Abstract
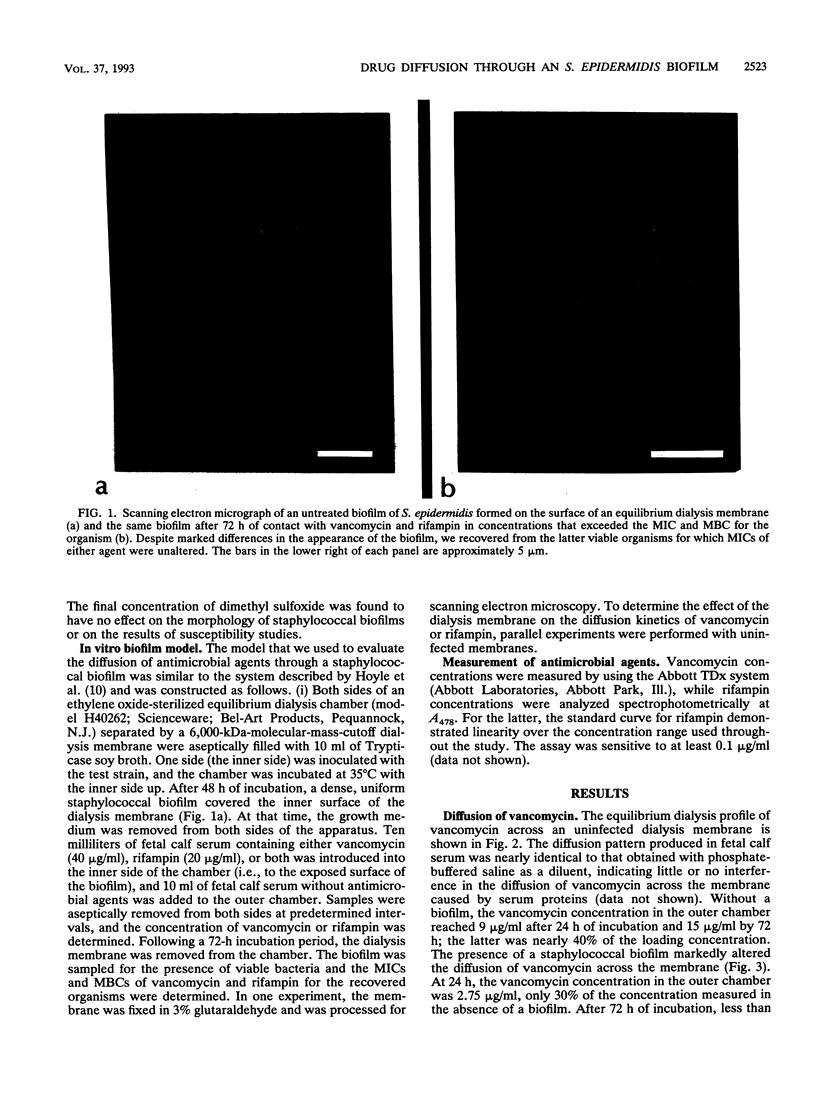
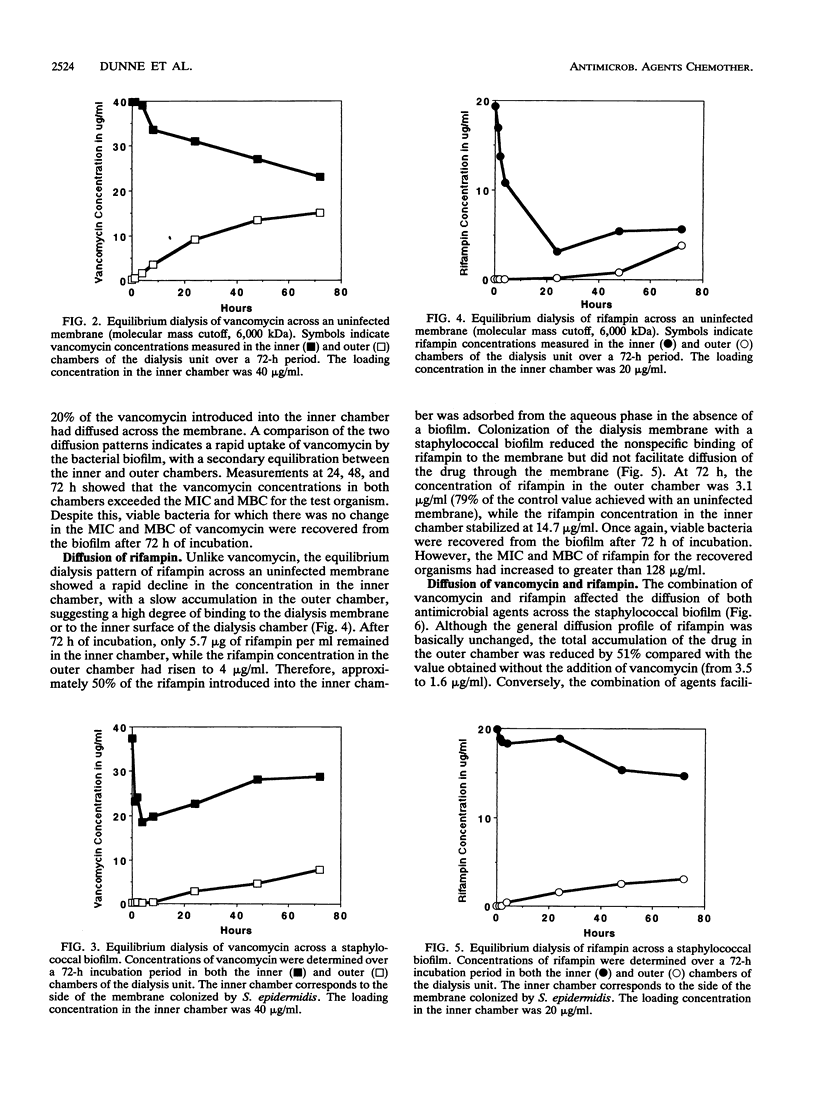
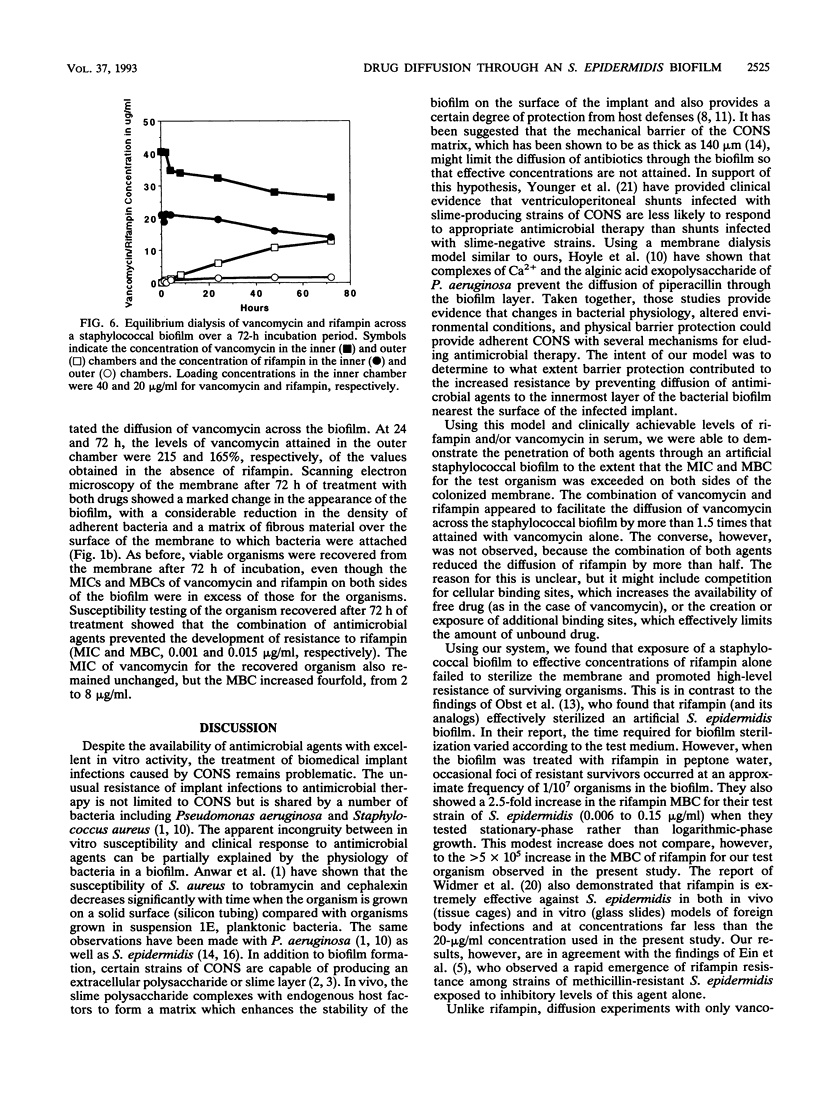
Using an equilibrium dialysis chamber, we evaluated the penetration of vancomycin, rifampin, or both through a staphylococcal biofilm to simulate treatment of an infected biomedical implant. A biofilm of ATCC 35984 (slime-positive Staphylococcus epidermidis; vancomycin MIC and MBC, 1 and 2 micrograms/ml, respectively; rifampin MIC and MBC, 0.00003 and 0.00025 micrograms/ml, respectively) was established on the inner aspect of the dialysis membrane (molecular mass exclusion, 6,000 kDa). Serum containing vancomycin (40 micrograms/ml), rifampin (20 micrograms/ml), or a combination of both was introduced into the inner chamber of the dialysis unit (in direct contact with the biofilm), and serum alone was added to the outer chamber. Rifampin and vancomycin concentrations in both chambers were determined over a 72-h period. In the absence of rifampin, the concentration of vancomycin in the outer chamber exceeded the MBC for the organism after 24 h, and the MBC increased to nearly 8.0 micrograms/ml by 72 h, demonstrating that therapeutic levels of vancomycin can penetrate a staphylococcal biofilm. However, viable bacteria were recovered from the biofilm after 72 h of treatment with no apparent increase in the MIC or MBC of vancomycin. Similarly, concentrations of rifampin exceeding the MBC were detected in the outer chamber after 24 h of treatment, but viable organisms were recovered from the biofilm after 72 h of treatment. In this case, the rifampin MBCs for surviving organisms increased from 0.00025 to > 128 micrograms/ml. The combination of agents prevented