Abstract
The abilities to infect and transmit efficiently among humans are essential for a novel influenza A virus to cause a pandemic. To evaluate the pandemic potential of widely disseminated H5N1 influenza viruses, a ferret contact model using experimental groups comprised of one inoculated ferret and two contact ferrets was used to study the transmissibility of four human H5N1 viruses isolated from 2003 to 2006. The effects of viral pathogenicity and receptor binding specificity (affinity to synthetic sialosaccharides with α2,3 or α2,6 linkages) on transmissibility were assessed. A/Vietnam/1203/04 and A/Vietnam/JP36-2/05 viruses, which possess “avian-like” α2,3-linked sialic acid (SA) receptor specificity, caused neurological symptoms and death in ferrets inoculated with 103 50% tissue culture infectious doses. A/Hong Kong/213/03 and A/Turkey/65-596/06 viruses, which show binding affinity for “human-like” α2,6-linked SA receptors in addition to their affinity for α2,3-linked SA receptors, caused mild clinical symptoms and were not lethal to the ferrets. No transmission of A/Vietnam/1203/04 or A/Turkey/65-596/06 virus was detected. One contact ferret developed neutralizing antibodies to A/Hong Kong/213/03 but did not exhibit any clinical signs or detectable virus shedding. In two groups, one of two naïve contact ferrets had detectable virus after 6 to 8 days when housed together with the A/Vietnam/JP36-2/05 virus-inoculated ferrets. Infected contact ferrets showed severe clinical signs, although little or no virus was detected in nasal washes. This limited virus shedding explained the absence of secondary transmission from the infected contact ferret to the other naïve ferret that were housed together. Our results suggest that despite their receptor binding affinity, circulating H5N1 viruses retain molecular determinants that restrict their spread among mammalian species.
As H5N1 influenza viruses expand their geographic and host range, whether the viruses have gradually acquired the characteristics that allow efficient transmission between humans is of great concern. To date, transmission to humans has been inefficient, occurring through close contact with infected poultry or consumption of its undercooked meat or blood (42), and reported probable human-to-human transmission has been limited (6, 37, 42). H5N1 virus may acquire efficient interhuman transmissibility in two predicted ways: genetic reassortment with circulating human influenza A viruses or the accumulation of mutations during adaptation in mammalian hosts (1, 15, 39). Incompatibility between the hemagglutinin (HA) of avian origin with matrix (M) gene segments of human origin (32, 33) and the recent observation that H5N1 avian-human reassortant viruses lack the ability to transmit between ferrets suggest that the genetic basis of influenza virus transmissibility may be highly complex (22). On the other hand, incidents of direct transmission of H5N1 viruses from infected domestic or wild aquatic birds to mammalian hosts (humans, felids, and stone martens) continue to be reported (5, 40, 45). These incidences of direct avian to mammalian transmission events may allow the H5N1 viruses to gradually become adapted to and spread among mammalian species, including humans.
There is limited knowledge about the potential routes and determinants required for H5N1 influenza virus transmission between humans. Receptor distribution in the human airway is proposed to restrict efficient interhuman transmission of H5N1 influenza virus (34). Human influenza viruses specifically recognize α2,6-linked sialic acid (SA) receptors, which are dominant on epithelial cells in the upper respiratory tract (34). In contrast, avian influenza viruses specifically recognize α2,3-linked SA receptors, which are located in the lower respiratory tract (34, 38) and are not easily reached by the large droplets (diameter of >10 μm) produced by coughing or sneezing (2). Amino acid changes in the receptor binding site of the HA glycoprotein may alter the virus receptor binding specificity, as observed with initial isolates from the human pandemics of 1918 (H1N1), 1957 (H2N2), and 1968 (H3N2) (24, 36). Because some of the circulating H5N1 avian viruses have demonstrated uncharacteristic affinity for α2,6-linked SA receptors (35, 43), it is important to evaluate their transmissibility in a suitable animal model.
Domestic ferrets (Mustela putorius furo, together with cats, dogs, and martens, which taxonomically belong to the order Carnivora) have been shown to be an appropriate animal model (21) for study of the pathogenicity (8, 23) and transmissibility (11, 12) of influenza viruses. On the basis of H5N1 virus cell tropism in their lower respiratory tract, ferrets have also been proposed to be a good small-animal model of human H5N1 pneumonia (38). Since 1997, highly pathogenic H5N1 viruses have evolved into multiple genetic clades and differ in their pathogenicity to mammalian species (8, 23, 31, 41). Some H5N1 viruses, particularly those isolated from humans, spread systemically to multiple organs of inoculated ferrets (8, 23, 31); however, it is not known whether this effect is predictive of efficient interhost spread. In the present study, we used a ferret contact model to study the transmissibility of four representative H5N1 viruses isolated from humans from 2003 to 2006. These isolates, selected from two different clades based on the HA phylogenetic tree of circulating H5N1 viruses, differ in their pathogenicity and in their affinity for avian-like (α2,3-linked SA) and human-like (α2,6-linked SA) receptors.
MATERIALS AND METHODS
Viruses and cells.
The A/Hong Kong/213/03 (HK/03), A/Vietnam/1203/04 (VN/04), A/Vietnam/JP36-2/05 (VN/05), and A/Turkey/65-596/06 (TK/06) human H5N1 influenza virus isolates were obtained through the WHO Global Influenza Surveillance Network. Recombinant A/Wuhan/359/05 (Wuhan/95) (H3N2) virus was generated as described previously (44). Experiments were conducted in an USDA-approved biosafety level 3+ containment facility. Experiments with recombinant Wuhan/95 (H3N2) virus (44) were conducted in a biosafety level 2 animal laboratory. Madin-Darby canine kidney (MDCK) cells were obtained from the American Type Culture Collection (Manassas, VA) and were maintained as described previously (44).
Infectivity.
The 50% tissue culture infectious dose (TCID50) and PFU were determined in MDCK cells after incubation at 37°C for 3 days, and the 50% egg infectious dose (EID50) was determined in 10-day-old embryonated chicken eggs. TCID50 and EID50 values were calculated by the Reed-Muench method (29).
Binding of virus to sialic acid-containing substrates.
