Abstract
Most reports dealing with vaccines against botulinum toxin have focused on the injection route of administration. This is unfortunate, because a mucosal vaccine is likely to be more efficacious for patients and pose fewer risks to health care workers and to the environment. Therefore, efforts were made to generate a mucosal vaccine that provides protection against the botulinum serotypes that typically cause human illness (serotypes A, B, and E). This work demonstrated that carboxy-terminal peptides derived from each of the three serotypes were able to bind to and penetrate human epithelial barriers in vitro, and there was no cross inhibition of membrane binding and transcytosis. The three polypeptides were then tested in vivo as a trivalent vaccine that could be administered to mice by the intranasal route. The results indicated that the mucosal vaccine evoked high secretory titers of immunoglobulin A (IgA), as well as high circulating titers of IgG and IgA, and it also evoked a high level of resistance to challenge with toxin. The immunoglobulin responses and the levels of resistance to challenge were increased by coadministration of adjuvants, such as chitosan and vitamin E. At least three mechanisms were identified to account for the antibody-induced resistance: (i) blockade of toxin absorption across epithelial cells, (ii) enhanced clearance of toxin from the circulation, and (iii) blockade of toxin action at the neuromuscular junction. These results are a compelling demonstration that a mucosal vaccine against multiple serotypes of botulinum toxin has been identified.
Botulinum toxin (BoNT) is a uniquely potent agent that is synthesized by the organisms Clostridium botulinum, Clostridium beratii, and Clostridium butyricum. This toxin, which exists in seven different serotypes (serotypes A to G) and more than 40 subtypes (30, 35), causes a serious and potentially life-threatening disease called botulism (12, 14). This disease can occur naturally, but it can also be a result of bioterrorism and biological warfare (3).
All serotypes of BoNT are synthesized as relatively inactive single-chain polypeptides with molecular masses of ca. 150 kDa. These precursors must undergo posttranslational modification (“nicking”), which yields dichain molecules in which a light chain (LC) is linked by a single disulfide bond to a heavy chain (HC). The three-dimensional structures of some of the serotypes have been determined (17, 37). This work has revealed that the molecule is composed of three lobes, which represent LC, the amino-terminal portion of HC, and the carboxy-terminal portion of HC.
Considerable progress has been made in determining the mechanism of toxin action, as well as the structure-function relationships that govern this action (31, 32). Botulinum toxin typically acts as an oral poison, although it can also be an inhalation poison (27). The sequence of events is the same for both routes of exposure (32). The toxin binds to the apical surface of epithelial cells, undergoes endocytosis and transcytosis, and then is released into the general circulation (1, 21, 22). A portion of the toxin escapes from the blood and lymph and reaches the extracellular space, where it acts on peripheral cholinergic nerve endings. The toxin molecule binds with high affinity to the plasma membrane and then undergoes receptor-mediated endocytosis and pH-induced translocation to reach the cytosol. The toxin acts inside cells to cleave polypeptides that are essential for transmitter release. Blockade of exocytosis produces the muscle weakness and paralysis that are hallmarks of the disease botulism (31, 32).
The fact that BoNT can produce a devastating disease, combined with the fact that it is a potential bioterrorism and biological warfare agent, has sparked intense efforts to develop a vaccine. Most current work on a botulism vaccine can be traced to previous preclinical studies of an injectable tetanus vaccine. The tetanus toxin molecule, like the BoNT molecule, is a protein with a molecular mass of ca. 150 kDa (4, 11, 28). It too is composed of three domains that can be designated LC, the amino-terminal portion of HC, and the carboxy-terminal portion of HC. Early studies of isolation and fragmentation of the tetanus toxin molecule led to the discovery that limited proteolysis combined with disulfide bond reduction produced two polypeptides: (i) LC linked to the amino-terminal portion of HC and (ii) the carboxy-terminal portion of HC. The latter was shown to be an efficacious parenteral vaccine against tetanus toxin (10, 13, 20).
Investigators in the BoNT field have subsequently generated the carboxy-terminal portion of HC, both by limited proteolysis of the wild-type toxin and by recombinant techniques. This polypeptide domain has been shown to be an injectable vaccine that is effective against the parent toxin (5, 6).
In a completely different line of research, an effort has been made to identify the minimum essential domain of the BoNT molecule that is needed for binding and penetration of gut and airway epithelial cells (23). This work has demonstrated that (i) the BoNT molecule by itself contains the information for binding and transcytosis across epithelial monolayers, and there is no need for auxiliary proteins that bacteria release in association with the toxin; (ii) both LC and the amino-terminal portion of HC can be removed from the holotoxin, and the residual carboxy-terminal domain is able to cross epithelial barriers; and (iii) the carboxy-terminal domain that undergoes binding and transcytosis retains all of its characteristic structural and functional properties (1, 21-23).
The different lines of research on the BoNT molecule have coalesced in what may be an exciting coincidence of findings. On the one hand, the carboxy-terminal end of HC has the properties of an immunogen. On the other hand, the same polypeptide has the ability to bind to and penetrate epithelial barriers in the gut and airway. These findings suggest that this molecule could be a mucosal vaccine against botulism.
In this report, a substantial body of evidence is presented to show that a mucosal vaccine against botulism has been identified. In addition, this report is the first to describe a recombinant trivalent vaccine against botulism, and it is the first to identify and quantify the various layers of antibody-induced protection against the toxin. Beyond this, the report introduces novel adjuvants to the clostridial toxin field, and it introduces the concept of a universal vaccine to the BoNT literature.
MATERIALS AND METHODS
Toxin.
Homogeneous BoNT type A (BoNT/A) was isolated from bacterial cultures as previously described (9, 30, 34). Homogeneous BoNT/B and BoNT/E were purchased from Metabiologics (Madison, WI). The homogeneity of the preparations was confirmed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) (18).
BoNT/A was isolated in a nicked and biologically active form. BoNT/B and BoNT/E were isolated in the single-chain form and subsequently nicked. To generate the two-chain form of these toxins, the single-chain molecules were proteolytically activated with trypsin. To facilitate subsequent separation of the toxin from the nicking enzyme, l-1-tosylamido-2-phenylethyl chloromethyl ketone-treated trypsin cross-linked to 4% beaded agarose was used (immobilized trypsin; Pierce Chemical, Rockford, IL). The trypsin slurry was washed three times with reaction buffer (10 mM sodium phosphate buffer, pH 7.5). Toxin was added and incubated with the enzyme at room temperature (21°C) for 1 h at a ratio of trypsin to toxin of 1:10. After incubation, the nicked toxin was separated from the beaded trypsin by filtration through a 0.2-μm centrifugal filter (Centrex microfilter unit; Schleicher & Schuell, Keene, NH). The nicked toxin was collected, aliquoted, and stored at −20°C until it was used. A sample of the material was examined by electrophoresis to verify the degree of nicking and the integrity of the dichain toxin.
Iodination.
BoNT/A was iodinated using 125I-Bolton-Hunter reagent, essentially according to the manufacturer's instructions. Pure neurotoxin (300 μg) in 200 μl of borate buffer (pH 7.8) was added to dried iodinated ester and incubated on ice for 15 min. The reaction was terminated by addition of 50 μl of 1 M glycine in borate buffer and incubation for 15 min. The total reaction mixture (250 μl) and rinse (250 μl) were loaded onto a Sephadex G-25 column that was preequilibrated with filtration buffer (150 mM Na2HPO4, 150 mM NaCl, 0.11% gelatin; pH 7.4). The labeled toxin was eluted with filtration buffer, and 0.5-ml fractions were collected. An aliquot (5 μl) of each fraction was assayed to determine the radioactivity. The labeled toxin peak, which eluted at the void volume, was pooled and stored at 4°C. The toxin concentration in the pooled fraction was determined spectrophotometrically at 278 nm using the following relationship: 1.63 A278 units = 1 mg/ml (9).
Iodinated samples were assayed with a gamma-counter to determine the number of disintegrations per minute. Sample concentrations and associated counts were used to calculate the specific activity.
Iodinated toxin purity and biological activity.
The homogeneity of 125I-labeled BoNT/A was determined by SDS-PAGE. The BoNT/A samples were separated on a 10% polyacrylamide gel by the method of Laemmli (18). Gels were run under nonreducing conditions and stained with Coomassie blue, followed by drying under a vacuum (Bio-Rad Laboratories model 224 gel slab dryer) for 2 h. The gels were exposed to Hyperfilm ECL (GE-Amersham Biosciences, Bucks, United Kingdom) for 24 to 48 h and developed using a Kodak O-XMAT film processor (Eastman Kodak Co., Rochester, NY). Developed film was analyzed to determine the presence of a 125I-labeled BoNT/A band (∼150 kDa).
BoNT/A was iodinated three times during the study, and the average specific activity was 2.76 × 102 Ci/mmol. Each batch of toxin was used for ca. 60 days. Aliquots of material that were used in individual experiments during this period were subjected to additional chromatography (Sephadex G-25) prior to use to ensure that free isotope and small polypeptide fragments were removed.
