Abstract
The filoviruses Ebola virus (EBOV) and Marburg virus (MARV) are responsible for devastating hemorrhagic fever outbreaks. No therapies are available against these viruses. An understanding of filoviral glycoprotein 1 (GP1) residues involved in entry events would facilitate the development of antivirals. Towards this end, we performed alanine scanning mutagenesis on selected residues in the amino terminus of GP1. Mutant GPs were evaluated for their incorporation onto feline immunodeficiency virus (FIV) particles, transduction efficiency, receptor binding, and ability to be cleaved by cathepsins L and B. FIV virions bearing 39 out of 63 mutant glycoproteins transduced cells efficiently, whereas virions bearing the other 24 had reduced levels of transduction. Virions pseudotyped with 23 of the poorly transducing GPs were characterized for their block in entry. Ten mutant GPs were very poorly incorporated onto viral particles. Nine additional mutant GPs (G87A/F88A, K114A/K115A, K140A, G143A, P146A/C147A, F153A/H154A, F159A, F160A, and Y162A) competed poorly with wild-type GP for binding to permissive cells. Four of these nine mutants (P146A/C147A, F153A/H154A, F159A, and F160A) were also inefficiently cleaved by cathepsins. An additional four mutant GPs (K84A, R134A, D150A, and E305/E306A) that were partially defective in transduction were found to compete effectively for receptor binding and were readily cleaved by cathepsins. This finding suggested that this latter group of mutants might be defective at a postbinding, cathepsin cleavage-independent step. In total, our study confirms the role of some GP1 residues in EBOV entry that had previously been recognized and identifies for the first time other residues that are important for productive entry.
Ebola virus (EBOV) and Marburg virus (MARV) cause severe hemorrhagic fevers that have high mortality rates. The viruses infect a variety of cell types, including alveolar macrophages, dendritic cells, and endothelial cells (32). The cellular receptor(s) has yet to be firmly established, but several cellular proteins have been implicated in filoviral entry. Folate receptor-α was initially reported to be a receptor for the filoviruses (4), but it has since been shown that cells that do not express the folate receptor are permissive for entry (25, 26). Lectin molecules, including DC-SIGN, mannose binding lectin (MBL), and human macrophage galactose- and N-acetylgalactosamine-specific C-type lectin (hMGL), have been shown to enhance EBOV entry, but they are not essential (1, 3, 11, 14, 17, 24, 28). Integrin β1 has been postulated to facilitate entry (29), and, most recently, members of the Tyro3 protein kinase family of proteins (23) have been demonstrated to play to role in mediating filovirus uptake.
EBOV and MARV are both members of the Filoviridae family and have been classified as separate genera due to a lack of serological cross-reactivity and genetic differences. Consistent with the taxonomic separation of the viruses, MARV and EBOV outbreaks have distinct geographical distributions in Africa (19). Both viruses have a broad tropism with similar or perhaps identical infectivity patterns across cell populations and species (32). This observation suggests that the filoviral glycoproteins (GP) utilize the same or similar receptor(s) for entry. Consistent with this, two recent studies demonstrated that the soluble receptor binding domain (RBD) from MARV GP1 can compete for binding to permissive cells with EBOV GP1 and, conversely, EBOV GP1 RBD competes with MARV binding (13, 16). However, the EBOV and MARV GP1s are only distantly related, containing 28% identity and 48% similarity within the most highly conserved amino-terminal residues of GP1. Despite the limited sequence identity, sequence alignments highlight small stretches of identical residues within the RBD of GP1.
The three-dimensional structure for the filoviral glycoproteins GP1 and GP2 on the surface of an infected cell or virion has not been determined. Previous studies have demonstrated that filoviral GPs are type 1 viral glycoproteins, and work has begun to identify important functional domains of both proteins (9, 10, 13, 15, 16, 18). The EBOV glycoprotein is produced as a single polypeptide that is cleaved by the cellular protease furin into GP1 and GP2, although the cleavage is not required for infectivity (8, 21, 30, 33). The two subunits are linked by a disulfide bond (10). The GP1 subunit is analogous to the HA1 subunit of influenza virus or the SU subunit of retroviral envelopes and is responsible for receptor binding. The GP2 subunit anchors the glycoprotein into the viral membrane and contains both a fusion peptide and a coiled-coil domain that bring about the fusion of the viral and cellular membranes. Among the various strains of EBOV, the first 300 residues of the GP1 subunit are highly conserved, but the remaining residues in GP1 are variable. The C-terminal, variable region of GP1 contains several O-linked glycosylation sites and has been termed the mucin domain (10, 34). The mucin domain can be deleted from the protein, and the glycoprotein remains functional and viral titers increase, indicating that the RBD is present in the amino-terminal 300 residues (10, 34). More recent studies have further mapped the RBD to residues 54 to 201 in GP1 (13).
Studies have identified important postbinding steps in the entry pathway of EBOV (5, 22). The EBOV enters cells through a low-pH-dependent mechanism involving the cellular endosomal compartment (7, 25). Low pH activates the cellular cathepsin B and L proteases that cleave GP1 and thereby presumably facilitate GP2 interactions with cellular membranes (5, 22). Additional, poorly defined, noncathepsin, low-pH events are postulated to be required for productive entry (2, 22).
Our study complements and expands previous EBOV GP1 mapping studies. We identify additional residues in EBOV GP1 that impact receptor recognition as well as identify residues within GP1 that are required for postbinding events.
MATERIALS AND METHODS
Cell lines and antibodies.
