Abstract
Background
Extensive research in developed countries has established that very low birth weight (VLBW) infants are particularly vulnerable to the effects of early nutritional deficiencies. There is, however, little information from poor countries on the long-term effects of these deficiencies in such infants.
Objective
Determine the association between neonatal feeding regimens and post-discharge morbidity/ mortality and neurological abnormalities at the age of two years for a cohort of VLBW infants.
Design
Prospective Cohort.
Methods
One hundred and seventy five VLBW infants were recruited over a consecutive period of one year and followed up to the age of two years corrected for gestation. With neonatal feeding regimes as the exposure variable, post-discharge re-hospitalization, mortality and Saigal and Rosenbaum's functional disability assessment scores were compared as the outcome variables.
Results
The 175 infants recruited into the study had median birth weight of 1400±103 grams and gestation 32 ±2.3 weeks. The male: female ratio was 2:3 while 64 (36.6%) had been born intrauterine growth retarded. During the newborn period, 83(47.4%), 35 (20.0%) and 57 (32.6%) of the infants fed on exclusive breast milk, pre-term formula and mixed preparations respectively. The median neonatal weight gain was 17 ±2.5, 15 ±2.0 and 13 ±3.9 grams/kilo/day for preterm formula, combined and exclusive breast milk fed infants respectively. More of the infants fed on breast milk alone were re-hospitalized compared to those on pre-term formula, RR 2.3; 95%CI 1.4–3.6 or mixed milk preparations, RR 1.9; 95% CI 1.4–2.7. Infants exclusively fed on breast milk had more neurological disabilities than those on pre-term formula alone, RR 3.2; 95% CI 1.2–8.1. Though only 22.9% of pre-term milk fed infants died compared to 36.1% of those on breast milk alone the difference was not statistically significant, P>0.05.
Conclusion
Nutritionally enhanced enteral feeds during the first month of life appear to have reduced post-discharge morbidity and improved neurological outcomes at two years in VLBW infants.
Keywords: early nutrition, very low birth weight
Introduction
The World Health Organization (WHO) recommends Mothers' milk alone during the first six months of life 1. Research in industrialized countries has established that Very Low Birth Weight (VLBW) infants require higher nutritional density than is available in unmodified mothers' milk if they are to achieve the recommended growth during the first month of life2,3. Lucas and colleagues2 in a large multi-center randomized trial reported that infants fed on Preterm Formula (PTF) grew significantly better than those fed on breast milk (BM) alone or in combination with PTF. Brooke et al 3, qlso comparing early growth in VLBW infants fed on different feeding regimes reported PTF as superior to either BM alone or in combination with PTF. The early 1990s witnessed the introduction of breast milk fortifies (BMF) for VLBW infants (4) with clinical trials quickly establishing that such preparations achieved physical growth similar to that of PTF5.
Adequate nutrition resulting in normal growth is particularly important in VLBW infants in whom subnormal growth during early infancy has been associated with reduced cognitive and physical development when such infants are evaluated later6–9. Studies in animals10–12 and humans13,14 have established that there are periods in early life when organisms are particularly vulnerable to irreversible damage due to exposure to extraneous factors like nutritional deficiency. In VLBW infants this period includes the first month of life.
Lucas and colleagues found that VLBW infants fed on enriched milk during the first month of life not only grew faster during that period15, they also performed better in neuro-development scores during the subsequent years8,9, 16. These multi-center trials demonstrated that the first month is indeed a vulnerable period for VLBW infants. It is therefore apparent that in regard to VLBW infants the WHO feeding strategy should include a rider stating that “breast milk fortification during the first month of life”. It is with this background, that the present study was conceived to investigate the effects of the neonatal feeding regimens used at the center on subsequent morbidity, mortality and neurological development.
