Abstract
The in vitro spectra of activity of tigecycline and tetracycline were determined for 2,490 bacterial isolates representing 50 different species or phenotypic groups. All isolates were tested simultaneously by broth microdilution using freshly prepared Mueller-Hinton broth and by disk diffusion. Portions of these data were submitted to the Food and Drug Administration (FDA) in support of the sponsor's application for new drug approval. In a separate study, MIC and disk diffusion quality control ranges were determined. The tigecycline MICs at which 50%/90% of bacteria were inhibited were (in μg/ml) as follows: for Streptococcus spp., 0.06/0.12; for Moraxella catarrhalis, 0.06/0.12; for Staphylococcus spp., 0.12/0.25; for Enterococcus spp., 0.12/0.25; for Listeria monocytogenes, 0.12/0.12; for Neisseria meningitidis, 0.12/0.25; for Haemophilus spp., 0.25/0.5; for Enterobacteriaceae, 0.05/2.0; for non-Enterobacteriaceae, 0.5/8.0. Tigecycline was consistently more potent than tetracycline against all species studied. The data from this study confirm the FDA-approved MIC and disk diffusion breakpoints for tigecycline for Streptococcus spp. other than Streptococcus pneumoniae, enterococci, and Enterobacteriaceae. Provisional breakpoints for Haemophilus spp. and S. pneumoniae are proposed based on the data from this study. The following MIC and/or disk diffusion quality control ranges are proposed: Staphylococcus aureus ATCC 29213, 0.03 to 0.25 μg/ml; S. aureus ATCC 25923, 20 to 25 mm; Escherichia coli ATCC 25922, 0.03 to 0.25 μg/ml and 20 to 27 mm; Pseudomonas aeruginosa ATCC 27853, 9 to 13 mm, Enterococcus faecalis ATCC 29212, 0.03 to 0.12 μg/ml; S. pneumoniae ATCC 49619, 0.015 to 0.12 μg/ml and 23 to 29 mm; Haemophilus influenzae ATCC 49247, 0.06 to 0.5 μg/ml and 23 to 31 mm; and Neisseria gonorrhoeae ATCC 49226, 30 to 40 mm.
Tigecycline (formerly GAR-936) is a new glycylcycline (24) compound with a broad spectrum of antibacterial activity (2-4, 8, 10, 13, 14, 23). In addition, it has been shown to be active against microorganisms known to be resistant to other classes of antimicrobial agents (1, 11, 12, 19, 20, 22). Recent studies have found that the age of the broth medium used for in vitro susceptibility testing can affect the MICs of tigecycline by as much as two to eightfold (5, 21). Susceptibility tests performed with medium which was ≤12 h old at the time of testing produced MICs which were substantially lower than those observed with medium that had been aged for various periods of time up to 1 month. The effects of medium aging could be counteracted by the addition of Oxyrase, a biocatalytic oxygen-reducing reagent, to the susceptibility testing medium. Further testing revealed that dissolving tigecycline in aged medium resulted in the formation of an oxidized tigecycline product which had decreased antibacterial activity (5). Once the MIC trays were frozen, the oxidation of the drug was minimal. MIC trays which were prepared using freshly prepared medium and stored at −20°C for several weeks produced results which were nearly identical to those obtained with trays tested on the same day as production with freshly prepared broth medium. These observations have resulted in the Clinical and Laboratory Standards Institute (CLSI) requirement that only freshly prepared medium (≤12 h old) be used for testing tigecycline by broth MIC methods (7).
Unfortunately, spectrum-of-activity studies published prior to this may be flawed in the respect that they were performed using agar dilution or using broth medium in which the age of the medium was either unknown or unstated.
Tigecycline is currently approved worldwide for the treatment of serious skin, skin structure, and intra-abdominal bacterial infections in hospitals. Bacterial isolates obtained during the clinical trials were tested and reported using freshly prepared medium which was less than 12 h old at the time of MIC tray production (6).
The present study was designed to compare the in vitro antibacterial activity of tigecycline with that of tetracycline against a broad range of bacterial pathogens, provide supplemental data for the sponsor's FDA new-drug application, determine correlation of tigecycline disk diffusion to MIC results for these microorganisms, and propose MIC and disk diffusion quality control ranges for eight different aerobic quality control strains.
MATERIALS AND METHODS
Bacteria tested.