Human embryonic kidney cells 293T (6) and a human glioblastoma line, SNB-19 (NCI 0502596), were maintained in high-glucose Dulbecco's modified Eagle's medium (DMEM) supplemented with penicillin and streptomycin. Medium was supplemented with 10% fetal calf serum. A rabbit polyclonal anti-EBOV (Zaire) GP1 (ZEBOV) antibody was used in these studies (10).
Plasmids.
The second-generation feline immunodeficiency virus (FIV) vector system utilized in this study was reported previously (12, 31). All glycoproteins were expressed from the cytomegalovirus (CMV) immediate-early promoter present in pcDNA3.1 (Invitrogen, Carlsbad, CA)-derived plasmids. The parental plasmid containing the ZEBOV GP gene (EbolaΔO) with a deleted GP1 mucin domain (pEZGPΔ309-489) has been described previously (10, 26) and was used throughout these studies, because viral titers are higher with the mucin domain deletion construct (10). The FIV gag-pol protein products were expressed from the CMV promoter in the plasmid pFIVΔΔ as previously described (26). The packaged genomes expressing either β-galactosidase (β-gal) or luciferase were called pFIVψβ-gal or pFIVψluciferase, respectively, and have also been previously described (26). All protein expression was driven by the CMV immediate-early promoter, except the luciferase-expressing construct, which was driven by the Rous sarcoma virus long terminal repeat.
PCR mutagenesis of ZEBOV GP1.
Alanine substitution mutations were produced using the Stratagene QuikChange mutagenesis kit according to the manufacturer's protocols. The site-directed mutations were confirmed by sequencing the length of the GP gene.
Generation of pseudotyped FIV particles.
Pseudotyped FIV particles were produced as previously described (26). 293T cells were transfected with a total of 75 μg of DNA consisting of a pEbolaΔO-expressing construct, a pFIVΔΔ construct that expresses gag-pol, and pFIVψ-β-gal or pFIVψluciferase at a ratio of 1:2:3, respectively. The DNA was transfected into 15-cm-diameter dishes of 293T cells using calcium-phosphate transfection (12). Supernatants were collected at 24, 36, 48, 60, and 72 h posttransfection and frozen at −80°C. The supernatants were thawed, filtered through a 0.45-μm-pore-size filter, and pelleted by a 16-h centrifugation step (7,000 rpm at 4°C in a Sorvall GSA rotor). The viral pellet was resuspended in 250 μl DMEM for an approximately 200-fold concentration. A reverse transcriptase (RT) assay was performed, viral input was normalized to RT activity (20), and the virus was either used immediately for infection or stored at −80°C until use.
Immunoblotting.
Equivalent RT units of viral particles were analyzed on a sodium dodecyl sulfate-4 to 20% polyacrylamide gel electrophoresis (SDS-PAGE) gel and transferred to nitrocellulose. The membranes were incubated with rabbit anti-ZEBOV GP polyclonal sera (10) (1:7,500) for 3 h and then incubated with peroxidase-conjugated goat anti-rabbit antiserum (1:20,000) (Sigma) for 1 h. The membranes were visualized by the chemiluminescence method according to the manufacturer's instructions (Pierce).
Transduction assay.
SNB-19 cells were seeded into 48-well plates (2.5 × 104 cells/well). Duplicate wells were transduced 24 h later with equivalent amounts of pseudotyped particles as determined by virion RT activity. Four days after transduction, the cells were fixed in 3.7% formalin and stained with 5-bromo-4-chloro-3-indolyl-â-d-galactopyranoside (X-Gal) for β-gal activity. The number of blue cells was recorded for each pseudotyped virus. Experimental results are shown as the number of cells transduced by virions containing the mutant glycoproteins divided by the number of cells transduced by virions containing the wild-type EbolaΔO in the same experiment. These values were multiplied by 100 to obtain percent control values. All studies were repeated in at least three independent experiments.
Binding competition assay.
SNB-19 cells were seeded into 48-well plates (2.5 × 104 cells/well). The following day, cells were incubated at 4°C for 30 min with equal quantities of wild-type or mutant GP-pseudotyped FIV particles containing a luciferase expression construct. These viral particles were normalized for RT activity. The quantity of luciferase-containing particles that were preincubated with monolayer was in greater than 1,000× excess of the β-gal reporter virion that was subsequently added. After the 30-min preincubation, wild-type EbolaΔO-pseudotyped FIV/β-gal particles were added to the cells at an approximate multiplicity of infection of 0.004. Plates were shifted to 37°C, and medium was replaced 24 h following transduction and maintained for 4 days. Cells were fixed and stained with X-Gal, and blue cells were counted. Results are shown as the ability of mutant glycoprotein-containing virions to compete for receptors on permissive cells divided by the ability of wild-type EbolaΔO-pseudotyped virions to compete. These values were multiplied by 100 to obtain percentages of the control values (EbolaΔO = 100%).
catL proteolysis assay.
FIV particles containing the mutant glycoproteins were produced and concentrated as described above. Pelleted viral particles were suspended in 100 μl acetate buffer (100 mM sodium acetate, pH 5.5, 1 mM EDTA, and 5 mM dithiothreitol) as described previously (5). Equivalent volumes of mutant GP1 protein, as determined by immunoblotting, were incubated with 0.5 mU of cathepsin L (Sigma) at 37°C for 1.5 h. Reactions were stopped with the addition of Sigma's protease cocktail (P-8340) and shifted to 4°C. The samples were visualized by separation on an SDS-16% PAGE gel and either silver stained directly with Invitrogen's SilverQuest per the manufacturer's instructions or transferred to a nitrocellulose membrane, followed by immunoblotting for GP1 to detect cathepsin L (catL) cleavage.