Virus binding affinity to fetuin (possessing both α2,3- and α2,6-linked SA) was tested in a direct solid-phase assay with the immobilized virus and horseradish peroxidase-conjugated fetuin (7). Virus binding affinity to sialylglycopolymers obtained by conjugation of a 1-N-glycyl derivative of 3′-sialyllactose (p3′SL) or 6′-sialyllactose (p6′SL) was tested by competitive assay based on inhibition of binding to peroxidase-labeled fetuin (25). The dissociation constants of virus-receptor analog complexes were calculated as the means of four individual experiments for each virus.
Transmissibility in the ferret contact model.
Transmissibility was tested in 4- to 6-month-old female ferrets of similar body weight (mean ± standard deviation [SD], 0.75 ± 0.07 kg) obtained through the ferret breeding program at St. Jude Children's Research Hospital or from Marshall Farms (North Rose, NY). All studies were conducted under applicable laws and guidelines and after approval from the St. Jude Children's Research Hospital Animal Care and Use Committee. Ferrets that were seronegative by the HA inhibition test to circulating influenza B viruses and H1N1, H3N2, and H5N1 influenza A viruses were used for the study of Wuhan/95 (H3N2) virus; most ferrets used for the study of H5N1 virus possessed low HA inhibition antibody titers (1:20 to 1:80) to A/New York/55/04 (H3N2) virus (see Table 3). To study the transmissibility of the virus, each experimental group comprised one inoculated ferret and two naïve contact ferrets. Ferrets were inoculated intranasally with 103 TCID50 of virus in 0.5 ml sterile phosphate-buffered saline under isoflurane anesthesia. At 2 days postinoculation (dpi), two naïve contact ferrets were placed in the same cage with each inoculated ferret. To monitor virus shedding, nasal washes and rectal swabs were collected from all ferrets every other day for 14 days and were titrated in MDCK cells. Seroconversion was monitored by determining the neutralizing antibody titers of the preexposure and postexposure ferret sera collected before and after 21 days of shared housing by the method described previously (9). The susceptibility of ferrets (inoculated and contact) that survived after a 21-day observation period was also confirmed by reinfecting them intranasally with 103 TCID50 of homologous virus (rechallenge was done for one experimental group per virus). Nasal washes and rectal swabs were collected from rechallenged ferrets every other day (from 2 to 8 dpi) to monitor whether the presence of neutralizing antibody can prevent virus shedding.
TABLE 3.
Ferret postexposure neutralizing antibody titers and virus shedding after rechallenge
| Virus | Study group | Neutralizing antibody titer in ferreta
|
Virus shedding after rechallenge in ferretb
|
||||
|---|---|---|---|---|---|---|---|
| Inoculated | Contact 1 | Contact 2 | Inoculated | Contact 1 | Contact 2 | ||
| HK/03 | 1 | 1:5,120 | < | < | ND | ND | ND |
| 2 | 1:5,120c | <c | 1:80c | − | + | − | |
| VN/04 | 1 | 1:1,280c | <c | <c | ND | ND | ND |
| 2 | NAVc | <c | <c | NAV | + | + | |
| VN/05 | 1 | 1:1,280c | <c | 1:1,280c | ND | ND | ND |
| 2 | NAVc | NAVc | <c | NAV | NAV | + | |
| TK/06 | 1 | 1:2,560c | <c | <c | − | + | + |
Sera were collected from the one inoculated ferret and the two contact ferrets in each experimental group after they had been housed together for 21 days. Neutralizing antibodies to homologous virus (100 TCID50) were titrated in MDCK cells. NAV, not available (animal died due to severe symptoms during the transmission experiment); <, titer of <1:20.
Ferrets that survived the transmission experiments were rechallenged intranasally with 103 TCID50 of homologous virus. Nasal washes and rectal swabs were collected every other day to detect virus shedding. +, virus shedding detected; −, virus shedding was not detected; ND, rechallenge of the homologous virus was not done in these ferrets.
This ferret exhibited an antibody titer of 1:20 to 1:80 against A/New York/55/04 (H3N2) virus by hemagglutination inhibition assay prior to the experiment.
Collection and virus titration of organs.
To determine the tropism and replication efficiency of the H5N1 viruses in ferret organs, we inoculated two ferrets with 103 TCID50 of each H5N1 virus and collected tissues at 5 dpi. Tissues were weighed and homogenized in sterile phosphate-buffered saline with antibiotics. Virus titers were measured in MDCK cells (lower detection limit, 101.5 TCID50/gram) and expressed as TCID50/gram tissue. Tissues were also fixed in 10% neutral buffered formalin and embedded in paraffin for histology examination or immunohistochemistry.
Histology analysis and immunohistochemistry.
Formalin-fixed and paraffin-embedded tissue sections were stained with hematoxylin and eosin for histological evaluation or with pooled monoclonal antibodies against influenza A virus nucleoprotein (NP) protein for detection of influenza viral antigen. Lung and brain tissue samples from a ferret inoculated with VN/04 virus were used as a positive control (high virus titers were detected in the lungs and brain from the same inoculated ferret).
Reverse transcription-PCR and virus sequencing.
Viral RNAs were isolated from allantoic fluid or cell culture supernatant (RNeasy; QIAGEN) and one-step reverse transcription-PCR was done with a universal primer set (14). The Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children's Research Hospital analyzed the sequences on Applied Biosystem 3700 DNA analyzers by using BigDye Terminator (v. 3) chemistry and synthetic oligonucleotides.
RESULTS
Selection and characterization of H5N1 viruses.
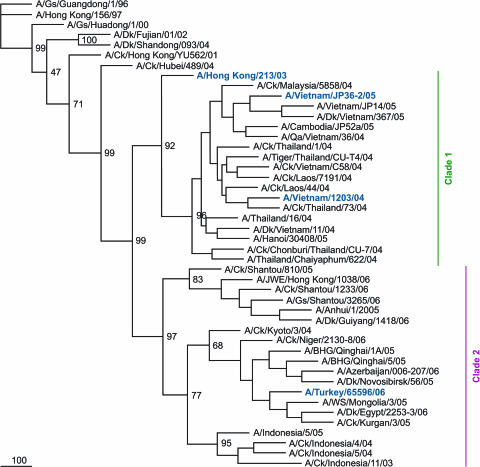
To obtain a broad representation of the genetic clades of circulating H5N1 viruses, four H5N1 human isolates were selected from clades 1 (HK/03, VN/04, and VN/05 viruses) and 2 (TK/06 virus) based on the phylogenetic analysis of the HA genes (Fig. 1). The selected H5N1 isolates had a history of limited passages in order to preserve potential molecular changes important for avian-human transmission (Table 1). Three of these isolates contained amino acid changes in the conserved HA receptor binding residues. The HK/03 and TK/06 viruses contained N at residue 223 rather than the conserved S223; VN/05 virus contained A at residue 133, whereas S133 is conserved in H5 HA (Table 1).
