Abstract
BACKGROUND
Most studies on religion/spirituality predicting health outcomes have been limited to church attendance as a predictor and have focused on healthy people. However, confronting a major medical crisis may be a time when people turn to the sacred.
OBJECTIVE
The purpose of this study was to determine the extent to which changes in spirituality/religiousness occur after HIV diagnosis and whether changes predict disease progression.
DESIGN/PARTICIPANTS
This longitudinal study examined the relationship between changes in spirituality/religiousness from before with after the diagnosis of HIV, and disease progression (CD4 and viral load [VL] every 6 months) over 4 years in 100 people with HIV. Measures included change in religiousness/spirituality after diagnosis of HIV, religiousness/spirituality at various times in one’s life, church attendance, depression, hopelessness, optimism, coping (avoidant, proactive), social support, CD4/VL, and health behaviors.
RESULTS
Forty-five percent of the sample showed an increase in religiousness/spirituality after the diagnosis of HIV, 42% remained the same, and 13% decreased. People reporting an increase in spirituality/religiousness after the diagnosis had significantly greater preservation of CD4 cells over the 4-year period, as well as significantly better control of VL. Results were independent of (i.e., held even after controlling for) church attendance and initial disease status (CD4/VL), medication at every time point, age, gender, race, education, health behaviors (adherence, risky sex, alcohol, cocaine), depression, hopelessness, optimism, coping (avoidant, proactive), and social support.
CONCLUSIONS
There is an increase in spirituality/religiousness after HIV diagnosis, and this increase predicts slower disease progression; medical personnel should be aware of its potential importance.
Keywords: spirituality, religiousness, HIV, disease progression, coping
An enduring question that has intrigued researchers and people in general alike is the extent to which religion/spirituality is related to health outcomes. Several excellent reviews have recently been published.1,2 These reviews have demonstrated that initially healthy people who regularly attend church services have a 25% to 30% reduction in mortality. However, most of these reviews have been limited to church/service attendance as that has been the predictor typically measured in large-scale epidemiological studies. Yet, crisis is a time when people may turn to God.3 Despite this hypothesis, to our knowledge, no one has tested the extent to which an increase in spirituality/religiousness occurs around a crisis point such as receiving a diagnosis of HIV, or the extent to which changes in spirituality/religiousness have been predictive of disease course. In addition, most studies on religion/spirituality and health have been conducted in healthy people (most often the elderly) with less attention to people with illness and almost no studies among people with HIV. Thus, the purpose of this study is to determine whether changes in spirituality/religiousness are related to disease progression, and to examine this specifically with patients facing a major medical illness, namely HIV.
A related question is whether any relationships between spirituality/religion and disease progression found are independent of possible confounding variables that might represent alternative explanations. In investigations of psychosocial variables related to disease progression, one typically controls for effects of age, gender, race, and education.4 More sophisticated analyses1 have controlled for the effects of variables related to both health and to religion/spirituality such as health behaviors. In fact, the Powell review determined that although church attendance was protective against the development of cardiovascular disease, this relationship was largely because more religious people have healthier behaviors.1
Beyond health behaviors, another pathway by which comforting beliefs could be related to slower disease progression is through psychological variables such as less depression or more optimism, which in turn have been related to slower disease progression.4–6 Koenig7 notes that there has been a reliable relationship between religion and better mental health. The finding that greater religiousness or spirituality is associated with less distress or depression has been found in HIV as well.8,9 Alternatively, it is possible that people who are more distressed turn to religion to cope, in which case people with higher religiousness/spirituality might do worse. All of this suggests that depression should be considered as a potential covariate, but that the relationship might not be simple. Social support is another variable that has been related both to religious involvement7 and to disease progression in HIV,4 and could be considered as a covariate. Thus, another goal of the study was to determine whether any relationship found between disease progression and spirituality/religion levels could be explained by health behaviors, depression/hopelessness, optimism, coping, or social support.
METHODS
Overview
The present study is a longitudinal study where 100 HIV positive participants were seen for an interview, completed questionnaires, and had blood drawn (for CD4 and viral load [VL]) every 6 months for 4 years. The present study was conducted as a substudy of a larger longitudinal study of the psychological and biological factors related to disease progression in HIV.5
Subjects
Inclusion/Exclusion Criteria
Entry to the parent study was designed toward selecting people in the midrange of HIV disease (CD4 cell counts between 150 and 500, never had a clinical AIDS defining symptom, CD4 nadir >75) and who were not actively using drugs, were not drug dependent, having dementia, or psychotic. Entry into the substudy occurred at a time point shortly after baseline (to reduce subject burden). Subjects in the parent study were eligible for the substudy if they were willing to fill out additional questionnaires for additional compensation. All procedures were Institutional Review Board approved and informed consent was obtained from all participants.