Statistical analysis.
Statistical analyses were conducted by Student's t test, utilizing the two-tailed distribution and two-sample equal-variance conditions. A significant difference was determined by a P value of <0.05.
RESULTS
Efficiency of GP1 incorporation onto virions.
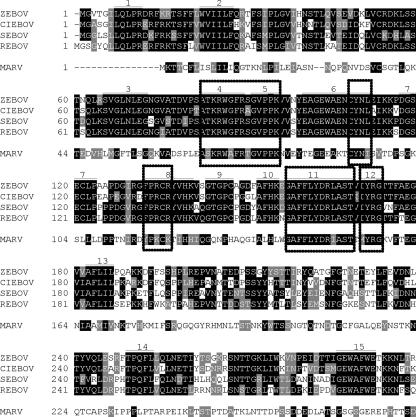
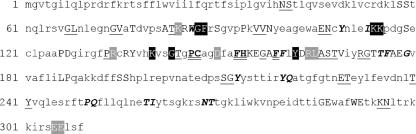
Recent recognition that the EBOV and MARV GPs compete with one another for entry suggested that the residues that comprise the receptor binding site (RBS) within the RBD of the two glycoproteins may be conserved. To identify potentially important residues to target for mutagenesis, sequence comparisons of representative glycoproteins from EBOV and MARV outbreaks were performed. The alignment of the GP1s from four different strains revealed 15 completely conserved regions, at least four residues long, among the EBOV strains investigated. These conserved regions are numbered in Fig. 1. When a MARV GP1 sequence was included in the analysis, five regions containing four or more identical or similar contiguous residues are present. These five regions are boxed in Fig. 1. These five regions were the primary focus in these mutagenesis studies, and we targeted two-thirds of these residues for mutagenesis. All mutated residues were changed to alanines except if the wild-type residue was an alanine, in which case the residue was mutated to a serine. In addition to these conserved regions, other basic, acidic, or bulky side chain residues were mutated to alanine either alone or in pairs along the RBD. The mutants were evaluated for their impact on transduction and early steps in entry.
FIG. 1.
Alignment of EBOV and MARV GP1 proteins. A ClustalW alignment of the amino-terminal 300 amino acids of four strains of EBOV and one strain of MARV identified conserved regions. The residues highlighted in black are identical, and those in gray are similar. Fifteen regions that are numbered are found to be identical in all EBOV strains. The regions similar between all EBOV strains and MARV are boxed. ZEBOV, Zaire EBOV; CIEBOV, Cote D'Ivoire EBOV; SEBOV, Sudan EBOV; REBOV, Reston EBOV.
Using a mucin domain deletion EBOV GP construct (10), a total of 63 EBOV GP RBD mutations were studied. Initial studies utilized immunoblots to evaluate the incorporation of the mutant GPs onto pseudotyped FIV virions (Table 1). The immunoblot analysis indicated that 46 of the 63 mutant GP1s were incorporated into virions at levels that were roughly equivalent to the incorporation of wild-type GP1 (>50 to ∼100% of the wild-type level). Seven other mutants consistently had approximately 50% of wild-type levels of GP1 incorporation into virions, and one mutant (F160A) had about 10 to 25% of wild-type levels. Nine mutations resulted in little (<10% of wild-type levels) or no detectable GP1 incorporated into virions. GP1 levels present in cell lysates from transfected 293T producer cells were consistent with the levels of GP1 incorporated in virions (data not shown). Presumably the nine mutations that displayed less than 10% of wild-type levels of GP1 decreased the stability of the GP1 protein, perhaps by altering GP conformation. Consistent with the reduced levels of GP1 incorporation into virions, these nine GP mutants supported little particle transduction (0 to 33%) of the permissive SNB-19 cell line. Five of the nine within this latter group of mutants contained mutations that were located between residues 214 and 270, providing evidence that this region of GP1 may play a role in protein stability.
TABLE 1.
