Abstract
Connexin43 (Cx43) is abundantly expressed in mammalian testes and implicated in the regulation of cell-to-cell interaction between germ cells and Sertoli cells, which is essential to the normal process of spermatogenesis. In the present study, we investigated the relation between Cx43 expression and the degree of spermatogenesis in infertile human testes. Immunohistochemical analysis of Cx43 was performed on testicular biopsies from 29 patients with azoospermia (n=23) and severe oligospermia (n=6), who gave informed consent to this experiment. The degree of testicular spermatogenesis was evaluated by Johnsen score. In the interstitium, immunostaining for Cx43 was localized to some focal parts of plasma membrane between neighboring Leydig cells. In seminiferous tubules with normal spermatogenesis, Cx43 expression was found between Sertoli cells and germ cells. However, Cx43 expression in maturation arrest was decreased and located mainly in the basal compartment of seminiferous tubules. Finally, there was a significant positive correlation between histological score of spermatogenesis and intensity of Cx43 (p=0.0294). These data suggest that the alteration of Cx43 expression may be involved in spermatogenic impairment, and that the communication between Sertoli cells and germ cells through Cx43 may be important for maturation of spermatogenesis.
Keywords: connexin43, Johnsen score, infertile human testes
I. Introduction
Approximately one in 10 couples suffer from infertility, and about half of this is attributable to the male [6]. Male infertility is induced by intrinsic factors such as genetic disorders, that may cause the impairment of spermatogenesis at several stages of the differentiation of spermatogonia into spermatocytes [9, 21, 29].
Gap junctions are one of the intercellular junctional complexes, which are involved in the regulation of cellular growth, differentiation, and tissue homeostasis [14]. In particular, gap junctions are essential to allow the electrical communication between cells, as demonstrated in the nervous and cardiovascular systems. Gap junctional proteins form intercellular membrane channels, which consist of two hemichannels, the so-called connexon. A connexon is formed by the hexametric assembly of connexins. Gap junctions among adjacent cells transfer small molecules (<1 kDa) such as ions, second messengers and possible morphogens to each other [17]. Around 20 highly homologous products of connexin genes have been identified in humans and in mice [30]. There is much variation in the range of connexins expressed in tissues. In mammals, connexin43 (Cx43) is the most ubiquitously expressed connexin, and is endogenously expressed in at least 35 distinct tissues encompassing over 35 cell types that include cardiomyocytes, keratinocytes, Sertoli cells, and Leydig cells [15].
Previous studies have indicated that Cx43 was mainly expressed in the rodent testis [23], and that mice lacking Cx43 have a failure of spermatogenesis [24]. Further, the defect of Cx43 expression could be a marker of undifferentiated Sertoli cells in human testes [4]. It is assumed that, within the seminiferous epithelium, the proliferation and differentiation of germ cells are regulated by paracrine communication pathways mediated by Sertoli cells [12]. Sertoli cells form gap junctions with spermatogonia [19] and are in contact with each other via a junctional complex of adhering junctions, gap junctions, tight junctions, and desmosomes constituting the anatomical basis of the blood-testis barrier [7, 22, 25]. In the normal adult seminiferous epithelium, primary spermatocytes migrate from the basal to the adluminal compartment. This migration is associated with the modulation of Sertoli-Sertoli cell junctions [26]. These data suggest that gap junctional intercellular communication (GJIC) may be involved in the coordination between the formation and breakdown of Sertoli-Sertoli cell junctions and germ cell differentiation [2].
Therefore, in the present study, we investigated the pattern of Cx43 expression in abnormal spermatogenesis of human infertile testis in order to clarify the mechanism of male infertility.