Description of the Sample
The sample of 100 people with HIV (see Table 1) was diverse with respect to gender, ethnicity, sexual orientation, and education. Many were poor, which is consistent with high unemployment or disability. Twenty-five percent attended religious services at least weekly, 23% went 1 to 3 times in the past month, and 52% did not go.
Table 1.
Descriptives for Demographic and Background Medical Variables
| Gender | |
| Male | 64% |
| Female | 36% |
| Age | |
| M | 38.00 |
| SD | 8.13 |
| Ethnicity | |
| Non-Hispanic white | 29.3% |
| African American | 38.4% |
| Hispanic white | 27.3% |
| Other | 5.1% |
| Education | |
| Some high school or less | 22% |
| High school graduation | 18% |
| Trade school/some college | 34% |
| College graduation | 19% |
| Graduation degree | 7% |
| Employment | |
| Full time | 13.1% |
| Part time | 19.2% |
| Unemployed | 17.2% |
| Disability | 41.4% |
| Other | 9.1% |
| Income | |
| Less than $10,000/y | 71% |
| $10,000 to $20,000/y | 15.2% |
| Greater than $20,000/y | 14.2% |
| Immune measures | |
| CD4 # | |
| M | 291.38 |
| SD | 96.53 |
| Viral load | |
| M | 48,350 |
| SD | 126,678 |
| Antiretroviral medication | |
| None | 20.3% |
| Combination therapy (non-HAART) | 16.5% |
| HAART | 63.2% |
| Medication adherence (average percentage of missed doses in past 3 d) | |
| M | 0.12 |
| SD | 0.25 |
| Route of infection | |
| Gay/bisexual sex | 46.5% |
| Heterosexual sex | 47.5% |
| IV drug use | 4.0% |
| Other | 2.0% |
| Time since diagnosis (mo) | |
| M | 88.26 |
| SD | 49.92 |
| Sexual orientation | |
| Homosexual/bisexual | 51.5% |
| Heterosexual | 48.5% |
HAART, highly active antiretroviral therapy.
n=99 for variables with decimal points.
At substudy entry, the average CD4 was 291 and the average VL was 48,350 copies/mL. Other background medical information is given in Table 1. The substudy participants did not differ significantly from the parent study on any of the variables in Table 1 (all χ2 nonsignificant).
Measures
Health Behaviors
Several heath behaviors relevant to HIV were assessed. Risky Sex was determined by interview (0=not active, 1=practicing safer sex [using condoms all of the time]; 2=practicing safer sex sometimes, 3=sexually active, but not practicing safer sex). Adherence was assessed by the interviewer-administered AIDS Clinical Trials Group (ACTG)10 measure calculated as the percentage of missed doses averaged over each time point for which the subject was taking medications. Past drug/alcohol abuse and dependence and psychotic symptoms were assessed using the Structured Clinical Interview for Diagnosis of Mental Disorders (SCID-DSM-III-R). Current alcohol and cocaine use was also assessed through questionnaire items asking how often the substance had been used in the past month.
Psychosocial Measures—Increase in Religiousness/Spirituality (INCRS)
Participants were asked “Compared to before you were HIV positive, did you become ___ religious/spiritual after you found out you were HIV positive?” (A) much less, (B) less, (C) the same, (D) more, and (E) much more. Religious service attendance was measured by asking how often participants attended services in the last month. Depression was assessed by the Beck Depression Inventory,11 hopelessness by the Beck Hopelessness Scale,12 optimism by a composite of the Life Orientation Test (LOT)13 and LOT-R,14 which assess dispositional optimism or the degree to which one generally anticipates positive outcomes (e.g., I always look on the bright side of things). Coping strategies were derived from the COPE.15 Two subscales, denial and behavioral disengagement, were combined to create an avoidant coping composite because of previous work relating them to disease outcomes in HIV.4,16 Proactive behavior was assessed by interview ratings of self-initiated behavior as described in Ironson et al.6 Social Support was assessed using the Enhancing Recovery in Coronary Heart Disease Clinical Trial (ENRICHD) Social Support Instrument (ESSI).17 All of the above measures were administered at the parent study baseline, except for INCRS, which was given at substudy entry.