Characteristics of GP1 mutant pseudotyped FIV particles
| Mutation(s) | GP1 incorporationa | Transduction efficiency (%)b |
|---|---|---|
| N40A/S41A | +++ | 171.8 ± 43.9 |
| S58A/S59A | +++ | 80.9 ± 9.7 |
| G67A/L68A | +++ | 192.6 ± 30.3 |
| G74A/V75A | +++ | 359.9 ± 51.3 |
| T77A | +++ | 129.7 ± 12.3 |
| A82S | +++ | 134.3 ± 9.0 |
| T83A | +++ | 183.7 ± 20.4 |
| K84A | ++ | 55.4 ± 4.9 |
| R85A | ++ | 147.6 ± 24.2 |
| W86A | +/− | 0 ± 0 |
| G87A/F88A | +++ | 0 ± 0 |
| S90A | +++ | 142.1 ± 2.5 |
| P94A | +++ | 97.1 ± 14.5 |
| V96A/V97A | +++ | 383.3 ± 16.9 |
| V97A | +++ | 160.6 ± 20.6 |
| N98A | +++ | 96.9 ± 6.5 |
| E106A/N107A | +++ | 181.5 ± 16.3 |
| Y109A/I113T | +/− | 0.4 ± 0.4 |
| K114A/K115A | +++ | 2.1 ± 0.6 |
| S119A | +++ | 63.6 ± 12.8 |
| P126A/D127A | +++ | 100.6 ± 41 |
| P133A | +++ | 280.0 ± 32.4 |
| R134A | +++ | 65 ± 24 |
| R136A/Y137A | +++ | 144.6 ± 46.3 |
| K140A | +++ | 25.1 ± 12.8 |
| G143A | +++ | 1 ± 0.2 |
| T144A | +++ | 182.4 ± 46.7 |
| P146A/C147A | +++ | 0.2 ± 0.2 |
| D150A | +++ | 67.9 ± 12.4 |
| F153A/H154A | +++ | 0 ± 0 |
| K155A | +++ | 109.4 ± 12.5 |
| E156A | +++ | 94.0 ± 9.7 |
| G157A | +++ | 157.8 ± 10.7 |
| A158S | +++ | 141.0 ± 12.9 |
| F159A | ++ | 0 ± 0 |
| F160A | + | 26.6 ± 13 |
| Y162A | ++ | 44.3 ± 12.7 |
| D163A | +++ | 98.2 ± 14.0 |
| R164A/L165A | ++ | 52.2 ± 24.4 |
| A166S | +++ | 163.9 ± 12.1 |
| S167F/R172A | +++ | 171.1 ± 26.5 |
| T168A | +++ | 218.4 ± 7.1 |
| V169A | +++ | 149.3 ± 12.3 |
| G173A | +++ | 199.3 ± 13.3 |
| T174A | +++ | 134.7 ± 24.6 |
| T175A/F176A | +/− | 0.5 ± 0.3 |
| A177S | +++ | 99.1 ± 6.9 |
| E178A | +++ | 139.7 ± 22.1 |
| G179A | +/− | 7.5 ± 4.4 |
| L186A/P187A | +++ | 138.6 ± 14.5 |
| S196A/S197A | ++ | 104.7 ± 26.8 |
| S212A/G213A | +++ | 159.2 ± 71.4 |
| Y214A | +/− | 0.1 ± 0.1 |
| Y221A/Q222A | +/− | 1.7 ± 1.1 |
| E230A/T231A | +++ | 170.8 ± 38.9 |
| T240A/Y241A | +++ | 232.1 ± 33.8 |
| P251A/Q252A | +/− | 1.3 ± 0.6 |
| T260A/I261A | +/− | 32.6 ± 12.9 |
| N269A/T270A | +/− | 24.7 ± 7.8 |
| G287A/E288A | +++ | 147.8 ± 13.3 |
| W292A/E293A | +++ | 115.9 ± 19 |
| K296A/N297A | +++ | 155.4 ± 20.8 |
| E305A/E306A | ++ | 37.8 ± 0.7 |
Mutant GP1s were examined for incorporation into virion particles by immunoblotting and were compared to the wild type. +++, ≥80% of wild type; ++, ≥50% of wild type; +, ≥25% of wild type; +/−, <25% of wild type.
Transduction efficiency was determined on permissive SNB-19 cells with virion input normalized for RT activity.
Transduction efficiency of GP1 mutants.
We examined the transduction efficiency of mutant GP-pseudotyped FIV particles that delivered a β-gal reporter gene into permissive SNB-19 cells (Table 1). The transduction ability of the mutant GP1-pseudotyped virions is reported as the percentage of transduction of the mutant divided by the transduction of the parental EbolaΔO GP-pseudotyped virions. Thirty-nine of the 63 mutation-containing virions transduced to 68% of wild-type values or greater. Interestingly, 18 of these mutant GP-pseudotyped virions were highly efficient at transduction, with 150% or greater values than the wild-type EbolaΔO GP-containing virions. For instance, mutant V96A/V97A GP-pseudotyped virions consistently transduced almost fourfold better than wild-type particles. The enhanced transduction of these mutant GP-pseudotyped virions suggested that the GP mutations might result in increased binding to the receptor and/or greater efficiency of early entry events, since significantly greater quantities of these mutant GP1s in viral particles were not evident in immunoblots (data not shown).
Fourteen of the mutants that had moderate to high levels of GP present on virions were found to transduce inefficiently, having 0 to 68% of wild-type levels of transduction of two permissive cell lines, SNB-19 and Vero cells. These mutants were K84A, G87A/F88A, K114A/K115A, R134A, K140A, G143A, P146A/C147A, D150A, F153A/H154A, F159A, F160A, Y162A, R164A/L165A, and E305A/E306A. Interestingly, some but not all of these mutants were located in the conserved regions of GP1 identified in Fig. 1. Many of the residues that were important for EBOV GP-dependent transduction (K114A/K115A, R134A, K140A, P146A/C147A, D150A, and F153A/H154A) were not conserved between EBOV and MARV. Mutagenesis of a number of residues within the conserved regions had no negative impact on transduction. For instance, alanine substitution of the residue T83, S90, G157, G173, or T174 slightly enhanced transduction efficiency.
Identification of residues within GP1 that reduce particle binding to cells.