FIG. 1.
Phylogenetic tree based on the HA gene (nucleotides 77 to 1200, 1,124 bp) of H5N1 influenza A viruses. The nucleotide sequences were analyzed by Phylip3.65 software using the neighbor-joining method with 100 bootstraps. The tree was rooted to the A/Gs/Guandong/1/96 HA sequence. Viruses in colored bold type were included in this study. Abbreviations: Ck, chicken; Dk, duck; Gs, goose; Qa, quail; JWE, Japanese white eye; WS, whooper swan; BHG, bar-headed goose.
TABLE 1.
Affinity of the H5N1 influenza viruses to sialyl substrates
| Virusa | Changes in HA receptor binding siteb | Affinity for sialyl substratec
|
||
|---|---|---|---|---|
| Fetuin | p6′SL | p3′SL | ||
| HK/03 (E2/E1) | S133, N223 | 0.18 ± 0.03 | 5.78 ± 0.82c | 1.05 ± 0.21 |
| VN/04 (E2/E1) | S133, S223 | 0.13 ± 0.03 | >100 | 1.21 ± 0.05 |
| VN/05 (C1/E1) | A133, S223 | 0.15 ± 0.08 | >100 | 0.12 ± 0.02d |
| TK/06 (E2/E1) | S133, N223 | 0.15 ± 0.06 | 10.34 ± 1.40c | 0.44 ± 0.05 |
Virus abbreviations: HK/03, A/HK/213/03; VN/04, A/VN/1203/04; VN/05, A/VN/JP36-2/05; TK/06, A/Turkey/65-596/06. Virus passage history is indicated in parentheses after the virus as follows: C, passaged in MDCK cells; E, passaged in embryonated chicken eggs (e.g., E2/E1, virus was passaged twice in embryonated chicken eggs prior to arrival at St. Jude's Children's Research Hospital; it was subsequently passaged once in eggs prior to the experiments).
Changes in conserved residues. H5 numbering was used.
The dissociation constant Kdiss = mean ± standard error × tα,n−1 (μM sialic acid), where tα is Student's coefficient with probability α = 0.95, from four independent experiments. Fetuin possesses both α2,3- and α2,6-linked SA, while p3′SL and p6′SL are synthetic sialosaccharides with α2,3 and α2,6 linkages, respectively.
Significantly different from the value for other viruses (P < 0.05 by analysis of variance).
We measured the receptor binding affinity of the four H5N1 viruses to high-molecular-weight sialic substrates. As shown by the dissociation constants (Table 1), all isolates exhibited affinity for p3′SL (synthetic sialosaccharides with α2,3 linkage). The HK/03 and TK/06 viruses showed a greater affinity for p6′SL (synthetic sialosaccharides with α2,6 linkage) than is typical of avian H5N1 influenza viruses, and both of these viruses had an N substitution at HA receptor binding residue 223. These results were consistent with previous reports (13, 35) that N223 may lead to changes of receptor binding affinity and/or specificity of the H5 HA glycoprotein.
The growth and infectivity of the H5N1 viruses were comparable in MDCK cells and embryonated chicken eggs (Table 2). Differences were observed between the isolates in plaque morphology: VN/04 and TK/06 viruses formed homogeneous large plaques (mean diameter ± SD, 2.6 ± 0.4 mm), VN/05 virus formed a mixture of small and medium-sized plaques (1.0 ± 0.6 mm), and HK/03 virus formed homogeneous small plaques (0.5 ± 0.1 mm).
TABLE 2.
Growth of the H5N1 influenza viruses
| Virus | Virus growtha
|
||
|---|---|---|---|
| Log10 TCID50/ml | Log10 PFU/ml | Log10 EID50/ml | |
| HK/03 | 8.5 ± 0.0 | 8.1 ± 0.03 | 8.5 ± 0.4 |
| VN/04 | 9.0 ± 0.0 | 9.1 ± 0.01 | 9.5 ± 0.3 |
| VN/05 | 8.4 ± 0.2 | 8.4 ± 0.1 | 9.3 ± 0.4 |
| TK/06 | 8.5 ± 0.0 | 8.3 ± 0.3 | 8.8 ± 0.4 |
All data are the mean ± SDs from three independent experiments.
Transmission in ferrets.
We showed previously that our ferret contact model is suitable for transmissibility studies of human H3N2 viruses (44). Applying the same experimental design, we assessed the transmissibility of each H5N1 virus in two independent ferret groups (the TK/06 virus was studied in only one ferret group).
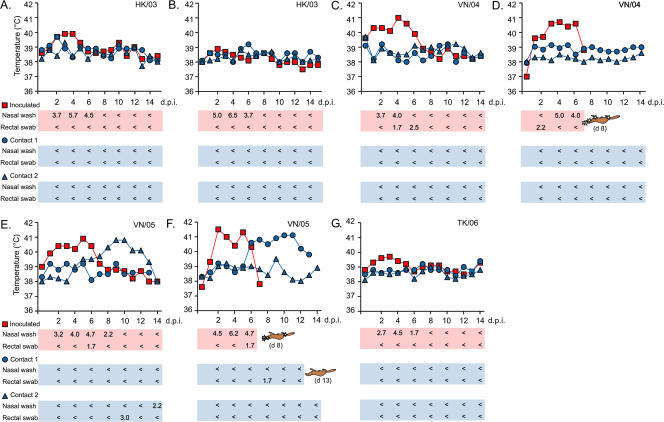
No significant difference was observed between the four viruses' nasal wash titers on days 2, 4, and 6 after inoculation with 103 TCID50 (Fig. 2). Nasal wash titers usually peaked at 4 dpi (range, 2 to 6 dpi), and peak titers were 4.0 to 6.5 log10 TCID50. Between 2 and 6 dpi, virus (1.7 to 2.5 log10 TCID50) was also detected in the rectal swabs of ferrets inoculated with VN/04 and VN/05 (Fig. 2).
FIG. 2.
