Abstract
Aims
The present study examined the relationship between cigarette smoking and alcohol use outcomes over an 8-year period following treatment for adolescent alcohol and other drug (AOD) use disorders.
Methods
The present study was based on a sample of 166 adolescents recruited during inpatient AOD abuse treatment. Included in this study were 123 (74% of the full sample) participants, of whom 41% were female, 81% identified themselves as White and who averaged 15.9 years of age (SD = 1.3) when entering treatment. Data for the present study were drawn from interviews conducted at the time of treatment and 2-, 4-, 6- and 8-years post-treatment.
Results
Twenty six percent of participants had quit smoking for >1 year at the 8-year assessment, while 44% reported persistent smoking over time. Overall smoking rates decreased significantly over time. Subjects associated with the highest alcohol involvement trajectory reported significantly greater likelihood of persistent smoking as well as higher current smoking and cigarette consumption across time points.
Conclusions
The significant declines observed in smoking from adolescence into young adulthood were contrary to expectations, indicating that this behaviour may be less stable than previously thought among adolescent AOD abusers. Smoking involvement over time was greater within the highest alcohol use trajectory, consistent with previous evidence for a positive relationship between these behaviours. However, when compared with the general population smoking rates remained very high regardless of alcohol involvement. Thus, individuals treated for AOD abuse as adolescents remained at elevated risk for tobacco related disease regardless of post-treatment AOD use outcomes.
INTRODUCTION
Cigarette smoking is more common, heavier and more persistent among individuals with higher alcohol consumption. For example, heavy drinking among smokers has been associated with increased quantity of cigarette use (Batel et al., 1995) and a greater likelihood of remaining a smoker (Murray et al., 1995). Similarly, alcohol dependent individuals who smoke cigarettes are found to consume alcohol with greater quantity and frequency (York and Hirsch, 1995) and have more severe alcohol dependence (Daeppen et al., 2000) relative to those who don’t smoke. This relationship is most apparent in clinical samples, as studies of smoking among adults treated for alcohol and other drug (AOD) use disorders consistently indicate that over 80% smoke cigarettes (Bien and Burge, 1990; Keuthen et al., 2000). In contrast, recent national survey data reveal that fewer than 25% of adults in the United States smoke (CDC, 2005). Not surprisingly, AOD abusers who smoke incur significant health consequences. For example, evidence suggests that tobacco and alcohol have synergistic effects that lead heavy drinkers who smoke to be at substantially increased risk for oral/pharyngeal cancers (Maier et al., 1992). Accordingly, tobacco is a significant contributor to mortality following treatment for AOD abuse and dependence (Hser et al., 1994; Hurt et al., 1996). A growing literature on tobacco use among adult AOD abusers reflects concern regarding the significant health consequences observed for individuals who combine these behaviours. However, despite evidence that smoking rates among youth treated for AOD use disorders are comparable to those of adults, relatively little research has addressed this issue.
The few studies reporting cigarette smoking among adolescents treated for AOD abuse consistently found that over 80% of these youth were smokers (Myers and Brown, 1994; Arria et al., 1995; McDonald et al., 2000; Myers and Macpherson, 2004). In an initial study of smoking among youth receiving AOD abuse treatment (Myers and Brown, 1994) we found that of 166 adolescent participants, 85% reported current (past 30-day) cigarette smoking, 77% reported daily smoking and 63% smoked 1/2 pack or more per day. In contrast, rates of cigarette smoking reported by national surveys of high school seniors at the time these data were collected (late 1980’s) indicated that approximately 30% of students were current smokers, 19% daily smokers, and 11-12% reported smoking 1/2 pack or more per day. Thus, adolescents treated for AOD use disorders smoke at substantially greater rates than high school students.
As with alcohol use disordered adults, evidence suggests that smoking persists following treatment for adolescent AOD problems. In our previous studies 75% of participants reported current cigarette use 2 years following treatment (Myers and Brown, 1994), and 80% of baseline smokers were still smoking 4 years following treatment (Myers and Brown, 1997). In examining health effects from smoking at 2-years post treatment, respiratory problems occurred significantly more often among heavier smoking youth (Myers and Brown, 1994).At the 4-year time point, baseline smokers whose cigarette use persisted reported significantly more alcohol dependence symptoms and tended to report higher levels of drug dependence (Myers and Brown, 1997). We were unable to identify any other reports on cigarette smoking following adolescent AOD use disorder treatment. These findings underscore the importance of this issue by providing evidence that health effects of smoking emerge during adolescence in this population. Further, smoking persists at high rates into early adulthood and appears associated with greater post-treatment alcohol involvement among adolescents treated for AOD use disorders.
Although our previous work indicated that some desistance of smoking occurs following treatment, little is known regarding cessation efforts among AOD abusing youth. Studies of general population samples find that most adolescent smokers want to stop smoking and often attempt smoking cessation (Ershler et al., 1989; Stanton et al., 1996; Burt and Peterson, 1998; Sussman et al., 1998), yet rarely succeed in sustaining abstinence (Burt and Peterson, 1998; Pierce et al., 1998; Zhu et al., 1999). Recently, we obtained similar findings in a study of smoking cessation efforts among adolescents receiving inpatient or outpatient AOD abuse treatment (Myers and Macpherson, 2004). Analyses indicated that 54% of participants had attempted to quit smoking within the last year. Half of those who had tried to quit reported returning to smoking within 1 week of cessation, 65% within 30 days, and 98% within 1 year. These rates are comparable to those reported for teen smokers in general and indicate that sustained smoking abstinence is relatively uncommon. However, little is known regarding long-term smoking cessation efforts (e.g. 1 year of abstinence or longer) among adolescent AOD abusers and the extent to which such efforts occur as they enter adulthood.
