hematopoietic LSK population and corresponding increased quiescent G0 phase Lin− cell pool in CD31KO marrow. Later, in the absence of CD31, immature megakaryocytes exhibit defects in translocating from the stromal cell niche to the vascular niche, which leads to the accumulation of megakaryocytes in BM. Although the short-term CFU assay suggests decreased functional progenitor cell (progenitor cells with short-term reconstituting capabilities, which represent relatively active cells) number in CD31KO BM, total CD41a+ cells and mature megakaryocytes were increased, which could be the combinatory effect of increased megakaryocytic progenitor cell number (most of them presumed to be quiescent cells with long-term reconstituting capabilities) and migration defects of megakaryocytes in CD31KO BM. Despite the reduction in platelet release caused by the decreased of association between CD31KO megakaryocytes and marrow sinusoidal vasculature, extramedullary splenic megakaryocytopoiesis is enhanced to generate a normal peripheral blood platelet number.
Although the observed abnormal megakaryocytosis in CD31KO marrow may be due to a combinatorial effect of both marrow microenvironment and intrinsic cell defects, the loss of CD31's scaffolding and signaling functions in both hematopoietic precursor cells and endothelial cells serves as a reasonable explanation of both. SHP-1 has been demonstrated to be expressed exclusively on hematopoietic cells, and SHP-1 activation is essential for hematopoietic development.32 CD31-induced SHP-1 recruitment may activate SHP-1 in hematopoietic cells, because we observed that CD31KO neutrophils exhibit decreased SHP-1 activity.21 Therefore, in the absence of CD31-SHP1 signaling, Tpo/SDF-1-induced megakaryocyte signaling cascades may be perturbed.
A recent paper published by Dhanjal et al22 reported similar numbers of CD41a+ cells in WT and CD31KO BM sections and similar proportions of CD41a+ cells localized to BM microvessels (identified by endoglin staining) by analyzing microscopic observation fields. The inconsistency between their data and our observations may be due to different methods of analysis. Namely,1 we used hematoxylin and eosin staining to identify mature megakaryocytes with typical morphologic characteristics, while Dhahjel et al22 used CD41a+ staining that theoretically comprises immature progenitor cells as well as mature megakaryocytes.2 Similarly, we used hematoxylin and eosin staining to demonstrate mature megakaryocyte localization rather than the localizations of all megakaryocytic cells shown by Dhanjal et al.22
Interestingly, despite the perturbed megakaryocytopoieis in CD31KO BM, both serum and plasma Tpo levels and peripheral blood platelet numbers were in the normal range in CD31KO mice. Presumably, there exists a compensatory extramedullary megakaryocytopoietic pathway in CD31KO mice. Investigations revealed that in CD31KO spleens CD41a+ cells were increased 2-fold compared with WT and Het littermates as evidenced by an increased percentage of megakaryocytes determined by FACS analyses and significantly more megakaryocytes observed microscopically. These findings—coupled with the fact that splenic sinusoid vasculature is discontinuous,33 likely providing easy access of platelets to the vasculature, while murine bone marrow microvasculature is thought to be continuous34 and possibly more restrictive—would result in normal peripheral platelet counts in CD31KO mice. Thus, it is hypothesized that increased KO spleen megakaryocytopoieis contributes to the hematostasis of platelets in peripheral blood (Figure 6). This concept was confirmed by our findings that splenectomy of CD31KO mice resulted in a significant reduction in the peripheral platelet counts. The exact mechanisms involved in the increased megakarycotye splenic homing and/or residency observed in the CD31KO mice remain unknown and a topic of future investigation. However, spleen CFU assays have revealed that the CD31KO splenic hematopoietic progenitor cells have differential differentiation capacity compared with that of WT progenitor cells, with more cells exhibiting the multilobed nuclear morphology (data not shown).
In summary, we have identified novel roles of PECAM-1 in modulating megakarycytopoiesis in a hierarchic manner, with PECAM-1 having multiple regulatory effects on megakaryocytes and their progenitors (Figure 6).
Acknowledgments
This work was supported in part by United States Public Health Service (USPHS) grants R37-HL28373 and PO1-DK55879 (J.A.M.) and a Reed Foundation Fellowship (Y.W.).
Footnotes
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: Y.W. and J.A.M. designed and performed research, collected and analyzed data, and wrote the paper; and T.W. and M.M. performed research and collected and analyzed data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Joseph A. Madri, Department of Pathology, Yale University School of Medicine, 310 Cedar St, New Haven, CT; e-mail: joseph.madri@yale.edu.