A total of 2,490 recent clinical bacterial isolates were selected as representative pathogens that cause infections for which tigecycline might be considered for therapy. All isolates were obtained from medical centers across North America and sent to the Clinical Microbiology Institute, where they were reidentified and placed in a large culture collection. These included 269 streptococci, 216 enterococci, 44 Staphylococcus aureus isolates, 86 coagulase-negative staphylococci, 1,352 Enterobacteriaceae, 153 nonfermentative gram-negative rods, 100 Listeria monocytogenes isolates, 64 Moraxella catarrhalis isolates, 93 Neisseria meningitidis isolates, and 113 Haemophilus spp. Two of the goals of this study were to test approximately 100 strains of species identified as a potential target for tigecycline therapy and to provide the sponsor with supplemental data for Staphylococcus spp. This collection includes isolates with a variety of previously established resistance phenotypes.
Antimicrobial susceptibility testing.
Tigecycline was provided as a sterile powder (lot no. MB1611) by Wyeth Research (Pearl River, NY). Tetracycline (lot no. 092K1607) was purchased from Sigma (St. Louis, MO) and was used as an internal quality control. The results for tigecycline were compared to those for tetracycline as a method of establishing relative potency. Disk diffusion susceptibility tests used commercially prepared 15-μg disks of tigecycline (lot no. 3259023) and 30-μg disks of tetracycline (lot no. 0175726) purchased from BD Microbiologic Systems (Cockeysville, MD).
All aerobic organisms were tested by the broth microdilution method recommended by the CLSI (15) using cation-adjusted Mueller-Hinton broth which was less than 12 h old at the time of MIC tray production. The medium was supplemented with 3% lysed horse blood for testing of all streptococci, L. monocytogenes, and N. meningitidis or made up as Haemophilus test medium for testing of Haemophilus spp. as recommended by the CLSI. All organisms were tested simultaneously by the disk diffusion method outlined by the CLSI (16) using Mueller-Hinton agar plus 5% sheep blood (streptococci, L. monocytogenes, M. catarrhalis, and N. meningitidis), Haemophilus test medium agar (Haemophilus spp.), or plain Muller-Hinton agar (all other genera).
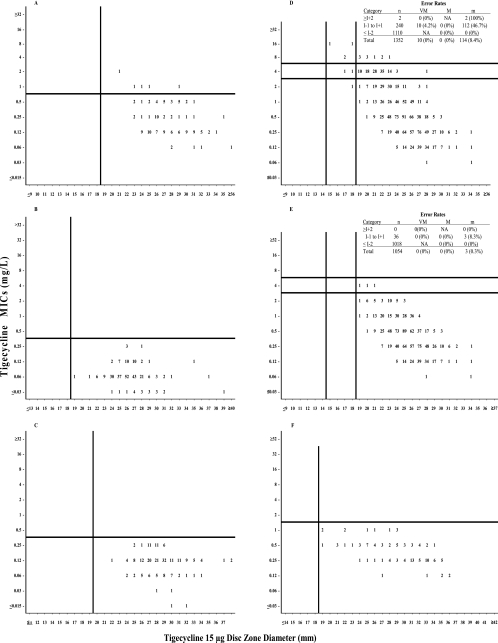
MIC-versus-zone-diameter scattergrams (Fig. 1A to F) were prepared using an error minimization approach (17). FDA disk diffusion interpretive criteria are confirmed or proposed for all strains.
FIG. 1.
Scattergrams of tigecycline MICs versus zone diameters (15-μg disks). (A) All staphylococci combined (including methicillin-resistant isolates; n = 130), (B) Streptococcus pneumoniae (n = 209) and nonpneumococcal streptococci (n = 60) combined, (C) all Enterococcus spp. combined (n = 216), (D) all Enterobacteriaceae combined (n = 1,352) (122/125 [97.6%] of the isolates with a tigecycline MIC of ≥4 μg/ml were Morganella, Proteus spp. other than P. vulgaris, or Providencia spp.), (E) Enterobacteriaceae without Morganella, Proteus spp. other than P. vulgaris, or Providencia spp. (n = 1,054), (F) Haemophilus spp. (n = 113). Horizontal lines represent proposed susceptible (lower line) and resistant (upper line) MIC breakpoints; vertical lines represent proposed susceptible (right line) and resistant (left line) zone diameter breakpoints. Abbreviations: n, number of strains tested; VM, very major errors; M, major errors; m, minor errors; I+2, intermediate MIC breakpoint plus 2 log2 dilutions; I−1 to I+1, intermediate MIC breakpoint plus or minus 1 log2 dilution; I−2, intermediate MIC breakpoint minus 2 log2 dilutions.
Quality control studies.