A number of studies provide evidence for a relationship between smoking status and post-treatment alcohol and other drug use. As noted above, we have previously reported that persistent smoking was associated with greater alcohol dependence symptomatology 4-years after treatment for adolescent AOD abuse (Myers and Brown, 1997). In addition, smoking cessation is associated with better post-treatment outcomes for adult AOD abusers who smoke. For example, an analysis of 2316 smokers from the drug abuse treatment outcome study (DATOS) (Lemon et al., 2003) found that self-reported smoking cessation was significantly related with greater rates of drug abstinence 12-months following treatment. Similarly, a study of participants in a medical care system (health maintenance organization) presenting for AOD abuse treatment found that baseline smokers who had quit at the 12-month follow-up were less likely to meet diagnostic criteria for alcohol dependence than persistent smokers (Klesges et al., 2003). Thus, available evidence indicates that smoking cessation is more likely for those with better post-treatment outcomes, in particular, those with lower levels of alcohol involvement. Whether this association holds following treatment for adolescent AOD abuse is currently unknown.
The present study builds upon and extends the findings from our previous investigations with this sample (Myers and Brown, 1994, 1997) by describing smoking patterns and examining the relationship between cigarette smoking and alcohol use outcomes over an 8-year period following treatment for adolescent AOD use disorders. Alcohol use outcomes were represented by four alcohol involvement trajectories previously derived for this sample (Chung et al., 2003; Tapert et al., 2003). Based on previous studies regarding the relationship between smoking and post-treatment alcohol involvement, we hypothesized that of baseline smokers, those who smoked at each assessment would be more prevalent in higher alcohol involvement trajectories. On the other hand, we anticipated that those who reported having quit smoking for at least 1 year at the time of the final follow-up assessment would more likely be classified in trajectories of lower alcohol involvement. For the full sample we anticipated that rates of current smoking would not decline significantly over time. Finally, consistent with evidence for a positive correlation between intensity of smoking and alcohol involvement, we hypothesized that subjects who reported current smoking, smoking more cigarettes and greater smoking frequency over time would be classified in higher alcohol involvement trajectories
MATERIALS AND METHODS
Participants
This sample included 166 adolescent inpatients consecutively admitted to one of four San Diego area drug and alcohol treatment centres. The average length of admission was 4 weeks. All met diagnostic and statistics manual (3rd edition) (DSM-III-R) (APA, 1987) criteria for alcohol abuse or dependence, and 97% also met criteria for other drug abuse or dependence. Exclusionary criteria included history of head trauma with sustained (>3 min) loss of consciousness, Axis I disorders preceding the onset of substance abuse problems other than conduct disorder, living more than 50 miles from the research facility, and lack of a parent or other resource person willing to provide corroborating information. We have previously reported on certain smoking characteristics from baseline to 4-years post-treatment in this sample (Myers and Brown, 1994, 1997), as well as trajectories of alcohol involvement during the 8 years following treatment (Chung et al., 2003; Tapert et al., 2003).
Of the 166 adolescents originally recruited, 123 (74%) were included in the present sample. Eight of the original participants were excluded because they had never smoked at baseline and did not initiate smoking during the subsequent 8-year follow-up period. Participants were also excluded from the present sample if they did not provide sufficient data to be classified in terms of alcohol (N = 9) or nicotine (N = 8) involvement, or both (N = 18). The current sample (N = 123) consisted of adolescents (41% female) with a mean age of 15.9 years (SD = 1.3, range 13-18) when entering treatment. In terms of ethnic diversity, 81% of participants identified themselves as Caucasian, 11% as Hispanic, 6% as African-American, and 1% as Native American.
Procedure
Each participant provided assent to take part in this research; separate informed consent was obtained from a parent or legal guardian. This procedure was approved by the individual treatment facilities as well as the Institutional Review Board of the University of California, San Diego. Adolescents and parents were interviewed separately, by different trained interviewers.
Adolescents were interviewed during the third week of treatment. The assessment consisted of a 90-min, confidential, in-person structured research interview, as well as a 2-h neuropsychological battery. Participants and their parents or guardians were interviewed separately at 6 months, 1 year, 2 years, 4 years, 6 years and 8 years post-treatment, either in their home or at the research facility. Data from the 6-month and 1-year measurement points were not reported separately, but were incorporated within the 2 year time point as appropriate, in order to standardize the assessment intervals. Information from parent/resource person interviews was used to corroborate adolescent self-reported substance use. In addition, 10% of participants were randomly selected to provide a urine sample for toxicology screening of illicit drug use at each interview. Toxicology results were compared with interview responses and reviewed with both interviewers and the Principal Investigator of the study and scored so as to present the data as accurately as possible.