Methods
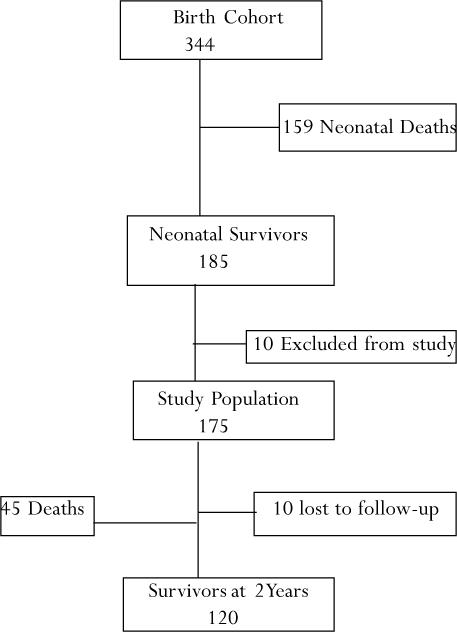
Out of a cohort of 344 infants weighing 1500grams or less and admitted to the newborn unit during the year 2002, 185 survived the newborn period. The 344 were the entire population of VLBW infants admitted to the newborn unit of Kenyatta National Hospital, the national referral and teaching facility for the University of Nairobi's College of Health Sciences.
Ten of the 185 Infants who survived the neonatal period were excluded due to clinically overt structural congenital anomalies (three), refusal of consent (two) and positive laboratory diagnosis of maternal human immunodeficiency viral infection (five). One hundred and seventy five were therefore consecutively recruited for this two-year follow-up, which continued through to March 2006.
By the time the study was concluded, 10 more had defaulted while 45 had died. The recruitment into follow up was done at the age of 28–30days. The birth and 28–30 day anthropometric measurements were recorded as well as details of their neonatal feeding regimes. The gestation, assessed using menstrual history and confirmed by Ballard's (17) clinical scoring method was also recorded.
Neonatal Feeding
The exposure variable for this study was the type of milk fed to the infants during the first month of life. The infants were fed every three hours with pre-calculated volumes of milk based on the day's requirements. The total volume given daily ranged from 80–240 milliliters/kilo/day depending on the postnatal age and individual infant's tolerance. The feeds were recorded on charts which captured the amount and type of milk given at each feed. This allowed for the specific identification of the predominant milk used during the first month of life.
The hospital policy allowed the use of one of three possible milk regimes; exclusive breast milk , mixed feeds and pre-term formula. The formula on the hospital formulary at the time of the study was Pre Nan from Nestle Foods Kenya. A mixed feed was defined as that containing at least 1/3 pre-term formula. Expressed breast milk was the preferred feed with formula only given to bridge the gap when mothers' milk was not adequate for the infants' needs. The infants in the exclusive PTF group belonged to mothers who could not provide at least one third of the required milk throughout the neonatal period. The investigators did not influence in any way the type or amount of milk the infants consumed or indeed any other aspect of neonatal care. No randomization of infants into feeding regimes was done nor would it have been allowed ethically.
Medical care
The infants received the routine neonatal care according to the protocols of the hospital. There was no interference by the investigators in the care prescribed by the primary physicians. They also received the standard oral vitamin and Iron supplements. These were administered from the ages of two and eight weeks respectively. No infant was given any form of parenteral nutrition.
Follow-up
The infants were seen monthly for the first three months after discharge then three monthly thereafter until they reached two years corrected for gestation. All the infants received the required primary care from the principal investigator in addition to the research reviews at each visit. Re-hospitalization was defined as any episode of hospital care lasting more than 24 continuous hours. Information on re-hospitalization was confirmed on medical records carried by the mother/guardian whenever possible. Recall was used in the absence of hospital records. The information regarding death was obtained either by self-reporting or home visits whenever patients missed an appointment. Cell phone tracing was employed when home visits failed. At the gestation adjusted age of two years, neurological assessments were performed on the 120 surviving infants. Two independent practitioners performed the examinations with 96.7% agreement. The four subjects with different scores had their evaluation repeated by the two assessors together and an agreed result determined.
Sample Size
The study sample was the total population of all the VLBW neonatal survivors available for the two year follow-up. They came from the 2002 birth cohort of VLBW infants admitted at the Kenyatta National Hospital. There was therefore no predetermined sample size.
Study Population Profiles
Loss to follow-up was declared upon failure to attend a scheduled appointment with subsequent inability to find the subject after home visits or telephone calls to patients or other known relative.
Neurological evaluation
The Saigal and Rosenbaum's (18) method was used in the assessment of functional disability. This tool incorporates both cognitive and physical developmental skills in its observations. It measures a child's ability to perform appropriately in the Ordinary Activities and Skills of Daily Living (OASDL) for his or her gestation corrected age. The skills tested are ambulation, feeding and active play. The assessment categorizes the children into normal, mild, moderate and severe (major) dysfunction groups.
