Abstract
Burkholderia mallei is the cause of glanders and a proven biological weapon. We identified and purified the type IV pilin protein of this organism to study its potential as a subunit vaccine. We found that purified pilin was highly immunogenic. Furthermore, mice infected via sublethal aerosol challenge developed significant increases in titers of antibody against the pilin, suggesting that it is expressed in vivo. Nevertheless, we found no evidence that high-titer antipilin antisera provided passive protection against a sublethal or lethal aerosol challenge and no evidence of protection afforded by active immunization with purified pilin. These results contrast with the utility of type IV pilin subunit vaccines against other infectious diseases and highlight the need for further efforts to identify protective responses against this pathogen.
Glanders, a contagious and fatal disease of odd-toed ungulates that has zoonotic potential, has been known since antiquity. It is caused by infection with the bacterium Burkholderia mallei. In solipeds (horses, mules, and donkeys), B. mallei can cause disease in two forms, respiratory (glanders) and subcutaneous (farcy) (26). Glanders remains a problem in parts of Asia, South America, and Africa (2). Humans may become infected with B. mallei through contact with infected animals, through laboratory accidents, and through inhalation (24). Spread from animals to humans in the natural setting is apparently inefficient, as animal handlers are uncommonly infected. In contrast, B. mallei poses a considerable risk to laboratory workers. Both O. Kalning and K. Helmann, who independently developed diagnostic tests for glanders in 1891, died of the disease within a year (26). A 1947 study described six cases of glanders in researchers who had worked with the organism at Camp Detrick, MD (12). More than 50 years later, glanders was diagnosed in a researcher who worked with the same organism at the same institute (now the U.S. Army Medical Research Institute of Infectious Diseases at Fort Detrick) (20). Most of these cases occurred in the absence of a definable laboratory accident or breach of procedure. Thus, aerosols containing the organism are believed to be highly infectious (24). Untreated human glanders has an extremely high mortality rate (24). However, early and aggressive treatment with combinations of systemic antibiotics can be curative (20).
B. mallei is one of the few pathogens that have been used as biological weapons. During World War I, undercover agents of the Central Powers infected animals destined for the Allies, as well as large numbers of Russian horses and mules on the eastern front, disrupting supply lines. The intent was to kill both the livestock and the humans with whom they came into contact (25). During World War II, the Japanese deliberately infected horses, civilians, and prisoners of war in China with B. mallei (10). The potential reemergence of B. mallei as a biological weapon is of great concern. B. mallei is highly infectious via the respiratory route as an aerosol. The incubation period is long, making it difficult to trace the source of an outbreak or attack. The symptoms are nonspecific, and there is virtually no modern clinical experience to facilitate disease recognition. The illness has a high mortality rate if not recognized and treated. The organism is resistant to multiple antibiotics, making it likely that empirical therapy will fail (11). Therapy must be continued for prolonged durations, potentially taxing antimicrobial supplies in the case of large numbers of exposures. There is no vaccine.
Type IV pili, or fimbriae, are produced by many species of pathogenic gram-negative bacteria (4). Type IV pilin proteins have been used successfully as subunit vaccines for the prevention of several diseases in animals. Purified Moraxella bovis type IV pili protected cattle against keratoconjunctivitis induced by experimental M. bovis infection (13). Comparable results were obtained when using recombinant pili expressed in Pseudomonas aeruginosa, demonstrating that the pilin protein was the immunogen (14). Similarly, purified type IV pili from Dichelobacter nodosus protected sheep against foot rot (21) and protection was also seen in animals vaccinated with recombinant pilin (7). A monoclonal antibody against the toxin-coregulated pilus provided passive protection against cholera in infant mice, indicating that antibodies alone can be protective (22). Additionally, a consensus sequence peptide conjugate vaccine derived from the receptor-binding domain of the P. aeruginosa type IV pilin provided modest protection against death in a mouse model of infection (3). These experiments suggest that type IV pilin proteins are good candidates to serve as subunit vaccines against infections with bacteria that produce type IV fimbriae.
Study of the closely related pathogen B. pseudomallei, which is responsible for the disease melioidosis, revealed a type IV pilus required for virulence (8). Analysis of the B. mallei genome reveals a putative type IV pilin gene. Given the sequence similarity between the predicted pilin proteins of B. mallei and B. pseudomallei, their relatedness to other type IV pilin proteins, the fact that there has been some success in type IV pilus-based vaccines in the past, and the urgent need for more research into potential biological weapons, we tested the hypothesis that a recombinant B. mallei type IV pilin protein subunit vaccine can provide protection against B. mallei disease in a relevant animal model.