Measures
Customary drinking & drug use record (CDDR)
The CDDR (Brown et al., 1998) is a structured interview that assesses alcohol and drug use as well as diagnostic and statistics manual (4th edition) (DSM-IV) (APA, 1994) substance use disorder diagnoses. The CDDR measures quantity and frequency of use of alcohol and nine other types of drugs, including nicotine (cigarettes). The Lifetime version was administered during treatment to measure recent use, as well as lifetime history of such use, including onset of use, use-related problems, and symptoms of abuse, dependence, and withdrawal. At each follow-up interview, the Current version of the CDDR was used to determine substance involvement during the past 90 days and the number of days since last use. The CDDR has been shown to be both reliable and valid with adolescents and adults from clinical and community samples (Brown et al., 1998).
Analytic plan
The purpose of this study was to assess the relationship between cigarette and alcohol use during an 8-year period following treatment for AOD use disorders. Cigarette use outcome variables, derived from the CDDR, included smoking cessation (i.e. whether at the 8-year interview participants had not smoked in the past year), persistent smoking (current smoking at each time point), smoking status at each time point (smoked in past 30 days), and days smoked per month and average cigarettes smoked per day in the past 3 months by time point.
Alcohol use involvement was based upon a previously reported semi parametric, group-based approach to describe trajectories of alcohol involvement in the present sample during the same 8-year period used in the present study (Chung et al., 2003; Tapert et al., 2003). Findings indicated that the best-fitting model for data over this 8-year period consisted of four separate trajectories, labeled abstainers (N = 29, 24% of the sample), infrequent drinkers (N = 28, 23%), worse with time (N = 44, 36%), and frequent drinkers (N = 22, 18%). As expected, these trajectories were significantly different in both number of alcohol related problems and alcohol dependence symptoms. In the current study, we used these classes to examine differences in smoking behaviour across alcohol involvement trajectories.
First, the relationship between persistent smoking and alcohol involvement trajectories was assessed with chi-square tests of proportions.
Next, smoking cessation was examined in relation to alcohol involvement trajectories using chi-square tests of proportions.
Subsequently, current smoking status over time was examined in relation to alcohol use trajectories using a longitudinal logistic regression model for correlated dichotomous outcomes estimated via the generalized estimating equations method (Liang and Zeger, 1986), implemented in SAS PROC GEE. In the GEE procedure model parameters are estimated using all available data, rather than excluding subjects with missing data. This model characterized the multiple dichotomous measures (smoking vs not smoking) in terms of probability of smoking at baseline and changes in the probability of smoking over time. The primary predictor variables included in both models consisted of three variables dummy-coded to test three a-priori contrasts: abstainer versus infrequent drinker, abstainer versus worse with time, and abstainer versus frequent drinker. (This coding scheme, whereby the ‘abstainers’ serve as the reference category, is repeated for subsequent analyses.) The model was initially fit including interactions between these three predictors and time, which were removed if nonsignificant. An m-dependent, or Toeplitz, correlation structure was selected based on the observed pattern of correlations of smoking status over time.
Finally, the relationships between alcohol use trajectory and cigarette use quantity and smoking frequency over time were assessed via mixed effects regression, implemented in SAS PROC MIXED. We opted for this procedure over repeated measures one-way analyses of varianceOne-Way Analyses of Variance (ANOVA) because it places no restrictions on the number of observations per subject, allowing participants with one or two missing data points to be included in the analyses. Both models incorporated linear trends and an uncorrelated variance-covariance structure, which was chosen after comparison with several other possibilities (Verbeke and Molenberghs, 2000). The three dummy-coded variables described above were also included as the primary predictors in both mixed effects regression models. Each model initially included interactions between these three variables and time. Non significant interactions with time were excluded from the final models.
RESULTS
Preliminary analyses
Demographic characteristics of the sample at baseline are shown in Table 1. Gender varied significantly by alcohol trajectory group (X2 (3) = 16.70, P = 0.001); about 60% of participants in the abstainer and infrequent drinker trajectories were female, compared with 21% and 32%, respectively, in the worse with time and frequent drinker groups. Consequently, gender was included as a covariate in subsequent analyses. ANOVAs indicated that the groups did not vary in terms of age at the beginning of treatment (F (3, 119) = 1.85, P = 0.142), age at which they first smoked a cigarette (F (3, 119) = 0.03, P = 0.994), cigarette consumption during the 3 months prior to entering treatment (F (3, 118) = 1.57, P = 0.201), or days smoked per month in the 3 months immediately preceding treatment (F (3, 119) = 0.70, P = 0.555). Additionally, post-hoc contrasts revealed no significant differences between any pair of groups on these four variables.
Table 1.
Baseline demographic characteristics of the sample by alcohol trajectory group
| Variable | Abstainers (N = 29) | Infrequent drinkers (N = 28) | Worse with time (N = 44) | Frequent drinkers (N = 22) | Total (N = 123) |
|---|---|---|---|---|---|
| Gender | 59% female | 61% female | 21% female | 32% female | 41% female |
| Age (M (SD)) | 16.2 (1.5) | 15.7 (1.3) | 16.1 (1.0) | 15.5 (1.6) | 15.9 (1.3) |
| Age when first smoked | 11.6 (3.8) | 11.9 (4.2) | 11.7 (4.6) | 11.7 (3.6) | 11.7 (4.1) |
| Cigarettes/day | 16.1 (14.8) | 12.7 (9.6) | 11.2 (10.1) | 16.2 (10.6) | 13.6 (11.4) |
| Days smoked per month | 24.4 (11.0) | 26.4 (9.5) | 24.5 (10.9) | 27.7 (7.5) | 25.5 (10.1) |
Binary logistic regressions were conducted to assess the influence of baseline smoking variables on whether baseline smokers (N = 93) reported current smoking at each time point (persistent smoking) or being quit from smoking for a year or longer at the 8-year assessment. None of these variables predicted either smoking cessation at the 8-year time point or persistent smoking.
