Abstract
Background
There is a growing concern surrounding crystal methamphetamine use in Canada despite surprisingly little empirical data to support such claims. We evaluated the trends in crystal methamphetamine injection and factors associated with injection of the drug among a cohort of injection drug users (IDU) in Vancouver.
Methods
We conducted a prospective analysis of factors associated with crystal methamphetamine injection among participants enrolled in the Vancouver Injection Drug Users Study (VIDUS). Since serial measures for each individual were available, variables potentially associated with crystal methamphetamine injection were evaluated using generalized estimating equations (GEE) with logit link for binary outcomes.
Results
Overall, 1587 IDU were enrolled into the VIDUS cohort between May 1996 and December 2004. The proportion of IDU who reported injecting crystal methamphetamine during the last six months increased during the study period (Cochran-Armitage trend test, p < 0.001). In multivariate GEE analyses, crystal methamphetamine injection was independently associated with younger age (Adjusted Odds Ratio [AOR]: 4.77, 95% Confidence Interval [CI] = 3.40 - 6.70), Caucasian ethnicity (AOR = 2.21, 95% CI = 1.57 - 3.12), syringe borrowing (AOR = 1.62, 95% CI = 1.22 - 2.13), and syringe lending (AOR = 1.40, 95% CI = 1.02 - 1.86).
Interpretation
There was a significant trend towards increasing crystal methamphetamine injection in this setting and elevated HIV risk behavior and younger age were independently associated with crystal methamphetamine injection. Given that banning precursor chemicals has had a limited effect on reducing methamphetamine supply in other jurisdictions, pragmatic and effective interventions are needed to address the growing use of this drug.
Keywords: HIV transmission , Injection drug use , Crystal methamphetamine
1. Introduction
Crystal methamphetamine use in Canada has received considerable media attention in recent years as the source of significant health, social, and economic harms for users of the drug and their communities (Lee, 2005; Mills, 2005). High rates of crystal methamphetamine use in Canada among certain groups, particularly street youth, gay and bisexual youth, and rave attendees, suggest growing popularity of the drug (Martin et al., 2006; Lampinen et al., 2006; Barrett et al., 2005; Gross et al., 2002). In British Columbia, crystal methamphetamine-related deaths have increased from 3 in 2000 to 33 in 2004, most commonly as a result of overdose or motor vehicle accidents (BC Coroners Service, 2005).
In August 2005, the federal government responded to this ‘epidemic’ by amending laws and assigning the harshest penalties available for the producers and distributors of any drug, thereby placing crystal methamphetamine in the ranks of cocaine and heroin (Cryderman, 2005; Mills, 2005; Canada Gazette, 2005). Restrictions on the purchase of precursor ingredients, which may be obtained from local pharmacies, have also been recently implemented to discourage the development and operation of clandestine crystal methamphetamine laboratories (Mills, 2005; Canada Gazette, 2005).
Despite the extensive media attention and legal changes that have been made to address the growing problem of crystal methamphetamine use in Canada, surprisingly little research has been conducted to assess purported increase in use of the drug. Of special importance is the lack of data on the prevalence of crystal methamphetamine injection despite the potential implications for transmission of HIV and other blood-borne diseases. Given the growing concern surrounding crystal methamphetamine use and the paucity of research on the topic, we sought to investigate trends in crystal methamphetamine injection and factors associated with crystal methamphetamine injection among a cohort of injection drug users in Vancouver.
2. Methods
2.1 Participant recruitment
Beginning in May 1996, persons who had reported injecting illegal drugs in the previous month were recruited into the Vancouver Injection Drug User Study (VIDUS), a prospective cohort study that has been described in detail previously (Tyndall et al., 2003; Wood et al., 2001; Miller et al., 2002). Briefly, persons were eligible for VIDUS if they had injected illegal drugs at least once in the previous month, resided in the greater Vancouver region, and provided written informed consent. At baseline and semi-annually, participants provide blood samples and complete an interviewer-administered questionnaire. Participants receive Can$20 for each study visit. The questionnaire elicits demographic data as well as information about drug use, HIV risk behavior, and drug treatment. The study is approved on an annual basis by the University of British Columbia Research Ethics Board.