MATERIALS AND METHODS
Expression and purification of the B. mallei putative type IV pilin subunit.
Type IV pilin subunits have hydrophobic amino termini that make extensive contacts with each other within the pilus core (5) but interfere with purification because of poor solubility. Additionally, type IV pilin proteins contain two cysteine residues that must form a disulfide bond in the periplasm for proper folding and stability (27). We previously created a cloning vector that allowed the periplasmic purification of N-terminally histidine-tagged, truncated, soluble type IV pilin from enteropathogenic Escherichia coli (16). This plasmid, pPF301, is a derivative of the pET39b+ expression vector (Novagen, EMD Biosciences, San Diego, CA) that encodes a translational fusion of the DsbA signal peptide and its signal peptidase cleavage site, immediately followed by the codons for six histidine residues, an NcoI restriction site, the truncated pilin gene sequences, and a BamHI site after the stop codon. Thus, soluble pilin protein expressed in this vector is targeted for proper folding in the periplasm by the DsbA signal sequence, which is cleaved off, leaving an N-terminal hexahistidine tag. For this study, we amplified the codons for the B. mallei pilin subunit from genomic DNA (a gift of David DeShazer), omitting the sequences specifying the hydrophobic 24 N-terminal amino acids of the mature protein, with primers Donne-736 (5′-CCA TGG AAC AGG ATT ATC TCG CGC GCA G-3′) and Donne-735 (5′-GGA TCC TCA CGC GCG GCA CTC GGG GG-3′), and cloned the product into the NcoI-BamHI sites of pPF301 to create pPF304, replacing the enteropathogenic E. coli pilin gene with that of B. mallei. The insert was confirmed by DNA sequencing. Plasmid pPF304 retains the pBR322 origin of replication, kanamycin resistance selection, T7 promoter, and lacI gene from pET39b+.
To overcome an apparent codon usage problem due to the high G-C gene content (72%), we transformed plasmid pPF304 into competent cells of E. coli expression strain BL21-CodonPlus(DE3)-RP (Stratagene, La Jolla, CA). Overnight cultures of bacteria in LB medium plus chloramphenicol (10 μg/ml) and kanamycin (50 μg/ml) were diluted 1:100 in 1 liter of the same medium and grown while shaking (225 rpm) at 37°C to an A600 of 0.6. Isopropyl-β-d-thiogalactopyranoside (IPTG) was added at a final concentration of 1 mM, and incubation was continued for 4 h. The culture was centrifuged (8,500 × g, 10 min, 4°C), and the pellet was suspended in 50 ml of lysis buffer (20 mM NaH2PO4, 500 mM NaCl, 10 mM, pH 7.4) with four Complete Mini EDTA-free protease inhibitor cocktail tablets (Roche Diagnostics, Indianapolis, IN) and lysed in a French press at 20,000 lb/in2. The lysate was centrifuged (19,140 × g) to remove unbroken cells, membranes, and debris, and the supernatant was applied to a nickel-nitrilotriacetic agarose column (QIAGEN, Valencia, CA). After washing with 100 ml of wash buffer (20 mM NaH2PO4, 500 mM NaCl, 20 mM, pH 7.4), pilin was eluted in 4 ml of elution buffer (20 mM NaH2PO4, 500 mM NaCl, 500 mM, pH 7.4). Eluates were then subjected to two rounds of Sephacryl S-200 16/60 gel filtration chromatography to obtain purified pilin, which was concentrated with a Centricon Plus-20 device (Millipore Corp., Billerica, MA). His-tagged bundlin and His-tagged BfpU were purified as previously described (6, 16). Protein concentrations were calculated from extinction coefficients (9).
Mouse immunization.
To determine whether purified pilin is antigenic, three female 6- to 8-week old CBA/J mice (Harlan Sprague-Dawley, Indianapolis, IN) were immunized subcutaneously with 100 μg of purified pilin protein in complete Freund's adjuvant (CFA; 1:1 [vol/vol] ratio emulsion; Difco Laboratories, Detroit, MI). Booster immunizations of 50 μg in incomplete Freund's adjuvant were given on days 21 and 42. Simultaneously, three control animals received injections with adjuvant alone. Mice were sacrificed on day 56.
For passive-protection experiments, 50 μl of pooled hyperimmune or control serum was administered via intraperitoneal (i.p.) injection to 6- to 8-week-old BALB/c female mice (six mice per group) (Charles River Laboratories, Wilmington, MA) 1 h prior to a challenge with approximately 2 or 14 50% lethal doses (LD50s) of B. mallei.