II. Materials and Methods
Patient profiles and tissue preparation
Testicular biopsy was performed in 29 infertile patients (age: 16–45 years; mean: 31.5 years) with obstructive and non obstructive azoospermia. Obstructive azoospermia was diagnosed in 4 cases. Testosterone level of each case was within normal range. Normal control testes were obtained from 70- to 75-year-old patients undergoing orchidectomy for prostate cancer (n=3). None of the patients had received hormonal therapy or chemotherapy before the collection of tissue samples and all of the patients gave informed consent for this study. Each specimen was pathologically classified into one of 4 groups: germ cell aplasia (n=4, mean Johnsen score 2.14), maturation arrest (n=13, mean Johnsen score 5.36), hypospermatogenesis (n=3, mean Johnsen score 8.84), normal spermatogenesis (n=9, mean Johnsen score 8.66). Pathological classification [28] of each specimens and Johnsen score were examined by a special pathologist. Johnsen score has been proposed for classification of the state of seminiferous tubular quality and there is a high correlation between this score count and sperm count. Each tubular section is given a score from 10 to 1 according to the presence or absence of the main cell types arranged in order of maturity. Presence of spermatozoa scores 10, 9 or 8; spermatids (and no further) 7 or 6; spermatocytes (and no further) 5 or 4; only spermatogonia 3, only Sertoli cells 2 and no cells 1 [13]. Specimens of testicular biopsy for histological examination were fixed by immersion in Bouin’s solution, embedded in paraffin using standard techniques and stained with hematoxylin and eosin.
Biochemicals and chemical reagents
Bovine serum albumin (BSA, minimum 99% pure, essentially free from fatty acids and globulins) and Brij 35 were purchased from Sigma Chemical Co. (St. Louis, MO). 3,3'-diaminobenzidine/4HCl (DAB) was purchased from Dojin Chemical Co. (Kumamoto, Japan).
Antibodies
Polyclonal rabbit anti-Cx43 antibody was purchased from Zymed Laboratories (San Francisco, CA). Horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG F(ab’)2 was purchased from Medical & Biological Laboratories (Nagoya, Japan). Normal goat IgG, and normal rabbit IgG were purchased from Sigma (St. Louis, MO).
Immunohistochemistry
Indirect enzyme-immunohistochemistry [1] was performed for detection of Cx43 protein. Specimens of testicular biopsy were fixed by immersion in 4% paraformaldehyde (pH 7.4) at room temperature and embedded in paraffin using standard techniques [8]. Serial sections were cut 5 µm in thickness and then placed onto 3-aminopropyltriethoxysilane-treated glass slides (Matsunami, Japan).
Paraffin sections were dewaxed with toluene and rehydrated by serial graded ethanol solutions, then the sections were autoclaved at 120°C for 10 min in 10 mM citrate buffer (pH 6.0). After inactivation of endogeneous peroxidase activity with 0.3% H2O2 in methanol (room temperature, 30 min), the sections were preincubated with 500 µg/ml normal goat IgG and 1% BSA in phosphate buffered saline (PBS) for 1 hr to block nonspecific reaction with polyclonal rabbit anti-Cx43 antibody. Then, the sections were reacted overnight with the first antibody at a dilution of 1:800. After washing with 0.075% Brij 35 in PBS and rinsing with PBS, the sections were incubated with HRP-labeled goat anti-rabbit IgG F(ab’)2 at a 1:100 dilution for 1 hr. After washing with 0.075% Brij 35 in PBS and rinsing with PBS, the sites of HRP were visualized by DAB and H2O2. Finally, the sections were counterstained with Mayer’s hematoxylin. As negative control, normal rabbit IgG was used instead of the first antibody in every experiment. As positive control, mouse cardiac muscle was used as described before [20].
Evaluation by image analysis
Quantitative analysis of Cx43 immunostaining was made by an image analyzer (DAB system; Carl Zeiss, Thornwood, NY). The sum of pixel signals was used as signal density for evaluation of the degree of staining and was expressed as pixel values in arbitrary units. Four images were acquired from a randomly selected part in seminiferous tubules on each slide. Total pixel number in positively stained areas was divided by the total pixel number in all measured areas to obtain a percentage of positive seminiferous tubule areas.
Statistical analysis
We evaluated the relationship between Johnsen score and the density of Cx43 immunostaining using regression analysis; if necessary, we transformed the measurements to make their distribution closer to normal distribution. We performed the necessary calculations using STATISTICA 2000 Release 5.5 A (StatSoft Japan Inc., Tokyo).