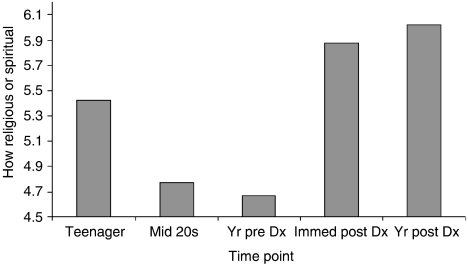
“Religiousness/Spirituality at various times in one’s life” measure. Finally, a series of 5 questions was asked to assess religiousness/spirituality at various times in one’s life. “How religious/spiritual did you consider yourself to be at each of these periods in your life? Please answer on a scale of 1 to 10 where 1=not religious/spiritual at all, and 10=very religious/spiritual.” The periods of time were: “(1) When you were a teenager.(2) During your mid 20s.(3) The year before you were diagnosed with HIV.(4) Right after you were diagnosed with HIV.(5) The year after you were diagnosed with HIV.” In contrast with the other questionnaire measures, this question was asked at a time point approximately 3 years after the rest of the substudy began, placing it close to the end of the 4-year period. It was given both for descriptive and validation purposes. The correlation between the INCRS variable and the increase in spirituality pre- to 1 year post-HIV diagnosis (question 5 minus 3) was 0.37 (P<.01). As it is statistically significant, but only moderate in size, this correlation provides some, but minimal indication of validity for the INCRS measure.
Disease Progression Markers
CD4 lymphocyte count (CD3+CD4+) was determined by whole-blood 4-color direct immunoflourescence using a Coulter XL-MCL flow cytometer (Beckman-Coulter, Miami, FL). VL utilized the Roche Amplicor RT/PCR assay (Roche Diagnostics Corp., Indianapolis, IN) sensitive to 400 copies of plasma RNA.
Statistical Methods
Hierarchical Linear Modeling (HLM)18 was used to analyze the association between INCRS and the change in CD4 or VL(log) over 4 years. HLM was chosen because it permits one to predict to slope over time (rather than a single time point) and to control for important medical variables that are changing at each time point (such as antiretroviral medications). The basic model is composed of 2 levels. At level 1, equations are used to model individual change in CD4 or VL over repeated time points. Level 2 equations model interindividual differences with between-person predictors such as education and spirituality variables. Thus, systematic variability of the slopes and intercepts at level 1 are modeled with the predictors at level 2. For example, a level 1 equation would model VL(log) for each individual from time and antiretroviral medication. At level 2, the slope of change in VL (differing between persons) is modeled from baseline VL, education, race, age, and gender. Increase in spirituality would be added in the last so that the significance of spirituality could be estimated independent of (i.e., controlling for) the covariates (antiretroviral medications, baseline VL or CD4, age, gender, race, and education). Details of the models and associated statistics for the parent study are provided in Ironson et al.5 In the current substudy of spirituality reported here, individual variation in the slope of CD4 over 4 years was significant, χ2 (94)=356.21, P<.001, as was the individual variation in slope of VL(log), χ2 (94)=190.38, P<.001.
We did not replace missing data. The HLM program (6.0) allows only for listwise deletion. This deletion was performed uniquely for each analysis rather than as a global (MDM creation) deletion in order to maximize the data available. By default, the HLM program uses a restricted maximum likelihood approach for parameter estimation. Missing data were minimal (n=95 to 100 for all variables except religious service attendance (n=92), and those who were missing were not significantly different from those not missing on any of the variables in the HLM analyses.
RESULTS
Increase in Religiousness/Spirituality
Forty-five percent of people in our sample reported an increase in religiousness/spirituality in response to finding out that they were HIV positive (27% more and 18% much more). Forty-two percent remained the same, and only 13% became less spiritual/religious (8% less and 5% much less) according to the INCRS measure. Results using the “religiousness/spirituality at various times in one’s life” measure, which, as noted, derived similar information, but asked in a different way (and toward the end of the 4 year period), are illustrated in Figure 1. Religiousness/spirituality increased significantly from before to after the HIV diagnosis (item 4-item 3; t=3.22, P<.01; item5-item3; t=4.73, P<.01). Interestingly, the sample reported feeling more religious/spiritual as teenagers than in their 20s, and had the lowest level of religiousness/spirituality the year before being diagnosed with HIV.