The results are interpreted as follows;
Normal: A child able to perform appropriately in OASDL for his or her gestation corrected age. No additional care taking burden. A two-year old child should be able to walk steadily, feed him or herself and undertake ambulatory play.
Mild dysfunction: A child who was able to perform appropriately in OASDL for corrected age despite developmental or structural abnormalities. These were children who performed normally but had identifiable physical or cognitive anomalies.
Moderate dysfunction: A child who required some additional adult care taking or help in OASDL beyond what is normally expected for the gestation corrected age. This was the group of children who were not able to walk steadily, required help when feeding and were sluggish on ambulatory playing
Major dysfunction: A child who required constant additional adult care or help in OASDL. This group consisted of children who were unable to walk without support, feed themselves or undertake ambulatory play.
Analysis
Using the Statistical Package for Social Sciences software, growth parameters were summarized as medians and comparisons made by Analysis of Variance or comparison of means. Categorical variables were compared on the EPINFO version 6 program using the chi-square distribution test and reported as Relative Risk (RR) and 95% Confidence Interval (CI) statistics.
Ethics
The hospital's ethics and standards committee approved the study. For each patient, the parent/guardian gave written consent for participation in the study after detailed explanation from the investigating team.
Results
Of the 175 initially recruited, 10 were lost to follow-up (default rate of 5%) while 45 were reported to have died.
The baseline characteristics for the 175 recruited infants
The baseline characteristics of the population are presented in table 1. The median birth weight was 1400±103g and gestation of 32 2.3weeks. The male : female ratio was 2:3 while 36.6% of them had suffered intrauterine growth retardation (IUGR). The most frequently employed neonatal feeding regimen was exclusive breast milk at 47.4% followed by mixed feeds at 32.6%. Only 20% of the infants were exclusively formula milk fed.
Table 1.
Baseline Population Characteristics
| Baseline characteristics | Observation | |
| Median±SD of birth weight in grams | 1400 ±103 | |
| Median±SD of gestation in weeks | 32 ± 2.3 | |
| Infant Gender; N (%) | 70 (40.0) | |
| Male | 105 (60.0) | |
| Female | ||
| Intrauterine growth; N (%) | ||
| IUGR1 | 64 (36.6) | |
| AGA2 | 111 (64.4) | |
| Neonatal Feeds; N (%) | ||
| Pre-term Formula | 35 (20.0) | |
| Mixed Feeds | 57 (32.6) | |
| Breast Milk | 83 (47.4) | |
IUGR= Intrauterine Growth Retardation,
AGA=Appropriate for Gestational Age
Table 2 shows a comparison of the baseline characteristics between the three feeding regimens in the study. No differences were found in, birth weight, gestation, sex ratio and IUGR rates. In neonatal weight gain however, there were statistically significant differences with infants fed on PTF displaying faster neonatal growth.
Table 2.
Comparative analysis of baseline Characteristics
| Baseline | Feeding regimen | |||
| Characteristics | Pre-term formula | Mixed feed | Breast milk | P value |
| Median±SD of birth weight in grams | 1420± 59 | 1400±95 | 1430±126 | 0.78* |
| Median±SD of gestation in weeks | 32.0±1.2 | 32.01.7 | 32.0±2.5 | 0.87* |
| Gender (% of Males) | 40.0 | 40.4 | 39.8 | 0.90# |
| Intrauterine Growth | 34.3 | 35.1 | 37.3 | 0.76# |
| SGA1 rate (%) | ||||
| Median±SD neonatal weight gain; g/kg/day | 17±2.5 | 15±2.0 | 12±3.9 | 0.001* |
Analysis of Variance,
Chi Square Test,
SGA
Post-discharge Re-hospitalization
The proportions of infants re-admitted to hospital were compared with the neonatal feeding regimes as the exposure variables. All the 175 infants recruited were included in this analysis employing the intention to treat method. Table 3 shows that the re-hospitalization rates were 34.3, 40.4 and 77.1% for the PTF, MF and BM alone groups respectively. Infants fed on BM alone were more likely to be re-hospitalized compared to those who received MF feeds or exclusive PTF. The statistical validation of these differences is included in the table.