Active immunization experiments followed two similar protocols. In each case, 6- to 8-week-old BALB/c female mice (10 mice per group) (Charles River Laboratories) were immunized intraperitoneally with either 100 μg of irradiation-killed B. mallei strain China 7 (ATCC 23344) plus adjuvant, 50 μg of B. mallei pilin plus adjuvant, Hanks’ balanced salt solution (HBSS), or adjuvant alone. For the first experiment, the adjuvant was RIBI (Corixa Corp., Seattle, WA) and all of the mice received a booster injection at week 4 identical to the primary injection and were challenged with approximately 7 LD50s at week 10. For the second experiment, the adjuvant for the primary injections was CFA, the mice received boosters at weeks 3 and 7 identical to the primary injection except that CFA was replaced with incomplete Freund's adjuvant, and the mice were challenged at week 10 with approximately 20 LD50s of B. mallei.
Challenge with live B. mallei bacteria.
Mice were infected with virulent B. mallei (ATCC 23344) by small-particle aerosol as previously described (19). This method delivers the bacteria to the lower respiratory tract via particles approximately 1 μm in size. The anticipated dose for lethal challenges was 10 LD50s, that for sublethal infection was slightly less than the LD50, and the dose delivered was confirmed by viable counting. Transponder chips (BioMedic Data Systems, Inc., Seaford, DE) were implanted subcutaneously for specific animal identification. Mice were monitored twice daily, and the number of deaths was recorded. Survival curves were calculated by the Kaplan-Meier method and compared by using the log rank test (version 13.0; SPSS, Chicago, IL). For some experiments, blood was obtained before immunization and 1 week before challenge.
Enzyme-linked immunosorbent assays (ELISAs).
Nunc-Immuno 96-well MaxiSorp plates (Nalge Nunc International, Rochester, NY) were coated with purified B. mallei pilin, with purified bundlin, or with purified BfpU (0.2 μg in 100 μl of phosphate-buffered saline [PBS], pH 7.4) and incubated at 4°C overnight. After washing in PBS plus 0.1% Tween 20, plates were blocked with 10% goat serum (Gibco, Paisley, Scotland, United Kingdom) in PBS plus 0.1% Tween 20 (blocking buffer) and incubated at 37°C for 1 h. After washing, six samples of control sera or duplicate samples of twofold serial dilutions of test sera in blocking buffer were added and the mixture was incubated at 37°C for 1 h. After washing, 100 μl of horseradish peroxidase-conjugated goat anti-mouse immunoglobulin G (IgG) secondary antibody (Sigma Chemical Co., St. Louis, MO) was added to each well at a dilution of 1:70,000 in blocking buffer and plates were incubated at 37°C for 1 h. After washing, 100 μl of SureBlue 3,3′,5,5′-tetramethylbenzidine peroxidase substrate (KPL, Gaithersburg, MD) was added to each well and plates were incubated in the dark for 20 min. The reaction was stopped by addition of 1 M sulfuric acid to each plate, and absorbance at 450 nm was recorded. The mean absorbance of four (blank) wells lacking primary antibody was subtracted from the values of all of the other wells. The endpoint titer for experimental samples was the lowest dilution that exceeded the mean plus 2 standard deviations of six negative control samples. Preimmune serum at a dilution of 1:100 served as the negative control for most experiments. For the initial experiment comparing preimmune to postimmunization samples, blank wells served as the negative control. Responses were compared by analysis of variance in Microsoft Excel.
RESULTS
B. mallei pilin is highly immunogenic.
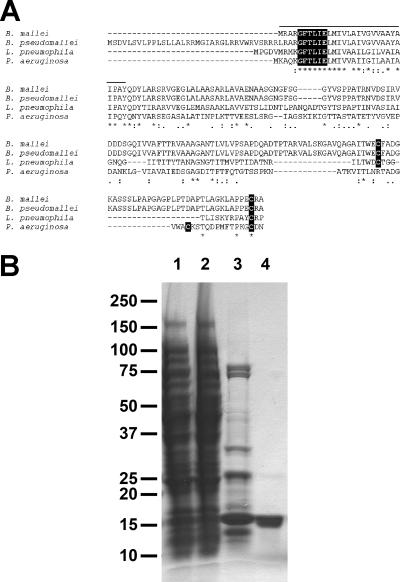
We searched the genome of B. mallei, which at the time was available in an unfinished state on the website of the Institute for Genomic Research, for genes with homology to that encoding the type IV pilin of P. aeruginosa strain PAO1. We found a single open reading frame with characteristics of a type IV pilin gene (Fig. 1A). The putative mature type IV pilin protein of B. mallei is identical to that of B. pseudomallei and closely related to those of other members of the genus. It is also closely related to that of Legionella pneumophila. The predicted protein has the characteristic prepilin peptidase cleavage motif (GFXXXE, where cleavage occurs between G and F), followed by a typical hydrophobic N-terminal sequence, as well as two conserved carboxyl-terminal cysteine residues predicted to form a disulfide bond.