FIGURE 1.
Religiousness/spirituality at various timepoints before and after receiving a diagnosis (Dx) of HIV seropositivity.
Change in Spirituality/Religiousness and Disease Progression
The key question was whether the change in spirituality/religiousness (INCRS) would predict change in disease progression markers in the longitudinal study over 4 years. As noted above, the primary analysis used in this study was to examine HLM level 2 equations where the slope of change in CD4 or VL was modeled from baseline CD4 or VL, education, race, age, and gender. An increase in spirituality was then added in last so that the significance of spirituality could be estimated independent of the covariates (antiretroviral medications at level 1, initial CD4 or VL, age gender, race, and education at level 2). The increase in religiousness/spirituality (INCRS) from before to after finding out that one was HIV positive was significantly related to change in CD4 over 4 years (t=3.03, see Table 2) and to change in VL(log) over 4 years (t=−2.94 see Table 3). Thus, people who showed more increase in spirituality after receiving an HIV diagnosis had significantly less loss of CD4 cells over the 4 years and better control of (lower increase in) VL compared with those who showed decreased spirituality. In fact, for every unit of increase in spirituality, there was a preservation of 1.39 CD4 cells per month or 16 CD4 cells per year. The decline ratio for CD4 for those who answered plus one (i.e., they became more religious/spiritual after finding out they were HIV positive) compared with minus one (i.e., they became less religious/spiritual after they found out they were HIV positive) was 0.22. Stated conversely, those who became less religious/spiritual after the diagnosis lost CD4 cells 4.5 times faster than those who become more religious/spiritual. Calculations for the decline ratio are given in Ironson et al.5 A ratio for VL could not be calculated as those who became more religious/spiritual had a slight decrease in VL(log)=−0.030, whereas those who had a decrease in INCRS had an increase in VL(log)=1.18. Thus, VL moved in opposite directions for those high versus low in INCRS.
Table 2.
Association Between Change in Spirituality and CD4 Slope Either Alone or in Combination with Other Predictors
| Other Predictor | Other Predictor Above† INCRS | Increase in Spirituality Above† Other Predictors | ||||
|---|---|---|---|---|---|---|
| γ | t‡ | P | γ | t‡ | P | |
| None | – | – | – | 1.39 | 3.03 | .004** |
| Church attendance | 0.061 | 3.52 | .001** | 1.49 | 3.17 | .003** |
| Health behaviors | ||||||
| Nonadherence (missed doses) | −1.33 | −0.60 | .550 | 1.38 | 2.86 | .006** |
| Risky sex | −0.42 | −0.85 | .399 | 1.56 | 3.23 | .002** |
| Alcohol use | 0.03 | 0.08 | .941 | 1.41 | 2.98 | .004** |
| Cocaine use | −0.55 | −1.13 | .264 | 1.40 | 2.96 | .004** |
| Affect | ||||||
| Optimism | 0.14 | 1.74 | .085 | 1.21 | 2.53 | .013* |
| Depression | −0.11 | −2.74 | .008** | 1.29 | 2.80 | .007** |
| Hopelessness | −0.10 | −0.86 | .392 | 1.32 | 2.72 | .008** |
| Coping | ||||||
| Avoidant | −0.39 | −2.50 | .015* | 1.36 | 3.08 | .003** |
| Proactive | 0.50 | 0.82 | .414 | 1.37 | 2.86 | .006** |
| Social support | −0.14 | −1.85 | .067 | 1.32 | 2.98 | .004** |
P<.05
P<.01.
As noted in text, the model controls for initial CD4, age, gender, education, and ethnicity.
df=99 for overall model, 92 for runs with covariates and 2 predictors, 93 for run with covariates and 1 predictor.
INCRS, increase in religiousness/spirituality.
Table 3.