Temperature changes and virus titers of human H5N1 influenza viruses in a ferret contact model. Virus titers (log10 TCID50/ml) are shown (<, below detection limit of 101.5 TCID50/ml). Shown are results for one donor ferret (inoculated) and two recipient (contact) ferrets in two independent tests of each virus. (A and B) HK/03 virus; (C and D) VN/04 virus; (E and F) VN/05 virus; (G) TK/06 virus. Overturned ferret figures indicate time of death (d, day), and the yellow stars indicate sites of virus isolation (virus was detected in the nasal turbinate, olfactory bulb, brain, trachea, lungs, and large intestine of an VN/04-inoculated ferret in panel D; virus was detected in the nasal turbinate, olfactory bulb, brain, and large intestine in panel F).
Transmission of virus from inoculated donors to naïve contact ferrets was confirmed by virus isolation from nasal washes or rectal swabs and/or by seroconversion. Histopathology examination was performed on ferrets that succumbed to infection. No transmission of the VN/04 or TK/06 virus was detected. One of four contact ferrets exposed to HK/03 had developed neutralizing antibody (titer of 1:80) when tested after 21 days of contact with the inoculated ferret but did not shed detectable virus or show signs of illness (Fig. 2). After rechallenge with HK/03 virus, this contact ferret did not shed virus, whereas the other seronegative (neutralizing antibody titer of <1:20) contact ferrets did (Table 3). These results showed that HK/03 virus is not transmitted efficiently between ferrets and appears not to cause symptomatic infection after transmission.
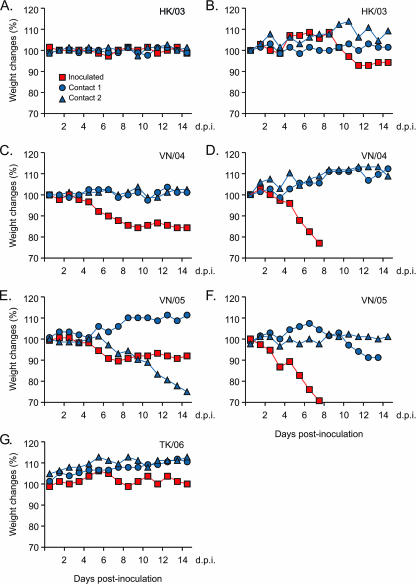
In two independent ferret groups, VN/05 virus was isolated from one of the two naïve contact ferrets of each group after 6 and 8 days of contact with the inoculated ferret, respectively (8 and 10 dpi for the inoculated ferret, respectively) (Fig. 2). One contact ferret in each group remained seronegative after 21 days of contact (Fig. 2 and Table 3), demonstrating the inefficiency of VN/05 transmission as well as the absence of secondary transmission from the infected contact ferret to the other naïve contact. Although virus titers were high in the nasal washes of inoculated ferrets, little or no virus was detected in the nasal washes of the infected contact ferrets (Fig. 2). VN/05 virus was detected on only 1 day in the nasal wash of one infected contact; virus was detected in the rectal swabs of both infected contact ferrets on 1 day (Fig. 2). Despite limited virus detection, both infected contact ferrets showed elevated temperature (maximum elevation of 2.8°C and 2.4°C to the baseline temperature, respectively) (Fig. 2), lethargy, weight loss (24.2% and 11.4% of the original body weight, respectively) (Fig. 3), and neurological signs (uncontrolled movement or hind limb paralysis). One infected contact ferret died after 11 days of contact due to severe clinical symptoms (labored breathing and neurological signs). Although no detectable virus was isolated from the nasal turbinate, brain, olfactory bulb, trachea, lungs, large intestine, or spleen, histological changes were observed in multiple organs (see below), and immunohistochemistry has detected viral antigen (NP) in few cells in the brain and liver (in repeated experiments; data not shown).
FIG. 3.
Ferret weight changes during H5N1 influenza virus transmission experiments. The changes in ferret weight are shown for one donor ferret (inoculated) and two recipient (contact) ferrets in two independent tests of each virus. (A and B) HK/03 virus; (C and D) VN/04 virus; (E and F) VN/05 virus; (G) TK/06 virus. Daily weight changes (as a percentage) of each ferret were compared to its own initial weight prior to the initiation of the experiments.
Compared to the human H3N2 Wuhan/95 virus, which was transmitted efficiently from the inoculated ferret to both naïve contact ferrets after 2 to 4 days of contact (44), the four H5N1 viruses demonstrated inefficient transmissibility in this animal model. However, we observed differences between the four H5N1 viruses. The VN/04 and TK/06 viruses were not transmitted to contact ferrets; the HK/03 virus was transmitted to one contact ferret but was detectable only by seroconversion; and the VN/05 virus was transmitted to one of two contact ferrets in each of the two ferret groups, as shown by virus shedding and/or seroconversion.
Pathogenicity of the H5N1 viruses in ferrets.
The four human H5N1 isolates differed in their pathogenicity in inoculated ferrets. VN/04 and VN/05 were lethal and caused neurological signs, temperature elevation (maximum elevation, 2.4 to 3.7°C), and weight loss (11% to 29%) (Fig. 3) similar to the disease signs previously reported (8, 23). In contrast, ferrets inoculated with the HK/03 and TK/06 viruses showed only slight temperature elevation (0.9 to 1.4°C) and weight loss (2.4% to 9.7%) (Fig. 3).
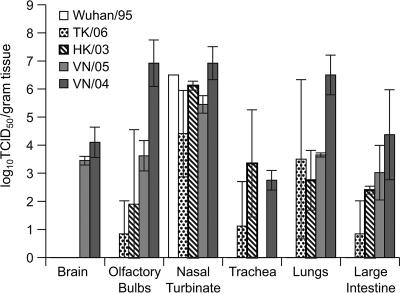
To evaluate virus replication and tissue tropism in the inoculated ferrets, we titrated virus in the nasal turbinate, trachea, lungs, brain, olfactory bulb, and large intestine of two ferrets per virus at 5 dpi (Fig. 4). For comparison, we inoculated one ferret with 103 TCID50 of recombinant Wuhan/95 (H3N2) virus. All four human H5N1 isolates were detected in the olfactory bulb, nasal turbinate, lungs, and large intestine; however, only the VN/04 and VN/05 viruses were detected in the brain (Fig. 4). In contrast, the H3N2 human influenza virus was detected only in the nasal turbinate (Fig. 4). Of the four H5N1 viruses, VN/04 replicated most efficiently in all ferret organs, except in the trachea.