Table 3.
Neonatal feeding and re-hospitalization
| N (%) | Statistics | |
| Feeding regimen | Re-hospitalized | RR*, 95% CI |
| Pre-term Formula; N=35 | 12 (34.3) | 1.0 |
| Mixed Feeds; N=57 | 23 (40.4) | 1.1 0.7–2.1 |
| Breast Milk; N=83 | 64 (77.1) | 2.3 1.4–3.6 |
| Mixed Feeds; N=57 | 23 (40.4) | 1.0 |
| Breast Milk; n=83 | 83 (77.1) | 1.9 1.4–2.7 |
Statistics by Chi square test.
RR=relative risk
Post-Discharge Mortality
The mortality among the three neonatal feeding regimens is presented in table 4. Intention to treat analysis was used in this variable as well.
Table 4.
Neonatal feeding and post-discharge mortality
| Feeding regiment | N (%) | Statistics |
| Who died | RR*, 95%CI | |
| Pre-term Formula; N=35 | 8 (22.9) | 1.0 |
| Mixed Feeds; N=57 | 17 (31.5) | 1.3 0.6–2.7 |
| Breast Milk; N=83 | 30 (36.1) | 1.6 0.8–3.1 |
| Mixed Feeds; N=57 | 17 (31.5) | 1.0 |
| Breast Milk; N=83 | 30 (36.1) | 1.2 0.7–2.0 |
Statistics by Chi square test.
RR=relative risk
Infants fed on BM alone had the highest post-discharge mortality, 36.1% followed by the MF group, 31.5%. The exclusively PTF fed group had the lowest mortality at 22.9%. These differences were, however, not statistically significant.
Functional Disability
Functional disability was compared between the three feeding groups as presented in table 5. This analysis involved only the 120 survivors at two years. The relative risk of developing functional disabilities for infants fed on BM alone compared to PTF was 3.2. Very Low Birth Weight infants predominantly fed on nutrient enriched milk during the first month of life had significantly better functional development in this cohort.
Table 5.
Neonatal feeding and functional disability
| Feeding regimen | N (%) | Statistics |
| Re-hospitalized | RR*, 95%CI | |
| Pre-term Formula; N=28 | 4 (14.3) | 1.0 |
| Mixed Feeds; N=41 | 11 (26.8) | 1.9 0.7–5.3 |
| Breast Milk; N=60 | 27 (45.0) | 3.2 1.2–8.1 |
| Mixed Feeds; N=41 | 11 (26.8) | 1.0 |
| Breast Milk; N=60 | 27 (45.0) | 1.7 0.9 –3.0 |
Fisher's exact test.
Chi square test
RR=relative risk
Discussion
The World Health Organization's infant feeding policy, adopted by most developing countries, has no birth weight stratification (1). As long as it is available, breast milk is exclusively recommended for all infants during the first six months of life. Nutrient enriched milk preparations are seldom available to such communities. The findings of the present study indicate that in order to apply this strategy to VLBW infants, the breast milk may need to be enriched to provide the additional nutrition required by such infants.
The infants whose neonatal diets consisted of BM alone grew at a slower rate than those on PTF or MF in this cohort. In this cohort, infants predominantly fed on BM had a median neonatal weight gain of 12g/kg/day, five grams lower than those fed on PTF. This was also below the expected minimum of 15g/kg/day recommended by established research19–21. This may have been due to the fact that the BM being un-fortified did not have nutritional density commensurate with the needs of VLBW infants. Previous studies have confirmed that VLBW infants need enriched milk during the first month of life if they have to achieve the desired growth 2, 3.
Brooke and colleagues (3) reported that infants fed on PTF grew at a mean weight of 21.5±5.2 g/kg/d, while the ones on BM alone grew at a significantly slower rate of 15.6± 5.4. Lucas and colleagues2 in a large randomized multi-centre trial reported neonatal weight gains of 18 and 12g/kg/day in VLBW infants fed on PTF and BM alone respectively. In both studies infants on combined BM and PTF grew at rates somewhere between these extremes. The findings of the present study are thus in agreement with previous reports. Very low birth weight infants with such slow neonatal weight may be at high risk to subsequent development of neurological disabilities.