Nomenclature.
According to accepted nomenclature (26), BoNT is the abbreviation for botulinum neurotoxin. LC is the accepted designation for the light chain, and HC is the designation for the heavy chain. Unfortunately, there is no accepted terminology for identifying polypeptides that represent HC fragments that are various lengths. Therefore, in this report, a simple convention is used. HC with a subscript indicates a polypeptide that begins at the carboxy terminus of the HC and has the molecular mass (in kilodaltons) indicated by the subscript. Thus, HC50 is a carboxy-terminal peptide that is derived from the HC and has a molecular mass of 50 kDa.
Cloning, expression, and purification of recombinant HC50 domains of BoNT/A, BoNT/B, and BoNT/E.
Gene segments encoding the HC50 fragments of BoNT/A (strain 62A; amino acids 861 to 1296), BoNT/B (strain Okra; amino acids 853 to 1291), and BoNT/E (strain NCTC 11219; amino acids 840 to 1252) were cloned into the vector pQE30 (QIAGEN, Germantown, MD), yielding expression plasmids pQEHC50 A, pQEHC50 B, and pQEHC50 E, respectively.
Escherichia coli BL21-codon plus(DE3)-RIL (Stratagene, Cedar Creek, TX) was used as the host strain for expression of HC50 domains. Cells were grown in Terrific broth (1.2% peptone, 2.4% yeast extract, 0.94% K2HPO4, 0.22% KH2PO4; Difco, Sparks, MD) at 37°C, with shaking to an A600 of 0.6 to 0.8. Isopropyl-β-d-thiogalactopyranoside (IPTG) at a final concentration of 0.5 mM was added, and the culture was incubated for 12 h at 25°C. The bacteria in 1 liter of an induced culture were harvested by centrifugation (6,000 × g, 15 min) at 4°C.
Cells were suspended in 200 ml of bacterial protein extract reagent (Pierce, Rockford, IL) at 4°C. Lysozyme (Sigma, St. Louis, MO) at a final concentration of 0.1 mg/ml, DNase (Sigma) at a final concentration of 0.01 mg/ml, and a protease inhibitor cocktail (Roche, Indianapolis, IN) were added to the cell suspension and incubated on a rotating shaker for 2 h. Four hundred milliliters of 50 mM sodium phosphate buffer containing 300 mM NaCl (pH 8.0) was added to the lysed cell suspension and allowed to stand for 30 min. The suspension was centrifuged at 27,000 × g for 40 min to remove the precipitate.
The clear supernatant was loaded onto a 5-ml column of Ni-nitrilotriacetic acid Superflow (QIAGEN) which was equilibrated with 50 mM sodium phosphate buffer containing 300 mM NaCl (pH 8.0). The column was washed with 50 volumes of washing buffer (50 mM sodium phosphate buffer containing 300 mM NaCl and 20 mM imidazole; pH 8.0). Bound protein was eluted from the column with an imidazole gradient (20 to 250 mM imidazole in 50 mM sodium phosphate buffer containing 300 mM NaCl [pH 8.0]). The active fractions (which eluted with ∼100 mM imidazole) were pooled and dialyzed against 50 mM sodium phosphate (pH 6.8). The dialysate was centrifuged at 27,000 × g for 30 min to remove the precipitate.
The clear supernatant was loaded onto a cation-exchange column containing 4 ml of CM Sepharose Fast Flow (GE-Amersham Bioscience) equilibrated with 50 mM sodium phosphate (pH 6.8). The column was washed with 50 volumes of 50 mM sodium phosphate (pH 6.8). Bound protein was eluted from the column with an NaCl gradient (50 to 500 mM NaCl in 50 mM sodium phosphate buffer [pH 6.8]). The active fractions (which eluted with ∼200 mM NaCl) were pooled and dialyzed against 50 mM sodium phosphate (pH 7.4). Approximately 15 to 20 mg of each HC50 polypeptide was obtained from 1 liter of bacterial culture. The purity of the HC50 polypeptides was confirmed by 10% SDS-PAGE.
Western blot analysis.
Rabbit and mouse antisera against HC50/A, HC50/B, and HC50/E were prepared in our laboratory. For Western blotting, samples were separated under reducing conditions by 10% SDS-PAGE using a Mini-Protean III electrophoresis cell (Bio-Rad Laboratories, Hercules, CA). Proteins were then transferred to a Nitropure nitrocellulose membrane using a Mini Trans-Blot electrophoretic transfer cell (Bio-Rad Laboratories) in Tris-glycine transfer buffer at 75 V for 90 min, as described by Towbin et al. (38). Blotted membranes were rinsed with phosphate-buffered saline-0.05% Tween 20 (PBST) (pH 7.5) and blocked with 5% nonfat powder milk in PBST at room temperature. For identification of recombinant toxin fragments, the membranes were washed three times with PBST and then incubated with the appropriate antiserum at a 1:5,000 dilution in PBST with 0.5% nonfat powdered milk at 4°C overnight. The membranes were then washed three times with PBST and incubated with secondary antibody at a 1:10,000 dilution in PBST with 0.5% nonfat powder milk for 1 h at room temperature. After this the membranes were washed three times with PBST at room temperature and visualized using SuperSignal West Pico chemiluminescence (Pierce Chemical) according to the manufacturer's instructions. The membranes were exposed to Hyperfilm ECL film (GE-Amersham Biosciences) for times adequate to visualize the chemiluminescent bands. HC50 fragments were identified by comparison with known protein standards.
Cell culture.
T-84 human epithelial cells were grown in a l:1 mixture of Dulbecco's modified Eagle's medium containing 1 g/liter d-glucose and Ham's F-12 nutrient medium supplemented with 5% newborn calf serum, 100 U/ml penicillin, 100 μg/ml ampicillin, and 15 mM HEPES. Cultures were maintained at 37°C in 6% CO2. T-84 cells were fed every 3 days and passaged (1:2) when they were 95% confluent, approximately every 6 days. Passages 65 through 90 were used for experiments described below.
Transcytosis assay.
Cells were grown in Transwell porous-bottom dishes on polycarbonate membranes with a 0.4-μm pore size. The growth area within each insert was 1.12 cm2. The Transwells were coated with 10 μg/cm2 rat tail collagen type 1. The coated wells were allowed to dry at room temperature overnight (18 h). After drying, the wells were sterilized under UV light for 1 h, which was followed by preincubation with cell culture medium (30 min). The preincubation medium was removed immediately before addition of cells and fresh medium.
T-84 cells were plated at a confluent density (ca. 1.5 × 105 cells) in the Transwells with 0.5 ml of medium in the upper chamber and 1.0 ml of medium in the lower chamber. The medium in the upper chamber bathed the apical (or mucosal) surface of cells, and the medium in the lower chamber bathed the basolateral (or serosal) surface of cells. The culture medium was changed every 2 days. The cultures were allowed to differentiate for at least 10 days before a transcytosis assay was performed. The formation of tight junctions was confirmed experimentally by measuring transepithelial electrical resistance. Experiments were performed with cultures that were between 10 and 15 days old.
The transcytosis assay was initiated by adding BoNT or HC50 to the upper chamber. Transport of these molecules was monitored for 18 to 20 h by collecting all of the medium from the bottom chamber. An aliquot (0.5 ml) of each sample was filtered through a Sephadex G-25 column, and 0.5-ml fractions were collected. The amount of polypeptide that crossed epithelial monolayers was determined in various ways, as described in Results.
Neuromuscular transmission.
Mouse phrenic nerve-hemidiaphragm preparations were excised and placed in tissue baths to assay the toxicity of BoNT in biological specimens (15). The tissues were suspended in physiological buffer that was aerated with 95% O2 and 5% CO2 (33). Phrenic nerves were stimulated continuously (0.2 Hz; 0.1- to 0.3-ms pulses), and muscle twitch was recorded. Toxin-induced paralysis was defined as a 90% reduction in the muscle twitch response to neurogenic stimulation.
Vaccination protocol.
Animals (18- to 20-g female BALB/c mice; Charles River Laboratories, Wilmington, MA) were immunized by the intranasal (i.n.) route or by the intramuscular (i.m.) route. For the former route, individual antigens or combinations of antigens (20 μg each) were administered by a single application of 20 μl of a phosphate-buffered saline solution (pH 7.4) to the nares of mice. For the latter route, antigens (5 or 20 μg) were administered in a single bolus (50 μl) of a phosphate-buffered saline solution. In both cases, animals received a prime dose at zero time and booster doses on days 14 and 28.
In some experiments, antigen was admixed with an adjuvant prior to administration. Two mucosal adjuvants (1% [wt/vol] chitosan and 5% [wt/vol] vitamin E TPGS) and one parenteral adjuvant (0.2% [wt/vol] alum) were tested.
In addition to the traditional modes of vaccine administration (e.g., exclusively i.n. or exclusively i.m.), one mixed mode of administration was tested. This involved an initial or prime dose administered by the injection route and two subsequent booster doses administered by the mucosal route. When an adjuvant was included, alum was used for the prime dose and vitamin E was used for each booster dose.