FIG. 1.
Identification and purification of the B. mallei type IV pilin protein. (A) Multiple-sequence alignment of predicted type IV pilin proteins from B. mallei, B. pseudomallei, L. pneumophila strain Philadelphia 1, and P. aeruginosa strain PAO1 was performed with CLUSTAL W version 1.83. Residues identical among all of these sequences are indicated by asterisks, and highly similar and similar residues are indicated by two dots and one dot, respectively. The conserved prepilin peptidase cleavage sites and cysteine residues are highlighted in black, and the hydrophobic N-terminal region of the B. mallei mature pilin omitted in the recombinant soluble purified protein is overlined. (B) Coomassie-stained gel of purified pilin. The total cell lysate (lane 1), flowthrough from nickel affinity chromatography (lane 2), eluate from nickel affinity chromatography (lane 3), and concentrated eluate from gel filtration chromatography (lane 4) are shown. The relative mobility of molecular mass markers (masses are shown in thousands on the left) is indicated.
We overcame several technical difficulties to produce highly purified B. mallei type IV pilin. To avoid problems with solubility due to the presence of the hydrophobic amino terminus, which is predicted to form a long alpha-helix buried within the pilus (4), we omitted the codons for the first 24 amino acids of the protein. To ensure proper disulfide bond formation and folding in the periplasm (27), we fused the truncated protein to the signal peptide of DsbA. For purification, we added an amino-terminal hexahistidine tag, reasoning that this location would allow the tag to protrude away from the rest of the protein (17). We overcame a limitation in expression levels that was apparently due to the high G+C codon usage of B. mallei by addition of a plasmid encoding specific tRNA molecules. Finally, we eliminated contaminating proteins by two rounds of gel filtration chromatography. These strategies allowed us to obtain highly purified protein for further study (Fig. 1B). The identity of the purified protein was verified by immunoblotting with a monoclonal antibody that recognizes the histidine tag (data not shown).
We immunized three mice with purified pilin and injected three control mice with adjuvant alone. All three of the mice immunized with the purified pilin developed strong IgG responses, with titers exceeding 1:320,000. In contrast, the control mice had titers below 1:100.
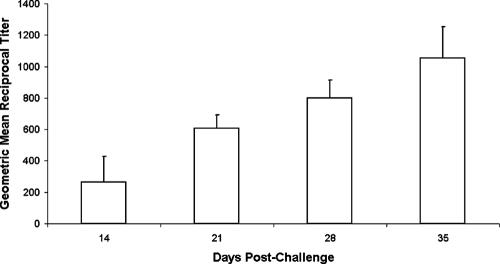
Inhalational challenge with live B. mallei induces an immune response to pilin.
To determine whether pili are produced in vivo and elicit an immune response, five mice were challenged via small-particle aerosol with a sublethal dose of 230 CFU of live B. mallei. Sera were collected weekly and analyzed by ELISA. Four of the five mice developed greater-than-fourfold titer increases (data not shown), and there was a significant increase in the response with time (P = 0.02; Fig. 2). This result suggests that mice infected via the respiratory route with live B. mallei are exposed to pilin protein and develop antibody responses to the antigen.
FIG. 2.
Antipilin antibody titers of mice in response to aerosol infection with live B. mallei. Five mice were infected via small-particle aerosol with 230 CFU of live B. mallei. Serum was drawn at the indicated times and tested by ELISA for IgG antibodies against purified pilin. Columns show the geometric mean reciprocal antibody titers, and error bars show the standard errors of the geometric means. There was a significant increase in titer over time (P = 0.02).
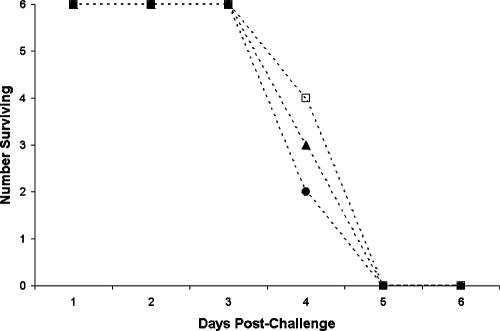
Antibodies against pilin do not protect mice against respiratory B. mallei infection.