References
- 1.Ilan N, Madri JA. PECAM-1: old friend, new partners. Curr Opin Cell Biol. 2003;15:515–524. doi: 10.1016/s0955-0674(03)00100-5. [DOI] [PubMed] [Google Scholar]
- 2.Solowiej A, Biswas P, Graesser D, Madri JA. Lack of platelet endothelial cell adhesion molecule-1 attenuates foreign body inflammation because of decreased angiogenesis. Am J Pathol. 2003;162:953–962. doi: 10.1016/S0002-9440(10)63890-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newman PJ, Newman DK. Signal transduction pathways mediated by PECAM-1: new roles for an old molecule in platelet and vascular cell biology. Arterioscler Thromb Vasc Biol. 2003;23:953–964. doi: 10.1161/01.ATV.0000071347.69358.D9. [DOI] [PubMed] [Google Scholar]
- 4.DeLisser HM, Christofidou-Solomidou M, Strieter RM, et al. Involvement of endothelial PECAM-1/CD31 in angiogenesis. Am J Pathol. 1997;151:671–677. [PMC free article] [PubMed] [Google Scholar]
- 5.Wee JL, Jackson DE. The Ig-ITIM superfamily member, PECAM-1 regulates the ‘outside-in’ signalling properties of integrin alpha(IIb)beta3 in platelets. Blood. 2005;106:3816–3823. doi: 10.1182/blood-2005-03-0911. [DOI] [PubMed] [Google Scholar]
- 6.Muller WA. The role of PECAM-1 (CD31) in leukocyte emigration: studies in vitro and in vivo. J Leukoc Biol. 1995;57:523–528. doi: 10.1002/jlb.57.4.523. [DOI] [PubMed] [Google Scholar]
- 7.Mahooti S, Graesser D, Patil S, et al. PECAM-1 (CD31) expression modulates bleeding time in vivo. Am J Pathol. 2000;157:75–81. doi: 10.1016/S0002-9440(10)64519-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gratzinger D, Canosa S, Engelhardt B, Madri JA. Platelet endothelial cell adhesion molecule-1 modulates endothelial cell motility through the small G-protein Rho. FASEB J. 2003;17:1458–1469. doi: 10.1096/fj.02-1040com. [DOI] [PubMed] [Google Scholar]
- 9.Graesser D, Solowiej A, Bruckner M, et al. Altered vascular permeability and early onset of experimental autoimmune encephalomyelitis in PECAM-1-deficient mice. J Clin Invest. 2002;109:383–392. doi: 10.1172/JCI13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sagawa K, Kimura T, Swieter M, Siraganian RP. The protein-tyrosine phosphatase SHP-2 associates with tyrosine-phosphorylated adhesion molecule PECAM-1 (CD31). J Biol Chem. 1997;272:31086–31091. doi: 10.1074/jbc.272.49.31086. [DOI] [PubMed] [Google Scholar]
- 11.Pumphrey NJ, Taylor V, Freeman S, et al. Differential association of cytoplasmic signalling molecules SHP-1, SHP-2, SHIP and phospholipase C-gamma1 with PECAM-1/CD31. FEBS Lett. 1999;450:77–83. doi: 10.1016/s0014-5793(99)00446-9. [DOI] [PubMed] [Google Scholar]
- 12.Jackson DE, Ward CM, Wang R, Newman PJ. The protein-tyrosine phosphatase SHP-2 binds platelet/endothelial cell adhesion molecule-1 (PECAM-1) and forms a distinct signaling complex during platelet aggregation. Evidence for a mechanistic link between PECAM-1- and integrin-mediated cellular signaling. J Biol Chem. 1997;272:6986–6993. doi: 10.1074/jbc.272.11.6986. [DOI] [PubMed] [Google Scholar]
- 13.Carrithers M, Tandon S, Canosa S, Michaud M, Graesser D, Madri JA. Enhanced susceptibility to endotoxic shock and impaired STAT3 signaling in CD31-deficient mice. Am J Pathol. 2005;166:185–196. doi: 10.1016/S0002-9440(10)62243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hua CT, Gamble JR, Vadas MA, Jackson DE. Recruitment and activation of SHP-1 protein-tyrosine phosphatase by human platelet endothelial cell adhesion molecule-1 (PECAM-1). Identification of immunoreceptor tyrosine-based inhibitory motif-like binding motifs and substrates. J Biol Chem. 1998;273:28332–28340. doi: 10.1074/jbc.273.43.28332. [DOI] [PubMed] [Google Scholar]
- 15.Ilan N, Cheung L, Miller S, Mohsenin A, Tucker A, Madri JA. Pecam-1 is a modulator of stat family member phosphorylation and localization: lessons from a transgenic mouse. Dev Biol. 2001;232:219–232. doi: 10.1006/dbio.2001.0186. [DOI] [PubMed] [Google Scholar]
- 16.Ilan N, Cheung L, Pinter E, Madri JA. Platelet-endothelial cell adhesion molecule-1 (CD31), a scaffolding molecule for selected catenin family members whose binding is mediated by different tyrosine and serine/threonine phosphorylation. J Biol Chem. 2000;275:21435–21443. doi: 10.1074/jbc.M001857200. [DOI] [PubMed] [Google Scholar]