In all vaccination paradigms, biological specimens (blood and serum) were collected on day 42. Within 1 to 5 days of specimen collection, animals were challenged with BoNT. Survivors were monitored for >1 week, an amount of time that exceeds the time necessary to detect 1 50% lethal dose (LD50) (96 h).
Enzyme-linked immunosorbent assay (ELISA).
Antibody titers in mouse serum were determined by standard procedures. Briefly, flat-bottom, 96-well Corning plates (Corning Incorporated, Corning, NY) were coated with the HC50 domains of BoNT (300 ng/well) and incubated at 4°C overnight, followed by washing with phosphate-buffered saline containing 0.1% Tween 20 (pH 7.4). The plates were blocked with 1% bovine serum albumin. Twofold serial dilutions of serum samples were added to the plates and incubated at 37°C for 60 min. Immunoglobulin G (IgG) titers were determined using peroxidase-conjugated goat anti-mouse IgG (Sigma-Aldrich, Inc., St. Louis, MO), and IgA titers were determined using peroxidase-conjugated goat anti-mouse IgA (Santa Cruz Biotechnology, Inc., Santa Cruz, CA). Secondary antibodies were diluted 1:1,000 in phosphate-buffered saline. The primary and secondary antibodies were incubated for 30 min at 37°C, after which 2,2′-azinobis(3-ethylbenthiazoline-6-sulfonic acid) was added as a substrate, and the plates were incubated for an additional 30 min at 37°C. The end point titers were the reciprocals of the last dilutions yielding an absorbance at 405 nm that was greater than the control value (preimmune serum).
Antibody titers were also determined for bronchoalveolar lavage (BAL) samples from mice. Specimens were obtained by anesthetizing animals with pentobarbital sodium (Nembutal; 50 mg/kg, given intraperitoneally [i.p.]). The complete lung along with the trachea was excised, and BAL samples were collected from individual mice by internal flushing through the trachea with cold 50 mM phosphate-buffered saline (pH 7.6) containing Complete protease inhibitors (Roche, Indianapolis, IN). The samples collected (1.5 ml per mouse) were then centrifuged at 6,000 rpm at 4°C for 10 min. Supernatants were collected and stored at −4°C for subsequent analysis.
The levels of antigen-specific secretory IgA in BAL samples were determined using an ELISA kit (Bethyl, Montgomery, TX). Briefly, 96-well polystyrene plates were coated with HC50 domains (100 μl, 20 μg/ml protein) in 0.05 M carbonate-bicarbonate buffer (pH 9.6). The plates were incubated at 37°C for 1 h and then overnight at 4°C. The plates were washed with buffer (50 mM Tris, 0.14 M NaCl, 0.05% Tween 20; pH 8.0) and blocked with 200 μl of 1% bovine serum albumin (Sigma) in Tris-NaCl buffer for 2 h at 37°C. After two washes with buffer, 100-μl portions of serially diluted BAL samples (starting at a 1:10 dilution in Tris-NaCl-Tween 20 buffer containing 1% bovine serum albumin) were added to the plates, which were incubated for 1 h at 37°C. The secretory IgA was detected by adding 100 μl/well of a 1:5,000 dilution of peroxidase-conjugated goat anti-mouse IgA antibody. Color was developed by adding 100 μl/well of a 1-mg/ml ortho-phenylenediamene substrate solution in sodium citrate buffer (pH 5.0) containing 2 μl of 30% H2O2. After incubation for 15 to 20 min at room temperature, the reaction was stopped using 50 μl of 2 N H2SO4. The optical density at 490 nm was determined using an ELISA reader (VERSA max; Molecular Devices).
Challenge with toxin.
The most characteristic outcome of BoNT action is neuromuscular blockade. This outcome is easily discernible as weakness and eventual paralysis of the muscles of locomotion and the muscles of respiration. During bioassays of resistance, as well as the associated experiments with antiserum, animals received doses of toxin sufficient to produce paralysis of respiration and death within minutes (ca. 100 to 120 min). To minimize the pain and suffering, animals were observed throughout the various protocols. When signs of neuromuscular weakness became obvious, animals were sacrificed in accordance with AAALAC guidelines (e.g., with CO2).
Blood and organ levels of toxin.
Iodinated BoNT/A was administered intravenously to mice via the tail vein, and 30 min later specimens were obtained by retroorbital bleeding. Experiments were performed using control animals (toxin only) and experimental animals (toxin preincubated with antiserum from vaccinated animals). The goal of the experiments was to determine the extent of toxin clearance in animals that had a circulating titer of antibody adequate to completely neutralize the dose of toxin administered.
In addition to monitoring the levels of toxin in blood, one set of experiments determined the extent of local toxin accumulation in tissues. Mice were anesthetized by administration of pentobarbital sodium (50 mg/kg), after which the thorax was opened and the heart was exposed. A butterfly needle (23 gauge) was inserted into the left ventricle, an incision was made in the right ventricle, and the body of the animal was perfused with a heparinized solution of phosphate-buffered saline (45 to 60 ml). Six major organs were removed from the body (liver, spleen, kidney, lung, brain, and heart), and the accumulation of iodinated toxin was determined.
RESULTS
BoNT/A HC50 is a mucosal vaccine.
In previous work, an effort has been made to identify the minimum essential domain of the BoNT molecule that retains full competence to bind to and penetrate human gut and airway epithelial cells. To date, this work has demonstrated that HC, HC88, HC66, and HC50 of BoNT/A all have within them the properties of a minimum essential domain (22, 23). In a parallel series of experiments, an effort has been made to identify an antigen that can act by the mucosal route (oral and/or inhalation) to evoke resistance to homologous toxin. This work has demonstrated that a modified botulinum holotoxin with point mutations in the histidine motif (15), as well as a full-length HC without modifications (27), can act as mucosal vaccines.
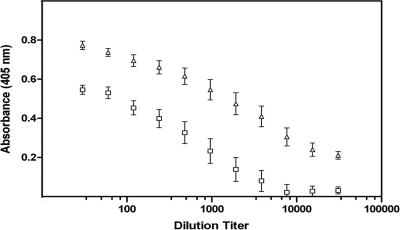
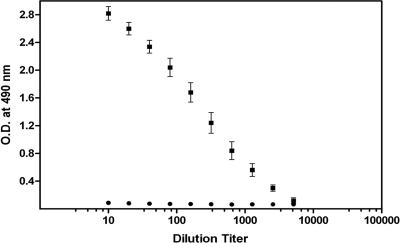
The current studies are a continuation of previous work on a minimum essential domain for binding and transcytosis and on an immunogenic domain that can act by the mucosal route to evoke resistance. Thus, BoNT/A HC50 is a rational choice for evaluation as a potential i.n. vaccine. Mice (n = 10) were vaccinated with this polypeptide i.n. (20 μg in 20 μl) at time zero, 14 days, and 28 days. Fourteen days after the final boost, aliquots of blood were obtained to determine the circulating levels of antibody. The results of the ELISA, which are shown in Fig. 1, demonstrate that there was a substantial IgG response and a more modest IgA response.
FIG. 1.
Immunoglobulin responses to the HC50 domain of BoNT/A. The polypeptide was administered to mice (n = 10) as an i.n. vaccine. Two weeks after the second booster, the dilution titers for IgG (▵) and for IgA (□) in serum were determined. The data show that mucosal vaccination evoked circulating titers of both antibodies.
Both control animals and vaccinated animals were challenged i.p. with BoNT/A (1 × 103 LD50 in 50 μl). As expected, control animals became seriously ill within a short time (100 min or less). Vaccinated animals survived the challenge, and there was never any evidence of illness.
The addition of an adjuvant enhances the immunoglobulin response to BoNT/A HC50.
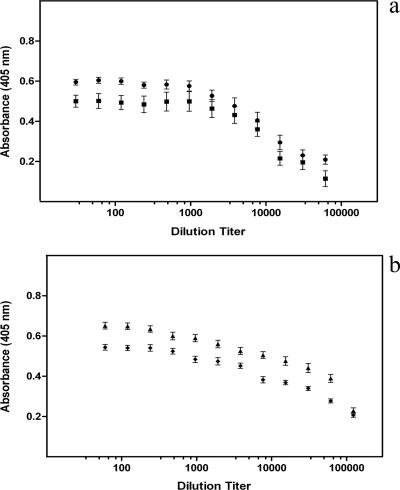
Mice (10 mice per group) were vaccinated with BoNT/A HC50 as described above in the absence or presence of an adjuvant. As described in Materials and Methods, two types of adjuvants were tested (chitosan and vitamin E). As shown in Fig. 2, both chitosan and vitamin E increased the levels of the immunoglobulin responses. The results of a quantitative comparison of the immunoglobulin responses in the absence and presence of adjuvant are shown in Table 1.
FIG. 2.