Three separate multilaboratory studies were undertaken in order to propose quality control ranges for MIC and disk diffusion methodologies. The testing laboratories included both hospital and commercial microbiology laboratories in the United States and are identified in Table 1. These studies closely followed the protocol described by the CLSI (17) with the exception that the number of testing facilities exceeded the minimum number of seven required sites. In addition, a total of up to six lots of broth medium was tested rather than the minimum of three lots. The quality control organisms were those recommended by the CLSI (18) and included S. aureus ATCC 29213 (MIC only) and ATCC 25923 (disk only), Enterococcus faecalis ATCC 29212 (MIC only), Streptococcus pneumoniae ATCC 49619 (MIC and disk), Pseudomonas aeruginosa ATCC 27853 (disk only), Escherichia coli ATCC 25922 (MIC and disk), Neisseria gonorrhoeae ATCC 49226 (disk only), and Haemophilus influenzae ATCC 49247 (MIC and disk). Internal quality control results for the control drug, tetracycline, were within published ranges available (18) for the majority of tests. When any control value was out of the established ranges, all of the tigecycline data associated with that day's testing were discarded. This study involved 10 replicate tests on up to six lots of Mueller-Hinton broth or three lots of agar, two lots of 15-μg tigecycline disks (BDMS lot no. 0167721 and Oxoid lot no. 241765), and one lot of 30-μg tetracycline disks (BDMS lot no. 1050730). This exercise generated a target of 600 MICs and 480 disk diffusion zone diameters with each appropriate quality control strain. Zone diameters were evaluated using the statistics of Gavan et al. (9).
TABLE 1.
Sites participating in quality control studies
| Participant | Institution, city, and state or province |
|---|---|
| S. Brown | Clinical Microbiology Institute, Wilsonville, OR |
| M. Baumana | St. Vincent's Hospital, Portland, OR |
| M. Coxb | Anaerobe Systems, Morgan Hill, CA |
| M. J. Ferraroa | Massachusetts General Hospital, Boston, MA |
| D. Hardy | Univ. of Rochester Medical Center, Rochester, NYd |
| J. Hindler | UCLA Medical Center, Los Angeles, CA |
| S. Jenkinsa | Carolinas Medical Center, Charlotte, NC |
| C. Knapp | TREK Diagnostic Systems, Westlake, OH |
| G. Overturfa | Univ. New Mexico Medical Center, Albuquerque, NM |
| G. Procop | Cleveland Clinic, Cleveland, OH |
| R. Rennie | Univ. of Alberta Hospital, Edmonton, Alberta, Canada |
| M. Saubollea | Good Samaritan Hospital, Phoenix, AZ |
| E. J. Baronc | Stanford Univ. Hospital and Clinics, Stanford, CA |
| F. Tenoverc | Centers for Disease Control and Prevention, Atlanta, GA |
S. aureus, E. coli, and E. faecalis MIC study only.
Disk diffusion study only.
S. pneumoniae and H. influenzae MIC study only.
Univ., university.
RESULTS
Spectrum-of-activity and interpretive-criteria study.
Table 3 summarizes the MICs of tigecycline and tetracycline against all bacterial isolates tested. Tigecycline exhibited excellent activity against all gram-positive species, M. catarrhalis, H. influenzae, and N. meningitidis, with MICs at which 90% of bacteria were inhibited (MIC90s) of ≤0.5 μg/ml. For the majority of these species, tigecycline was 2 to 1,024 times more potent than tetracycline. MICs were not significantly affected by increasing resistance to penicillin (S. pneumoniae), oxacillin (staphylococci), vancomycin (enterococci), or the presence of extended-spectrum β-lactamases (ESBLs) (E. coli and Klebsiella pneumoniae). In each of these instances, the MIC90 of the resistant strains was within 1 doubling dilution of that of the more susceptible isolates. Good activity was also noted for Haemophilus parainfluenzae and the majority of the Enterobacteriaceae species. The MIC90s for these species ranged from 0.25 μg/ml (Citrobacter koseri) to 2 μg/ml (Klebsiella oxytoca, ESBL+ K. pneumoniae, Proteus vulgaris, Serratia marcescens, and Salmonella enterica serovar Typhimurium). Good activity was also noted for Pasteurella multocida (MIC90 = 0.25 μg/ml). Decreased in vitro activity was noted for Morganella spp., Proteus spp. other than P. vulgaris, Providencia spp., Burkholderia cepacia, P. aeruginosa, and Stenotrophomonas maltophilia, which had MIC90s of ≥4 μg/ml for tigecycline. A total of 122/125 (97.6%) of the isolates with an individual MIC of ≥4 μg/ml were from among this group of microorganisms.
TABLE 3.