III. Results
Immunohistochemical analysis of Cx43 expression in human infertile testes
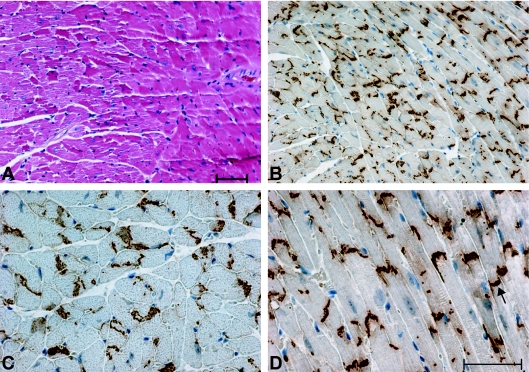
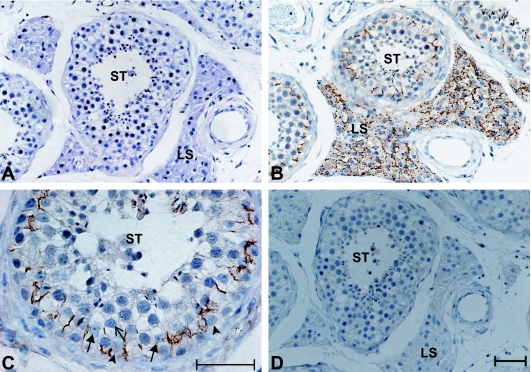
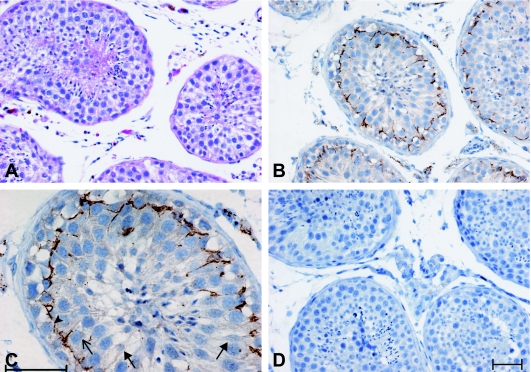
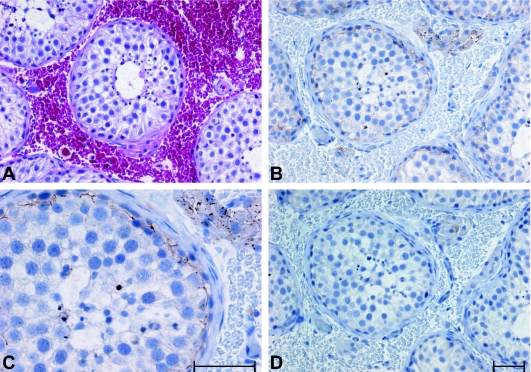
To confirm the specificity of anti-Cx43, we firstly examined the expression of Cx43 in paraffin embedded sections of mouse heart immunohistochemically. As shown in Figure 1, intercalated disks, which are known to be positive to Cx43, were strongly stained under our conditions. When the sections from normal control testes of patients undergoing orchidectomy for prostate cancer were reacted with anti-Cx43, a very strong brown staining was found in the part of plasma membrane of Sertoli cells which was adjacent to the apical part of spermatogonia and to the basal part of primary spermatocytes, in the seminiferous tubules (Fig. 2C). In the interstitium, the staining for Cx43 was also detected on the plasma membranes of Leydig cells (Fig. 2B). In the case of obstructive azoospermia histologically showing the “sloughing off of germ cells,” the expression patterns of Cx43 were similar to that of normal testes (Fig. 3). In the hypospermatogenesis case which showed maturation arrest exhibiting lack of mature sperm, there was essentially no difference in the expression pattern of Cx43, compared to that of normal testes (data not shown). However, the positive area for Cx43 on the plasma membrane of Sertoli cells was decreased and restricted to the basal compartment of seminiferous tubules (Fig. 4). Moreover, in the case of germ cell aplasia that showed Sertoli cell-only syndrome, i.e., lacking any germ cells, the staining for Cx43 was almost nonexistent in the seminiferous tubules while strong signal of Cx43 was detected on the plasma membrane of Leydig cells (Fig. 5).