Next, the effect of age at first cigarette, baseline smoking quantity and smoking frequency on post-treatment smoking variables over time (current smoking status, smoking quantity and frequency) were tested separately for the full sample (N = 123). A longitudinal logistic regression model showed that baseline smoking quantity (z = 1.39, P = 0.166) and smoking frequency (z = 1.32, P = 0.188) did not predict current smoking status over the remaining time points. Age at first cigarette was a significant predictor (z = -2.35, P = 0.019), such that those who were younger when they first smoked had a greater probability of current smoking. A mixed effects regression model indicated that number of cigarettes consumed at years 2, 4, 6, and 8 was predicted by age first smoked (t (299) = -2.08, P = 0.039) and baseline smoking quantity (t (299) = 4.50, P < 0.001), but not by baseline smoking frequency (t (299) = 0.67, P = 0.501). Participants who were younger when they first tried smoking and those who smoked at a higher rate upon entering treatment smoked more cigarettes at the subsequent assessments. A similar pattern was observed for smoking frequency at years 2, 4, 6, and 8. Participants who were younger when they first smoked (t (304) = -2.34, P = 0.020) and those who smoked more cigarettes at baseline (t (304) = 1.99, P = 0.047) reported smoking on more days per month throughout the post-treatment period. There was also a trend toward individuals who smoked on more days per month at baseline continuing that pattern at years 2, 4, 6, and 8 (t (304) = 1.75, P = 0.082).
Smoking patterns among baseline smokers
Of the 110 subjects who were current smokers at the time of treatment, 93 (85%) completed 8-year assessments and were included in this set of analyses. At the final (8-year) assessment 22% (N = 24) of those who smoked during substance abuse treatment had quit smoking for at least 1 year. Of these, approximately 90% reported not smoking for at least 2 years. Individuals associated with the abstainer trajectory had the highest proportion of quitters (N = 8, 38%) while frequent drinkers had the lowest proportion (N = 3, 16%) (see Table 2). However, chi-square tests of proportions indicated that this difference was not significant across all four trajectories (X2 (3) = 3.91, P = 0.272). When examining only the abstainer and frequent drinking trajectories a non significant trend emerged such that quitting was more likely among abstainers (X2 (1) = 2.82, P = 0.093) than frequent drinkers.
Table 2.
Proportion of current smokers at the time of treatment who quit or smoked persistently by alcohol use trajectory group
| Alcohol use trajectory group |
|||||
|---|---|---|---|---|---|
| Abstainers (N = 21) (%) | Infrequent drinkers (N = 22) (%) | Worse with time (N = 31) (%) | Frequent drinkers (N = 19) (%) | Total (N = 93) (%) | |
| Quit smoking | 38 | 18 | 29 | 16 | 26 |
| Smoked persistently | 24 | 45 | 45 | 63 | 44 |
Approximately 44% of baseline smokers (N = 41) reported persistent smoking (i.e. current smoking at each assessment). As shown in Table 2, persistent smoking was more common among frequent drinkers than the other three groups, but the proportions did not vary significantly across alcohol trajectory classes (X2 (3) = 5.77, P = 0.123). Comparison of proportion of persistent smokers across only the abstainer and frequent drinker trajectories did indicate a significant difference showing persistence was more likely among frequent drinkers (X2 (1) = 5.77, P = 0.016).
Smoking over time in relation to alcohol use trajectories
Prior to examining the relationship between smoking variables over time and alcohol trajectories, we considered whether smoking differences between trajectory groups could be explained by baseline differences in drinking. Specifically, we used mixed effects regression analysis to test whether number of lifetime drinks, number of alcohol dependence symptoms, and number of alcohol withdrawal symptoms, all measured at baseline, predicted cigarettes per month, days smoked per month, and smoking status over time. In each analysis, the baseline drinking variable did not significantly predict smoking behaviour over time.
Next, we assessed the effect of alcohol trajectory class on current smoking status at each measurement point via a longitudinal logistic regression model. Overall, the proportion of participants who had smoked in the past 30 days decreased over time, from 90% at baseline to 64% at the 8-year assessment. As shown in Table 3, the main effect of time was significant (z = -6.74, P < 0.0001), indicating that the probability of current smoking decreased over time for all classes (see Fig. 1). There was a marginal effect of gender (z = 1.89, P = 0.059), such that male participants were somewhat more likely to be current smokers than female participants. The infrequent drinker and worse with time groups did not differ significantly from abstainers. All interactions with time were non significant and were excluded from the final model. There was a significant effect of being in the frequent drinker group (z = 2.37, P = 0.018), indicating that throughout the study participants in this group were approximately three times more likely to be current smokers than those in the abstainer group.