Indeed, in this cohort, infants fed on BM alone during the neonatal period had more neurological disabilities than those fed on exclusive PTF who had grown significantly faster during the newborn period (RR 3.2; 1.2–8.1). The findings of this cohort are consistent with those reported by Lucas8 who also compared PTF and un-fortified BM in terms of their subsequent neurological development. It is, nevertheless, known that when VLBW infants are fed on enriched mothers' milk, their subsequent developmental are better than even those fed on PTF. Lucas and colleagues16 reposted significantly better cognitive scores at eight years among infants who had used breast milk during the first month of life. It is therefore likely that the significantly poorer growth observed among the infants on exclusive breast milk in the present cohort was the predominant causative factor in the increased occurrence of neurological disabilities observed. The established advantages of breast milk on brain development may not be fully realized if adequate growth does not occur. A systematic review of several studies by Smart confirms the latter observation 11. This prospective cohort therefore adds to the body of information regarding the association between adequate neonatal nutrition and later neurological development in VLBW infants.
The re-hospitalization rate for infants fed on beast milk alone was significantly higher than either of the other two feeding categories. Nutrient enrichment of the diets during the first month of life thus appeared to improve subsequent health. This suggests that better nourished infants suffered less morbidity and were less likely to be hospitalized after the initial discharge. Though the results do not provide direct evidence for this, the authors speculate that the children who had not grown well at the end of the newborn period, may have had weaker immunity becoming more vulnerable to the common community infections.
It was not possible to analyze the contribution of HIV and possible differences in socio-economic status with respect all the outcome variables reported in the present study. These may have been important confounders in this study. HIV testing was seldom performed in this cohort making it impossible to assess this variable. Beast milk fed infants may have been more exposed to this virus partly explaining their increased morbidity and mortality. Though socio-economic status influences morbidity, mortality and neurological development, this information was also not specifically sub-analyzed.
In conclusion, this study agrees with previous workers that early nutrition affects early growth and subsequent neuro-developmental scores of VLBW infants and that reliance on un-fortified breast milk may not be optimal in this population of high-risk newborns. The results also suggests the possibility that early nutritional interventions may improve the post-discharge morbidity in this population.
Acknowledgement
The University of Nairobi: This manuscript was extracted from the principal author's (FW) thesis accepted in 2006 for a Doctorate of Medicine in that university. Kenyatta National Hospital administration: They allowed and partly sponsored the research. Ms Janet Musia: The tireless data manager. Ms Penina Mukuhi, Developmental specialist who performed the functional disability tests for comparison with the author.
Conflict of interest
The authors had no linkages, affiliations or any manner of support or influence from Nestle foods Kenya, the manufacturer of the preterm formula used in by the infants recruited in this study.
References
- 1.On optimal period of exclusive breast feeding. Geneva: WHO/NHD/01.09; 2002. Report of an expert consultative group; pp. 1–10. [Google Scholar]