2.2 Variables of Interest
The primary endpoint in this analysis was self-reported crystal methamphetamine injection. Explanatory variables of interest in this analysis included socio-demographic information: gender, age (< 24 vs ≥ 24), and ethnicity (Caucasian yes/no). Drug use variables considered included: borrowing and lending used syringes, daily heroin and cocaine injection, and daily crack cocaine smoking. Other risk characteristics considered included: sex trade involvement, residence in the Downtown Eastside (i.e., Vancouver's illegal drug use and HIV epicenter), and condom use with regular and casual sex partners. All behaviors referred to activities in the six months prior to interview and variable definitions were identical to earlier reports (Tyndall et al., 2003; Miller et al., 2002; Wood et al., 2002).
2.3 Statistical Methods
Since analyses of factors associated with crystal methamphetamine injection included serial measures for each subject, we used generalized estimating equations (GEE) for binary outcomes with logit link for the analysis of correlated data to determine which factors were independently associated with crystal methamphetamine injection (Diggle et al., 1996). These methods provided standard errors adjusted by multiple follow-ups per person using an exchangeable correlation structure (Diggle et al., 1996). We also tested for potential changes in methamphetamine use over time using the Cochran-Armitage test for trend.
The multivariate model was fit using an a priori defined model building protocol involving adjustment for all variables at p < 0.05 in bivariate analyses. All statistical analyses were performed using SAS software version 8.0 (SAS, Cary, NC). All p-values are two sided.
3. Results
Overall, 1587 IDU were enrolled into the VIDUS cohort between May 1996 and December 2004. Of these individuals, 1381 (87%) had at least one follow-up visit, and 259 (16.3%) have died since enrolment. These participants contributed to 13,623 observations during the follow-up period. The mean number of follow-up visits was 8.62, and the median number of follow-up visits was 9 (Inter-quartile range 4–13). The median age of the cohort at baseline was 33 years and HIV prevalence of the cohort is 28.8%. The proportion of Caucasian individuals was 58.9%, the proportion of individuals of Aboriginal descent was 26.8%, and the proportion of females was 36.3%.
The crude proportion of individuals in the VIDUS cohort who reported injecting crystal methamphetamine in the six months prior to their interview for each year during the period between 1997 and 2004 is shown in Figure 1. The proportion of individuals who reported injecting crystal methamphetamine in the previous six months increased, from 2.5% in 1997 to 6.7% in 2004 (Cochran-Armitage trend test p < 0.001). In 1996, the proportion reporting crystal methamphetamine injection was 4.8%, but data from 1996 were excluded from the figure since data for the entire year were unavailable since the cohort began enrollment in May 1996.
Figure 1.
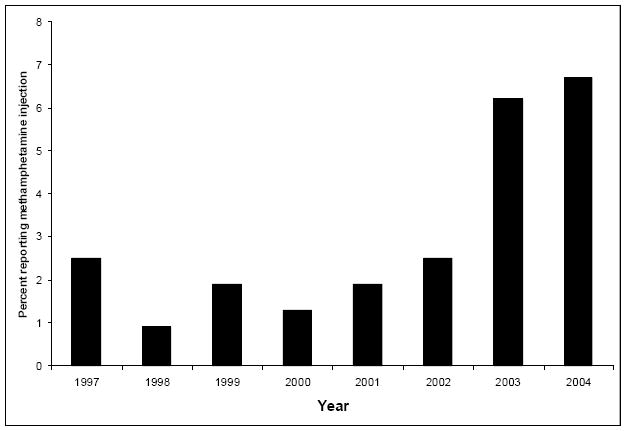
The crude proportion of individuals reporting crystal methamphetamine injection during the six months prior to the interview for each year between 1997 and 2004.
Table 1 shows the results of the bivariate and multivariate GEE analysis of factors associated with crystal methamphetamine injection. In bivariate GEE logistic analyses, crystal methamphetamine injection was significantly associated with: being 24 years old or younger (odds ratio [OR] = 5.10), Caucasian ethnicity (OR = 2.16), sex trade involvement (OR = 1.73), daily cocaine injection (OR = 1.26), daily heroin injection (OR = 1.40), daily crack use (OR = 1.32), borrowing syringes (OR = 2.04) and lending syringes (OR = 1.93). Gender, DTES residence, and condom use with regular and casual sex partners were not significantly associated with crystal methamphetamine injection.
Table 1.