Table 3.
Longitudinal logistic regression model of current smoking status over time
| Variable | Unstandardized regression coefficient | Standard error | Z-score | Odds ratio (95% CI) | P-value |
|---|---|---|---|---|---|
| Time | -0.22 | 0.03 | -6.74 | 0.80 (0.76-0.85) | <0.0001 |
| Gender | 0.55 | 0.29 | 1.89 | 1.73 (0.98-3.06) | 0.059 |
| Infrequent | 0.51 | 0.40 | 1.30 | 1.67 (0.76-3.65) | 0.194 |
| Worse | -0.08 | 0.35 | -0.23 | 0.92 (0.46-1.83) | 0.819 |
| Frequent | 1.14 | 0.48 | 2.37 | 3.13 (1.22-8.01) | 0.018 |
Fig. 1.
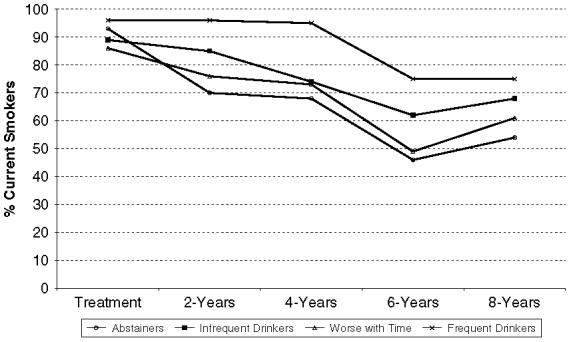
Rates of current (past 30 day) smoking across assessments by alcohol use trajectory.
We then conducted a mixed effects regression to examine the effect of alcohol trajectory class on average monthly cigarette consumption (i.e. total number of cigarettes) over the five assessment points. The final model is shown in Table 4. There was a significant effect of time (t (437) = -4.33, P < 0.0001), indicating that, across trajectory groups, cigarette consumption declined significantly over time. The effect of gender was not significant. Neither the infrequent drinkers nor those in the worse with time group were significantly different from abstainers. None of the trajectory comparison variables interacted significantly with time; consequently, these interactions were not included in the final model. However, there was a significant difference between frequent drinkers and abstainers (t (437) = 2.44, P = 0.015), such that frequent drinkers smoked significantly more cigarettes throughout the study period.
Table 4.
Mixed effects regression model of cigarettes per month over time
| Variable | Unstandardized regression coefficient | Standard error | T-score | P-value |
|---|---|---|---|---|
| Time | -12.71 | 2.93 | -4.33 | <0.0001 |
| Gender | 55.08 | 36.02 | 1.53 | 0.127 |
| Infrequent | 70.62 | 48.28 | 1.46 | 0.144 |
| Worse | 13.25 | 45.72 | 0.29 | 0.772 |
| Frequent | 128.67 | 52.76 | 2.44 | 0.015 |
Finally, we conducted a similar mixed effects regression analysis to assess whether there was an effect of drinking trajectory on days smoked per month over time. The final model is shown in Table 5. The main effect of time was significant (t (450) = -7.59, P < 0.0001), meaning that across classes participants’ smoking frequency declined over time. Smoking frequency did not vary by gender. As in the analysis of cigarettes smoked per month, neither the infrequent drinker nor worse with time groups were significantly different from the abstainers. All interactions with time were nonsignificant and were excluded from the final model. The comparison of frequent drinkers to abstainers, however, was significant (t (450) = 2.03, P = 0.043). The valence of the effect indicates that throughout the course of the study, frequent drinkers smoked more frequently than abstainers.
Table 5.
Mixed effects regression model of days smoked per month over time
| Variable | Unstandardized regression coefficient | Standard error | T-score | P-value |
|---|---|---|---|---|
| Time | -1.20 | 0.16 | -7.59 | <0.0001 |
| Gender | 2.06 | 1.66 | 1.25 | 0.213 |
| Infrequent | 2.70 | 2.22 | 1.22 | 0.224 |
| Worse | 0.13 | 2.11 | 0.06 | 0.953 |
| Frequent | 4.91 | 2.42 | 2.03 | 0.043 |
DISCUSSION
The present study examined smoking patterns and the relationship between smoking variables and alcohol use trajectories over a period of 8 years following treatment for adolescent AOD abuse. Observed patterns of cigarette use for subjects who smoked at the time of treatment were such that approximately one-quarter had quit smoking for over a year by the final time point assessed, while less than half reported persistent smoking. In contrast with our prediction, a significant decline was observed in overall rates of current smoking across time. The relationships between smoking variables and alcohol use trajectories were generally consistent with hypotheses. Overall, lower rates of quitting and more persistent smoking were associated with the frequent drinker alcohol use trajectory. Similarly, participants associated with the highest alcohol use trajectory (i.e. frequent drinkers) reported significantly greater cigarette involvement across time points. No differences in smoking were observed for the other trajectory classes, although abstainers tended to report the lowest levels of smoking. Overall, the present findings are consistent with previous work demonstrating a correspondence between heavy drinking and smoking.