FIG. 4.
Virus titers detected in tissues of inoculated ferrets at 5 days postinoculation. Virus in brain, olfactory bulb, nasal turbinate, trachea, lungs, and large intestine was titrated in MDCK cells. Each data point represents the virus titer (log10 TCID50/gram tissue) (mean ± SD) from two ferrets (data for the Wuhan/95 virus were obtained from one ferret).
Differences in pathogenicity were also apparent on histopathologic examination. In the brains of VN/04- and VN/05-infected ferrets (inoculated or contact ferrets) (Fig. 5A and B), there were multiple foci of meningeal, perivascular, and parenchymal mononuclear cell infiltrates and neuronophagia. H5N1 viral antigen was detected by immunohistochemistry in neurons associated with the brain lesions (Fig. 5B). In the lungs of VN/04 -and VN/05-infected ferrets, there was either moderate bronchopneumonia with extensive bronchiolar and alveolar epithelial necrosis, hypertrophy, and hyperplasia associated with a mixed inflammatory cell infiltrate or a mild focal bronchointerstitial pneumonia (Fig. 5A). In the livers of VN/04- and VN/05-infected ferrets, multifocal hepatitis consisting of biliary epithelial hyperplasia and necrosis, hemorrhage, hepatocellular necrosis, and mixed inflammatory cell infiltrates in the parenchyma and portal tracts was apparent (Fig. 5A). H5N1 viral antigen was also detected by immunohistochemistry in hepatocytes associated with liver lesions (Fig. 5B). In contrast, histological changes were detected only in the lungs of HK/03- and TK/06-infected ferrets, and there were no detectable features of viral infection in the brains or in the livers (Fig. 5A). The lungs had a few foci of bronchopneumonia, involving bronchioles, with minimal alveolar disease and/or interstitial hypercellularity (Fig. 5A).
FIG. 5.
Histopathologic findings in ferrets with H5N1 virus infection. (A) Views of hematoxylin-and-eosin-stained brain, lung, and liver samples of HK/03- and TK/06-inoculated ferrets and a VN/05-infected contact ferret. Uninfected ferret tissues were included as negative controls. Magnification, ×10. (B) Immunohistochemistry detected H5N1 viral antigen in the brain and liver of VN/04-inoculated or VN/05-infected contact ferrets. Magnification, ×20.
Molecular changes during transmission of VN/05 virus.
To monitor the molecular changes during transmission of VN/05 virus, we analyzed the full genome sequences of viruses isolated from the VN/05-infected contact ferrets. We identified five amino acid changes in three gene segments (one in PB1, three in PA, and one in NA) (Table 4) compared to the VN/05 stock virus sequences. Among these five amino acid differences, only the V→L change at residue 341 in PA is consistently observed in the viruses isolated from the two infected contact ferrets. An H→Y change at residue 274 in NA was identified in the virus isolated from the contact ferret in the first experimental group. The H274Y amino acid change has been reported to confer resistance to oseltamivir carboxylate in human H1N1 or H5N1 viruses (4, 10, 19).
TABLE 4.
Molecular changes during transmission of VN/05 influenza virus
| Gene segment | Position | Residue in stock virus | Amino acid change
|
|
|---|---|---|---|---|
| Group 1, contact ferret 2 | Group 2, contact ferret 1 | |||
| PB1 | 123 | T | A/T | A |
| PA | 52 | H | H/R | H/R |
| 341 | V | L | L | |
| 388 | G/S | S | S | |
| NA | 274a | H | Y | H |
N2 numbering was used.
DISCUSSION
We studied the transmissibility of four human H5N1 isolates (collected from 2003 to 2006) that differed in their pathogenicity in ferrets and their binding affinity for synthetic sialosaccharides with α2,3 and α2,6 linkages. The inefficient transmission of both the low-pathogenic HK/03 and the high-pathogenic VN/05 viruses suggests that there is no direct correlation between the viral pathogenicity in ferrets and the transmissibility of the H5N1 viruses in this animal model. However, it was interesting to note that the less pathogenic HK/03 virus caused only asymptomatic infection in one contact ferret, while the more pathogenic VN/05 virus caused severe clinical signs in the infected contact ferrets. The inefficient transmission of HK/03 and the nontransmission of TK/06 virus demonstrate that the observed binding affinity for human-like α2,6-linked SA receptors is not sufficient to allow efficient transmission of H5N1 virus among ferrets. It is likely that further adaptations are required for the surface glycoproteins as well as the internal genes of the avian-derived H5N1 viruses to cooperate efficiently with the mammalian cell machinery.
The four H5N1 human isolates included in the present study may harbor a multiple of virus genomes, some of which could differ in important biological properties. VN/05 virus, which was transmitted inefficiently but reproducibly, may possess molecular determinants in the internal genes that better adapt it to mammalian hosts. Although we could not exclude the possibility that the amino acid changes identified from VN/05 contact ferrets were present in a subpopulation of the virus stock, our results suggest that adaptation and/or selection of the VN/05 virus occurred during transmission. Continuing passaging the transmitted variant among ferrets may elucidate the molecular determinants important for interspecies transmission.
In a previous study using the same experimental design, we found that ferrets inoculated with 103 TCID50 of the human Wuhan/95 (H3N2) influenza virus shed virus in nasal washes for 6 days, with a peak virus titer (6.3 log10 TCID50/ml) at 2 dpi (44). Although some of the H5N1 viruses in this study had comparable peak nasal wash titers (4.0 to 6.5 log10 TCID50), the peak occurred later, at 4 dpi (range, 2 to 6 dpi). Whereas human H3N2 virus was transmitted efficiently from the inoculated ferret to both naïve ferrets after 2 to 4 days of contact (44), transmission of the VN/05 H5N1 viruses was not detected until after 6 to 8 days of contact, consistent with the reported incubation time for human H5N1 infection (4, 16, 28, 42). The observation that Wuhan/95 (H3N2) virus (44) reached peak titer earlier than the four H5N1 human isolates suggests that replication efficiency in the upper respiratory tract may explain the greater transmission efficiency of the Wuhan/95 virus.