Association Between Change in Spirituality and VL(log) Slope Either Alone or in Combination with Other Predictors
| Other Predictor Above* INCRS | Increase in Spirituality Above* Other Predictors | |||||
|---|---|---|---|---|---|---|
| γ× 102 | t† | P | γ× 102 | t† | P | |
| None | – | – | – | −0.607 | −2.94 | .005** |
| Church attendance | 0.00 | 0.02 | .984 | −0.725 | −3.66 | .001** |
| Health behaviors | ||||||
| Nonadherence (missed doses) | 1.03 | 1.16 | .250 | −0.612 | −2.88 | .005** |
| Risky sex | −0.29 | −1.10 | .275 | −0.817 | −4.28 | .000** |
| Alcohol use | −0.04 | −0.21 | .832 | −0.624 | −3.05 | .003** |
| Cocaine use | 0.11 | 0.61 | .544 | −0.619 | −3.01 | .004** |
| Affect | ||||||
| Optimism | 0.02 | 0.42 | .675 | −0.588 | −2.77 | .007** |
| Depression | 0.03 | 1.28 | .205 | −0.588 | −2.82 | .006** |
| Hopelessness | 0.06 | 1.47 | .146 | −0.575 | −2.75 | .008** |
| Coping | ||||||
| Avoidant | 0.20 | 2.67 | .009** | −0.604 | −2.86 | .006** |
| Proactive | −0.30 | −1.09 | .281 | −0.620 | −2.95 | .004** |
| Social support | 0.02 | 0.64 | .522 | −0.599 | −2.88 | .005** |
P<.01.
As noted in text, the model controls for initial VL(log), age, gender, education, and ethnicity.
df=99 for overall model, 92 for runs with covariates and 2 predictors, 93 for run with covariate and 1 predictor.
INCRS, increase in religiousness/spirituality; VL, viral load.
The next analysis (see Tables 2 and 3) examined whether INCRS would remain significant independent of (i.e., after controlling for) church attendance, psychosocial variables, and health behaviors. INCRS was significantly correlated with only 2 of these variables: optimism (0.24, P<.05) and hopelessness (−0.21, P<.05). Each variable (such as frequency of attending religious services) was added to the level 2 HLM model, together with INCRS (controlling for the standard covariates). With both service attendance and INCRS in the model, INCRS remained a significant predictor of both CD4 (t=3.17) and VL (t=−3.66). Interestingly, while testing both in the model, attending services contributed unique variance in CD4 (t=3.52), but not VL. Thus, both INCRS and attending services independently predict change in CD4 over time. (Notably, INCRS had a very low correlation with church attendance, r=−0.03.)
As can be seen in Tables 2 and 3, INCRS remained a significant predictor of CD4 (or VL) over 4 years when controlling for health behaviors (adherence, risky sex, use of alcohol, and use of cocaine), affect (optimism, depression, or hopelessness), coping (avoidant, proactive), or social support. Thus, the relationship between INCRS and slower disease progression could not be accounted for by any of the above variables. Interestingly, only depression, avoidant coping, and church attendance remained significant predictors of CD4 change after controlling for INCRS, and only avoidant coping remained a significant predictor of VL(log) increase after controlling for INCRS.
Table 4 compares effect sizes for variables significant in the above analysis. The first and third columns (superscript a) allow for the comparison of the effect size found for INCRS for predicting CD4 (0.301), and INCRS for predicting VL (0.293) to other psychosocial variables that have predicted disease progression in HIV. (Data for the psychosocial variables are from the parent study5,6 using the cumulative average where possible,5 as those would be expected to give the most reliable estimates of the true effect sizes.) As can be seen, the effect size for INCRS is moderate, and slightly larger than that found for other psychosocial variables that have predicted disease progression in HIV. The second and fourth columns allow for the comparison of the effect size for INCRS predicting CD4 or VL alone, or after controlling for standard covariates and the additional predictor. In all cases, the effect size maintains its significance and relative size, varying only from 0.259 to 0.373.
Table 4.
Effect Sizes (ES) for (a) Predictors Controlling for Standard Covariates Only, or for (b) INCRS Controlling for Predictors and Standard Covariates
| Predictor | CD4 | VL(log) | ||
|---|---|---|---|---|
| ES* | INCRS† | ES* | INCRS† | |
| INCRS | 0.301 | 0.301 | 0.293 | 0.293 |
| Religious service attendance | 0.220 | 0.329 | 0.028 | 0.373 |
| Optimism | 0.158 | 0.256 | 0.153 | 0.279 |
| Depression | 0.250 | 0.282 | 0.248 | 0.283 |
| Hopelessness | 0.200 | 0.274 | 0.225 | 0.277 |
| Avoidant | 0.200 | 0.307 | 0.242 | 0.287 |
| Proactive | 0.258 | 0.290 | 0.045 | 0.298 |
Effect size calculated using published data from parent study (n=177; Ironson, 2005), except for religious service attendance (n=161), which is from unpublished data, or for INCR (n=100) from substudy data. All models control for standard covariates (age, gender, race, education, and baseline CD4/VL(log).