Examination of smoking cessation and persistence following treatment for adolescent AOD abuse revealed higher quit rates and lower persistence than might be expected for this population. This finding is also noteworthy since participants in the present study were not exposed to any tobacco-related intervention as part of their adolescent AOD abuse treatment. In a study of the natural history of cigarette smoking in a community sample (Rose et al., 1996), 17% of smokers were found to have quit for at least 6 months at the final assessment (at which time subjects where 24-32 years of age). Another prospective investigation of quitting among young adult smokers (Tucker et al., 2005) found that 26% reported quitting for at least 6 months over the 6 years between ages 23 and 29. The present sample reported higher quit rates than either of these community studies, with 26% quit for 1 year or longer at the 8-year assessment. Previous studies of non-clinical samples have reported higher levels of smoking persistence than observed in the present investigation. In a separate study of the community sample reported on above, Chassin and her colleagues (Chassin et al., 1996) found substantial persistence of smoking from adolescence into early adulthood, with little decline evident after the mid 20’s. A prospective investigation of alcohol and tobacco involvement patterns in a high-risk sample of college students yielded a trajectory that represented comorbid alcohol and tobacco dependence (Jackson et al., 2000). Individuals associated with the comorbid trajectory showed increases in tobacco use dependence diagnoses through the college years, with only a slight decline when assessed in their mid-20’s. In contrast, for the present sample rates of current smoking declined from 90% during treatment to 64% at 8-year follow-up, a reduction of approximately 29%. One factor that may have influenced the larger than expected decline in smoking in our sample, the majority of whom reside in California, was exposure to the California Tobacco Control Program (Gilpin et al., 2004). This program was implemented in 1989 and led to substantial declines in youth and adult smoking, with a 22% reduction observed in smoking among 18-24 year olds between 1990 and 1995 (TCS, 2005) (a period that overlaps substantially with post-treatment data collection for the current study). In addition, we have previously reported that smoking rates during treatment may have been temporarily increased by greater exposure to cigarettes (Myers and Brown, 1994), thus possibly inflating the extent of reduction. Finally, adolescents typically display intermittent patterns of smoking, often not smoking daily and smoking relatively few cigarettes per smoking day (e.g. Mermelstein et al., 2002). In contrast, adolescent AOD abusers are very heavy smoking youth who evidence tobacco-related negative health consequences during adolescence (Myers and Brown, 1994). As such, the higher quit rates and greater reductions observed in the present participants when compared to community samples may be motivated by a relatively rapid accumulation of negative consequences from smoking. Regardless, the reductions observed over time in rates of smoking following treatment for adolescent AOD abuse indicate that this behaviour may be less stable than previously thought.
Subjects associated with the heaviest alcohol use trajectory (frequent drinkers) were less likely to have quit smoking, smoked more persistently and reported higher cigarette consumption over time than those classified in the other trajectories. This finding was generally consistent with our hypotheses, although we had anticipated greater differentiation across trajectories. The most consistent differences were observed between the most stable trajectories, abstainers and frequent drinkers, which were associated with the lowest and highest levels across smoking variables examined. The lack of significant differences across all four trajectories may be due to the relatively small sample sizes associated with each trajectory class, as well as the variable patterns of alcohol use reflected by the infrequent drinkers and worse with time trajectories.
Overall, the pattern of significant relationships between cigarette and alcohol use trajectories was consistent with previous research indicating a positive relationship between smoking and drinking. The mechanism underlying this relationship is presumed to be complex and composed of multiple levels of influence. For example, evidence supports the hypothesis that alcohol potentiates the pleasurable effects of nicotine (Narahashi et al., 2001; Rose et al., 2002). Similarly, the priming theory, based on classical conditioning principles, suggests that following paired use of alcohol and nicotine, the use of one may act as a cue to prime the use of the other. Support for the priming theory comes from studies that have found a positive relationship between smoking and drinking (Batel et al., 1995; Murray et al., 1995; York and Hirsch, 1995). The present divergence in smoking and drinking behaviours observed over time between the frequent drinker and abstainer trajectories could be interpreted to support the priming theory. Environmental factors may also have contributed to the pattern of results in this sample. For example, in addition to the well-established role of peers in adolescent AOD involvement, substance use in the social environment is also found to influence adult AOD abuse (Beattie et al., 1992). Thus, frequent drinkers who smoked were likely to associate with others who engaged in the same behaviours, and thereby received social reinforcement for drinking and smoking. In contrast, abstainers were presumably less likely to associate with substance users, potentially resulting in less exposure to and reinforcement for smoking than experienced by frequent drinkers. Studies of smoking cessation efforts in early adulthood find that while several variables predict cessation, transitions into adult social roles (e.g. marriage, work) are particularly influential (Chassin et al., 1996; Rose et al., 1996; Tucker et al., 2005). Successful cessation during early adulthood has been found associated with employment as well as lower levels of smoking (Rose et al., 1996) and less exposure to smokers (Tucker et al., 2005). In a previous study we found that youth who abstained from alcohol and other drug use following treatment had better social and occupational functioning than adolescents reporting post-treatment substance involvement (Brown et al., 1994). Thus, the higher rates of cessation associated with the alcohol abstainer trajectory may reflect the combined influences of less alcohol consumption, reduced exposure to smoking and assuming age-appropriate social roles.