- 2.Lucas A, Gore SM, Cole TJ, Bam ford MF, Dissector JFB, Barr I, Diablo L, Cork S, Lucas PJ. Multi-centre trial on feeding the low birth weight infants: effects of diet on early growth. Archives of Diseases of Childhood. 1984;59:722–730. doi: 10.1136/adc.59.8.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooke OG, Wood C, Barley J. Energy balance, nitrogen balance, and growth in pre-term infants feed on expressed milk, a pre-term infant formula, and two low-salute adapted formulae. Arch Diseases of Child. 1982;57:898–904. doi: 10.1136/adc.57.12.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guido EM, Iolanda M. Fortification of human milk. Nestle nutrition workshop series pediatric program. Vol. 43. Philadelphia: Lippincott Williams and Wilkins; 1999. pp. 81–93. [Google Scholar]
- 5.Schanler RJ, Shulman RJ, Lau C. Feeding strategies for premature infants: Beneficial outcomes of feeding fortified human milk versus pre-term formula. Pediatrics. 1999;103:1150–1157. doi: 10.1542/peds.103.6.1150. [DOI] [PubMed] [Google Scholar]
- 6.Hack M, Merkatz IR, Gordon D, Jones PK, Fanaroff AA. The prognostic significance of postnatal growth in VLBW infants. Am J Obstetric Gynecology. 1982;143:693–699. doi: 10.1016/0002-9378(82)90117-x. [DOI] [PubMed] [Google Scholar]
- 7.Hack M, Merkatz IR, McGrath SK, Jones PK, Fanaroff AA. Catch up growth in VLBW infants. Arch Dis Child. 1984;138:370–375. doi: 10.1001/archpedi.1984.02140420036013. [DOI] [PubMed] [Google Scholar]
- 8.Lucas A, Morley R, Cole TJ, Gore SM, Davis JA, Bamford MF, Dosetor JF. Early diet in pre-term babies and developmental status in infancy. Arch Dis Child. 1989;64:1570–1578. doi: 10.1136/adc.64.11.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucas A, Morley R, Cole TJ, Gore SM, et al. Early diet in pre-term babies and developmental status at 18 months. The Lancet. 1990;335:1477–1481. doi: 10.1016/0140-6736(90)93026-l. [DOI] [PubMed] [Google Scholar]
- 10.McCance RA. Food growth and time. Lancet. 1962;ii:271–272. doi: 10.1016/s0140-6736(62)90499-3. [DOI] [PubMed] [Google Scholar]
- 11.Smart J. Under nutrition, learning and memory: review of experimental studies. In: Tailor TG, Jenkins NK, editors. Proceedings of XIII International congress of nutrition. London: John Libbey; 1986. pp. 74–78. [Google Scholar]
- 12.Dobbing J, Sands J. Vulnerability of developing brain. IX. The effect of nutritional growth retardation on the timing of the brain growth spurt. Biol Neonate. 1971;19:363–378. doi: 10.1159/000240430. [DOI] [PubMed] [Google Scholar]
- 13.Drillien CM. The incidence of mental and physical handicaps in school age children of very low birth weight. Pediatrics. 1967;39:238–248. [PubMed] [Google Scholar]
- 14.Lubchenco LO, Delivoria-Papadopoulos M, Butterfield LJ, et al. Long-term follow-up studies of prematurely born infants. I. Relationship of handicaps to nursery routines. J Pediatric. 1972;80:501–508. doi: 10.1016/s0022-3476(72)80517-1. [DOI] [PubMed] [Google Scholar]
- 15.Lucas A. Nutrition of the Very Low Birth Weight Infant. Nestle Nutrition Workshop Series. Vol. 43. Philadelphia: Lippincott Williams and Wilkins; 1999. Early nutrition and later outcome; pp. 2–18. [Google Scholar]
- 16.Lucas A, Morley M, Cole TJ, Lister G, Leeson-Payne Breast milk and subsequent intelligence quotient in children born pre-term. The Lancet. 1992;339:261–264. doi: 10.1016/0140-6736(92)91329-7. [DOI] [PubMed] [Google Scholar]
- 17.Ballard J, Norak KC, Driver M. A simplified score for assessment of foetal maturity on newly born infants. J pediatrics. 1979;95:769–774. doi: 10.1016/s0022-3476(79)80734-9. [DOI] [PubMed] [Google Scholar]
- 18.Saigal Saroj, Rosenbaum P, Stoskopf B, Milner R. Follow-up of infant's 501 to 1500 gm birth weight delivered to residents of a geographically defined region with perinatal intensive care facilities. J of Pediatrics. 1982;100:606–613. doi: 10.1016/s0022-3476(82)80767-1. [DOI] [PubMed] [Google Scholar]
- 19.Babson SG. Growth of LBW infants. Journal of Pediatrics. 1970;77:11–20. doi: 10.1016/s0022-3476(70)80039-7. [DOI] [PubMed] [Google Scholar]
- 20.Casey PH, Kraemar HC, Bernbaum J, Yogman MW, Sells JC. Growth status and growth rates of a varied sample of LBW infants. Journal of Pediatrics. 1991;119:599–605. doi: 10.1016/s0022-3476(05)82414-x. [DOI] [PubMed] [Google Scholar]
- 21.Gardiner D, Pearson A growth chart for premature and other infants. Arch of Diseases of Child. 1971;46:783–787. doi: 10.1136/adc.46.250.783. [DOI] [PMC free article] [PubMed] [Google Scholar]