Based on substudy sample (n=100) controlling for standard covariates and predictor.
INCRS, increase in religiousness/spirituality; VL, viral load.
DISCUSSION
The first interesting result is that many people (45%) reported an increase in religiousness/spirituality after the diagnosis of HIV. This was corroborated as a significant increase by the “religiousness/spirituality at various times in one’s life” measure. Being diagnosed with a devastating illness may be a time when people re-examine their relation to the sacred. This increase in spirituality is consistent with and may contribute to the observation that many patients (49%) feel that life with HIV is better than it was before getting diagnosed.19 Spirituality/religiousness may contribute to this through their role in coping and meaning making.20 The process by which HIV transforms the lives of people with HIV and the impact of spirituality and coping is quite moving and is further described qualitatively elsewhere.21 For many people, getting HIV becomes a catalyst for positive change, and spirituality is often involved in that change.21
Could this increase in spirituality be related to the maintenance of health? In another study of people with HIV in this issue,20 50% of people with HIV believed that their religiousness/spirituality helped them live longer.22 While we did not examine prediction of mortality, our results showed that those who reported an increase in spirituality had significantly better maintenance of CD4 cells, and significantly better control of the HIV virus. The effect is both statistically and clinically significant as people who showed a decrease in spirituality lost CD4 cells 4.5 times faster than people who showed increased spirituality/religiousness. The effect sizes also highlight the importance of INCRS in comparison with other, more well-established psychosocial predictors of disease progression such as depression and avoidant coping.4,5 Additionally important is our finding that the INCRS-disease progression relationship is independent of other variables known to predict disease progression in HIV, such as depression. As such, it adds a new variable for clinicians seeing patients with HIV to be aware of—one that could have linkages to health in addition to quality of life (other articles in this issue).
While the substudy results corroborated findings in the literature for depression and avoidant coping4,5 even above the effects of INCRS, adherence failed to predict to CD4 or VL changes. We believe this is an issue of sampling as the larger parent study did find adherence significantly predicted better control of VL in 177 people.5 Note that the results for psychosocial predictors in this substudy might also differ from the parent as this substudy controlled for INCRS.
What could possibly account for the relationship between the increase in spirituality and slower disease progression? Behavioral medicine theorizes that the relationship between psychosocial variables and disease course may occur through 3 major pathways: psychological, behavioral, and biological.23 Higher spirituality has been related to a number of these pathways including lower cortisol, less depression, hopelessness, safer sex, and less smoking.8 In the present study, although increase in spirituality was significantly correlated with more optimism and less hopelessness, neither these nor any of the other pathways tested (health behaviors, negative affect or optimistic outlook, coping, or social support) provided the answer. Biological pathways were not tested in this study. Some candidates for psychoendocrine or psychoneuroimmune pathways include cortisol, norepinephrine, or natural killer cells as these have been related to spirituality (cortisol),8 stress,23,24 and HIV disease processes.4,25,26 Having ruled out many potential mediators, it is not clear at this point just what is responsible for this relationship and that remains for future study. Our data do not address the possibility of divine intervention, although it should be noted that the beliefs of many of the people in our sample include this as a possible pathway.
The effect of INCRS was present even after accounting for church attendance, which has been the major variable studied in predicting mortality to date.1,2 In fact, our data indicate that both INCRS and church attendance contribute uniquely and significantly to the prediction of slower loss of CD4 cells, and are virtually independent. Church attendance is a commonly used, albeit limited, proxy for religiousness. The distinction between religiousness and spirituality is presently one of intense interest and discussion.27,28 They are both multifaceted and may involve differences in beliefs and contextual differences in lifestyle, nutritional practices, and social support.
The first limitation of the study is that the establishment of a relationship between an increase in spirituality and a change in CD4/VL over time does not infer causality. Both directions are feasible: that spirituality increases (decreases) are a result of continued good (poor) health or that spirituality increases result in better health. INCRS was measured retrospectively, introducing a possible bias. Longitudinal designs could be strengthened by repeatedly measuring changes in spirituality and health in order to disentangle this chicken and egg question.