Several important limitations must be considered when interpreting the present findings. First, the present sample is of modest size, and along with small group sizes for each alcohol use trajectory class, limited our ability to detect significant effects. Similarly, the small numbers indicate caution in generalizing these findings. Next, the study from which these data were drawn was not originally designed to investigate tobacco use in detail, providing a limited range of smoking variables and a reliance on uncorroborated selfreport of cigarette use. Also, illicit drug use, which likely influences patterns of tobacco use, was not considered in the present analyses. In addition, the latent class analyses from which the alcohol use trajectories were derived indicate class membership in a probabilistic fashion. Thus, treating subjects associated with a given trajectory as belonging to a unique category may introduce bias into group comparison statistics. Finally, examination of smoking in relation to trajectories of alcohol use may obscure the reciprocal effects whereby changes in use of one substance may influence use of the other (Sher et al., 1996). Future studies that examine in more detail the temporal relationship between smoking cessation efforts and AOD involvement are needed to better understand these patterns.
Overall, although participants in the present study evidenced more cessation and less persistence than anticipated, smoking rates remained very high when compared with the general population. Notably, over half of those associated with the abstainer alcohol use trajectory reported smoking 8-years following treatment. Thus, individuals treated for AOD abuse as adolescents, regardless of post-treatment AOD use outcomes, remained at elevated risk for tobacco related disease. These findings reinforce the importance of recent efforts to address tobacco use in the course of adolescent AOD abuse treatment (McDonald et al., 2000; Myers and Brown, 2005) and commend greater attention to this issue.
Acknowledgement
This study was supported by grants from National Institute on Alcohol Abuse and Alcoholism (AA07033, Sandra Brown, PI) and the National Institute on Drug Abuse (DA017652, Mark Myers, PI).
REFERENCES
- APA . Diagnostic and Statistical Manual of Mental Disorders. 3rd edn, revised American Psychiatric Association; Washington, DC: 1987. [Google Scholar]
- APA . Diagnostic and Statistical Manual of Mental Disorders. 4th edn. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Arria AM, Dohey MA, Mezzich AC, et al. Self-reported health problems and physical symptomatology in adolescent alcohol abusers. Journal of Adolescent Health. 1995;16:226–231. doi: 10.1016/1054-139X(94)00066-N. [DOI] [PubMed] [Google Scholar]
- Batel P, Pessine F, Maitre C, et al. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;9:977. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- Beattie MC, Longabaugh R, Fava JL. Assessment of alcohol-related workplace activities: development and testing of “your workplace”. Journal of Studies on Alcohol. 1992;53:469–475. doi: 10.15288/jsa.1992.53.469. [DOI] [PubMed] [Google Scholar]
- Bien TH, Burge R. Smoking and drinking: a review of the literature. International Journal of the Addictions. 1990;25:1429. doi: 10.3109/10826089009056229. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, et al. Correlates of success following treatment for adolescent substance abuse. Applied & Preventive Psychology. 1994;3:61–73. [Google Scholar]
- Brown SA, Myers MG, Lippke L, et al. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Burt RD, Peterson AV. Smoking cessation among high school seniors. Preventive Medicine. 1998;27:319–327. doi: 10.1006/pmed.1998.0269. [DOI] [PubMed] [Google Scholar]
- CDC Cigarette smoking among adults—United States, 2004. Morbidity and Mortality Weekly Report. 2005;54:1121–1124. [PubMed] [Google Scholar]
- Chassin L, Presson CC, Rose JS, et al. The natural history of cigarette smoking from adolescence to adulthood: demographic predictors of continuity and change. Health Psychology. 1996;15:478–484. doi: 10.1037//0278-6133.15.6.478. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Grella CE, et al. Course of alcohol problems in treated adolescents. Alcoholism-Clinical and Experimental Research. 2003;27:253–261. doi: 10.1097/01.ALC.0000053009.66472.5E. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Smith TL, Danko GP, et al. Clinical correlates of cigarette smoking and nicotine dependence in alcohol-dependent men and women. Alcohol and Alcoholism. 2000;35:171. doi: 10.1093/alcalc/35.2.171. [DOI] [PubMed] [Google Scholar]
- Ershler J, Leventhal H, Fleming R, et al. The quitting experience for smokers in sixth through twelfth grades. Addictive Behaviors. 1989;14:365–378. doi: 10.1016/0306-4603(89)90024-5. [DOI] [PubMed] [Google Scholar]
- Gilpin EA, White MM, White VM, et al. Tobacco Control Successes in California: A Focus on Young People, Results from the California Tobacco Surveys, 1990-2002. University of California; San Diego, La Jolla, CA: 2004. [Google Scholar]
- Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Preventive Medicine. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, et al. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. Journal of the American Medical Association. 1996;275:1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Wood PK. Prospective analysis of comorbidity: tobacco and alcohol use disorders. Journal of Abnormal Psychology. 2000;109:679–694. doi: 10.1037//0021-843x.109.4.679. [DOI] [PubMed] [Google Scholar]