Mice immunized with purified pilin protein produced high-titer antibodies. To determine whether these antibodies can protect against infection, we conducted two passive-immunotherapy experiments. In each experiment, groups of five or six mice received 50 μl of pooled hyperimmune serum or pooled control serum from the mice that received adjuvant alone via i.p. injection. An additional group of mice received an i.p. injection of 50 μl of HBSS. One hour later, we challenged all of the animals via small-particle aerosol with live B. mallei. In the first experiment, despite a challenge dose of 1,990 CFU (∼2 LD50s), no mice had succumbed to the infection by day 20. Therefore, all of the mice were sacrificed and the viable B. mallei bacteria in their livers and spleens were enumerated by plate counting. There was no significant difference (P = 0.37) in the geometric mean numbers of CFU recovered from the livers of the mice that received hyperimmune serum (2.9 × 105), control serum (3.4 × 106), or HBSS (2.6 × 105). Similarly, there was no significant difference (P = 0.32) in the geometric mean numbers of CFU recovered from the spleens of these mice (2.2 × 103, 1.6 × 104, and 7.4 × 104, respectively). In a second experiment, similar groups of six mice received 14,261 CFU (approximately 14 LD50s) via small-particle aerosol. All succumbed to infection on either the fourth or the fifth day after the challenge (Fig. 3). Thus, we are unable to conclude that passive immunization with high-titer antipilin serum protects mice against either lethal or sublethal B. mallei infection via the aerosol route.
FIG. 3.
Effect of passive immunization on the survival of mice challenged via aerosol with live B. mallei. Groups of six mice each received i.p. injections of 50 μl of HBSS (solid triangles), pooled serum from three mice sham immunized with adjuvant alone (open squares), or pooled hyperimmune serum from three mice immunized with purified B. mallei pilin (solid circles). One hour later, mice were challenged with 14,261 CFU (approximately 14 LD50s) of live B. mallei via small-particle aerosol. The number of mice surviving on each day postchallenge is shown.
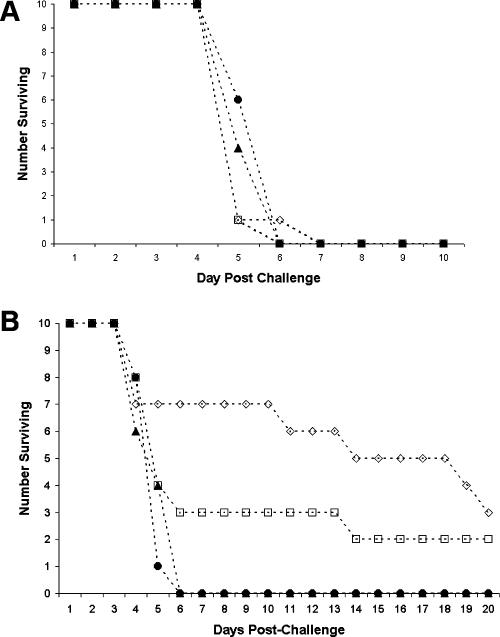
Immunization with pilin does not protect mice against lethal respiratory B. mallei infection.
The failure of passive immunization to protect mice against sublethal or lethal respiratory B. mallei infection does not preclude protection by active immunization, which could involve cell-mediated, as well as humoral, responses or could require higher antibody levels than are attainable by passive immunization. Therefore, we immunized groups of 10 mice with either purified B. mallei pilin or irradiated B. mallei organisms, administered adjuvant alone, or injected them with HBSS. The animals received a booster dose at week 4. Ten weeks after the initial injection, we challenged the mice via small-particle aerosol with 6,965 CFU (∼7 LD50s) of live B. mallei. We found no difference in overall mortality (100% in each group) or time to death (Fig. 4A). We repeated the experiment, this time with a different adjuvant and two booster immunizations at weeks 3 and 7. Preimmune and prechallenge sera were drawn to ensure that the animals had high-titer responses to the pilin. At week 10, the mice were challenged via small-particle aerosol with 21,558 CFU (∼20 LD50s) of live B. mallei. Prior to immunization, no mice had antipilin titers greater than 1:100 and all of the mice immunized with the pilin responded with prechallenge titers greater than or equal to 1:100,000 (geometric mean titer = 1:200,000). In contrast, none of 10 control mice that received adjuvant alone had a prechallenge titer of greater than 1:100. The antibody response in the immunized mice was directed primarily against the pilin protein itself rather than against the histidine tag, as no mice had a titer of greater than 1:2,000 against the His-tagged bundlin type IV pilin protein or against His-tagged BfpU. Nevertheless, there was no significant difference in either total mortality or median time to death (5 days) for mice immunized with pilin versus mice that received adjuvant alone or only saline (Fig. 4B). In contrast, the mice that were immunized with the irradiated organisms survived for a median of 14 days and their overall time to death was significantly longer than that of either the saline control or pilin group (P = 0.001) but not that of the adjuvant control group (P = 0.25).