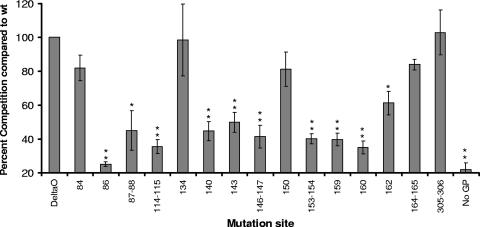
Fourteen GP mutants with poor virion-associated transduction efficiencies (0 to 68% of the wild-type level) but had at least 25% of wild-type levels of virion-associated GP1 were examined in binding competition assays using permissive SNB-19 cells. Virions containing a luciferase reporter gene were normalized for RT activity and preincubated with cells. The cells were subsequently infected with wild-type EbolaΔO-pseudotyped FIVψβ-gal. The transductions were fixed and stained for β-gal expression 4 days after transduction. The competition studies are shown in Fig. 2. Wild-type EbolaΔO GP1 and W86A GP that produced no detectable levels of virion-associated GP and did not mediate transduction were also included in the binding study as well as virions not containing any GP. The ability of the mutant GP1-pseudotyped virions to compete for binding are shown as percentages of the level of competition of wild-type EbolaΔO/FIVψ luciferase. K84A, R134A, D150A, R164A/L165A, and E305A/E306A were statistically indistinguishable from wild-type EbolaΔO in their ability to compete for binding. The observation that these mutants retained the ability to bind to the receptor suggested that their reduced transduction efficiency resulted from postbinding entry defects. G87A/F88A, K114A/K115A, K140A, G143A, P146A/C147A, and F153A/H154A produced near wild-type levels of glycoprotein on particles but had reduced ability to compete for binding, suggesting these mutations play a role in receptor binding. F159A, F160A, and F162 also demonstrated poor binding competition but had somewhat reduced GP incorporation onto virions. To explore this region further, a leucine-for-phenylalanine substitution of residue 159 (F159L) was generated. This mutant transduced to wild-type levels, indicating that phenylalanine at position 159 is not absolutely required for entry (data not shown).
FIG. 2.
Ability of FIV virions pseudotyped with EbolaΔO GP1 mutant glycoproteins to compete with wild-type EbolaΔO-GP1-pseudotyped virus for binding to permissive cells. Mutant and wild-type (wt) EbolaΔO-pseudotyped FIV particles containing a luciferase reporter gene were normalized for RT activity, and equivalent numbers of particles were incubated with SNB-19 cells. The cells were subsequently challenged with EbolaΔO GP-pseudotyped FIV β-gal (multiplicity of infection, 0.004). β-gal expression was determined 4 days after transduction. The data are represented as percentages of the wild-type competition. Data represent the averages and standard errors from three experiments performed in duplicate. Significant differences between the ability of wild-type and mutant GPs to compete for binding was determined by Student's t test. *, P < 0.05; **, P < 0.001.
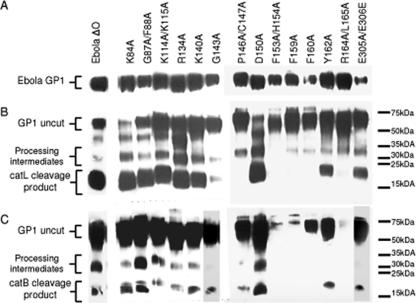
Identification of residues that alter cathepsin cleavage.
Although recent studies demonstrated that EBOV GP-pseudotyped particle entry is dependent on cathepsin cleavage of GP1, residues that affect cleavage by the enzyme have not been identified (5, 22). To determine if some of the mutant GP1s that were poor transducers were cathepsin insensitive and therefore were unable to efficiently mediate entry of virions, catL or cathepsin B (catB) proteolysis of virion-associated GP1 proteins was performed. Wild-type GP1 and the 14 mutants used in the binding competition assays were pseudotyped onto particles, concentrated, and resuspended in a low-pH acetate buffer. The quantity of GP1 present in the concentrated samples varied between mutants, since virion association of mutant GPs varied. Thus, GP1 immunoblots were used to normalize the quantity of GP used in the cathepsin assays (Fig. 3A), and equivalent quantities of particle-associated GP1s were incubated with catL (Fig. 3B) or catB (Fig. 3C). Cathepsin L cleavage studies that are shown were performed at pH 5.5; however, similar cleavage results were obtained at the lower pH of 4.5 (data not shown). Cleavage of wild-type GP1 by catL and catB produced the predicted 18- to 22-kDa protein, as did cleavage of K84A, G87A/F88A, K114A/K115A, R134A, K140A, and D150A. Y162A and E305A/E306A were cleaved by catL and catB but not as efficiently as the others. Limited amounts of the catL cleavage product of G143A were evident, and overexposure of the blot was required to see the catB cleavage product for both G143A and E305A/E306A.
FIG. 3.
Cathepsin L and B proteolysis of mutant EBOV GP1s. The mutant particles were normalized for GP1 content (A) and then cleaved with catL (B) or catB (C). The digested particles were separated by SDS-PAGE and immunoblotted for GP1. The blot is a representative blot from three experiments. Overexposure of the gel was required to see the catB cleavage product for G143A and E305A/E306A. Overexposure of lanes containing P146A/C147A, F153A/H154A, F159A, F160A, and R164/L165A did not result in detectable cleavage products.