Bivariate and multivariate GEE* of factors associated with crystal methamphetamine injection (n = 1587)
| Characteristic | Unadjusted Odds Ratio | (95% C.I.) | Adjusted Odds Ratio | (95% C.I.) |
|---|---|---|---|---|
| Age* | ||||
| ≥ 24 | ||||
| ≤ 24 | 5.10 | (3.71 – 7.04) | 4.77 | (3.40 – 6.70) |
| Gender | ||||
| Female | ||||
| Male | 0.84 | (0.60 – 1.17) | ||
| DTES Residence | ||||
| No | ||||
| Yes | 1.03 | (0.85 – 1.26) | ||
| Condom Use- | ||||
| Regular Sex Partner | ||||
| No | ||||
| Yes | 0.97 | (0.78 – 1.21) | ||
| Condom Use- | ||||
| Casual Sex Partner | ||||
| No | ||||
| Yes | 0.92 | (0.76 – 1.10) | ||
| Caucasian* | ||||
| No | ||||
| Yes | 2.16 | (1.54 – 3.04) | 2.21 | (1.57 – 3.12) |
| Sex Trade | ||||
| No | ||||
| Yes | 1.73 | (1.38 – 2.18) | 1.28 | (0.97 – 1.68) |
| Cocaine Use | ||||
| < Daily | ||||
| ≥ Daily | 1.26 | (1.05 – 1.52) | 1.19 | (0.94 – 1.50) |
| Heroin Use | ||||
| < Daily | ||||
| ≥ Daily | 1.40 | (1.15 – 1.69) | 1.03 | (0.82 – 1.29) |
| Crack Use* | ||||
| < Daily | ||||
| ≥ Daily | 1.32 | (1.08 – 1.61) | 1.33 | (1.04 – 1.69) |
| Syringe Borrowing | ||||
| No | ||||
| Yes | 2.04 | (1.64 – 2.53) | 1.61 | (1.22 – 2.13) |
| Syringe Lending* | ||||
| No | ||||
| Yes | 1.93 | (1.52 – 2.43) | 1.38 | (1.02 – 1.86) |
GEE = Generalized Estimating Equation, C.I. = Confidence Interval. Variables shown in the multivariate model above were adjusted for DTES residence, gender, sex-trade involvement, daily cocaine use, and daily heroin use.
Indicates variable remained p < 0.05 in the final
The multivariate GEE analysis included all variables that were statistically significant in bivariate analyses at p < 0.05. As shown here, being 24 years of age or younger (adjusted odds ratio [AOR] = 4.77), Caucasian ethnicity (AOR = 2.21), frequent crack use (AOR = 1.30), syringe borrowing (AOR = 1.62), and syringe lending (AOR = 1.40) were independently associated with crystal methamphetamine injection during follow-up. Sex trade involvement, daily cocaine use, and daily heroin use were not associated with crystal methamphetamine injection in multivariate analyses.
4. Discussion
We found a significant trend towards increasing crystal methamphetamine injection among a cohort of IDU in Vancouver. Alarmingly, injection of methamphetamine was significantly associated with younger age, and both distributive and receptive syringe sharing. Our findings are consistent with anecdotal and media reports of increasing crystal methamphetamine use in Canada, particularly among youth, although the increase observed among this IDU population is not as dramatic as has been suggested for crystal methamphetamine use among non-injectors. Although there is evidence from the U.S. indicating that use of this drug has rapidly increased in recent years, spreading eastward from western and southwestern regions of the country (Yacoubian and Peters, 2004; Anglin et al., 2000; Glittenberg & Anderson, 1999), these data regarding injection of crystal methamphetamine are novel to our knowledge.
This study is the first to demonstrate an independent association between syringe sharing and crystal methamphetamine injection and indicates that individuals who inject this drug may be at increased risk for contracting HIV and other blood-borne infections. There is evidence to support a link between crystal methamphetamine use and HIV sexual risk behaviours among men who have sex with men (MSM) (Patterson et al., 2005; Semple et al., 2004). However, our findings pertaining to drug-related HIV-risk behaviours indicate that injection-related risk practices may represent another important mode of HIV transmission among crystal methamphetamine users. Given that crystal methamphetamine production is a highly profitable and easily concealable endeavor, and demand for the drug is increasing, legal remedies and law enforcement may have a negligible impact on use. Indeed, enforcement activities have had a limited impact on the supply of illegal substances imported from South East Asia and Central America (Wood et al., 2003). With respect to the banning of precursor chemicals, similar bans have been in place in the U.S. since 1996 and, though temporary disruptions to methamphetamine drug markets have been observed, use of methamphetamine has nevertheless grown unabated (Cunningham & Liu, 2005; Cunningham & Liu, 2003; Reuter, 2003). Therefore, there is an urgent need for evidence-based HIV prevention and drug treatment programs for crystal methamphetamine injectors in order to minimize the harms associated with use of this drug (Reuter, 2003; Kerr et al., 2005).