A second limitation of the study is that the INCRS measure was a single item with 5 options. While it adds a different construct beyond a single item measure of church attendance that has been used for years in studies of mortality,1 one cannot possibly measure the richness of the concept of increase in spirituality with a single item. Changes in spirituality often involve changes in views of self, view of others, view of the world, view of God, and values and priorities.21 People often re-examine who they are and the meaning of life, and often make concomitant changes in their behavior such as getting off drugs.21 Positive and negative methods of religious coping29 are also relevant. In fact, Pargament and colleagues30 found that religious struggle predicted mortality among medically ill elderly patients followed for 2 years.
The correlation between INCRS and the measure “religiousness/spirituality at various times in one’s life” difference in religion/spirituality pre- to post-HIV diagnosis was, while significant, lower than expected. Part of this may be accounted for by the 3-year difference in question administration. The difference in the way the questions were asked may also account for some of the discrepancy. Finally, some validity to measurement may be given by the remarkable consistency in percent of people with HIV showing an increase in spirituality between our study (45%) and the Cotton et al.22 study (41%) in this issue.
The generalizability of the findings may be limited by the sample being in the midrange of illness. Participants were chosen for the parent study this way as we hypothesized that relationships between psychosocial variables and health would be the strongest in that range. Another limitation is that this study did not address the relationship between increase in spirituality and quality of life. Significant correlations were found between INCRS, optimism, and hopelessness, suggesting that this might be a fruitful area for future research. Several of the other papers in this issue address the spirituality-quality of life relationship.
In conclusion, the relationship between an increase in spirituality/religiousness and slower disease progression is present and physicians should be aware of it. Given the potential health impact of change in spirituality/religiousness surrounding the diagnosis of HIV, both physicians, psychologists, social workers, and clergy ought to consider addressing religious/spiritual coping in their practice. In fact, some studies have suggested that many patients are comfortable with physicians discussing spirituality with them.31 How does one go about addressing this potentially sensitive issue? One way would be to ask a patient how they are coping with the diagnosis and HIV. A follow-up question may be whether the patient has religious or spiritual beliefs that are helping them to cope. A recent report by Kristeller et al.31 outlines a way in which physicians can bring this up that appears to be well accepted by patients. Readers may find additional material for assessing and managing religious and spiritual issues with patients in the March 2006 special issue of Psychiatric Annals,32 which is devoted entirely to this topic. In conclusion, these findings suggest a way that coping by turning to spirituality or religiousness may have health benefits.
Acknowledgments
This research was graciously supported by the Metanexus/Templeton Foundation, and by National Institute of Mental Health Grant (R01MH53791, and R01MH066697) Principal Investigator: Gail Ironson. Special thanks to Dr. Sol Katz and the Metanexus group for their support of the project, and to Brian Gonzalez for help with technical aspects of the manuscript.
REFERENCES
- 1.Powell LH, Shahabi L, Thoresen CE. Religion and spirituality linkages to physical health. Am Psychol. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 2.McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: a meta-analytic review. Health Psychol. 2000;19:211–22. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 3.Kirkpatrick L. Attachment, Evolution and the Psychology of Religion. New York: Guilford Press; 2005. [Google Scholar]
- 4.Leserman J, Petitto JM, Gu H, et al. Progression to AIDS, a clinical AIDS condition and mortality; psychosocial and physiological predictors. Psychol Med. 2002;32:1059–73. doi: 10.1017/s0033291702005949. [DOI] [PubMed] [Google Scholar]
- 5.Ironson G, O’Cleirigh C, Fletcher MA, et al. Psychosocial factors predict CD4 and viral load change in men and women in the era of HAART. Psychosomat Med. 2005;67:1013–21. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ironson G, Balbin E, Stuetzle R, et al. Dispositional optimism and the mechanisms by which it predicts slower disease progression in HIV: proactive behavior, avoidant coping, and depression. Int J Behav Med (Special Issue on Positive Psychology) 2005;12:86–97. doi: 10.1207/s15327558ijbm1202_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koenig HG. Psychoneuroimmunology and the faith factor. J Gender-Specific Med. 2000;3:37–44. [PubMed] [Google Scholar]