- 17.Biswas P, Zhang J, Schoenfeld JD, et al. Identification of the regions of PECAM-1 involved in beta- and gamma-catenin associations. Biochem Biophys Res Commun. 2005;329:1225–1233. doi: 10.1016/j.bbrc.2005.02.095. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson R, Lyons AB, Roberts D, Wong MX, Bartley PA, Jackson DE. Platelet endothelial cell adhesion molecule-1 (PECAM-1/CD31) acts as a regulator of B-cell development, B-cell antigen receptor (BCR)-mediated activation, and autoimmune disease. Blood. 2002;100:184–193. doi: 10.1182/blood-2002-01-0027. [DOI] [PubMed] [Google Scholar]
- 19.Payne GW, Madri JA, Sessa WC, Segal SS. Histamine inhibits conducted vasodilation through endothelium-derived NO production in arterioles of mouse skeletal muscle. FASEB J. 2004;18:280–286. doi: 10.1096/fj.03-0752com. [DOI] [PubMed] [Google Scholar]
- 20.Enciso JM, Gratzinger D, Camenisch TD, Canosa S, Pinter E, Madri JA. Elevated glucose inhibits VEGF-A-mediated endocardial cushion formation: modulation by PECAM-1 and MMP-2. J Cell Biol. 2003;160:605–615. doi: 10.1083/jcb.200209014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Y, Stabach P, Michaud M, Madri JA. Neutrophils lacking platelet-endothelial cell adhesion molecule-1 exhibit loss of directionality and motility in CXCR2-mediated chemotaxis. J Immunol. 2005;175:3484–2491. doi: 10.4049/jimmunol.175.6.3484. [DOI] [PubMed] [Google Scholar]
- 22.Dhanjal TS, Pendaries C, Ross EA, et al. A novel role for PECAM-1 in megakaryocytokinesis and recovery of platelet counts in thrombocytopenic mice. Blood. 2007;109(10):4237–4244. doi: 10.1182/blood-2006-10-050740. [DOI] [PubMed] [Google Scholar]
- 23.Pinter E, Mahooti S, Wang Y, Imhof BA, Madri JA. Hyperglycemia-induced vasculopathy in the murine vitelline vasculature: correlation with PECAM-1/CD31 tyrosine phosphorylation state. Am J Pathol. 1999;154:1367–1379. doi: 10.1016/S0002-9440(10)65391-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Romanic AM, Madri JA. The induction of 72-kD gelatinase in T cells upon adhesion to endothelial cells is VCAM-1 dependent. J Cell Biol. 1994;125:1165–1178. doi: 10.1083/jcb.125.5.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coligan JE, Kruisbeek AM, Margulies GH, Shevach EM, Strober W, editors. Current Protocols in Immunology.Vol 1. 5. Vol. 1. Hoboken, NJ: John Wiley & Sons; 1994. Survival surgery: removal of the spleen or thymus. pp. 1.10.1–1.10.3. [Google Scholar]
- 26.Avecilla ST, Hattori K, Heissig B, et al. Chemokine-mediated interaction of hematopoietic progenitors with the bone marrow vascular niche is required for thrombopoiesis. Nat Med. 2004;10:64–71. doi: 10.1038/nm973. [DOI] [PubMed] [Google Scholar]
- 27.Wong MX, Jackson DE. Regulation of B cell activation by PECAM-1: implications for the development of autoimmune disorders. Curr Pharm Des. 2004;10:155–161. doi: 10.2174/1381612043453504. [DOI] [PubMed] [Google Scholar]
- 28.Cheshier SH, Morrison SJ, Liao X, Weissman IL. In vivo proliferation and cell cycle kinetics of long-term self-renewing hematopoietic stem cells. Proc Natl Acad Sci U S A. 1999;96:3120–3125. doi: 10.1073/pnas.96.6.3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huttmann A, Liu SL, Boyd AW, Li CL. Functional heterogeneity within rhodamine123(lo) Hoechst33342(lo/sp) primitive hemopoietic stem cells revealed by pyronin Y. Exp Hematol. 2001;29:1109–1116. doi: 10.1016/s0301-472x(01)00684-1. [DOI] [PubMed] [Google Scholar]
- 30.Dangerfield J, Larbi KY, Huang MT, Dewar A, Nourshargh S. PECAM-1 (CD31) homophilic interaction up-regulates alpha6beta1 on transmigrated neutrophils in vivo and plays a functional role in the ability of alpha6 integrins to mediate leukocyte migration through the perivascular basement membrane. J Exp Med. 2002;196:1201–1211. doi: 10.1084/jem.20020324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pestonjamasp K, Amieva MR, Strassel CP, Nauseef WM, Furthmayr H, Luna EJ. Moesin, ezrin, and p205 are actin-binding proteins associated with neutrophil plasma membranes. Mol Biol Cell. 1995;6:247–259. doi: 10.1091/mbc.6.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paling NR, Welham MJ. Tyrosine phosphatase SHP-1 acts at different stages of development to regulate hematopoiesis. Blood. 2005;105:4290–4297. doi: 10.1182/blood-2004-08-3271. [DOI] [PubMed] [Google Scholar]
- 33.Junqueira LC, Carneiro J, editors. 11th ed. New York, NY: McGraw-Hill; 2005. Basic Histology: Text and Atlas. [Google Scholar]
- 34.Lapidot T, Dar A, Kollet K. How do stem cells find their way home? Blood. 2005;106:1901–1910. doi: 10.1182/blood-2005-04-1417. [DOI] [PubMed] [Google Scholar]