Fig. 1.
Immunohistochemical detection of Cx43 are found in specialized plasma membrane regions of mouse cardiac myocytes, known as the intercalated disks. (A) H & E staining, ×200. (B) A longitudinal section, ×200. (C) A cross section, ×400. (D) A longitudinal section, arrows indicate intercalated disks, ×200. Bar=50 µm.
Fig. 2.
Immunohistochemical detection of Cx43 between Sertoli cells and germ cells in seminiferous tubules and among Leydig cells in interstitium. (A) H & E staining, ×200. (B) ×200. (C) ×400. (D) Negative control, ×200. ST, seminiferous tubules; LS, Leydig cells. Arrows indicate Sertoli cells, arrowheads indicate spermatogonia, trident indicates primary spermatocytes. Bar=50 µm.
Fig. 3.
Immunohistochemical detection of Cx43 of normal spermatogenesis (Johnsen score 8.88). (A) H & E staining, ×200. (B) ×200. (C) ×400. (D) Negative control, ×200. Arrows indicate Sertoli cells, arrowheads indicate spermatogonia, trident indicates primary spermatocytes. Bar=50 µm.
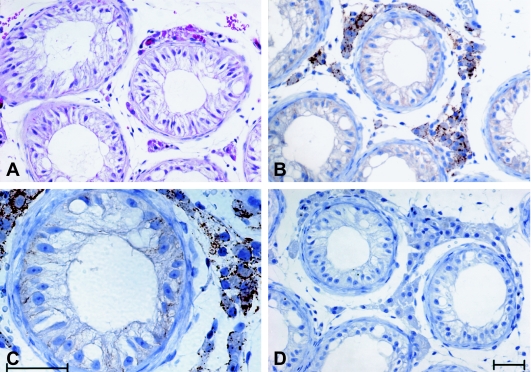
Fig. 4.
Immunohistochemical detection of Cx43 of maturation arrest (Johnsen score 3.24). Positive area for Cx43 on the plasma membrane of Sertoli cells was decreased and restricted to the basal compartment of seminiferous tubules while strong signal of Cx43 was found on the plasma membrane of Leydig cells. (A) H & E staining, ×200. (B) ×200. (C) ×400. (D) Negative control, ×200. Bar=50 µm.
Fig. 5.
Immunohistochemical detection of Cx43 of germ cell aplasia (Johnsen score 2.00). Staining for Cx43 was almost nonexistent in the seminiferous tubules of germ cell aplasia while strong signal of Cx43 was found on the plasma membrane of Leydig cells. (A) H & E staining, ×200. (B) ×200. (C) ×400. (D) Negative control, ×200. Bar=50 µm.
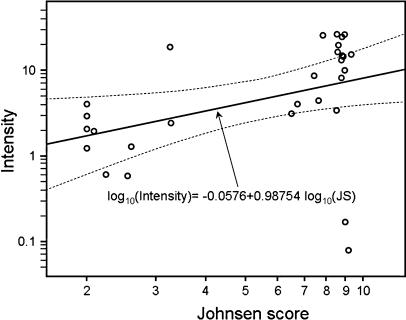
Quantitative analysis of the correlation between histological score (Johnsen score) of spermatogenesis and staining density of Cx43 in testes
As shown in Figure 6, a significant increase in the expression of Cx43 with Johnsen score was noted in seminiferous tubules (p=0.0294). In addition, significant correlation between histological score and expression of Cx43 in Leydig cells was not detected (Spearman rank correlation coefficient=−0.13, p=0.6664) (figure not shown).
Fig. 6.