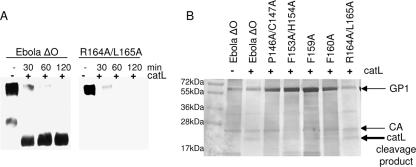
There were no 18- to 22-kDa cleavage products following catL treatment of the P146A/C147A, F153A/H154A, F159A, F160A, and R164A/L165A mutants, even upon overexposure of the membrane. P146A/C147A did show a low level of cleavage by catB. Four of the five mutants that were not cleaved by catL also showed a decreased ability to compete for wild-type GP1 binding (P146A/C147A, F153A/H154A, F159A, and F160A). Because R164A/L165A did compete for entry, we examined the ability of catL to cleave R164A/L165A more thoroughly. A time course experiment cleaving both wild-type GP and R164A/L165A showed a loss of the full-length glycoprotein over time. Concomitantly, an 18- to 22-kDa band became evident with wild-type GP. However, no cleavage product was observed with R164A/L165A (Fig. 4A). To determine if the catL cleavage product of R164A/L165A was present but simply not detected with our polyclonal antisera, we performed catL cleavage assays with those mutants that showed no catL cleavage product and then silver stained the gel (Fig. 4B). The silver stain gel showed a catL cleavage product with wild-type GP and R164A/L165A, but three- to fivefold greater quantities of P146A/C147A, F153A/H154A, F159A, or F160A GP-pseudotyped virions did not yield an apparent catL cleavage product. This finding indicates that the R164A/L165A GP mutant is cut by cathepsin and that residues R164/L165 are important for the detection of the cathepsin cleavage product with our polyclonal anti-EBOV-GP1 serum. In contrast, P146A/C147A, F153A/H154A, F159A, and F160A GPs were cleaved very poorly by cathepsins. The observations that these residues impacted both receptor binding and cathepsin cleavage suggest that mutations in these residues result in significant GP conformational changes.
FIG. 4.
R164A/L165A constitutes an immunodominant epitope of the 18- to 22-kDa cleavage product. Cleavage of wild-type EBOV and R164A/L165A by catL was examined over time (A). Silver-stained SDS-PAGE of catL cleavage products (B). Bands corresponding to uncut GP1, FIV capsid protein (CA), and the catL cleavage products are identified, and molecular size markers are shown.
K84A, R134A, D150A, and E305A/E306A competed for receptor binding almost as well as wild-type GP1, displayed the 18- to 22-kDa catL cleavage product, and yet transduced cells at less than 68% of wild-type levels. Schornberg et al. have previously suggested that additional low-pH-dependent entry steps that are cathepsin independent may be important for EBOV entry (22). These four mutations may be defective in the ill-defined postbinding, cathepsin-independent steps. However, it should be noted that these mutants are all able to support at least modest levels of transduction. Thus, if these mutants are deficient in the latter step, this event must not be absolutely required for entry or the mutations did not completely abrogate the step.
DISCUSSION
Here we identified a number of residues within the RBD of the EBOV GP1 protein that impact virus entry and begin to identify which step within the entry process is affected by each mutant. Our GP1 mutants that showed transduction defects fell into four categories: (i) mutations that transduced poorly due to low protein incorporation on virions, (ii) mutations that competed poorly for receptor binding, (iii) mutations that altered conformation, and (iv) mutations that resulted in low transduction but effectively competed for receptor binding and were cleaved by cathepsins, suggesting that they manifested a defect at a postbinding, cathepsin-independent entry step (Fig. 5; Table 2).
FIG. 5.
Summary of mutant phenotypes. Mutants were classified after examining GP1 incorporation, transduction efficiency, binding competition, and cathepsin cleavage assays. Residues in black capital letters transduced cells at wild-type levels (65% to 150% of wild type), those that did not incorporate GP1 well are in boldface italics; residues that are involved with receptor binding are highlighted in black; residues that are involved in GP1 conformation are double underlined; residues that are involved in a postbinding, cathepsin cleavage-independent step are highlighted in gray; and residues that transduced more than 150% of the wild type are underlined once.
TABLE 2.
Summary of the biological activities altered by mutations in EBOV GP1
| Mutation(s) | GP1 incorporation | Transduction efficiency | Competition efficiency | Cathepsin cleavage | Biological classificationb |
|---|---|---|---|---|---|
| ΔO | +++ | 100 | 100 | +++ | Wild type |
| K84A | ++ | 55.4 | 82.0 | +++ | IV |
| W86A | +/− | 0 | 25.2 | NAa | I |
| G87A/F88A | +++ | 0 | 45.0 | +++ | II |
| Y109A/I113T | +/− | 0.4 | NA | NA | I |
| K114A/K115A | +++ | 2.1 | 35.5 | +++ | II |
| R134A | +++ | 65 | 98.4 | +++ | IV |
| K140A | +++ | 25.1 | 44.7 | +++ | II |
| G143A | +++ | 1 | 50.0 | + | II |
| P146A/C147A | +++ | 0.2 | 41.5 | +/− | III |
| D150A | +++ | 67.9 | 81.2 | +++ | IV |
| F153A/H154A | +++ | 0 | 40.2 | +/− | III |
| F159A | ++ | 0 | 39.8 | +/− | III |
| F160A | + | 26.6 | 35.0 | +/− | I |
| Y162A | ++ | 44.3 | 61.3 | ++ | II |
| R164A/L165A | ++ | 52.2 | 84.0 | +++ | IV |
| T175A/F176A | +/− | 0.5 | NA | NA | I |
| G179A | +/− | 7.5 | NA | NA | I |
| Y214A | +/− | 0.1 | NA | NA | I |
| Y221A/Q222A | +/− | 1.7 | NA | NA | I |
| P251A/Q252A | +/− | 1.3 | NA | NA | I |
| T260A/I261A | +/− | 32.6 | NA | NA | I |
| N269A/T270A | +/− | 24.7 | NA | NA | I |
| E305A/E306A | ++ | 37.8 | 102.9 | ++ | IV |
NA, not applicable.
Mutants were classified by their defect in GP1 incorporation (I), receptor binding (II), conformational defect (III), or postbinding, postcleavage entry steps (IV).