FIG. 4.
Effect of active immunization on the survival of mice challenged via aerosol with live B. mallei. (A) Ten mice each received HBSS (solid triangles), adjuvant alone (open squares), 50 μg of purified B. mallei pilin (solid circles), or 100 μg of irradiated B. mallei (open diamonds). Booster injections were given at week 4. Ten weeks after the initial injection, all of the mice were challenged via small-particle aerosol with 6,965 CFU (approximately 7 LD50s) of live B. mallei via small-particle aerosol. The number of mice surviving on each day postchallenge is shown. (B) Mice were injected as described for panel A but received an additional booster injection and a different adjuvant. They were challenged with 21,558 CFU (approximately 22 LD50s) of live B. mallei via small-particle aerosol. The number of mice surviving on each day postchallenge is shown.
DISCUSSION
B. mallei causes diseases with important economic impact in many parts of the world and is a proven biological weapon. It is highly infectious when aerosolized and causes a potentially lethal infection in humans that requires prolonged antibiotic therapy. An effective vaccine against B. mallei would be desirable. Type IV fimbriae are important virulence factors for many species of gram-negative bacteria (4). Type IV pilin proteins have proven to be efficacious as subunit vaccines to prevent a variety of infections in animals due to bacteria that produce these fimbriae (3, 7, 13, 14, 21, 22). Therefore, we tested the hypothesis that immunization with the type IV pilin protein of B. mallei would be effective at curtailing morbidity and mortality in an animal model of infection. Although the pilin protein proved to be highly immunogenic, we did not find support for this hypothesis.
There could be several reasons why we did not detect a protective effect of passive or active immunization with the purified pilin protein. For example, there is no doubt that the model we used has limitations. In the natural setting, glanders is spread among solipeds through respiratory secretions, which contaminate feeds and are ingested by other animals, or by inoculation through abraded skin (15). We infected animals via small-particle aerosol because it mimics the route likely to be encountered if B. mallei is used as a biological weapon. However, this route may bypass colonization of the upper respiratory tract, where type IV pili may be expressed and important for initial adherence. Thus, a pilin vaccine might still have utility against infection in the natural setting. Other aspects of the model may also preclude a role for antipilin immunity in protection. For example, type IV fimbriae may not be important in mice but could play an important role in natural hosts or in accidental or intentional human infection.
Alternatively, it could be that active or passive immunization with purified pilin failed to provide protection because type IV pili are not produced during infection and therefore the bacteria are not recognized by antipilin antibodies. However, this does not appear to be the case, as we were able to detect a significant rise in antipilin antibody titer in mice infected via the aerosol route with a sublethal dose of B. mallei. This result suggests that the pili are indeed produced in vivo, although it is conceivable that the mice were exposed to another antigen related to pilin during infection that elicited cross-reactive antibodies. It is also possible that the infecting organisms had preformed pili but that production of pili is rapidly down-regulated during infection. In this case, antibodies against pilin could be generated but would not be able to protect against infection once the bacteria no longer produce the protein. However, the fact that the pilin from the closely related pathogen B. pseudomallei is required for virulence suggests that the B. mallei pili might also be produced during infection (8). Furthermore, though not successful against B. mallei, an antipilin vaccine strategy might be successful in preventing disease due to B. pseudomallei, which expresses an identical pilin protein. Since animals infected with B. mallei produce antibodies against the pilin protein, the purified pilin might also have utility as a serological test for infection with B. mallei or B. pseudomallei. As current methods are inadequate, a sensitive and specific diagnostic test would be welcome (24).
Another possible explanation for the failure of antipilin antibodies to protect against experimental infection concerns the route of immunization. We found that the purified soluble pilin protein was highly immunogenic when administered subcutaneously. However, we did not measure antibody levels in the respiratory tract. It is conceivable that local antibody concentrations were insufficient for protection. Vaccination by another route, such as topical administration to the nasal mucosa, might elicit a protective local response. Alternatively, the antibody response to the pilin may be directed predominantly against epitopes that are not protective.