Immunoglobulin responses to the HC50 domain of BoNT/A when it was coadministered with an adjuvant. (a) The polypeptide was administered to mice (10 mice per group) as an i.n. vaccine with chitosan (▪) or with vitamin E (•), and the magnitudes of the IgG responses were determined. (b) The polypeptide was administered to mice (10 mice per group) as an i.n. vaccine with chitosan (⧫) or with vitamin E (▴), and the magnitudes of the IgA responses were determined. The adjuvants enhanced the responses to both immunoglobulins, but the effect with IgA was greater. This was probably a reflection of the fact that the response to IgA in the absence of adjuvant (see Fig. 1) was lower.
TABLE 1.
Fifty percent dilution titers of sera from mice vaccinated with BoNT/A HC50
| Adjuvant | Immunoglobulin titers
|
|
|---|---|---|
| IgG | IgA | |
| None | 1:4,000 | 1:800 |
| Chitosan | 1:10,000 | 1:40,000 |
| Vitamin E | 1:20,000 | 1:80,000 |
The results of the i.p. challenge experiments (1 × 103 mouse LD50 in 50 μl) were identical to those described above. Thus, control animals succumbed to the effects of toxin within ca. 100 min, but vaccinated animals never developed signs of botulism, even when they were monitored for an extended time (>1 week).
BoNT HC50, in the absence or presence of an adjuvant, can function as an injection vaccine.
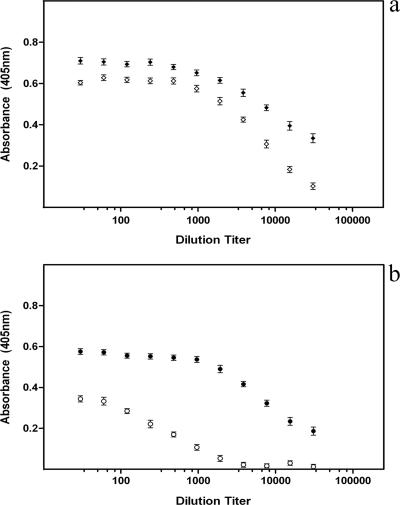
Several investigators have shown that the HC50 domains of tetanus toxin and BoNT can evoke immunity to the parent holotoxins (see the introduction for references). This work typically involved administration of an adjuvant (alum) (see Materials and Methods) but did not typically involve measurement of circulating IgA titers. Therefore, mice (n = 10) were vaccinated by i.m. injection (5 μg BoNT/A HC50 in 50 μl) in the absence or presence of an adjuvant (alum). Fourteen days after the second booster, aliquots of blood were obtained for determination of the immunoglobulin responses. In addition, animals were challenged with holotoxin by the i.p. route.
In the absence of the adjuvant the HC50 polypeptide evoked a strong IgG response, and in the presence of the adjuvant this response was somewhat elevated (Fig. 3a). In the absence of the adjuvant there was a modest IgA response, but in the presence of the adjuvant there was a strong response (Fig. 3b).
FIG. 3.
Immunoglobulin responses to the HC50 domain of BoNT/A administered as an injection (i.m.) vaccine. The polypeptide was given to mice (10 mice per group) in the absence (open symbols) or in the presence (solid symbols) of an adjuvant (alum). (a) Magnitudes of IgG responses. (b) Magnitudes of IgA responses. The adjuvant enhanced the responses to both classes of immunoglobulin, and the magnitude of the enhancement was substantial for IgA.
Two types of challenge experiments were performed. Vaccinated animals that did not receive an adjuvant, as well as the matched controls, were challenged i.p. with 1 × 103 mouse LD50 (50 μl). As described above, all control animals were seriously ill after 100 min or less. All vaccinated animals survived without any signs of illness for >1 week. Vaccinated animals that received the adjuvant, as well as matched controls, were challenged i.p. with 1 × 104 mouse LD50 (50 μl). Again, the control animals were clearly ill within a matter of minutes, whereas the vaccinated animals survived without illness for an extended time (>1 week).
HC50 domain of BoNT/A can function as a mixed-mode vaccine.
The most rational approach for vaccine administration may not be solely by the injection route or solely by the mucosal route. A realistic alternative may be to use a combination of the two. Therefore, mice were vaccinated by combining an initial injection (20 μg of antigen in 50 μl physiological saline, given i.m.) at time zero with two boosters (20 μg of antigen in 20 μl physiological saline, given i.n.) at 14 and at 28 days. Alum was used as the adjuvant for the initial injection, and vitamin E was used as the adjuvant for the subsequent i.n. boosters.
Fourteen days after the final booster, aliquots of blood were obtained to determine the circulating titers of IgG and IgA. As shown in Fig. 4, the mixed mode of vaccine administration evoked substantial responses for both classes of immunoglobulin. The magnitudes of these responses were comparable to the magnitudes observed after i.m. injection alone (Fig. 3) and after i.n. administration alone (Fig. 2).
FIG. 4.
Immunoglobulin responses to the HC50 domain of BoNT/A when it was administered as a mixed-mode vaccine. The polypeptide was given to mice (n = 10) in an initial i.m. injection with alum as an adjuvant and in two subsequent i.n. boosters with vitamin E as an adjuvant. The results demonstrated that the mixed-mode vaccination paradigm elicited substantial IgG (⧫) and IgA (•) responses.
Vaccinated animals and control animals were challenged i.p. with the holotoxin (1 × 103 mouse LD50 in 50 μl), and the results were consistent with the results described above. All control animals succumbed to the poison within minutes (120 min or less), and all mixed-mode-vaccinated animals survived without signs of illness for >1 week.
BoNT/B HC50 and BoNT/E HC50 can bind to and penetrate monolayers of human epithelial cells.
The HC, HC88, HC66, and HC50 domains of BoNT/A have all been shown to cross barriers formed by immortalized human epithelial cells (T-84 and Caco-2) (1, 22, 23), as well as barriers formed by primary human epithelial cells (A. B. Maksymowych and L. L. Simpson, unpublished data). This process involves binding of polypeptide to the apical surface, endocytosis, and transcytosis, followed by release of polypeptide on the basolateral surface. Therefore, experiments to assess the abilities of BoNT/B HC50 and BoNT/E HC50 to cross epithelial barriers were performed.
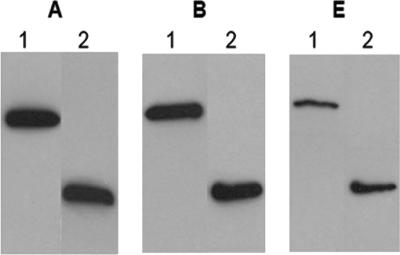
T-84 cells were grown in a Transwell apparatus, as described in Materials and Methods. BoNT/B holotoxin and its HC50 domain, as well as BoNT/E holotoxin and its HC50 domain, were added to the apical surface of epithelial cells, and the accumulation of these polypeptides on the basal side of cells was monitored. Parallel experiments were done with BoNT/A holotoxin and its HC50 domain for comparison. The results (Fig. 5) revealed that the HC50 subunit of each serotype and the homologous neurotoxin at an equimolar concentration were comparable in terms of the ability to penetrate monolayers of human epithelial cells. These results make it clear that the minimum essential domain for transcytosis of each serotype is localized in the HC50 domain.
FIG. 5.
Transcytosis of BoNT/A HC50 (gel A), BoNT/B HC50 (gel B), and BoNT/E HC50 (gel E). Equimolar concentrations of the three polypeptides (1 × 10−8 M) or the corresponding parent toxins were added to the upper wells of T-84 monolayers in a Transwell apparatus, and the accumulation in the lower wells was assayed by Western blotting. Lane 1, holotoxin added; lane 2, HC50 domains added. Note that the levels of transcytosis for each holotoxin and its HC50 domain were comparable.
Transcytosis in the presence of multiple serotypes.
Research on multivalent vaccines appears to reflect two expectations: (i) vaccination should evoke resistance to multiple serotypes of toxin, but (ii) protection is needed for only one serotype at a time. Although it is appropriate to expect that a multivalent vaccine will provide protection against several serotypes, it may not be appropriate to expect that a bioterrorism or biological warfare incident will involve only one serotype at a time. Therefore, experiments were performed to monitor transcytosis of multiple serotype polypeptides given together.
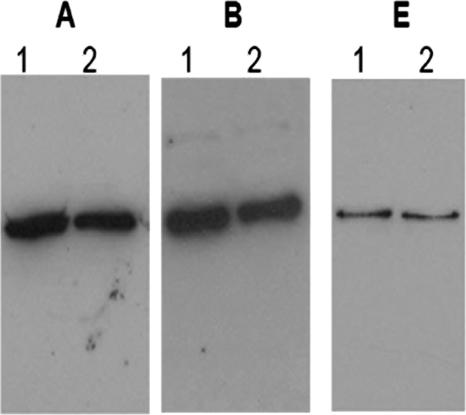
Figure 6 shows the results of experiments in which the three serotypes of greatest concern to human health (serotypes A, B, and E) were added simultaneously to the apical surfaces of epithelial cells. As this figure shows, the transcytosis of each HC50 domain remained constant, regardless of whether the domain was added alone or with other domains.