The different replication efficiencies of H5N1 and human H3N2 influenza viruses in the upper respiratory tract may reflect preferential targeting of different subsets of human airway epithelial cells by viruses with human-like versus avian-like receptor binding specificity (26). However, it was also shown recently that despite lacking α2, 3-linked SA receptors, productive H5N1 viral replication can still be detected in the ex vivo cultures of human nasopharyngeal, adenoid, and tonsillar tissues with a high inoculation dose (108 to 1010 TCID50/ml or multiplicity of infection of 5.0) (27). Although our receptor binding assay may not reflect the complex nature of SA receptors presented on the airway epithelial cells, the HK/03 and TK/06 viruses show affinity for both types of receptors and may be able to target both subsets of cells. HK/03 virus was shown previously to bind extensively to both bronchial and alveolar cells in lung specimens from healthy humans, whereas human-derived influenza viruses bound more extensively to bronchial cells and avian-derived viruses bound more extensively to alveolar epithelial cells (34). Our histopathologic examination also revealed that HK/03 and TK/06 viruses caused bronchopneumonia in inoculated ferrets, with lesions occurring predominantly in the bronchioles. These results suggest that the detected binding affinity of HK/03 and TK/06 viruses to α2,6-linked receptor (p6′SL) may have allowed them to target a subset of cells similar to those targeted by the human-derived influenza viruses. However, the HK/03 and TK/06 viruses did not show significantly greater replication efficiency in the upper respiratory tract (reflected by nasal wash and nasal turbinate titers) or the trachea than did VN/04 and VN/05 viruses, suggesting that additional molecular determinants restrict their replication efficiency in mammalian cells.
The two contact ferrets infected with VN/05 virus experienced severe pneumonia, neurological signs as well as systemic virus spread, and one died of infection. However, little or no virus was detected in the nasal washes. Inefficient viral replication in the upper respiratory tract, together with pneumonia and systemic virus spread in these contact ferrets, suggests that infection may have initiated in the lower respiratory tract via small infectious droplet nuclei (2) as proposed recently (34). Further, the detection of virus in the rectal swabs of both VN/05-infected contact ferrets suggests that virus may have infected animals via feces-contaminated food or water. Consumption of duck blood or possibly undercooked poultry has been implicated as a risk factor for human H5N1 infection (42), and felids have been infected after feeding on H5N1 virus-infected poultry carcasses (17, 18, 30). In ferrets inoculated with VN/04 and VN/05, virus was shed in the feces, and virus-induced lesions were observed in the liver hepatocytes and biliary ducts. This observation suggests the possibility of systemic virus spreading via blood from the primary infection site (respiratory tract) to multiple organs, including the liver, where virus replication may lead to virus spreading to the intestinal lumen through the hepatobiliary system.
Different mammals (pigs, mice, cats, and ferrets) have been used to study the transmission of H5N1 viruses (3, 18, 20, 22, 30). No transmission in pigs (3) or in BALB/c mice (20) was detected with H5N1 viruses isolated from Vietnam or Thailand in 2004, whereas transmission from a H5N1 virus-inoculated cat to contact cats was reported (18, 30). Using ferrets, the inefficient transmission of H5N1 virus and reassortant H5N1-human virus was recently reported by Maines et al. (22). With the respiratory droplet experimental design (inoculated and contact ferrets placed in adjacent cages separated by a perforated wall), seroconversion without virus isolation was detected in two of three contact ferrets in the A/Hong Kong/486/97 virus group and in one of three ferrets in the H5N1-human reassortant (rg486:VicHANA) group. With the contact experimental design (one inoculated ferret placed in a cage with one contact ferret) (22), no transmission of recent H5N1 viruses (HK/03, A/Indonesia/5/05, or A/VN/30408/05) was observed. In the present study, H5N1 viruses that differed in pathogenicity and binding affinity for synthetic sialosaccharides with α2,3 and α2,6 linkages were selected, and a different experimental design was applied. By placing the inoculated ferret with two naïve contact ferrets in the same cage, we were able to evaluate primary transmission as well as the possibility of secondary transmission. Although we observed seroconversion in one of four contact ferrets in the HK/03 virus group and detected virus in two of four contact ferrets in the VN/05 virus group, one naïve ferret remained seronegative after 21 days of contact with a ferret inoculated with VN/05 virus and with a ferret infected by contact. Therefore, inefficient primary transmission (from the inoculated ferret to one of two contact ferrets) occurred but secondary transmission (from the infected contact to the other naïve contact ferret) did not occur. The scant virus shedding from the VN/05-infected contact ferrets explains the absence of secondary transmission. Our result is consistent with the observations that most human H5N1 infections were due to direct avian-human contact and secondary human-to-human transmission is limited.
Highly pathogenic H5N1 viruses continue to evolve rapidly and to generate new lineages and antigenic variants. Monitoring newly emerged antigenic variants and selecting proper vaccine candidates are important for pandemic preparedness. Overall, our results show that circulating H5N1 viruses, including those with increased receptor binding affinity for human-like synthetic sialosaccharides with α2,6 linkage, are not transmitted efficiently in the ferret contact model. However, the transmission of the HK/03 and VN/05 viruses indicates that some of the circulating H5N1 viruses may transmit better than others in mammals. The available in vitro assays do not allow us to predict the potential transmissibility of H5N1 viruses in mammals. Here we have demonstrated a useful animal model system to evaluate the transmissibility of H5N1 viruses. We propose that future selection of H5N1 vaccine candidates among new antigenic variants should take into account the transmissibility of the virus.
Acknowledgments
We thank the Refik Saydam Hygiene Institute in Turkey, Ahmet F. Oner, and the WHO Global Influenza Surveillance Network for providing the H5N1 viruses; Nicolai V. Bovin for the gift of sialic polymer substrates; David Boltz, Richard Webby, and Christoph Scholtissek for advice; Patrick Seiler, Jennifer Humberd, Cedric Proctor, Jennifer McClaren, and Dorothy Bush for technical assistance; Julie Groff and Betsy Williford for illustrations; and Sharon Naron for editorial assistance.
This study was supported by grants AI95357 and CA21765 from the National Institutes of Health and by the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Published ahead of print on 25 April 2007.