Our study has allowed recognition of novel functional domains within EBOV GP1. We identify residues G87/F88, K114/K115, K140, G143, and Y162 as important for receptor binding. Previously, EBOV GP transduction studies purported that F88 is important in receptor binding (15, 18). Despite our hypothesis that residues that are important for binding will be completely conserved across the filovirus family, we implicated several residues in receptor binding that were not conserved in MARV. Furthermore, some of these binding mutants occur between residues 114 and 143, a region not previously implicated in receptor binding (15). K114A/K115A, K140A, and G143A, mutants within the 114 to 143 region, had low transduction levels and demonstrated a decreased ability to bind to permissive cells, potentially implicating this region as part of the RBS.
Some more carboxy-terminal mutations between residues 146 and 159 not only poorly competed for binding but also were not cleaved by catL (P146A/C147A, F153A/H154A, F159A, and F160A). The inability of this group of mutants to bind to permissive cells and undergo catL proteolysis suggested the possibility that the mutations result in conformational changes that reduce both receptor binding and cathepsin recognition, ultimately leading to poor transduction. This conclusion is consistent with findings reported by Manicassamy et al. (15) and stand in contrast to a report by Mpanju et al. (18).
Finally, we identified five mutants (K84A, R134A, D150A, R164A/L165A, and E305A/E306A) that, when virion associated, had reduced transduction but effectively competed for receptor binding and were proteolytically cleaved by cathepsins. Recent studies have proposed that low-pH-dependent events in addition to cathepsin cleavage are needed for productive entry of EBOV GP-pseudotyped virions (2, 22). These five mutants may be defective in this downstream event. Further studies with these mutants will be needed to definitively characterize their entry defect(s). R134 has previously been implicated in a neutralizing epitope on the glycoprotein (27). An R134Q change allowed escape from a neutralizing antibody, suggesting that the residue is close to the RBS and/or aids in its conformation. Our study identified R134 as a residue not involved directly in receptor binding but as important for viral entry. R164A/L165A appeared to compose an important epitope in our polyclonal rabbit anti-GP1 antisera. This dominant epitope is needed to detect the 18- to 22-kDa cathepsin cleavage product that has been shown to be necessary for receptor binding (5).
Along with the various mutations that inhibited transduction, a number of mutants showed an increase in transduction efficiency above wild-type levels. Many of the mutations that increased transduction were found in highly conserved regions between all strains of EBOV and MARV. These mutations may have implications for gene therapy if they can more efficiently deliver targeted gene products. Although further analysis of the mutants has yet to be performed, these mutations may be selected against during an in vivo infection. For instance, these changes in the protein's structure that enhance binding to the receptor on human cells may not be optimal for entry into cells of the natural reservoir. Alternatively, these regions may have immunologically based constraints that prevent mutations from occurring in these regions.
Kuhn et al. investigated regions in the EBOV GP1 that are important for virion binding. They produced soluble GP1-Fc fusion protein constructs with N- and C-terminal truncations to determine the smallest region that can compete for transduction (13). They narrowed the RBD to residues 54 through 201 (13). This region of the EBOV GP1 protein competed for entry of both EBOV- and MARV-pseudotyped lentiviral vectors, suggesting that the domain binds to a receptor common to both viruses. Our data are consistent with the truncation study, since all residues important for binding were located between residues 87 and 162.
Manicassamy et al. performed site-directed mutagenesis analysis on EBOV GPΔO (15). In their transduction study, they classified the region between residues 57 and 64 as well as residues F88, K95, and I170 as part of the RBD. Our study also demonstrated the importance of F88 for wild-type binding to permissive cells. More recently, Mpanju et al. performed limited mutagenesis of EBOV GP1 and also found F88 and F159 to be important for EBOV glycoprotein-dependent entry (18).
There are several potential vaccine approaches that appear to protect laboratory animals from fatal doses of EBOV and MARV, but the vaccines require inoculation either preexposure or soon after exposure. Currently there is no treatment to stop the spread of the virus once infected. Defining interactions between the viral glycoprotein and the cellular receptor may allow for drug development that could limit viral spread in the infected individual and reduce infection during an outbreak. In total, the recent mutagenesis analysis of EBOV GP1 begins to elucidate the structure and functional domains of filoviral GP1.
Acknowledgments
This work was supported by NIH R21 AI064526 (W.M.) and NIH R01 HL075363 (P.B.M.). M.A.B. was supported through the Training in Molecular Virology T32 A1007533 grant from the NIAID.
We thank Patrick Sinn for helpful comments on the manuscript.
Footnotes
Published ahead of print on 2 May 2007.