FIG. 6.
Individual and combined rates of transcytosis of BoNT/A HC50 (gel A), BoNT/B HC50 (gel B), and BoNT/E HC50 (gel E). Equimolar concentrations of the three polypeptides (1 × 10−8 M) were added to the apical surfaces of T-84 monolayers, and the accumulation of the polypeptides on the basal side of the cells was assayed by Western blotting. Lane 1, HC50 domain added alone; lane 2, three HC50 domains added together. The results indicate that simultaneous addition of HC50 domains did not inhibit or reduce the extent of transcytosis of any of the domains.
Multiple HC50 domains can be administered simultaneously to create a multivalent mucosal vaccine.
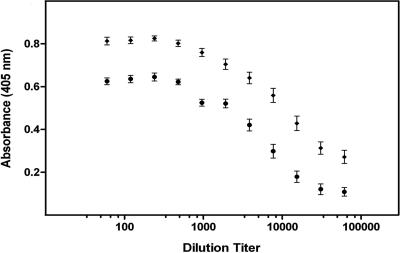
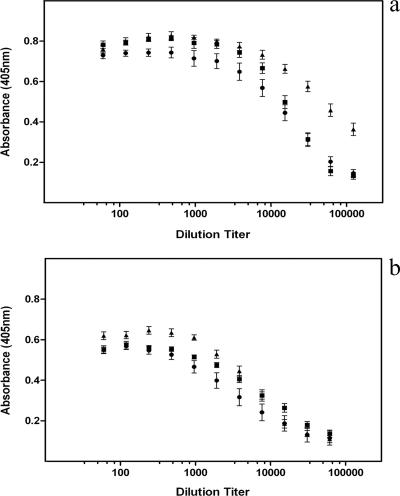
The HC50 domains of BoNT/A, BoNT/B, and BoNT/E were administered together (20 μg each) in the presence of vitamin E as an i.n. vaccine. A total of 20 mice were vaccinated. At the end of the protocol, animals were randomly assigned to two groups containing 10 mice each that were challenged by the i.n. route or the i.p. route.
The ELISA data indicated that all three antigens evoked a substantial IgG response (Fig. 7a) and a substantial IgA response (Fig. 7b). These data provide further support for the premise that combined administration of three antigens does not lead to inhibition of absorption of any one of the antigens. Also, as a comparison of Fig. 7 with Fig. 2 shows, the magnitude of the immunoglobulin response for an individual antigen in the trivalent formulation (e.g., BoNT/A HC50) was in the same range as the magnitude of the immunoglobulin response for the individual antigen in a monovalent formulation. Thus, simultaneous administration of multiple antigens did not result in immune suppression.
FIG. 7.
Immunoglobulin responses to i.n. administration of a trivalent vaccine. The HC50 domains of three serotypes were administered as described in the text, and the magnitudes of the IgG responses (a) and IgA responses (b) were determined. The results indicate that all three antigens evoked substantial responses. ▴, BoNT/A; ▪, BoNT/B; •, BoNT/E.
Mice were challenged by two routes with BoNT, i.p. (n = 10) and i.n. (n = 10). For each route of administration, half of the mice received 1 × 103 mouse LD50 (n = 5), and the other half received 1 × 104 mouse LD50 (n = 5). In addition, animals were challenged simultaneously with all three serotypes (serotypes A, B, and E), and thus the cumulative dose was either 3 × 103 LD50 or 3 × 104 LD50. Control animals that received either 3 × 103 or 3 × 104 LD50 became seriously ill within minutes. By contrast, all vaccinated animals survived at least 1 week, regardless of the dose or the route of challenge. This means that not only were animals protected against a substantial monovalent challenge, but they were also protected against a substantial polyvalent challenge.
HC50 domains of BoNT/A, BoNT/B, and BoNT/E can be administered simultaneously to create a multivalent mixed-mode vaccine.
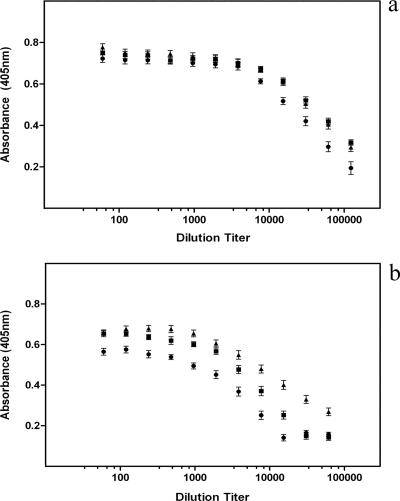
Mice were vaccinated by combining an initial injection of antigens with two subsequent i.n. administrations of antigens. For the initial i.m. injection, all three antigens (20 μg each) were mixed with alum prior to administration. For the subsequent boosters, all three antigens (20 μg each) were mixed with vitamin E prior to administration. Fourteen days after the last booster, aliquots of blood were obtained to determine the circulating titers of IgG and IgA. At the same time, animals were randomly assigned to two groups (10 mice per group) for inhalation challenge and i.p. challenge.
The results obtained with the multivalent mixed-mode vaccine (Fig. 8a and b) were similar to the results obtained with the multivalent mucosal vaccine (Fig. 7a and b). Thus, all three of the HC50 domains evoked substantial IgG and IgA responses.
FIG. 8.
Immunoglobulin responses to mixed-mode administration of a trivalent vaccine. The HC50 domains of three serotypes were administered as described in the text, and the magnitudes of the IgG responses (a) and IgA responses (b) were determined. The results clearly show that all three antigens evoked substantial responses. ▴, BoNT/A; ▪, BoNT/B; •, BoNT/E.
Mice were challenged with toxin by two routes of administration, as described above. As before, animals received a combination challenge in which serotype A, B, and E toxins were given together (1 × 104 mouse LD50 each). Similar to the results obtained with mucosal vaccination, the results obtained with mixed-mode vaccination revealed that all control animals quickly became ill (<80 min), whereas the vaccinated animals survived without signs of illness (>1 week).
Antibodies can associate with toxin to block binding and transcytosis across epithelial cells.
There are several possible mechanisms by which antibodies directed against BoNT can diminish or eliminate the lethal effects of the molecule. One obvious possibility is that these antibodies bind at or near the toxin domain responsible for association with epithelial cells, which in turn would block absorption of the toxin molecule. This possibility was assessed by using BoNT/A as a prototype.
There are two potential sources of antibody that could act to block toxin absorption: (i) secretory IgA generated in the lumen of the airway and (ii) circulating immunoglobulin that is transported into the lumen. Experiments described above demonstrated that mucosal vaccination led to a robust circulating IgA response. It was necessary to show that an identical vaccination paradigm would elicit a strong secretory IgA response.
Mice (n = 5) were vaccinated i.n. using BoNT/A HC50 as a prototype. As described above, there was an initial administration, followed by two boosters (20 μg per administration), each of which was given with vitamin E as an adjuvant. Two weeks after the final boost, animals were sacrificed, and BAL samples were obtained. The ELISA titers for antigen-specific secretory IgA revealed that there was a substantial response (Fig. 9).
FIG. 9.
Mucosal antibody responses to vaccination with BoNT/A HC50. The antigen was administered as an i.n. vaccine in combination with vitamin E, and the magnitude of the secretory IgA response was determined (▪). The data show that there was a substantial response. A matched group of animals was vaccinated by the i.m. route (antigen plus alum), and again the responses were measured. As expected, parenteral administration of the HC50 domain did not evoke a significant mucosal antibody response (•). O.D., optical density.
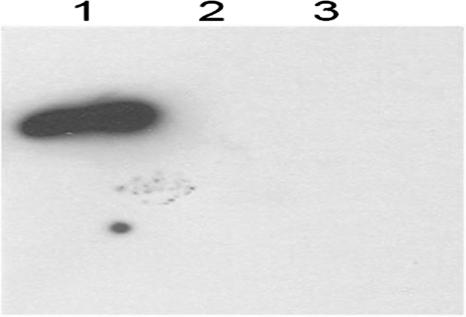
Secretory IgA (0.1 ml of lavage fluid) or a combination of circulating IgG and IgA (0.1 ml of antiserum) was obtained from vaccinated animals and incubated with BoNT/A (1 × 10−8 M). After 30 min, the mixtures were added to the apical surfaces of T-84 monolayers in a Transwell apparatus. Medium in the basal chamber was collected and handled as described in Materials and Methods. Aliquots were used for Western blot analyses, as shown in Fig. 10. As expected, untreated toxin was able to bind to and penetrate epithelial barriers, whereas antibody-pretreated toxin had virtually no ability to cross these barriers.
FIG. 10.
Effect of neutralizing antibodies on binding and transcytosis of BoNT/A. Toxin (1 × 10−8 M) was incubated alone or with BAL samples (0.1 ml) or antiserum (0.1 ml) obtained from mice that had been immunized with BoNT/A HC50 vaccine. After incubation (1 h), the solutions were added to apical wells containing monolayers of epithelial cells, and transcytosis was monitored. The results demonstrated that untreated toxin crossed epithelial barriers (lane 1) but antibody-pretreated toxin did not cross these barriers (lane 2, antiserum; lane 3, BAL sample).