REFERENCES
- 1.Belshe, R. B. 2005. The origins of pandemic influenza—lessons from the 1918 virus. N. Engl. J. Med. 353:2209-2211. [DOI] [PubMed] [Google Scholar]
- 2.Bridges, C. B., M. J. Kuehnert, and C. B. Hall. 2003. Transmission of influenza: implications for control in health care settings. Clin. Infect. Dis. 37:1094-1101. [DOI] [PubMed] [Google Scholar]
- 3.Choi, Y. K., T. D. Nguyen, H. Ozaki, R. J. Webby, P. Puthavathana, C. Buranathal, A. Chaisingh, P. Auewarakul, N. T. Hanh, S. K. Ma, P. Y. Hui, Y. Guan, J. S. Peiris, and R. G. Webster. 2005. Studies of H5N1 influenza virus infection of pigs by using viruses isolated in Vietnam and Thailand in 2004. J. Virol. 79:10821-10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Jong, M. D., T. T. Tran, H. K. Truong, M. H. Vo, G. J. Smith, V. C. Nguyen, V. C. Bach, T. Q. Phan, Q. H. Do, Y. Guan, J. S. Peiris, T. H. Tran, and J. Farrar. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353:2667-2672. [DOI] [PubMed] [Google Scholar]
- 5.Eurosurveillance. 2006. Avian influenza H5N1 detected in German poultry and a United Kingdom wild bird. Eurosurveillance 11:E060406.1. http://www.eurosurveillance.org/ew/2006/060406.asp#1. [PubMed] [Google Scholar]
- 6.Eurosurveillance. 2006. Avian influenza H5N1 outbreaks in Romanian and Danish poultry, and large H5N1 cluster in an Indonesian family. Eurosurveillance 11:E060525.1. http://www.eurosurveillance.org/ew/2006/060525.asp#1. [PubMed]
- 7.Gambaryan, A. S., and M. N. Matrosovich. 1992. A solid-phase enzyme-linked assay for influenza virus receptor-binding activity. J. Virol. Methods 39:111-123. [DOI] [PubMed] [Google Scholar]
- 8.Govorkova, E. A., J. E. Rehg, S. Krauss, H. L. Yen, Y. Guan, M. Peiris, D. T. Nguyen, T. H. Hanh, P. Puthavathana, T. L. Hoang, C. Buranathai, W. Lim, R. G. Webster, and E. Hoffmann. 2005. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J. Virol. 79:2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Govorkova, E. A., R. J. Webby, J. Humberd, J. P. Seiler, and R. G. Webster. 2006. Immunization with reverse-genetics-produced H5N1 influenza vaccine protects ferrets against homologous and heterologous challenge. J. Infect. Dis. 194:159-167. [DOI] [PubMed] [Google Scholar]
- 10.Gubareva, L. V. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199-203. [DOI] [PubMed] [Google Scholar]
- 11.Herlocher, M. L., S. Elias, R. Truscon, S. Harrison, D. Mindell, C. Simon, and A. S. Monto. 2001. Ferrets as a transmission model for influenza: sequence changes in HA1 of type A (H3N2) virus. J. Infect. Dis. 184:542-546. [DOI] [PubMed] [Google Scholar]
- 12.Herlocher, M. L., R. Truscon, S. Elias, H. L. Yen, N. A. Roberts, S. E. Ohmit, and A. S. Monto. 2004. Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J. Infect. Dis. 190:1627-1630. [DOI] [PubMed] [Google Scholar]
- 13.Hoffmann, E., A. S. Lipatov, R. J. Webby, E. A. Govorkova, and R. G. Webster. 2005. Role of specific hemagglutinin amino acids in the immunogenicity and protection of H5N1 influenza virus vaccines. Proc. Natl. Acad. Sci. USA 102:12915-12920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 15.Horimoto, T., and Y. Kawaoka. 2005. Influenza: lessons from past pandemics, warnings from current incidents. Nat. Rev. Microbiol. 3:591-600. [DOI] [PubMed] [Google Scholar]
- 16.Kandun, I. N., H. Wibisono, E. R. Sedyaningsih, Yusharmen, W. Hadisoedarsuno, W. Purba, H. Santoso, C. Septiawati, E. Tresnaningsih, B. Heriyanto, D. Yuwono, S. Harun, S. Soeroso, S. Giriputra, P. J. Blair, A. Jeremijenko, H. Kosasih, S. D. Putnam, G. Samaan, M. Silitonga, K. H. Chan, L. L. Poon, W. Lim, A. Klimov, S. Lindstrom, Y. Guan, R. Donis, J. Katz, N. Cox, M. Peiris, and T. M. Uyeki. 2006. Three Indonesian clusters of H5N1 virus infection in 2005. N. Engl. J. Med. 355:2186-2194. [DOI] [PubMed] [Google Scholar]
- 17.Keawcharoen, J., K. Oraveerakul, T. Kuiken, R. A. Fouchier, A. Amonsin, S. Payungporn, S. Noppornpanth, S. Wattanodorn, A. Theambooniers, R. Tantilertcharoen, R. Pattanarangsan, N. Arya, P. Ratanakorn, D. M. Osterhaus, and Y. Poovorawan. 2004. Avian influenza H5N1 in tigers and leopards. Emerg. Infect. Dis. 10:2189-2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuiken, T., G. Rimmelzwaan, D. van Riel, G. van Amerongen, M. Baars, R. Fouchier, and A. Osterhaus. 2004. Avian H5N1 influenza in cats. Science 306:241. [DOI] [PubMed] [Google Scholar]
- 19.Le, Q. M., M. Kiso, K. Someya, Y. T. Sakai, T. H. Nguyen, K. H. Nguyen, N. D. Pham, H. H. Ngyen, S. Yamada, Y. Muramoto, T. Horimoto, A. Takada, H. Goto, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 20.Lowen, A. C., S. Mubareka, T. M. Tumpey, A. Garcia-Sastre, and P. Palese. 2006. The guinea pig as a transmission model for human influenza viruses. Proc. Natl. Acad. Sci. USA 103:9988-9992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maher, J. A., and J. DeStefano. 2004. The ferret: an animal model to study influenza virus. Lab. Anim. (New York) 33:50-53. [DOI] [PubMed] [Google Scholar]