Our study has limitations. First, as with most other cohort studies of IDU, VIDUS is not a random sample and cannot be presumed to be wholly representative of injecting drug users in the population. Moreover, we speculate that the observed findings from this sample might generalize elsewhere, but this speculation must be evaluated in light of results of future similar studies on this topic. Second, while some studies have suggested that self-reports of IDU are valid (Drake, 1998), syringe sharing is a stigmatized behaviour and it is therefore likely that syringe borrowing rates were under-estimated in the present study (Des Jarlais et al., 1999). Nevertheless, we know of no reason why this concern would be differentially distributed between methamphetamine users and non-users.
In summary, we found a significant trend of increasing crystal methamphetamine injection among IDU in Vancouver. Crystal methamphetamine injection was independently associated with syringe sharing, indicating the potential for increased HIV transmission as popularity of this drug increases. Since changing the penalties for methamphetamine production and the banning of precursor chemicals are likely to have a negligible impact on the use of this drug (Cunningham & Liu, 2005; Cunningham & Liu, 2003; Reuter, 2003), evidence-based interventions are urgently needed to address the severe potential harms for individuals who inject crystal methamphetamine.
Acknowledgments
We would particularly like to thank the VIDUS participants for their willingness to participate in the study. We also thank Drs. Kevin Craib, Richard Harrigan, David Patrick, Martin Schechter, Patricia Spittal, and Mr. Will Small for their research assistance, and John Charette, Caitlin Johnston, Cody Callon, Vanessa Volkommer, Steve Kain, Kathy Churchill, Dave Isham, Nancy Laliberte, Sue Currie, Bonnie Devlin, and Peter Vann for their administrative assistance. The study was supported by the US National Institutes of Health (grant no. RO1 DAO11591-04A1) and the Canadian Institutes of Health Research (MOP-67262).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anglin MD, Burke C, Perrochet B, Stamper E, Dawud-Noursi S. History of the methamphetamine problem. J Psychoactive Drugs. 2000;32(2):137–41. doi: 10.1080/02791072.2000.10400221. [DOI] [PubMed] [Google Scholar]
- Barrett SP, Gross SR, Garand I, Pihl RO. Patterns of simultaneous polysubstance use in Canadian rave attendees. Subst Use Misuse. 2005;40:1525–37. doi: 10.1081/JA-200066866. [DOI] [PubMed] [Google Scholar]
- Cunningham JK, Liu L. Impacts of federal precursor chemical regulations on methamphetamine arrests. Addiction. 2005;100:479–488. doi: 10.1111/j.1360-0443.2005.01032.x. [DOI] [PubMed] [Google Scholar]
- Cunningham JK, Liu L. Impacts of federal ephedrine and pseudoephedrine regulations on methamphetamine-related hospital admissions. Addiction. 2003;98:1129–1137. doi: 10.1046/j.1360-0443.2003.00450.x. [DOI] [PubMed] [Google Scholar]
- Deaths with Methamphetamine Present-2000-2004. Vancouver: BC Coroners Service; 2005. Available from: http://www.pssg.gov.bc.ca/coroners/statistics/pdfs/METHAMPHETAMINE_DEATHS_IN_BC.pdf. [Google Scholar]
- DC Des Jarlais, D Paone, J Milliken, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomized trial. Lancet. 1999;353(9165):1657–61. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Liang K, Zeger S. Analysis of longitudinal data. New York, NY: Oxford University Press; 1996. [Google Scholar]
- Drake S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–63. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Glittenberg J, Anderson C. Methamphetamines: use and trafficking in the Tucson-Nogales area. Subst Use Misuse. 1999;34(14):1977–89. doi: 10.3109/10826089909039435. [DOI] [PubMed] [Google Scholar]