Antiserum from immunized animals promotes toxin clearance from the general circulation and enhances accumulation in the liver and spleen.
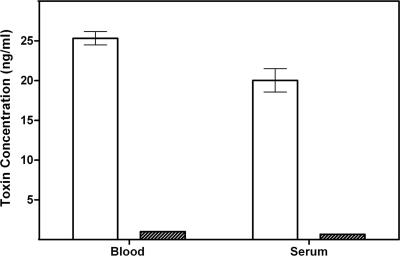
Control mice (three or more mice per group) received a single intravenous bolus of 125I-labeled BoNT/A, and 30 min after this aliquots of blood were collected and assayed to determine the presence of toxin. The total duration of the experiment was (i) less than the half-time for toxin elimination from the general circulation and (ii) less than the time necessary for significant metabolic transformation of toxin in blood (29). Experimental animals received an equivalent dose of toxin that had been preincubated with a neutralizing dose of antiserum collected from animals that received trivalent vaccine (0.01 ml; 30 min of incubation; room temperature). The data revealed that neutralizing antibody greatly increased the rate of toxin clearance from the blood (Fig. 11). The toxin levels in the blood and serum of experimental animals were approximately 1 order of magnitude less than those in control animals.
FIG. 11.
Effect of neutralizing antibodies on the circulating levels of BoNT/A. 125I-labeled BoNT/A was incubated alone (open bars) or with antiserum (cross-hatched bars) from animals that had been immunized with trivalent mucosal vaccine (0.01 ml; 30 min; room temperature). Mice were injected intravenously with the material, and 30 min later samples of blood were collected. The results demonstrated that neutralizing antibodies resulted in a dramatic reduction in blood and serum levels of toxin.
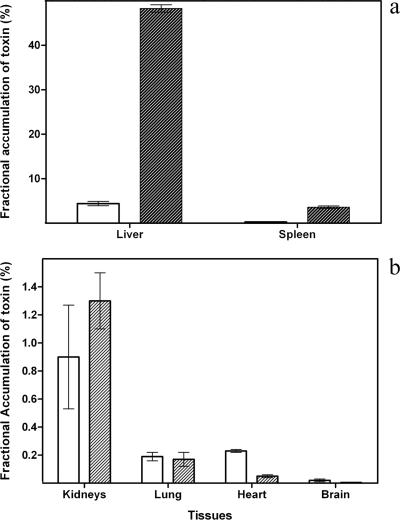
The BoNT molecule (ca. 150 kDa), especially when the toxin molecule is decorated with antibody, is too large to undergo significant renal clearance. On the other hand, hepatic uptake and splenic uptake are likely mechanisms for clearance of an antigen-antibody complex. Therefore, 125I-labeled BoNT/A was injected into control animals and vaccinated animals as described above, and 30 min later the animals were anesthetized and perfused. The livers and spleens were subsequently excised and assayed to determine the accumulation of toxin (Fig. 12a). In control animals the percentage of the total dose administered that could be recovered in the liver was 4.43%, and in experimental animals the percentage that could be recovered in the liver was 48.3%; the difference was quantitatively (ca. 11-fold) and statistically (P < 0.001) significant. Similarly, the percentage of the total dose administered that could be recovered in the spleens of control animals was 0.3%, whereas the percentage that could be recovered in the spleens of experimental animals was 3.6%; the difference was also quantitatively (12-fold) and statistically (P < 0.001) significant. The levels of labeled BoNT/A were also determined for four other tissues (kidney, lung, heart, and brain). As shown in Fig. 12b, neutralizing antiserum did not result in enhanced accumulation of toxin in any of these tissues.
FIG. 12.
Effects of neutralizing antibodies on the accumulation of toxin in various tissues. 125I-labeled BoNT/A was incubated alone (open bars) or with antiserum (cross-hatched bars) and administered as described in the legend to Fig. 11. After 30 min, animals were anesthetized and perfused for subsequent removal of organs. The data show that pretreatment of toxin with neutralizing antibodies resulted in marked increases in the accumulation in livers and spleens (a). Antibody pretreatment did not increase the accumulation in tissues that are ordinarily not related to immune processing (b).
Antibodies from immunized animals can block the neuroparalytic actions of BoNT.
The HC50 domain of BoNT is known to possess the molecular determinants that govern toxin binding to neuronal membranes (31). This raises the possibility that at least one of the clonal antibodies in the serum of immunized animals could associate with the toxin in a way that would block toxin binding and/or block toxin internalization. To test the possibility that antiserum directed against HC50 could antagonize toxin-induced paralysis, unlabeled BoNT/A (1 × 10−8 M) was incubated without or with mouse trivalent antiserum (0.1 ml; 30 min; room temperature). The mixtures were subsequently diluted and added to murine phrenic nerve-hemidiaphragm preparations (four preparations per group) to obtain a final toxin concentration of 1 × 10−11 M. The results (Fig. 13) demonstrated that the paralysis times for control tissues were ca. 100 to 140 min. Tissues that were treated with toxin that had been preincubated with immune serum showed no onset of neuromuscular blockade during a 100- to 140-min period.
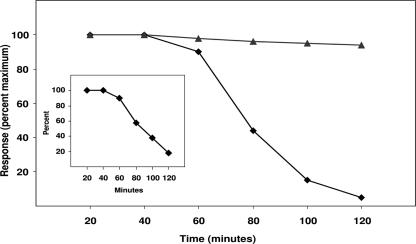
FIG. 13.
Effects of neutralizing antibodies on the neuromuscular blocking properties of BoNT/A. Toxin (1 × 10−8 M) was incubated alone or with antiserum from animals that had been immunized with trivalent vaccine (0.1 ml; 30 min; room temperature). The mixtures were then added to phrenic nerve-hemidiaphragm preparations (four preparations per group) to obtain a final toxin concentration of 1 × 10−11 M. Untreated toxin caused paralysis of transmission (i.e., a 90% reduction in twitch amplitude) within 100 to 140 min (⧫). In the same time frame, antibody-pretreated toxin did not paralyze transmission (▴). An equivalent experiment was done in which toxin was preincubated with preimmune serum (inset). This pretreatment did not significantly affect the potency of the toxin.
DISCUSSION
BoNT is the etiologic agent that causes the disease botulism. This disease can occur naturally, but it can also be a result of bioterrorism or biological warfare. The number of outbreaks of naturally occurring botulism and the number of cases per outbreak are too low to be a driving force in the development of a vaccine. On the other hand, concern about the potential use of the toxin in acts of bioterrorism or biological warfare has served as a powerful motivation to develop a vaccine.
Although it is understandable that there is a sense of urgency concerning the need for a vaccine, this should not obscure the fact that development of the final product should be governed by the principles of rational vaccine design. Two of the most important areas in which these principles should apply are (i) the selection of an antigen and (ii) the selection of a route of administration for that antigen.
Selection of an antigen.
In historical attempts to develop a botulinum vaccine workers focused on chemical toxoids (i.e., formalin inactivation of impure toxin preparations), whereas in more recent attempts workers have focused on recombinant toxoids (6). Vaccine candidates in the latter category have included the holotoxin with point mutations to eliminate catalytic activity (15) and various subunit polypeptides. The subunit vaccine that has emerged as the favored candidate is HC50 (also known as HCC and fragment C [6]).
There are a variety of reasons to believe that HC50 is a rational choice. To begin with, it is modeled after an analogous polypeptide from tetanus toxin that has been shown to be a highly efficacious vaccine against the parent molecule (10, 13, 20). In addition, the HC50 domain of BoNT has a large number of epitopes. In fact, there are more epitopes in this polypeptide than there are in the rest of the toxin molecule combined (7). This suggests that (i) this polypeptide should evoke a robust polyclonal response against the native toxin and (ii) increasing the length of the polypeptide (HC66, HC88, etc.) may not lead to increases in resistance that would be clinically significant.
These observations, combined with reports that HC50 is an efficient immunogen in laboratory animal studies, strongly support the premise that a rational vaccine candidate has been identified. However, there is even more evidence that supports the use of this subunit vaccine. As previously reported, the HC50 domain of BoNT/A possesses all of the structural information necessary for binding to and penetration of gut and airway epithelial barriers (23). This means that the BoNT/A HC50 domain can simultaneously serve as a delivery device and as an immunogen in a mucosal botulinum vaccine.
Selection of a route of administration.
There are at least two powerful reasons to seek a mucosal (“needle-free”) vaccine against BoNT. One of these reasons is broad and is related to the discipline of immunology; the second is highly specific and is related to the mechanism of BoNT action. In broad terms, there is wide recognition in the field of immunology that injectable vaccines should give way to needle-free vaccines (24). Indeed, every major health care entity that supports vaccine research, including the National Institutes of Health, the World Health Organization, and the Bill and Melinda Gates Foundation, has encouraged efforts to develop needle-free approaches. The reasons for this are compelling, and they include (i) the reduced need for, and cost of, health care personnel; (ii) the elimination of accidental needle sticks and their potential contribution to blood-borne diseases; (iii) the reduced burden of storing medical waste; and (iv) the elimination of the potential for environmental contamination. There is no reason why a vaccine against BoNT should be exempt from these considerations.