Scatter plots of histological Johnsen score (JS) and Cx43 immunostaining intensity, with both measurements expressed on base 10 log-scale. Open circles depict the measurements. Solid line indicates the regression line for log10 (JS) and log10 (intensity), while the two dotted curves depict the 95% confidence limits for the population regression line.
IV. Discussion
Intercellular communication via gap junctions is believed to be involved in the control of cell growth and differentiation [14]. Gap junctions allow for the electrical communication between cells, as demonstrated in the nervous and cardiovascular systems. In non-excitable tissues, the biochemical nature of the messengers transmitted across gap junction channels under defined physiological situations is not totally clear [16]. Cx43 protein, which is the predominant component of gap junction in the testes, is expressed in the Sertoli cells and in basally located germ cells, spermatogonia and spermatocytes [3, 23, 27]. In the present study, to examine the involvement of Cx43 protein in spermatogenesis, we examined the expression of Cx43 protein in various clinical stages of infertile human testes immunohistochemically. In seminiferous tubules of normal spermatogenesis and hypospermatogenesis, Cx43 expression was found between adjacent Sertoli cells and between Sertoli cells and germ cells. However, the expression of Cx43 in maturation arrest was obviously decreased, and its localization was changed from the apical compartment of seminiferous tubules to the basal compartment. When the quantitative analysis of Cx43 expression was performed by an image analyzer, there was a significant positive correlation between histological score of spermatogenesis and expression of Cx43 in seminiferous tubules. However, there was no significant correlation between histological score and expression of Cx43 in Leydig cells. There is strong evidence that the defect of Cx43 expression in Sertoli cells could be a marker of undifferentiated Sertoli cell functionality [4]. Further, mice lacking Cx43 have a failure of spermatogenesis [24]. Thus, the expression of Cx43 protein in various stages of impaired testes suggests that this gap junction protein is involved in a specific function during male germ cell differentiation. These results suggest that the spermatogenic function in seminiferous tubules might be related to the preservation of Cx43 expression in Sertoli cells, spermatogonia and spermatocytes.
Recently, chemical agents, such as pesticides, have been suggested as possible carcinogens and as factors of impaired spermatogenesis [10]. Defamie et al. reported that lindane (γ-hexachlorocyclohexane), a widely-used agriculture pesticide, impaired GJIC in 42GPA9 mouse Sertoli cell lines, and that the alterations in gap junctions may be involved in the pathogenesis of neoplastic seminoma proliferation [5]. Therefore, one of the mechanisms which will induce the impairment of spermatogenesis may initially be related to impairment of GJIC, and then may disrupt the control of germ cell proliferation by Sertoli cells.
In the present study, the expression of Cx43 in seminiferous tubules has been demonstrated even in aged men (average 72 years). Aging in men is associated with a decline in trophic factors such as testosterone, alterations in body composition and impaired energy and body weight regulation [18]. However, in general, endocrine functions are sufficient to maintain fertility in elderly men because, qualitative functional semen parameters are apparently not affected by age [11]. According to our study, there was no significant difference in Cx43 expression of seminiferous tubules between young and aged men in normal spermatogenesis. These results suggest that the local regulation via intercellular communication is important in spermatogenesis. Further studies are needed to clarify the molecular role of Cx43 expression in spermatogenesis.
In conclusion, according to the localization of Cx43 expression, the communication between Sertoli cells and germ cells may play an important role in the maturation of spermatogenesis. Therefore, the alteration of Cx43 expression may be one of the major causes of spermatogenic impairment.