Immunization with purified pilin elicited robust levels of specific IgG antibodies, but we did not determine whether the antigen also stimulated a potent cell-mediated immune response. B. mallei appears to be a facultative intracellular pathogen that is capable of surviving and multiplying in macrophage-like cell lines (18). It is therefore likely that a cytolytic, cell-mediated immune response is necessary to control the infection and antibodies may play a limited role in protection. Nevertheless, monoclonal antibodies that recognize B. mallei lipopolysaccharide were able to confer passive protection against a B. mallei challenge in a model similar to the one that we used (23). Such antibodies might prevent initial infection before the organism adopts an intracellular lifestyle.
It is noteworthy that mice immunized with irradiated B. mallei organisms plus Freund's adjuvant survived significantly longer than did mice immunized with purified pilin plus Freund's adjuvant or than control mice that received only saline injections. This result requires confirmation, as there was no significant difference between the survival time of mice that received the irradiated organisms and that of the group that received adjuvant alone. There was also no effect of the same antigen with a different adjuvant and administration schedule. Nonetheless, this observation appears to be novel, as previous attempts at B. mallei immunization have not resulted in significant protection (1). If confirmed by further study, efforts to determine which components of the organisms are responsible for the modest degree of protection observed should be pursued in an effort to develop a safe and effective vaccine against this potentially dangerous pathogen.
Acknowledgments
We thank Virginia Lockatell for technical assistance.
This work was supported by Public Health Service awards R03 AI-54690 and R01 AI-37606 from the National Institutes of Health.
Editor: D. L. Burns
Footnotes
Published ahead of print on 2 April 2007.
REFERENCES
- 1.Amemiya, K., G. V. Bush, D. DeShazer, and D. M. Waag. 2002. Nonviable Burkholderia mallei induces a mixed Th1- and Th2-like cytokine response in BALB/c mice. Infect. Immun. 70:2319-2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartlett, J. G. 1992. Glanders, p. 1293-1295. In S. L. Gorbach, J. G. Bartlett, and N. R. Blacklow (ed.), Infectious diseases. W. B. Saunders Company, Philadelphia, PA.
- 3.Cachia, P. J., L. M. Glasier, R. R. Hodgins, W. Y. Wong, R. T. Irvin, and R. S. Hodges. 1998. The use of synthetic peptides in the design of a consensus sequence vaccine for Pseudomonas aeruginosa. J. Pept. Res. 52:289-299. [DOI] [PubMed] [Google Scholar]
- 4.Craig, L., M. E. Pique, and J. A. Tainer. 2004. Type IV pilus structure and bacterial pathogenicity. Nat. Rev. Microbiol. 2:363-378. [DOI] [PubMed] [Google Scholar]
- 5.Craig, L., N. Volkmann, A. S. Arvai, M. E. Pique, M. Yeager, E. H. Egelman, and J. A. Tainer. 2006. Type IV pilus structure by cryo-electron microscopy and crystallography: implications for pilus assembly and functions. Mol. Cell 23:651-662. [DOI] [PubMed] [Google Scholar]
- 6.Daniel, A., A. Singh, L. J. Crowther, P. J. Fernandes, W. Schreiber, and M. S. Donnenberg. 2006. Interaction and localization studies of enteropathogenic Escherichia coli type IV bundle-forming pilus outer membrane components. Microbiology 152:2405-2420. [DOI] [PubMed] [Google Scholar]
- 7.Egerton, J. R., P. T. Cox, B. J. Anderson, C. Kristo, M. Norman, and J. S. Mattick. 1987. Protection of sheep against footrot with a recombinant DNA-based fimbrial vaccine. Vet. Microbiol. 14:393-409. [DOI] [PubMed] [Google Scholar]
- 8.Essex-Lopresti, A. E., J. A. Boddey, R. Thomas, M. P. Smith, M. G. Hartley, T. Atkins, N. F. Brown, C. H. Tsang, I. R. Peak, J. Hill, I. R. Beacham, and R. W. Titball. 2005. A type IV pilin, PilA, contributes to adherence of Burkholderia pseudomallei and virulence in vivo. Infect. Immun. 73:1260-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gill, S. C., and P. H. von Hippel. 1989. Calculation of protein extinction coefficients from amino acid sequence data. Anal. Biochem. 182:319-326. (Erratum, 189:283, 1990.) [DOI] [PubMed] [Google Scholar]