Susceptibilities of aerobic bacteria to tigecycline and tetracycline
| Species (na)b | MIC of drug (μg/ml)
|
|||||
|---|---|---|---|---|---|---|
| Tigecycline
|
Tetracycline
|
|||||
| Range | 50% | 90% | Range | 50% | 90% | |
| All strains combined (2,490) | 0.015-32 | 0.25 | 2 | 0.015->32 | 2 | >32 |
| Gram-positive strains | ||||||
| All streptococci combined (269) | 0.03-0.25 | 0.06 | 0.12 | 0.12->32 | 0.5 | >32 |
| S. agalactiae (20) | 0.06-0.06 | 0.06 | 0.06 | 0.25->32 | 32 | >32 |
| S. pneumoniae, penicillin-S (23) | 0.03-0.12 | 0.06 | 0.06 | 0.12-0.5 | 0.25 | 0.5 |
| S. pneumoniae, penicillin-I (100) | 0.03-0.25 | 0.06 | 0.12 | 0.12->32 | 0.25 | >32 |
| S. pneumoniae, penicillin-R (86) | 0.03-0.25 | 0.06 | 0.12 | 0.25->32 | 32 | 32 |
| S. pyogenes (40) | 0.03-0.06 | 0.06 | 0.06 | 0.12-32 | 0.25 | 16 |
| All staphylococci combined (130) | 0.06-2 | 0.12 | 0.25 | 0.12->32 | 0.25 | >32 |
| All S. aureus strains combined (44) | 0.12-1 | 0.12 | 0.5 | 0.25->32 | 0.25 | >32 |
| S. aureus, methicillin-R (24) | 0.12-1 | 0.12 | 0.25 | 0.25->32 | 0.25 | >32 |
| S. aureus, methicillin-S (20) | 0.12-0.25 | 0.12 | 0.12 | 0.25->32 | 0.25 | 0.5 |
| All coagulase-negative staphylococci combined (86) | 0.06-2 | 0.12 | 0.5 | 0.12->32 | 1 | >32 |
| S. epidermidis, methicillin-R (21) | 0.06-0.5 | 0.12 | 0.5 | 0.25->32 | 2 | 32 |
| S. epidermidis, methicillin-S (35) | 0.06-1 | 0.12 | 0.5 | 0.12->32 | 1 | >32 |
| S. haemolyticus (30) | 0.06-2 | 0.25 | 0.5 | 0.12->32 | 0.5 | >32 |
| All enterococci combined (216) | 0.015-0.25 | 0.12 | 0.25 | 0.015->32 | 2 | >32 |
| E. avium (40) | 0.015-0.25 | 0.12 | 0.12 | 0.015->32 | 16 | >32 |
| E. casseliflavus (23) | 0.12-0.25 | 0.12 | 0.25 | 0.25-32 | 1 | 32 |
| E. faecalis, vancomycin-R (34) | 0.06-25 | 0.12 | 0.25 | 0.25->32 | 1 | >32 |
| E. faecalis, vancomycin-S (19) | 0.12-25 | 0.12 | 0.25 | 1->32 | 32 | >32 |
| E. faecium, vancomycin-R (20) | 0.06-0.25 | 0.12 | 0.12 | 0.25->32 | 16 | >32 |
| E. faecium, vancomycin-S (40) | 0.06-0.25 | 0.12 | 0.12 | 0.12->32 | 0.5 | >32 |
| E. gallinarium (40) | 0.06-0.25 | 0.12 | 0.25 | 0.25->32 | 1 | >32 |
| Listeria monocytogenes (100) | 0.06-0.12 | 0.12 | 0.12 | 0.25->32 | 1 | 1 |
| Gram-negative strains | ||||||
| Moraxella catarrhalis (64) | 0.06-0.25 | 0.06 | 0.12 | 0.06-16 | 0.25 | 0.5 |
| Neisseria meningitidis (93) | 0.03-0.5 | 0.12 | 0.25 | 0.03-1 | 0.25 | 0.5 |
| All Haemophilus spp. combined (113) | 0.12-1 | 0.25 | 0.5 | 0.25->32 | 0.5 | 2 |
| H. influenzae (64) | 0.12-1 | 0.25 | 0.5 | 0.25-32 | 0.5 | 0.5 |
| H. parainfluenzae (49) | 0.12-1 | 0.5 | 1 | 0.25->32 | 0.5 | 8 |
| All Enterobacteriaceae combined (1,352) | 0.06-16 | 0.5 | 2 | 0.25->32 | 16 | >32 |
| Citrobacter freundii (20) | 0.12-2 | 0.25 | 0.5 | 0.5->32 | 1 | 2 |
| Citrobacter. koseri (41) | 0.12-1 | 0.25 | 0.25 | 1-4 | 1 | 1 |
| Enterobacter aerogenes (21) | 0.25-1 | 0.5 | 1 | 1->32 | 2 | >32 |
| Enterobacter cloacae (20) | 0.25-0.5 | 0.5 | 0.5 | 1-2 | 2 | 2 |
| Escherichia coli (20) | 0.12-0.5 | 0.25 | 0.5 | 1->32 | 2 | >32 |
| Escherichia coli, ESBL+ (20) | 0.25-1 | 0.25 | 0.5 | 1->32 | >32 | >32 |
| Klebsiella oxytoca (19) | 0.25-2 | 0.5 | 2 | 1-8 | 1 | 4 |