V. References
- 1.Aoki D., Yamamoto F. T., Hishikawa Y., Nakamura M., Sakai H., Kanetake H., Koji T. Coexpression of keratinocyte growth factor and its receptor in normal and prostate cancer tissues: possible formation of autonomous andromedin loop. Acta Histochem. Cytochem. 2004;37:379–389. [Google Scholar]
- 2.Batias C., Defamie N., Lablack A., Thepot D., Fenichel P., Segretain D., Pointis G. Modified expression of testicular gap-junction connexin 43 during normal spermatogenetic cycle and in altered spermatogenesis. Cell Tissue Res. 1999;298:113–121. doi: 10.1007/s004419900076. [DOI] [PubMed] [Google Scholar]
- 3.Batias C., Siffroi J. P., Fenichel P., Points G., Segretain D. Connexin43 gene expression and regulation in the rodent seminiferous epithelium. J. Histochem. Cytochem. 2000;48:793–805. doi: 10.1177/002215540004800608. [DOI] [PubMed] [Google Scholar]
- 4.Defamie N., Mograbi B., Roger C., Cronier L., Malassine A., Brucker D. F., Fenichel P., Segretain D., Pointis G. Disruption of gap junctional intercellular communication by lindane is associated with aberrant localization of connexin43 and zonula occludens-1 in 42GPA9 Sertoli cells. Carcinogenesis. 2001;22:1537–1542. doi: 10.1093/carcin/22.9.1537. [DOI] [PubMed] [Google Scholar]
- 5.Defamie N., Berthaut I., Mograbi B., Chevallier D., Dadoune J., Fenichel P., Segretain D., Pointis G. Impaired gap junction connexin43 in Sertoli cells of patients with secretory azoospermia: a marker of undifferentiated Sertoli cells. Lab. Invest. 2003;83:449–456. doi: 10.1097/01.lab.0000059928.82702.6d. [DOI] [PubMed] [Google Scholar]
- 6.De Kretser D. M., Baker H. W. Infertility in men: recent advances and continuing controversies. J. Clin. Endocr. Metab. 1999;84:3443–3450. doi: 10.1210/jcem.84.10.6101. [DOI] [PubMed] [Google Scholar]
- 7.Dym M., Fawcett D. W. The blood-testis barrier in the rat and the physiological compartmentation of the seminiferous epithelium. Biol. Reprod. 1970;3:308–326. doi: 10.1093/biolreprod/3.3.308. [DOI] [PubMed] [Google Scholar]
- 8.Eguchi J., Koji T., Nomata K., Yoshii A., Shin M., Kanetake H. Fas-Fas ligand system as a possible mediator of spermatogenic cell apotosis in human maturation-arrested testes. Hum. Cell. 2002;15:61–67. doi: 10.1111/j.1749-0774.2002.tb00100.x. [DOI] [PubMed] [Google Scholar]
- 9.Escalier D. Impact of genetic engineering on the understanding of spermatogenesis. Hum. Reprod. Update. 2001;7:191–210. doi: 10.1093/humupd/7.2.191. [DOI] [PubMed] [Google Scholar]
- 10.Hauser R. The environment and male fertility: recent research on emerging chemicals and semen quality. Semin. Reprod. Med. 2006;24:156–167. doi: 10.1055/s-2006-944422. [DOI] [PubMed] [Google Scholar]
- 11.Hermann M., Untergasser G., Rumpold H., Berger P. Aging of the male reproductive system. Exp. Gerontol. 2000;35:1267–1279. doi: 10.1016/s0531-5565(00)00159-5. [DOI] [PubMed] [Google Scholar]
- 12.Jegou B. The Sertoli-germ cell communication network in mammals. Int. Rev. Cytol. 1993;147:25–96. [PubMed] [Google Scholar]
- 13.Johnsen S. G. Testicular biopsy score count—a method for registration of spermatogenesis in human testes: normal values and results in 335 hypogonadal males. Hormones. 1970;1:2–25. doi: 10.1159/000178170. [DOI] [PubMed] [Google Scholar]
- 14.Kumar N. M., Gilula N. B. The gap junction communication channel. Cell. 1996;84:381–388. doi: 10.1016/s0092-8674(00)81282-9. [DOI] [PubMed] [Google Scholar]