The second reason for pursuing a mucosal vaccine is related specifically to the mechanism of toxin action. The majority of all reported cases of naturally occurring botulism are due to mucosal exposure, and it is anticipated that most if not all cases of a potential bioterrorism incident or biological warfare incident would also be due to mucosal exposure. This is a strong argument against an injection vaccine and in favor of a mucosal vaccine, because the latter has the potential to act in the lumen of the gut and airway to evoke the production of antibodies (i.e., secretory IgA) that could block absorption of the toxin. An injection vaccine does not have this benefit.
To return to a point discussed above, the HC50 domain may be an ideal choice as a mucosal vaccine, because this molecule has the properties of both an immunogen and a delivery device. These dual functions represent a major advance over current efforts to develop a mucosal vaccine. For example, use of the recombinant polypeptide obviates the need for chemically induced toxoids (16). Similarly, the inherent ability of the polypeptide to penetrate epithelial barriers and evoke an immune response circumvents the need for ancillary devices, such as a virus (19).
Identification of a mucosal vaccine.
The data presented in this paper demonstrate that the HC50 domain is an effective inhalation vaccine. In an initial series of experiments utilizing BoNT/A as a prototype, the HC50 domain evoked a significant IgG response and a more modest IgA response. It also provided resistance against a challenge dose of BoNT.
One well-recognized approach for enhancing an immunoglobulin response is to combine the antigen of interest with an adjuvant. This concept is technically sound, but it presents a difficulty in the context of trying to develop a vaccine that can be licensed for human use. Almost all agents that have been examined as mucosal adjuvants, such as the cholera toxin B subunit, are not approved for clinical use. One potential solution to this problem is to select an agent for which there are a minimum of regulatory obstacles. Therefore, we used vaccination protocols in which two natural products (chitosan and vitamin E) were evaluated to determine their utility as adjuvants (2, 8, 25, 36). Administration of the HC50 domain of BoNT/A simultaneously with chitosan or with vitamin E (Fig. 2) had the intended effect of boosting the levels of the immunoglobulin responses.
Trivalent vaccine against botulism.
BoNT serotypes A, B, and E are the serotypes most often implicated in human illness. This suggests that the greatest need is for a multivalent preparation that provides protection against all three of these serotypes. This goal appears to be attainable, because (i) the HC50 domains of these serotypes are able to penetrate epithelial barriers (Fig. 5) and (ii) the same domains are immunogens that evoke protection against the corresponding parent toxins (Fig. 7). This is an encouraging basis on which to seek a trivalent vaccine, but at the same time it leaves three important questions unanswered. First, can HC50 domains given in combination penetrate epithelial barriers as well as HC50 domains given individually? Second, can HC50 domains given in combination evoke an immune response comparable to that evoked by peptides that are given individually? Third, can a trivalent vaccine evoke resistance of a magnitude sufficient to afford protection against a combination challenge?
The question about membrane penetration has been addressed using monolayers of human epithelial cells. These cells have proven to be useful in studies in which the kinetics of BoNT/A binding and transcytosis have been analyzed, as well as in studies in which BoNT/A molecules crossing epithelial barriers have been visualized (1, 22). This work was extended here to include the HC50 domains of BoNT/B and BoNT/E. In the context of vaccine research, the important observation resulting from these experiments is that each HC50 domain retained its characteristic ability to cross epithelial barriers, even when it was added along with other such domains (Fig. 6). This is predictive evidence that the three domains could be administered as a trivalent vaccine.
The question about immunogenicity was answered by coadministration of the three HC50 domains by two regimens, mucosal vaccination alone and an initial injection followed by mucosal boosters. Interestingly, these two approaches produced very similar outcomes. Both resulted in substantial IgG and IgA responses. Using BoNT/A HC50 as an indicator, one can deduce that the magnitudes of the immunoglobulin responses for monovalent vaccination (Fig. 2) and trivalent vaccination (Fig. 7 and 8) were not significantly different. The data indicate that simultaneous vaccination with three antigens did not compromise the ability of the immune system to respond to any one of the antigens.
Finally, the question about induced resistance was answered by challenging animals with a mixture of the three holotoxins. Equal doses of the holotoxins were mixed to produce final doses of 3 × 103 or 3 × 104 LD50. Regardless of whether animals received the trivalent vaccine by mucosal administration or by mixed-mode administration, all test animals survived. These data demonstrate that a trivalent vaccine that acts by the mucosal route has been identified.
Mechanisms of resistance.
There are a number of mechanisms by which immunoglobulin-mediated resistance could decrease toxicity. The sequence of events that underlies toxin action suggests that an ideal vaccine candidate should possess at least three of these mechanisms. A clonal population should possess within it antibodies that act (i) in the lumen of the gut or airway to block toxin absorption, (ii) in the general circulation to enhance clearance from the blood and accumulation in the liver and spleen, and (iii) at the neuromuscular junction to antagonize blockade of exocytosis. The clonal population evoked by trivalent vaccination had in it antibodies that could be shown to act at all three sites.
When tested with a model system for binding and transcytosis in human epithelial cells, both BAL samples (secretory IgA) and antiserum (circulating IgG and IgA) from animals that had received HC50 as a vaccine blocked the ability of BoNT to cross epithelial barriers (Fig. 10). The results indicated that the level of inhibition of binding and transcytosis was greater than 99%. If this outcome were a close approximation of events in vivo, it would mean that mucosal immunity in the lumen of the gut or airway can be an important factor contributing to resistance.
In related experiments, the pharmacokinetics of BoNT/A elimination were studied using control and experimental animals. The experiments were conducted over a period of time (30 min) during which the fractional distribution of toxin out of the circulation and into peripheral cholinergic nerve endings of control animals had not yet produced serious neuromuscular blockade (29). These experiments demonstrated that a neutralizing dose of trivalent antiserum resulted in a rapid and dramatic increase in the rate of clearance of BoNT/A from the blood (Fig. 11). This phenomenon was accompanied by an equally dramatic accumulation of toxin in the liver and spleen (Fig. 12). It is very likely that hepatic and splenic accumulation is a prelude to metabolic degradation and eventual systemic elimination of toxin fragments.
The final mechanism by which an ideal vaccine candidate could evoke immunoresistance is antagonism of toxin-induced neuromuscular blockade (31, 32). The possibility that this occurs was tested by using an isolated phrenic nerve-hemidiaphragm preparation, which means that mechanisms such as inhibition of luminal absorption and enhancement of systemic clearance could not have contributed to the outcome. These experiments clearly demonstrated that anti-HC50 antibodies antagonized toxin action in isolated neuromuscular preparations.
Concept of a universal vaccine.
The discipline of immunology typically uses the term “universal vaccine” to convey one of two concepts: (i) a single antigen can be administered by all of the routes that are commonly used for vaccines or (ii) a single antigen can be used to evoke resistance to multiple strains, serotypes, or other variants of a pathogen. The data suggest that the HC50 domain is close to satisfying the expectation for a single antigen that is active when it is administered by multiples routes.
Numerous investigators have contributed to the observation that the HC50 domain of all BoNT serotypes can be administered by injection to evoke an immune response. It has also been shown that the inactive holotoxin, the entire HC, and the HC50 domains of several serotypes are active when they are administered by the oral and/or inhalation routes (see the Introduction). In addition, a single paradigm that incorporates both injection and nasal routes of administration can evoke robust immunity (this study).
It is customary to divide routes of potential vaccine administration into three broad categories: injection, mucosal, and cutaneous (24). As mentioned above, the HC50 domain of BoNT is already known to be effective as an injection vaccine, a mucosal vaccine, and a mixed-mode vaccine. To date, the HC50 domain has not been shown to be a cutaneous vaccine. In fact, this domain by itself does not penetrate the stratum corneum (unpublished data). However, there have been several recent and notable advances in the transcutaneous delivery of antigens. Therefore, vaccination protocols aimed at transcutaneous delivery of HC50 are currently being investigated, in the hope of establishing that HC50 is a true universal vaccine.
Acknowledgments
This work was supported in part by National Institutes of Health contract N01-AI30028, by National Institutes of Health grants NS22153 and GM57342, and by a sponsored research agreement with DOR Biopharma.
Editor: D. L. Burns
Footnotes
Published ahead of print on 19 March 2007.