the development of resistance to rifampin, improved the perfusion of vancomycin through the biofilm, and decreased the penetration of rifampin but did not sterilize the membrane. These observations provide evidence that bactericidal levels of vancomycin, rifampin, or both can be attained at the surface of an infected implant. Despite this, sterilization of the biofilm was not accomplished after 72 h of treatment.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anwar H., Strap J. L., Costerton J. W. Eradication of biofilm cells of Staphylococcus aureus with tobramycin and cephalexin. Can J Microbiol. 1992 Jul;38(7):618–625. doi: 10.1139/m92-102. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Parisi J. T., Bisno A. L., Simpson W. A., Beachey E. H. Characterization of clinically significant strains of coagulase-negative staphylococci. J Clin Microbiol. 1983 Aug;18(2):258–269. doi: 10.1128/jcm.18.2.258-269.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport D. S., Massanari R. M., Pfaller M. A., Bale M. J., Streed S. A., Hierholzer W. J., Jr Usefulness of a test for slime production as a marker for clinically significant infections with coagulase-negative staphylococci. J Infect Dis. 1986 Feb;153(2):332–339. doi: 10.1093/infdis/153.2.332. [DOI] [PubMed] [Google Scholar]
- Ein M. E., Smith N. J., Aruffo J. F., Heerema M. S., Bradshaw M. W., Williams T. W., Jr Susceptibility and synergy studies of methicillin-resistant Staphylococcus epidermidis. Antimicrob Agents Chemother. 1979 Nov;16(5):655–659. doi: 10.1128/aac.16.5.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etienne J., Brun Y., el Solh N., Delorme V., Mouren C., Bes M., Fleurette J. Characterization of clinically significant isolates of Staphylococcus epidermidis from patients with endocarditis. J Clin Microbiol. 