- 22.Maines, T. R., L. M. Chen, Y. Matsuoka, H. Chen, T. Rowe, J. Ortin, A. Falcon, N. T. Hien, L. Q. Mai, E. R. Sedyaningsih, S. Harun, T. M. Tumpey, R. O. Donis, N. J. Cox, K. Subbarao, and J. M. Katz. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci. USA 103:12121-12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maines, T. R., X. H. Lu, S. M. Erb, L. Edwards, J. Guarner, P. W. Greer, D. C. Nguyen, K. J. Szretter, L. M. Chen, P. Thawatsupha, M. Chittaganpitch, S. Waicharoen, D. T. Nguyen, T. Nguyen, H. H. Nguyen, J. H. Kim, L. T. Hoang, C. Kang, L. S. Phuong, W. Lim, S. Zaki, R. O. Donis, N. J. Cox, J. M. Katz, and T. M. Tumpey. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 79:11788-11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matrosovich, M., A. Tuzikov, N. Bovin, A. Gambaryan, A. Klimov, M. R. Castrucci, I. Donatelli, and Y. Kawaoka. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 74:8502-8512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matrosovich, M. N., A. S. Gambaryan, A. B. Tuzikov, N. E. Byramova, L. V. Mochalova, A. A. Golbraikh, M. D. Shenderovich, J. Finne, and N. V. Bovin. 1993. Probing of the receptor-binding sites of the H1 and H3 influenza A and influenza B virus hemagglutinins by synthetic and natural sialosides. Virology 196:111-121. [DOI] [PubMed] [Google Scholar]
- 26.Matrosovich, M. N., T. Y. Matrosovich, T. Gray, N. A. Roberts, and H. D. Klenk. 2004. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc. Natl. Acad. Sci. USA 101:4620-4624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nicholls, J. M., M. C. Chan, W. Y. Chan, H. K. Wong, C. Y. Cheung, D. L. Kwong, M. P. Wong, W. H. Chui, L. L. Poon, S. W. Tsao, Y. Guan, and J. S. Peiris. 2007. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat. Med. 13:147-149. [DOI] [PubMed] [Google Scholar]
- 28.Oner, A. F., A. Bay, S. Arslan, H. Akdeniz, H. A. Sahin, Y. Cesur, S. Epcacan, N. Yilmaz, I. Deger, B. Kizilyildiz, H. Karsen, and M. Ceyhan. 2006. Avian influenza A (H5N1) infection in eastern Turkey in 2006. N. Engl. J. Med. 355:2179-2185. [DOI] [PubMed] [Google Scholar]
- 29.Reed, L. J., and H. Muench. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 30.Rimmelzwaan, G. F., D. van Riel, M. Baars, T. M. Bestebroer, G. van Amerongen, R. A. Fouchier, A. D. Osterhaus, and T. Kuiken. 2006. Influenza A virus (H5N1) infection in cats causes systemic disease with potential novel routes of virus spread within and between hosts. Am. J. Pathol. 168:176-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salomon, R., J. Franks, E. A. Govorkova, N. A. Ilyushina, H. L. Yen, D. J. Hulse-Post, J. Humberd, M. Trichet, J. E. Rehg, R. J. Webby, R. G. Webster, and E. Hoffmann. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scholtissek, C., R. Rott, M. Orlich, E. Harms, and W. Rohde. 1977. Correlation of pathogenicity and gene constellation of an influenza A virus (fowl plague). I. Exchange of a single gene. Virology 81:74-80. [DOI] [PubMed] [Google Scholar]
- 33.Scholtissek, C., J. Stech, S. Krauss, and R. G. Webster. 2002. Cooperation between the hemagglutinin of avian viruses and the matrix protein of human influenza A viruses. J. Virol. 76:1781-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shinya, K., M. Ebina, S. Yamada, M. Ono, N. Kasai, and Y. Kawaoka. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435-436. [DOI] [PubMed] [Google Scholar]
- 35.Shinya, K., M. Hatta, S. Yamada, A. Takada, S. Watanabe, P. Halfmann, T. Horimoto, G. Neumann, J. H. Kim, W. Lim, Y. Guan, M. Peiris, M. Kiso, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Characterization of a human H5N1 influenza A virus isolated in 2003. J. Virol. 79:9926-9932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stevens, J., O. Blixt, L. Glaser, J. K. Taubenberger, P. Palese, J. C. Paulson, and I. A. Wilson. 2006. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J. Mol. Biol. 355:1143-1155. [DOI] [PubMed] [Google Scholar]
- 37.Ungchusak, K., P. Auewarakul, S. F. Dowell, R. Kitphati, W. Auwanit, P. Puthavathana, M. Uiprasertkul, K. Boonnak, C. Pittayawonganon, N. J. Cox, S. R. Zaki, P. Thawatsupha, M. Chittaganpitch, R. Khontong, J. M. Simmerman, and S. Chunsutthiwat. 2005. Probable person-to-person transmission of avian influenza A (H5N1). N. Engl. J. Med. 352:333-340. [DOI] [PubMed] [Google Scholar]
- 38.van Riel, D., V. J. Munster, E. de Wit, G. F. Rimmelzwaan, R. A. Fouchier, A. D. Osterhaus, and T. Kuiken. 2006. H5N1 virus attachment to lower respiratory tract. Science 312:399. [DOI] [PubMed] [Google Scholar]
- 39.Webby, R., E. Hoffmann, and R. Webster. 2004. Molecular constraints to interspecies transmission of viral pathogens. Nat. Med. 10:S77-S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization Epidemic and Pandemic Alert and Response (EPR). 2006. Confirmed human cases of avian influenza A (H5N1). World Health Organization. http://www.who.int/csr/disease/avian_influenza/country/en/.
- 41.World Health Organization Global Influenza Program Surveillance Network. 2005. Evolution of H5N1 avian influenza viruses in Asia. Emerg. Infect. Dis. 11:1515-1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.The Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5. 2005. Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 353:1374-1385. [DOI] [PubMed] [Google Scholar]
- 43.Yamada, S., Y. Suzuki, T. Suzuki, M. Q. Le, C. A. Nidom, Y. Sakai-Tagawa, Y. Muramoto, M. Ito, M. Kiso, T. Horimoto, K. Shinya, T. Sawada, M. Kiso, T. Usui, T. Murata, Y. Lin, A. Hay, L. F. Haire, D. J. Stevens, R. J. Russell, S. J. Gamblin, J. J. Skehel, and Y. Kawaoka. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444:378-382. [DOI] [PubMed] [Google Scholar]
- 44.Yen, H. L., L. M. Herlocher, E. Hoffmann, M. N. Matrosovich, A. S. Monto, R. G. Webster, and E. A. Govorkova. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yingst, S. L., M. D. Saad, and S. A. Felt. 2006. Qinghai-like H5N1 from domestic cats, northern Iraq. Emerg. Infect. Dis. 12:1295-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]