- Gordon J. The Gazette; 2006. Jul 11, Crystal meth use soars to new high: Seizure of synthetic drugs on rise; p. A10. [Google Scholar]
- Gross SR, Barrett SP, Shestowsky JS, Pihl RO. Ecstasy and drug consumption patterns: A Canadian rave population study. Can J Psychiatry. 2002;47:546–51. doi: 10.1177/070674370204700606. [DOI] [PubMed] [Google Scholar]
- Kerr T, Wood E, Grafstein E, Ishida T, Shannon K, Lai C, Montaner J, Tyndall MW. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health (Oxf) 2005;27(1):62–6. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- Lampinen TM, McGhee D, Martin I. Increased use of “club” drug use among gay and bisexual high school students in British Columbia. J Adolesc Health. 2006;38(4):458–61. doi: 10.1016/j.jadohealth.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Lee J. Crystal meth ‘a massive problem’. The Vancouver Sun. 2005 Sep 29;:A.4. [Google Scholar]
- Martin I, Lampinen TM, McGhee D. Methamphetamine use among marginalized youth in British Columbia. Can J of Public Health. 2006;07(4):320–4. doi: 10.1007/BF03405613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CL, Johnston C, Spittal PM, Li K, Laliberte N, Montaner JS, Schechter MT. Opportunities for prevention: Hepatitis C prevalence and incidence in a cohort of young injection drug users. Hepatology. 2002;36(3):737–42. doi: 10.1053/jhep.2002.35065. [DOI] [PubMed] [Google Scholar]
- Mills A. Ottawa toughens laws on crystal meth; Sentences lengthened for possession, trafficking of drug substance abuse experts warn that move won't deter use. Toronto Star. 2005 Aug 12;:A.06. [Google Scholar]
- Order Amending Schedule I to the Controlled Drugs and Substances Act. 24. Vol. 139. Canada Gazette; 2005. Nov 30, Available at: http://canadagazette.gc.ca/partII/2005/20051130/html/sor337-e.html. [Google Scholar]
- Patterson TL, Semple SJ, Zians JK, Strathdee S. Methamphetamine-using HIV-positive men who have sex with men: Correlates of polydrug use. Journal of Urban Health. 2005;82(N1 S1):120–126. doi: 10.1093/jurban/jti031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter P. Does precursor regulation make a difference? Addiction. 2003;98:1177–1179. doi: 10.1046/j.1360-0443.2003.00483.x. [DOI] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. A comparison of injection and non-injection methamphetamine-using HIV positive men who have sex with men. Drug & Alcohol Dependence. 2004;76:203–212. doi: 10.1016/j.drugalcdep.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Tyndall MW, Currie S, Spittal P, Li K, Wood E, O'Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17(6):887–93. doi: 10.1097/00002030-200304110-00014. [DOI] [PubMed] [Google Scholar]
- Wood E, Tyndall MW, Spittal PM, Li K, Anis AH, Hogg RS, Montaner JS, O'Shaughnessy MV, Schechter MT. Impact of supply-side policies for control of illicit drugs in the face of the AIDS and overdose epidemics: investigation of a massive heroin seizure. CMAJ. 2003;168(2):165–9. [PMC free article] [PubMed] [Google Scholar]
- Wood E, Tyndall MW, Spittal PM, Li K, Hogg RS, Montaner JS, O'Shaughnessy MV, Schechter MT. Factors associated with persistent high-risk syringe sharing in the presence of an established needle exchange programme. AIDS. 2002;16(6):941–3. doi: 10.1097/00002030-200204120-00021. [DOI] [PubMed] [Google Scholar]
- Wood E, Tyndall MW, Spittal PM, Li K, Kerr T, Hogg RS, Montaner JS, O'Shaughnessy MV, Schechter MT. Unsafe injection practices in a cohort of injection drug users in Vancouver: could safer injecting rooms help? CMAJ. 2001;165(4):405–10. [PMC free article] [PubMed] [Google Scholar]
- Yacoubian GS, Peters RJ. Exploring the prevalence and correlates of methamphetamine use: Findings from Sacramento's ADAM program. J Drug Education. 2004;34(3):281–294. doi: 10.2190/QBHY-ADHA-MYMW-HCMR. [DOI] [PubMed] [Google Scholar]