1988 Apr;26(4):613–617. doi: 10.1128/jcm.26.4.613-617.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber B. F., Kaplan M. H., Clogston A. G. Staphylococcus epidermidis extracted slime inhibits the antimicrobial action of glycopeptide antibiotics. J Infect Dis. 1990 Jan;161(1):37–40. doi: 10.1093/infdis/161.1.37. [DOI] [PubMed] [Google Scholar]
- Hogt A. H., Dankert J., Hulstaert C. E., Feijen J. Cell surface characteristics of coagulase-negative staphylococci and their adherence to fluorinated poly(ethylenepropylene). Infect Immun. 1986 Jan;51(1):294–301. doi: 10.1128/iai.51.1.294-301.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle B. D., Alcantara J., Costerton J. W. Pseudomonas aeruginosa biofilm as a diffusion barrier to piperacillin. Antimicrob Agents Chemother. 1992 Sep;36(9):2054–2056. doi: 10.1128/aac.36.9.2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G. M., Lee D. A., Regelmann W. E., Gray E. D., Peters G., Quie P. G. Interference with granulocyte function by Staphylococcus epidermidis slime. Infect Immun. 1986 Oct;54(1):13–20. doi: 10.1128/iai.54.1.13-20.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obst G., Gagnon R. F., Harris A., Prentis J., Richards G. K. The activity of rifampin and analogs against Staphylococcus epidermidis biofilms in a CAPD environment model. Am J Nephrol. 1989;9(5):414–420. doi: 10.1159/000168004. [DOI] [PubMed] [Google Scholar]