REFERENCES
- 1.Ahsan, C. R., G. Hajnoczky, A. B. Maksymowych, and L. L. Simpson. 2005. Visualization of binding and transcytosis of botulinum toxin by human intestinal epithelial cells. J. Pharmacol. Exp. Ther. 315:1028-1035. [DOI] [PubMed] [Google Scholar]
- 2.Alpar, H. O., J. E. Eyles, E. D. Williamson, and S. Somavarapu. 2001. Intranasal vaccination against plague, tetanus and diphtheria. Adv. Drug Deliv. Rev. 51:173-201. [DOI] [PubMed] [Google Scholar]
- 3.Arnon, S. S., R. Schechter, T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, J. Hauer, M. Layton, S. Lillibridge, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, D. L. Swerdlow, K. Tonat, and Working Group on Civilian Biodefense. 2001. Botulinum toxin as a biological weapon: medical and public health management. JAMA 285:1059-1070. [DOI] [PubMed] [Google Scholar]
- 4.Bleck, T. P. 2000. Clostridium tetani, p. 2537-2543. In G. M. Mandell Dolin (ed.), Principles and practice of infectious diseases, 5th ed. Churchill Livingstone, New York, NY.
- 5.Byrne, M. P., T. J. Smith, V. A. Montgomery, and L. A. Smith. 1998. Purification, potency, and efficacy of the botulinum neurotoxin type A binding domain from Pichia pastoris as a recombinant vaccine candidate. Infect. Immun. 66:4817-4822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrne, M. P., and X. Smith. 2000. Development of vaccines for prevention of botulism. Biochimie 82:955-966. [DOI] [PubMed] [Google Scholar]
- 7.Chen, F., G. M. Kuziemko, P. Amersdorfer, C. Wong, J. D. Marks, and R. C. Stevens. 1997. Antibody mapping to domains of botulinum neurotoxin serotype A in the complexed and uncomplexed forms. Infect. Immun. 65:1626-1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Constantinides, P. P., J. Han, and S. S. Davis. 2006. Advances in the use of tocols as drug delivery vehicles. Pharm. Res. 23:243-255. [DOI] [PubMed] [Google Scholar]
- 9.DasGupta, B. R., and V. Sathyamoorthy. 1984. Purification and amino acid composition of type A botulinum neurotoxin. Toxicon 22:415-424. [DOI] [PubMed] [Google Scholar]
- 10.Fairweather, N. F., V. A. Lyness, and D. J. Maskell. 1987. Immunization of mice against tetanus with fragments of tetanus toxin synthesized in Escherichia coli. Infect. Immun. 55:2541-2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finegold, S. M. 1998. Tetanus, p. 693-722. In L. H. Collier, A. Balows, and M. Sussman (ed.), Bailey and Scott's diagnostic microbiology, 9th ed. Arnold, London, United Kingdom.
- 12.Hatheway, C. L. 1995. Botulism: the present status of the disease. Curr. Top. Microbiol. Immunol. 195:55-75. [DOI] [PubMed] [Google Scholar]
- 13.Helting, T. B., and H. H. Nau. 1984. Analysis of the immune response to papain digestion products of tetanus toxin. Acta Path Microbiol. Immunol. Scan 92:59-63. [DOI] [PubMed] [Google Scholar]
- 14.Johnson, E. A., and M. C. Goodnough. 1998. Botulism, p. 723-741. In L. H. Collier, A. Balows, and M. Sussman (ed.), Microbiology and microbial infections, 9th ed. Arnold, London, United Kingdom.
- 15.Kiyatkin, N., A. B. Maksymowych, and L. L. Simpson. 1997. Induction of immune response by oral administration of recombinant botulinum toxin. Infect. Immun. 65:4586-4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobayashi, R., T. Kohda, K. Kataoka, H. Ihara, S. Kozaki, D. W. Pascual, H. F. Staats, H. Kiyono, J. R. McGhee, and K. Fujihashi. 2005. A novel neurotoxoid vaccine prevents mucosal botulism. J. Immunol. 174:2190-2195. [DOI] [PubMed] [Google Scholar]
- 17.Lacy, D. B., and R. C. Stevens. 1998. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 5:898-902. [DOI] [PubMed] [Google Scholar]
- 18.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 19.Maddaloni, M., H. F. Staats, D. Mierzejewska, T. Hoyt, A. Robinson, G. Callis, S. Kozaki, H. Kiyono, J. R. McGhee, K. Fujihashi, and D. W. Pascual. 2006. Mucosal vaccine targeting improves onset of mucosal and systemic immunity to botulinum neurotoxin a. J. Immunol. 177:5524-5532. [DOI] [PubMed] [Google Scholar]
- 20.Makoff, A. J., S. P. Ballantine, A. E. Smallwood, and N. F. Fairweather. 1989. Expression of tetanus toxin fragment C in E. coli: its purification and potential use as a vaccine. Bio/Technology 7:1043-1046. [Google Scholar]
- 21.Maksymowych, A. B., M. Reinhard, C. J. Malizio, M. C. Goodnough, E. A. Johnson, and L. L. Simpson. 1999. Pure botulinum toxin is absorbed from the stomach and small intestine and produces peripheral neuromuscular blockade. Infect. Immun. 67:4708-4712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maksymowych, A. B., and L. L. Simpson. 1998. Binding and transcytosis of botulinum neurotoxin by polarized human colon carcinoma cells. J. Biol. Chem. 273:21950-21957. [DOI] [PubMed] [Google Scholar]
- 23.Maksymowych, A. B., and L. L. Simpson. 2004. Structural features of the botulinum neurotoxin molecule that govern binding and transcytosis across polarized human intestinal epithelial cells. J. Pharmacol. Exp. Ther. 310:633-641. [DOI] [PubMed] [Google Scholar]
- 24.Mitragotri, S. 2005. Immunization without needles. Nat. Rev. Immunol. 5:905-916. [DOI] [PubMed] [Google Scholar]
- 25.Mu, L., and S. S. Feng. 2002. Vitamin E TPGS used as emulsifier in the solvent evaporation/extraction technique for fabrication of polymeric nanospheres for controlled release of paclitaxel (taxol). J. Control. Release 80:129-144. [DOI] [PubMed] [Google Scholar]
- 26.Niemann, H. 1992. Clostridial neurotoxins—proposal of a common nomenclature. Toxicon 30:223-225. [DOI] [PubMed] [Google Scholar]
- 27.Park, J. B., and L. L. Simpson. 2003. Inhalational poisoning by botulism toxin and inhalation vaccination with its heavy-chain component. Infect. Immun. 71:1147-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pellizzari, R., O. Rossetto, G. Schiavo, and C. Montecucco. 1999. Tetanus and botulinum neurotoxins: mechanism of action and therapeutic uses. Philos. Trans. R. Soc. Lond. B Biol. Sci. 354:259-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ravichandran, E., Y. Gong, F. H. Al Saleem, D. M. Ancharski, S. G. Joshi, and L. L. Simpson. 2006. An initial assessment of the systemic pharmacokinetics of botulinum toxin. J. Pharmacol. Exp. Ther. 318:1343-1351. [DOI] [PubMed] [Google Scholar]
- 30.Sakaguchi, G. 1982. Clostridium botulinum toxins. Pharmacol. Ther. 19:165-194. [DOI] [PubMed] [Google Scholar]
- 31.Schiavo, G., M. Matteoli, and C. Montecucco. 2000. Neurotoxins affecting neuroexocytosis. Physiol. Rev. 80:717-766. [DOI] [PubMed] [Google Scholar]
- 32.Simpson, L. L. 2004. Identification of the major steps in botulinum toxin action. Annu. Rev. Pharmacol. Toxicol. 44:167-193. [DOI] [PubMed] [Google Scholar]
- 33.Simpson, L. L., A. B. Maksymowych, and S. Hao. 2001. The role of zinc binding in the biological activity of botulinum toxin. J. Biol. Chem. 276:27034-27041. [DOI] [PubMed] [Google Scholar]
- 34.Simpson, L. L., J. J. Schmidt, and J. L. Middlebrook. 1988. Isolation and characterization of the botulinum neurotoxins. Methods Enzymol. 165:76-85. [DOI] [PubMed] [Google Scholar]
- 35.Smith, T. J., J. Lou, I. N. Geren, C. M. Forsyth, R. Tsai, S. L. LaPorte, W. H. Tepp, M. Bradshaw, E. A. Johnson, L. A. Smith, and J. D. Marks. 2005. Sequence variation with botulinum neurotoxin serotypes impacts antibody binding and neutralization. Infect. Immun. 73:5450-5457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Somavarapu, S., S. Pandit, G. Gradassi, M. Bandera, E. Ravichandran, and H. O. Alpar. 2005. Effect of vitamin E TPGS on immune response to nasally delivered diphtheria toxoid loaded poly(caprolactone) microparticles. Int. J. Pharm. 298:344-347. [DOI] [PubMed] [Google Scholar]
- 37.Swaminathan, S., and S. Eswaramoorthy. 2000. Structural analysis of the catalytic and binding sites of Clostridium botulinum neurotoxin B. Nat. Struct. Biol. 7:693-699. [DOI] [PubMed] [Google Scholar]
- 38.Towbin, H., T. Staehelin, and J. Gordon. 1979. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc. Natl. Acad. Sci. USA 76:4350-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]