| Klebsiella pneumoniae (20) | 0.5-2 | 0.5 | 1 | 1-8 | 2 | 4 |
| Klebsiella pneumoniae, ESBL+ (36) | 0.25-4 | 1 | 2 | 1->32 | >32 | >32 |
| Morganella morganii (20) | 1-8 | 4 | 4 | 2->32 | >32 | >32 |
| Proteus mirabilis (20) | 1-4 | 2 | 4 | 32->32 | >32 | >32 |
| Providencia rettgeri (100) | 0.25-16 | 4 | 4 | 1->32 | 32 | >32 |
| Providencia stuartii (98) | 0.25-8 | 2 | 4 | 2->32 | >32 | >32 |
| Proteus vulgaris (60) | 0.5-2 | 1 | 2 | 1->32 | 8 | 32 |
| Shigella boydii (106) | 0.12-1 | 0.25 | 0.5 | 0.25->32 | >32 | >32 |
| Shigella dysenteriae (92) | 0.12-1 | 0.25 | 0.25 | 1->32 | >32 | >32 |
| Shigella flexneri (100) | 0.06-1 | 0.25 | 0.25 | 0.5->32 | >32 | >32 |
| Shigella sonnei (103) | 0.12-1 | 0.25 | 0.5 | 0.5->32 | >32 | >32 |
| Salmonella enterica | ||||||
| Serovar Enteritidis (100) | 0.12-2 | 0.5 | 1 | 0.5->32 | 1 | >32 |
| Serovar Paratyphi (111) | 0.12-2 | 0.5 | 1 | 0.5->32 | 1 | 32 |
| Serovar Typhi (105) | 0.06-1 | 0.25 | 0.5 | 0.25->32 | 1 | 4 |
| Serovar Typhimurium (100) | 0.25-2 | 1 | 2 | 1->32 | >32 | >32 |
| Serratia marcescens (20) | 1-4 | 1 | 2 | 8->32 | 16 | >32 |
| All non-Enterobacteriaceae combined (153) | 0.06-32 | 0.5 | 8 | 0.12->32 | 4 | >32 |
| All Acinetobacter spp. (41) | 0.12-4 | 0.5 | 2 | 0.25->32 | 2 | 8 |
| Burkholderia cepacia (32) | 0.06-16 | 1 | 8 | 0.12->32 | >32 | >32 |
| Pseudomonas aeruginosa (20) | 8-32 | 16 | 16 | 16->32 | 32 | >32 |
| Pasteurella multocida (40) | 0.06-0.25 | 0.06 | 0.25 | 0.12-32 | 1 | 16 |
| Stenotrophomonas maltophilia (20) | 0.06-8 | 1 | 4 | 0.25-32 | 8 | 32 |
n, no. of strains.
S, sensitive; I, intermediate; R, resistant.
Figure 1A to F shows the scattergrams of tigecycline MICs versus disk diffusion zone diameters. FDA susceptible-only MIC breakpoints and disk diffusion breakpoints for tigecycline of ≤0.25 μg/ml and ≥19 mm for the nonpneumococcal streptococci and enterococci and ≤0.5 μg/ml and ≥19 mm for the staphylococci and MIC breakpoints of ≤2, 4, and 8 μg/ml and ≥19 mm, 15 to 18 mm, and ≤14 mm for susceptible, intermediate, and resistant for the Enterobacteriaceae were confirmed (Table 2). Provisional susceptible-only breakpoints of ≤1 μg/ml and ≥19 mm for Haemophilus spp. and ≤0.25 μg/ml and ≥19 mm for S. pneumoniae are proposed based on the data from this study. The zone diameter breakpoints proposed were designed to minimize the interpretive discrepancies between the two types of susceptibility testing methods.
TABLE 2.
FDA-approved susceptibility test result interpretive criteria for tigecycline
| Pathogen | MIC (μg/ml)a
|
Disk diffusion (zone diam, mm)
|
||||
|---|---|---|---|---|---|---|
| S | I | R | S | I | R | |
| S. aureus | ≤0.5 | ≥19 | ||||
| Streptococcus spp. other than S. pneumoniae | ≤0.25 | ≥19 | ||||
| E. faecalis (vancomycin susceptible only) | ≤0.25 | ≥19 | ||||
| Enterobacteriaceaeb | ≤2 | 4 | ≥8 | ≥19 | 15-18 | ≤14 |
The current absence of resistant isolates precludes defining any results other than “susceptible.” Isolates yielding MIC results suggestive of the “nonsusceptible” category should be submitted to a reference laboratory for further testing.