- 10.Hawley, R. J., and E. M. Eitzen, Jr. 2001. Biological weapons—a primer for microbiologists. Annu. Rev. Microbiol. 55:235-253. [DOI] [PubMed] [Google Scholar]
- 11.Heine, H. S., M. J. England, D. M. Waag, and W. R. Byrne. 2001. In vitro antibiotic susceptibilities of Burkholderia mallei (causative agent of glanders) determined by broth microdilution and E-test. Antimicrob. Agents Chemother. 45:2119-2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howe, C., and W. R. Miller. 1947. Human glanders: report of six cases. Ann. Intern. Med. 26:93-115. [DOI] [PubMed] [Google Scholar]
- 13.Lepper, A. W., L. J. Moore, J. L. Atwell, and J. M. Tennent. 1992. The protective efficacy of pili from different strains of Moraxella bovis within the same serogroup against infectious bovine keratoconjunctivitis. Vet. Microbiol. 32:177-187. [DOI] [PubMed] [Google Scholar]
- 14.Lepper, A. W. D., J. L. Atwell, P. R. Lehrbach, C. L. Schwartzkoff, J. R. Egerton, and J. M. Tennent. 1995. The protective efficacy of cloned Moraxella bovis pili in monovalent and multivalent vaccine formulations against experimentally induced infectious bovine keratoconjunctivitis (IBK). Vet. Microbiol. 45:129-138. [DOI] [PubMed] [Google Scholar]
- 15.McGilvray, C. D. 1944. The transmission of glanders from horse to man. Can. J. Public Health 35:268-275. [Google Scholar]
- 16.Ramboarina, S., P. Fernandes, P. Simpson, G. Frankel, M. Donnenberg, and S. Matthews. 2004. Complete resonance assignments of bundlin (BfpA) from the bundle-forming pilus of enteropathogenic Escherichia coli. J. Biomol. NMR 29:427-428. [DOI] [PubMed] [Google Scholar]
- 17.Ramboarina, S., P. J. Fernandes, S. Daniell, S. Islam, P. Simpson, G. Frankel, F. Booy, M. S. Donnenberg, and S. Matthews. 2005. Structure of the bundle-forming pilus from enteropathogenic Escherichia coli. J. Biol. Chem. 280:40252-40260. [DOI] [PubMed] [Google Scholar]
- 18.Ribot, W. J., and R. L. Ulrich. 2006. The animal pathogen-like type III secretion system is required for the intracellular survival of Burkholderia mallei within J774.2 macrophages. Infect. Immun. 74:4349-4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roy, C. J., M. Hale, J. M. Hartings, L. Pitt, and S. Duniho. 2003. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal. Toxicol. 15:619-638. [DOI] [PubMed] [Google Scholar]
- 20.Srinivasan, A., C. N. Kraus, D. DeShazer, P. M. Becker, J. D. Dick, L. Spacek, J. G. Bartlett, W. R. Byrne, and D. L. Thomas. 2001. Glanders in a military research microbiologist. N. Engl. J. Med. 345:256-258. [DOI] [PubMed] [Google Scholar]
- 21.Stewart, D. J., B. L. Clark, J. E. Peterson, D. L. Emery, E. F. Smith, D. A. Griffiths, and I. J. O'Donnell. 1985. The protection given by pilus and whole cell vaccines of Bacteroides nodosus strain 198 against ovine foot-rot induced by strains of different serogroups. Aust. Vet. J. 62:153-159. [DOI] [PubMed] [Google Scholar]
- 22.Sun, D., J. M. Seyer, I. Kovari, R. A. Sumrada, and R. K. Taylor. 1991. Localization of protective epitopes within the pilin subunit of the Vibrio cholerae toxin-coregulated pilus. Infect. Immun. 59:114-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Treviño, S. R., A. R. Permenter, M. J. England, N. Parthasarathy, P. H. Gibbs, D. M. Waag, and T. C. Chanh. 2006. Monoclonal antibodies passively protect BALB/c mice against Burkholderia mallei aerosol challenge. Infect. Immun. 74:1958-1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Waag, D. M., and D. DeShazer. 2004. Glanders, new insights into an old disease, p. 209-238. In L. E. Lindler, F. J. Lebeda, and G. W. Korch (ed.), Biological weapons defense: infectious diseases and counterterrorism. Humana Press, Inc., Totowa, NJ.
- 25.Wheelis, M. 1998. First shots fired in biological warfare. Nature 395:213. [DOI] [PubMed] [Google Scholar]
- 26.Wilkinson, L. 1981. Glanders: medicine and veterinary medicine in common pursuit of a contagious disease. Med. Hist. 25:363-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang, H.-Z., and M. S. Donnenberg. 1996. DsbA is required for stability of the type IV pilin of enteropathogenic Escherichia coli. Mol. Microbiol. 21:787-797. [DOI] [PubMed] [Google Scholar]