- Keuthen NJ, Niaura RS, Borrelli B, et al. Comorbidity, smoking behavior and treatment outcome. Psychotherapy and Psychosomatics. 2000;69:244. doi: 10.1159/000012403. [DOI] [PubMed] [Google Scholar]
- Klesges LM, Johnson KC, Somes G, et al. Use of nicotine replacement therapy in adolescent smokers and nonsmokers. Archives of Pediatrics & Adolescent Medicine. 2003;157:517–522. doi: 10.1001/archpedi.157.6.517. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Friedmann PD, Stein MD. The impact of smoking cessation on drug abuse treatment outcome. Addictive Behaviors. 2003;28:1323–1331. doi: 10.1016/s0306-4603(02)00259-9. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Maier H, Dietz A, Gewelke U, et al. Tobacco and alcohol and the risk of head and neck cancer. Clinical Investigator. 1992;70:320. doi: 10.1007/BF00184668. [DOI] [PubMed] [Google Scholar]
- McDonald CA, Roberts S, Descheemaeker N. Intentions to quit smoking in substance-abusing teens exposed to a tobacco program. Journal of Substance Abuse Treatment. 2000;18:291–308. doi: 10.1016/s0740-5472(99)00067-7. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Colby SM, Patten C, et al. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine & Tobacco Research. 2002;4:395–403. doi: 10.1080/1462220021000018470. [DOI] [PubMed] [Google Scholar]
- Murray RP, Istvan JA, Voelker HT, et al. Level of involvement with alcohol and success at smoking cessation in the Lung Health Study. Journal of Studies on Alcohol. 1995;56:74. doi: 10.15288/jsa.1995.56.74. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. Smoking and health in substance abusing adolescents: a two year follow-up. Pediatrics. 1994;93:561–566. [PubMed] [Google Scholar]
- Myers MG, Brown SA. Cigarette smoking four years following treatment for adolescent substance abuse. Journal of Child & Adolescent Substance Abuse. 1997;7:1–15. [Google Scholar]
- Myers MG, Macpherson L. Smoking cessation efforts among substance abusing adolescents. Drug and Alcohol Dependence. 2004;73:209–213. doi: 10.1016/j.drugalcdep.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. A controlled study of a cigarette smoking cessation intervention for adolescents in substance abuse treatment. Psychology of Addictive Behaviors. 2005;19:230–233. doi: 10.1037/0893-164X.19.2.230. [DOI] [PubMed] [Google Scholar]
- Narahashi T, Soderpalm B, Ericson M, et al. Mechanisms of alcohol-nicotine interactions: alcoholics versus smokers. Alcoholism-Clinical and Experimental Research. 2001;25:152S–456S. doi: 10.1097/00000374-200105051-00026. [DOI] [PubMed] [Google Scholar]
- Pierce JP, Gilpin EA, Emery SL, et al. A Report to the California Department of Health Services. University of California; San Diego, CA: 1998. Tobacco control in California: Who’s winning the war? An evaluation of the Tobacco Control Program, 1989-1996. [Google Scholar]
- Rose JS, Chassin L, Presson CC, et al. Prospective predictors of quit attempts and smoking cessation in young adults. Health Psychology. 1996;15:261–268. doi: 10.1037//0278-6133.15.4.261. [DOI] [PubMed] [Google Scholar]
- Rose JE, Brauer LD, Behm FM, et al. Potentiation of nicotine reward by alcohol. Alcoholism-Clinical and Experimental Research. 2002;26:1930–1931. doi: 10.1097/01.ALC.0000040982.92057.52. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Gotham HJ, Erickson DJ, et al. A prospective, high-risk study of the relationship between tobacco dependence and alcohol use disorders. Alcoholism-Clinical and Experimental Research. 1996;20:485–492. doi: 10.1111/j.1530-0277.1996.tb01079.x. [DOI] [PubMed] [Google Scholar]
- Stanton WR, Lowe JB, Gillespie AM. Adolescents’ experiences of smoking cessation. Drug and Alcohol Dependence. 1996;43:63–70. doi: 10.1016/s0376-8716(97)84351-7. [DOI] [PubMed] [Google Scholar]
- Sussman S, Dent CW, Severson H, et al. Self-initiated quitting among adolescent smokers. Preventive Medicine. 1998;27:A19–A28. doi: 10.1006/pmed.1998.0379. [DOI] [PubMed] [Google Scholar]
- Tapert SF, McCarthy DM, Aarons GA, et al. Influence of language abilities and alcohol expectancies on the persistence of heavy drinking in youth. Journal of Studies on Alcohol. 2003;64:313–321. doi: 10.15288/jsa.2003.64.313. [DOI] [PubMed] [Google Scholar]
- TCS . Fact Sheet: Adult Smoking Trends in California. California Department of Health Services; Sacramento, CA: 2005. [Google Scholar]
- Tucker JS, Ellickson PL, Orlando M, et al. Predictors of attempted quitting and cessation among young adult smokers. Preventive Medicine. 2005;41:554–561. doi: 10.1016/j.ypmed.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. Springer-Verlag; New York: 2000. [Google Scholar]
- York JL, Hirsch JA. Drinking patterns and health status in smoking and nonsmoking alcoholics. Alcoholism-Clinical and Experimental Research. 1995;19:666. doi: 10.1111/j.1530-0277.1995.tb01565.x. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Sun J, Billings SC, et al. Predictors of smoking cessation in U.S. adolescents. American Journal of Preventive Medicine. 1999;16:202–207. doi: 10.1016/s0749-3797(98)00157-3. [DOI] [PubMed] [Google Scholar]