Tigecycline has decreased in vitro activity against Morganella spp., Proteus spp., and Providencia spp.
The error rates for the majority of species were within the limits established by the CLSI (17). The profound activity of tigecycline against all gram-positive isolates is readily apparent. The error rates for S. pneumoniae and Streptococcus spp. other than S. pneumoniae (Fig. 1B), the enterococci (Fig. 1C), and Haemophilus spp. (Fig. 1F) were all zero. The staphylococcal isolates (44 S. aureus isolates and 86 coagulase negative staphylococci) showed 5 strains above the S. aureus FDA sensitive-only breakpoint, including one strain of S. haemolyticus which was 2 dilutions above and the 4 strains (3 coagulase-negative staphylococci and a single strain of S. aureus known to be methicillin resistant and vancomycin intermediate) which were 1 dilution above the breakpoint (Fig. 1A). This strain of S. aureus was retested recently and had a tigecycline MIC of 0.5 μg/ml on retest.
The very major and minor error rates for the Enterobacteriaceae (Fig. 1D) were high. The vast majority of these errors were due to Morganella morganii, Proteus spp. other than P. vulgaris, and Providencia spp. If these strains were eliminated from consideration, the very-major-error rate would drop to 0 while minor error rates would drop to 3 out of 1,054 isolates or 0.3% (Fig. 1E). Included among these strains are isolates known to produce ESBLs.
Quality control studies.
Quality control ranges for MIC testing were proposed on the basis of the modal MICs observed ± 1 log2 dilution. If the MIC distribution was bimodal, then a four-dilution range was proposed. Disk diffusion zone diameter ranges were proposed using the method of Gavan et al. (9) with adjustments as needed in order to encompass at least 95% of observed values. The proposed MIC and zone diameter ranges are presented in Tables 4 and 5, respectively. These quality control ranges were accepted by the Antimicrobial Susceptibility Testing Subcommittee of the CLSI at their January 2004 and June 2004 meetings and later by the FDA.
TABLE 4.
Tigecycline MIC quality control
| Quality control strain | No. of occurrences at MIC (μg/ml) ofa,b:
|
% in rangec | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.015 | 0.03 | 0.06 | 0.12 | 0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | 32 | 64 | ||
| E. coli ATCC 25922 | 0 | 0 | 401 | 176 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| S. aureus ATCC 29213 | 0 | 48 | 194 | 277 | 61 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 99.5 |
| E. faecalis ATCC 29212 | 0 | 86 | 374 | 132 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 99.2 |
| S. pneumoniae ATCC 49619 | 0 | 146 | 90 | 4 | 0 | 0 | 0 | 0 | 100 | |||||
| H. influenzae ATCC 49247 | 0 | 0 | 9 | 107 | 113 | 11 | 0 | 0 | 100 | |||||
The target of 600 replicates per strain was not met for all test species.
Numbers within recommended quality control ranges are represented in bold.
Percentage of results which fall within the recommended range. Acceptable limit, ≥95%.
TABLE 5.
Number of occurrences at each zone diameter for tigecycline disk diffusion quality control
| Zone diam (mm) | No. of occurrences for strain (% within range)a:
|
|||||
|---|---|---|---|---|---|---|
| E. coli ATCC 25922 (99.0) | S. aureus ATCC 25923 (99.1) | P. aeruginosa ATCC 27853 (99.0) | S. pneumoniae ATCC 49619 (99.0) | N. gonorrhoeae ATCC 49226 (99.2) | H. influenzae ATCC 49247 (97.9) | |
| 8 | 1 | |||||
| 9 | 48 | |||||
| 10 | 136 | |||||
| 11 | 206 | |||||
| 12 | 83 | |||||
| 13 | 4 | |||||
| 14 | 2 | |||||
| 15 | ||||||
| 16 | ||||||
| 17 | ||||||
| 18 | ||||||
| 19 | 5 | 1 | ||||
| 20 | 10 | 18 | ||||
| 21 | 25 | 47 | 1 | 2 | ||
| 22 | 16 | 132 | 2 | 7 | ||
| 23 | 58 | 143 | 37 | 9 | ||
| 24 | 123 | 78 | 111 | 5 | ||
| 25 | 160 | 32 | 104 | 29 | ||
| 26 | 70 | 2 | 99 | 2 | 46 | |
| 27 | 11 | 1 | 40 | 69 | ||
| 28 | 2 | 48 | 1 | 89 | ||
| 29 | 27 | 1 | 81 | |||
| 30 | 3 | 10 | 57 | |||
| 31 | 24 | 22 | ||||
| 32 | 41 | |||||
| 33 | 53 | |||||
| 34 | 72 | |||||
| 35 | 93 | |||||
| 36 | 79 | |||||
| 37 | 50 | |||||
| 38 | 34 | |||||
| 39 | 10 | |||||
| 40 | 7 | |||||
| 41 | 1 | |||||
| 42 | ||||||
Numbers within recommended quality control ranges are represented in bold.