- Russell P. B., Kline J., Yoder M. C., Polin R. A. Staphylococcal adherence to polyvinyl chloride and heparin-bonded polyurethane catheters is species dependent and enhanced by fibronectin. J Clin Microbiol. 1987 Jun;25(6):1083–1087. doi: 10.1128/jcm.25.6.1083-1087.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheth N. K., Franson T. R., Sohnle P. G. Influence of bacterial adherence to intravascular catheters on in-vitro antibiotic susceptibility. Lancet. 1985 Dec 7;2(8467):1266–1268. doi: 10.1016/s0140-6736(85)91552-1. [DOI] [PubMed] [Google Scholar]
- Simon V. C., Simon M. Antibacterial activity of teicoplanin and vancomycin in combination with rifampicin, fusidic acid or fosfomycin against staphylococci on vein catheters. Scand J Infect Dis Suppl. 1990;72:14–19. [PubMed] [Google Scholar]
- Wang I. W., Anderson J. M., Marchant R. E. Staphylococcus epidermidis adhesion to hydrophobic biomedical polymer is mediated by platelets. J Infect Dis. 1993 Feb;167(2):329–336. doi: 10.1093/infdis/167.2.329. [DOI] [PubMed] [Google Scholar]
- West T. E., Walshe J. J., Krol C. P., Amsterdam D. Staphylococcal peritonitis in patients on continuous peritoneal dialysis. J Clin Microbiol. 1986 May;23(5):809–812. doi: 10.1128/jcm.23.5.809-812.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widmer A. F., Frei R., Rajacic Z., Zimmerli W. Correlation between in vivo and in vitro efficacy of antimicrobial agents against foreign body infections. J Infect Dis. 1990 Jul;162(1):96–102. doi: 10.1093/infdis/162.1.96. [DOI] [PubMed] [Google Scholar]
- Younger J. J., Christensen G. D., Bartley D. L., Simmons J. C., Barrett F. F. Coagulase-negative staphylococci isolated from cerebrospinal fluid shunts: importance of slime production, species identification, and shunt removal to clinical outcome. J Infect Dis. 1987 Oct;156(4):548–554. doi: 10.1093/infdis/156.4.548. [DOI] [PubMed] [Google Scholar]