- 15.Laird D. W. Life cycle of connexins in health and disease. Biochem. J. 2006;394:527–543. doi: 10.1042/BJ20051922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lawrence T. S., Beers W. H., Gilula N. B. Transmission of hormonal stimulation by cell-to-cell communication. Nature. 1978;272:501–506. doi: 10.1038/272501a0. [DOI] [PubMed] [Google Scholar]
- 17.Loewenstein W. R., Rose B. The cell-cell channel in the control of growth. Semin. Cell Biol. 1992;3:59–79. doi: 10.1016/s1043-4682(10)80008-x. [DOI] [PubMed] [Google Scholar]
- 18.Matsumoto A. M., Marc B. T., Gruenewald D. A., Wolden H. T., Naai M. A. Aging and the neuroendocrine regulation of reproduction and body weight. Exp. Gerontol. 2000;35:1251–1265. doi: 10.1016/s0531-5565(00)00158-3. [DOI] [PubMed] [Google Scholar]
- 19.McGinley D. M., Posalaky Z., Porvaznik M., Russell L. D. Gap junctions between Sertoli and germ cells of rat seminiferous tubules. Tissue Cell. 1979;11:741–754. doi: 10.1016/0040-8166(79)90028-4. [DOI] [PubMed] [Google Scholar]
- 20.Mori K., Noguchi M., Matsuo M., Nomata K., Suematsu T., Kanetake H. Decreased cellular membrane expression of gap junctional protein, connexin 43, in rat detrusor muscle with chronic partial bladder outlet obstruction. Urology. 2005;65:1254–1258. doi: 10.1016/j.urology.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 21.Okabe M., Ikawa M., Ashkenas J. Male infertility and the genetics of spermatogenesis. Am. J. Hum. Genet. 1998;62:1274–1281. doi: 10.1086/301895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pelletier R. M., Byers S. W. The blood-testis barrier and Sertoli cell junctions: structural considerations. Microsc. Res. Tech. 1992;20:3–33. doi: 10.1002/jemt.1070200104. [DOI] [PubMed] [Google Scholar]
- 23.Risley M. S., Tan I. P., Roy C., Saez J. C. Cell-, age- and stage-dependent distribution of connexin 43 gap junctions in testes. J. Cell Sci. 1992;103:81–96. doi: 10.1242/jcs.103.1.81. [DOI] [PubMed] [Google Scholar]
- 24.Roscoe W. A., Barr K. J., Mhawi A. A., Pomerantz D. K., Kidder G. M. Failure of spermatogenesis in mice lacking connexin43. Biol. Reprod. 2001;65:829–838. doi: 10.1095/biolreprod65.3.829. [DOI] [PubMed] [Google Scholar]
- 25.Russell L. Desmosome-like junctions between Sertoli and germ cells in the rat testis. Am. J. Anat. 1977;148:301–312. doi: 10.1002/aja.1001480302. [DOI] [PubMed] [Google Scholar]
- 26.Russell L. D., Peterson R. N. Sertoli cell junctions: morphological and functional correlates. Int. Rev. Cytol. 1985;94:177–211. doi: 10.1016/s0074-7696(08)60397-6. [DOI] [PubMed] [Google Scholar]
- 27.Steger K., Tetens F., Bergmann M. Expression of connexin 43 in human testis. Histochem. Cell Biol. 1999;112:215–220. doi: 10.1007/s004180050409. [DOI] [PubMed] [Google Scholar]
- 28.Sternberg S. S. In “Sternberg’s Diagnostic Surgical Pathology”, vol. 2, 4th ed. Lippincott Williams & Wilkins; Philadelphia: 1999. Nonneoplastic diseases of the testis; pp. 2133–2166. [Google Scholar]
- 29.Toshimori K., Ito C., Maekawa M., Toyama Y., Suzuki T. F., Saxena D. K. Impairment of spermatogenesis leading to infertility. Anat. Sci. Int. 2004;79:101–111. doi: 10.1111/j.1447-073x.2004.00076.x. [DOI] [PubMed] [Google Scholar]
- 30.Willecke K., Eiberger J., Degen J., Eckardt D., Romualdi A., Guldenagel M., Deutsch U., Soehl G. Structural and functional diversity of connexin genes in the mouse and human genome. Biol. Chem. 2002;383:725–737. doi: 10.1515/BC.2002.076. [DOI] [PubMed] [Google Scholar]