DISCUSSION
The in vitro activity of tigecycline against gram-positive strains, M. catarrhalis, N. meningitidis, and H. influenzae, was excellent. Tigecycline was consistently more potent than tetracycline against all species under study. MICs were not significantly affected by increasing resistance to penicillin (S. pneumoniae), oxacillin (staphylococci), or vancomycin (enterococci) or the presence of ESBLs (E. coli and K. pneumoniae). Tentative disk diffusion breakpoints based upon provisional MIC breakpoints can be proposed for S. pneumoniae and Haemophilus spp., and FDA-approved breakpoints are confirmed for the other species. The following MIC and/or disk diffusion quality control ranges were established: S. aureus ATCC 29213, 0.03 to 0.25 μg/ml; S. aureus ATCC 25923, 20 to 25 mm; E. coli ATCC 25922, 0.03 to 0.25 μg/ml and 20 to 27 mm, E. faecalis ATCC 29212, 0.03 to 0.12 μg/ml; P. aeruginosa ATCC 27853, 9 to 13 mm; S. pneumoniae ATCC 49619, 0.015 to 0.12 μg/ml and 23 to 29 mm; H. influenzae ATCC 49247, 0.06 to 0.5 μg/ml and 23 to 31 mm; and N. gonorrhoeae ATCC 49226, 30 to 40 mm. These quality control ranges for both MIC and disk diffusion methodologies have been accepted and published by the CLSI and are in the package insert for tigecycline.
Acknowledgments
Financial support for this project was provided by Wyeth Research, Pearl River, NY.
Footnotes
Published ahead of print on 9 May 2007.
REFERENCES
- 1.Betriu, C., E. Culebras, I. Rodriguez-Avial, M. Gomez, B. A. Sanchez, and J. J. Picazo. 2004. In vitro activities of tigecycline against erythromycin-resistant Streptococcus pyogenes and Streptococcus agalactiae; mechanisms of macrolide and tetracycline resistance. Antimicrob. Agents Chemother. 48:323-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boucher, H. W., C. B. Wennersten, and G. M. Eliopoulos. 2000. In vitro activities of the glycylcycline GAR-936 against gram-positive bacteria. Antimicrob. Agents Chemother. 44:2225-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouchillon, S. K., D. J. Hoban, B. M. Johnson, J. L. Johnson, A. Hsiung, and M. J. Dowzicky. 2005. In vitro activity of tigecycline against 3,989 gram-negative and gram-positive clinical isolates from the United States Tigecycline Evaluation and Surveillance Trial (TEST Program: 2004). Diagn. Microbiol. Infect. Dis. 52:173-179. [DOI] [PubMed] [Google Scholar]
- 4.Bouchillon, S. K., D. J. Hoban, B. M. Johnson, T. M. Stevens, M. J. Dowzicky, D. H. Wu, and P. A. Bradford. 2005. In vitro evaluation of tigecycline and comparative agents in 3,049 clinical isolates; 2001 to 2002. Diagn. Microbiol. Infect. Dis. 51:291-295. [DOI] [PubMed] [Google Scholar]
- 5.Bradford, P. A., P. J. Petersen, M. Young, C. H. Jones, M. Tischler, and J. O'Connell. 2005. Tigecycline MIC testing by broth dilution requires use of fresh medium or addition of the biocatalytic oxygen-reducing reagent Oxyrase to standardize the test method. Antimicrob. Agents Chemother. 49:3903-3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradford, P. A., D. T. Weaver-Sands, and P. J. Petersen. 2005. In vitro activity of tigecycline against isolates from patients enrolled in phase 3 clinical trials of treatment for complicated skin and skin-structure infections and complicated intra-abdominal infections. Clin. Infect. Dis. 41(Suppl. 5):315-332. [DOI] [PubMed] [Google Scholar]
- 7.Clinical and Laboratory Standards Institute. 2005. Performance standards for antimicrobial susceptibility testing: approved standard M100-S15, 15th informational supplement, vol. 25. Clinical and Laboratory Standards Institute, Wayne, PA.