- 8.Ironson G, Solomon G, Balbin E, O’Cleirigh C, George A. The ironson-woods spirituality/religiousness index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Ann Behav Med. 2002;24:34–48. doi: 10.1207/S15324796ABM2401_05. [DOI] [PubMed] [Google Scholar]
- 9.Simoni JM, Ortiz MZ. Mediational models of spirituality and depressive symptomatology among HIV-positive Puerto Rican women. Cultural Diversity Ethnic Minority Psychol. 2003;9:3–15. doi: 10.1037/1099-9809.9.1.3. [DOI] [PubMed] [Google Scholar]
- 10.Chesney MA, Ickovics JR, Chambers DB, et al. Patient care committee & adherence working group of the adult aids clinical trials group. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. AIDS Care. 2000;12:255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 11.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 12.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–5. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 13.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implication of generalized outcome expectancies. Health Psychol. 1985;4:219–47. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 14.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery and self-esteem): a re-evaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–78. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 15.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–83. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 16.Ironson G, Friedman A, Klimas N, et al. Distress, denial, and low adherence to behavioral interventions predict faster disease progression in gay men infected with human immunodeficiency virus. Int J Behav Med. 1994;1:90–105. doi: 10.1207/s15327558ijbm0101_6. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell PH, Powell L, Blumenthal J, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD social support inventory. J Cardiopulm Rehab. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 19.Tsevat J, Sherman SN, McElwee JA, et al. The will to live among HIV-infected patients. Ann Intern Med. 1999;131:194–8. doi: 10.7326/0003-4819-131-3-199908030-00006. [DOI] [PubMed] [Google Scholar]
- 20.Jacobson CJ, Luckhaupt S, Delaney S, Tsevat J. Religio-biography, coping, and meaning-making among persons with HIV/AIDS. J Sci Stud Relig. 2006;45:39–56. [Google Scholar]
- 21.Ironson G, Kremer H, Ironson D. Spirituality, spiritual experiences, and spiritual transformations in the face of HIV. In: Koss-Chiono J, Hefner P, editors. Spiritual Transformation and Healing: Anthropological, Religious, Neuroscientific, and Clinical Perspectives. Walnut Creek, CA: Altamira Press; 2006. p. 241. [Google Scholar]
- 22.Cotton S, Tsevat J, Szaflarski M, et al. Religious and spiritual experiences of people with HIV. J Gen Intern Med. 2006;21:s5–13. [Google Scholar]
- 23.Schneiderman N, Ironson G, Siegel S. Stress and health: psychological, behavioral, and biological determinants. Ann Rev Clin Psychol. 2005:607–28. doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analysis of 30 years of inquiry. Psychol Bull. 2004;130:601–30. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole SW, Korin YD, Fahey JL, Zack JA. Norepinephrine accelerates HIV replication via protein kinase A-dependent effects on cytokine production. J Immunol. 1998;161:610–6. [PubMed] [Google Scholar]
- 26.Ironson G, Balbin E, Solomon G, et al. Relative preservation of natural killer cell cytotoxicity and number in healthy AIDS patients with low CD4 counts. AIDS. 2001;15:2065–73. doi: 10.1097/00002030-200111090-00001. [DOI] [PubMed] [Google Scholar]
- 27.Hill P, Pargament K. Advances in the conceptualization and measurement of religion and spirituality. Implications for physical and mental health research. Am Psychol. 2003;58:64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- 28.Woods TE, Ironson G. Religion and spirituality in the face of illness: how cancer, cardiac, and HIV patients describe their spirituality/religiosity. J Health Psychol. 1999;4:393–412. doi: 10.1177/135910539900400308. [DOI] [PubMed] [Google Scholar]
- 29.Pargament KI, Koenig HG, Perez L. The many methods of religious coping: development and validation of the RCOPE. J Clini Psychol. 2000;56:519–43. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 30.Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients: a two year longitudinal study. Arch Intern Med. 2001;161:1881–5. doi: 10.1001/archinte.161.15.1881. [DOI] [PubMed] [Google Scholar]
- 31.Kristeller JL, Rhodes M, Cripe LD, Sheets V. Oncologist assisted spiritual intervention study (OASIS): patient acceptability and initial evidence of effects. Int J Psychiatr Med. 2005;35:329–47. doi: 10.2190/8AE4-F01C-60M0-85C8. [DOI] [PubMed] [Google Scholar]
- 32.Psychiatric Annals. Special Issue: Spirituality in Psychiatric Practice: Guidelines for assessing and managing religious and spiritual issues. March 2006. pp. 137–204.