- 8.Gales, A. C., R. N. Jones, S. S. Andrade, A. S. Pereira, and H. S. Sader. 2005. In vitro activity of tigecycline, a new glycylcycline, tested against 1,326 clinical bacterial strains isolated from Latin America. Braz. J. Infect. Dis. 9:348-356. [DOI] [PubMed] [Google Scholar]
- 9.Gavan, T. L., R. N. Jones, A. L. Barry, P. C. Fuchs, E. H. Gerlach, J. M. Matsen, L. B. Reller, C. Thornsberry, and L. D. Thrupp. 1981. Quality control limits for ampicillin, carbenicillin, mezlocillin, and piperacillin disk diffusion susceptibility tests: a collaborative study. J. Clin. Microbiol. 14:67-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein, E. J., D. M. Citron, C. V. Merriam, Y. Warren, and K. Tyrrell. 2000. Comparative in vitro activities of GAR-936 against aerobic and anaerobic animal and human bite wound pathogens. Antimicrob. Agents Chemother. 44:2747-2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoellman, D. B., G. A. Pankuch, M. R. Jacobs, and P. C. Appelbaum. 2000. Antipneumococcal activities of GAR-936 (a new glycylcycline) compared to those of nine other agents against penicillin-susceptible and -resistant pneumococci. Antimicrob. Agents Chemother. 44:1085-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitzis, M. D., A. Ly, and F. W. Goldstein. 2004. In vitro activities of tigecycline (GAR-936) against multidrug-resistant Staphylococcus aureus and Streptococcus pneumoniae (letter). Antimicrob. Agents Chemother. 48:366-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Low, D. E., B. N. Kreiswirth, K. Weiss, and B. M. Willey. 2002. Activity of GAR-936 and other antimicrobial agents against North American isolates of Staphylococcus aureus. Int. J. Antimicrob. Agents 20:220-222. [DOI] [PubMed] [Google Scholar]
- 14.Milatovic, D., F. J. Schmitz, J. Verhoef, and A. C. Fluit. 2003. Activities of the glycylcycline tigecycline (GAR-936) against 1,924 recent European clinical bacterial isolates. Antimicrob. Agents Chemother. 47:400-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Committee for Clinical Laboratory Standards. 2003. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard M7-A6. CLSI, Wayne, PA.
- 16.National Committee for Clinical Laboratory Standards. 2003. Performance standards for antimicrobial disk susceptibility tests: approved standard M2-A8. CLSI, Wayne, PA.
- 17.National Committee for Clinical Laboratory Standards. 2001. Development of in vitro susceptibility testing criteria and quality control parameters: approved standard M23-A2. CLSI, Wayne, PA.
- 18.National Committee for Clinical Laboratory Standards. 2004. Performance standards for antimicrobial susceptibility testing: approved standard M100-S14, 14th informational supplement, vol. 24. CLSI, Wayne, PA.
- 19.Pachon-Ibanez, M. E., M. E. Jimenez-Mejias, C. Pichardo, A. C. Llanos, and J. Pachon. 2004. Activity of tigecycline (GAR-936) against Acinetobacter baumannii strains, including those resistant to imipenem. Antimicrob. Agents Chemother. 48:4479-4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel, R., M. S. Rouse, K. E. Piper, and J. M. Steckelberg. 2000. In vitro activity of GAR-936 against vancomycin-resistant enterococci, methicillin-resistant Staphylococcus aureus and penicillin-resistant Streptococcus pneumoniae. Diagn. Microbiol. Infect. Dis. 38:177-179. [DOI] [PubMed] [Google Scholar]
- 21.Petersen, P. J., and P. A. Bradford. 2005. Effect of medium age and supplementation with the biocatalytic oxygen-reducing reagent oxyrase on in vitro activities of tigecycline against recent clinical isolates. Antimicrob. Agents Chemother. 49:3910-3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petersen, P. J., P. A. Bradford, W. J. Weiss, T. M. Murphy, P. E. Sum, and S. J. Projan. 2002. In vitro and in vivo activities of tigecycline (GAR-936), daptomycin, and comparative antimicrobial agents against glycopeptide-intermediate Staphylococcus aureus and other resistant gram-positive pathogens. Antimicrob. Agents Chemother. 46:2595-2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen, P. J., N. V. Jacobus, W. J. Weiss, P. E. Sum, and R. T. Testa. 1999. In vitro and in vivo antibacterial activities of a novel glycylcycline, the 9-t-butylglycylamido derivative of minocycline (GAR-936). Antimicrob. Agents Chemother. 43:738-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sum, P. E., and P. Petersen. 1999. Synthesis and structure-activity relationship of novel glycylcycline derivatives leading to the discovery of GAR-936. Bioorg. Med. Chem. Lett. 9:1459-1462. [DOI] [PubMed] [Google Scholar]