REFERENCES
- 1.Alvarez, C. P., F. Lasala, J. Carrillo, O. Muniz, A. L. Corbi, and R. Delgado. 2002. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J. Virol. 76:6841-6844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bar, S., A. Takada, Y. Kawaoka, and M. Alizon. 2006. Detection of cell-cell fusion mediated by Ebola virus glycoproteins. J. Virol. 80:2815-2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baribaud, F., R. W. Doms, and S. Pohlmann. 2002. The role of DC-SIGN and DC-SIGNR in HIV and Ebola virus infection: can potential therapeutics block virus transmission and dissemination? Expert Opin. Ther. Targets 6:423-431. [DOI] [PubMed] [Google Scholar]
- 4.Chan, S. Y., C. J. Empig, F. J. Welte, R. F. Speck, A. Schmaljohn, J. F. Kreisberg, and M. A. Goldsmith. 2001. Folate receptor-alpha is a cofactor for cellular entry by Marburg and Ebola viruses. Cell 106:117-126. [DOI] [PubMed] [Google Scholar]
- 5.Chandran, K., N. J. Sullivan, U. Felbor, S. P. Whelan, and J. M. Cunningham. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DuBridge, R. B., P. Tang, H. C. Hsia, P. M. Leong, J. H. Miller, and M. P. Calos. 1987. Analysis of mutation in human cells by using an Epstein-Barr virus shuttle system. Mol. Cell. Biol. 7:379-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Empig, C. J., and M. A. Goldsmith. 2002. Association of the caveola vesicular system with cellular entry by filoviruses. J. Virol. 76:5266-5270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldmann, H., V. E. Volchkov, V. A. Volchkova, and H. D. Klenk. 1999. The glycoproteins of Marburg and Ebola virus and their potential roles in pathogenesis. Arch. Virol. Suppl. 15:159-169. [DOI] [PubMed] [Google Scholar]
- 9.Ito, H., S. Watanabe, A. Sanchez, M. A. Whitt, and Y. Kawaoka. 1999. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J. Virol. 73:8907-8912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeffers, S. A., D. A. Sanders, and A. Sanchez. 2002. Covalent modifications of the Ebola virus glycoprotein. J. Virol. 76:12463-12472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ji, X., G. G. Olinger, S. Aris, Y. Chen, H. Gewurz, and G. T. Spear. 2005. Mannose-binding lectin binds to Ebola and Marburg envelope glycoproteins, resulting in blocking of virus interaction with DC-SIGN and complement-mediated virus neutralization. J. Gen. Virol. 86:2535-2542. [DOI] [PubMed] [Google Scholar]
- 12.Johnston, J. C., M. Gasmi, L. E. Lim, J. H. Elder, J. K. Yee, D. J. Jolly, K. P. Campbell, B. L. Davidson, and S. L. Sauter. 1999. Minimum requirements for efficient transduction of dividing and nondividing cells by feline immunodeficiency virus vectors. J. Virol. 73:4991-5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuhn, J. H., S. R. Radoshitzky, A. C. Guth, K. L. Warfield, W. Li, M. J. Vincent, J. S. Towner, S. T. Nichol, S. Bavari, H. Choe, M. J. Aman, and M. Farzan. 2006. Conserved receptor-binding domains of Lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J. Biol. Chem. 281:15951-15958. [DOI] [PubMed] [Google Scholar]
- 14.Lasala, F., E. Arce, J. R. Otero, J. Rojo, and R. Delgado. 2003. Mannosyl glycodendritic structure inhibits DC-SIGN-mediated Ebola virus infection in cis and in trans. Antimicrob. Agents Chemother. 47:3970-3972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manicassamy, B., J. Wang, H. Jiang, and L. Rong. 2005. Comprehensive analysis of Ebola virus GP1 in viral entry. J. Virol. 79:4793-4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manicassamy, B., J. Wang, E. Rumschlag, S. Tymen, V. Volchkova, V. Volchkov, and L. Rong. 2006. Characterization of Marburg virus glycoprotein in viral entry. Virology 358:79-88. [DOI] [PubMed] [Google Scholar]
- 17.Marzi, A., T. Gramberg, G. Simmons, P. Moller, A. J. Rennekamp, M. Krumbiegel, M. Geier, J. Eisemann, N. Turza, B. Saunier, A. Steinkasserer, S. Becker, P. Bates, H. Hofmann, and S. Pohlmann. 2004. DC-SIGN and DC-SIGNR interact with the glycoprotein of Marburg virus and the S protein of severe acute respiratory syndrome coronavirus. J. Virol. 78:12090-12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mpanju, O. M., J. S. Towner, J. E. Dover, S. T. Nichol, and C. A. Wilson. 2006. Identification of two amino acid residues on Ebola virus glycoprotein 1 critical for cell entry. Virus Res. 121:205-214. [DOI] [PubMed] [Google Scholar]
- 19.Peterson, A. T., J. T. Bauer, and J. N. Mills. 2004. Ecologic and geographic distribution of filovirus disease. Emerg. Infect. Dis. 10:40-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reed-Inderbitzin, E., and W. Maury. 2003. Cellular specificity of HIV-1 replication can be controlled by LTR sequences. Virology 314:680-695. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez, A., Z. Y. Yang, L. Xu, G. J. Nabel, T. Crews, and C. J. Peters. 1998. Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J. Virol. 72:6442-6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schornberg, K., S. Matsuyama, K. Kabsch, S. Delos, A. Bouton, and J. White. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J. Virol. 80:4174-4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimojima, M., A. Takada, H. Ebihara, G. Neumann, K. Fujioka, T. Irimura, S. Jones, H. Feldmann, and Y. Kawaoka. 2006. Tyro3 family-mediated cell entry of Ebola and Marburg viruses. J. Virol. 80:10109-10116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simmons, G., J. D. Reeves, C. C. Grogan, L. H. Vandenberghe, F. Baribaud, J. C. Whitbeck, E. Burke, M. J. Buchmeier, E. J. Soilleux, J. L. Riley, R. W. Doms, P. Bates, and S. Pohlmann. 2003. DC-SIGN and DC-SIGNR bind ebola glycoproteins and enhance infection of macrophages and endothelial cells. Virology 305:115-123. [DOI] [PubMed] [Google Scholar]
- 25.Simmons, G., A. J. Rennekamp, N. Chai, L. H. Vandenberghe, J. L. Riley, and P. Bates. 2003. Folate receptor alpha and caveolae are not required for Ebola virus glycoprotein-mediated viral infection. J. Virol. 77:13433-13438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sinn, P. L., M. A. Hickey, P. D. Staber, D. E. Dylla, S. A. Jeffers, B. L. Davidson, D. A. Sanders, and P. B. McCray, Jr. 2003. Lentivirus vectors pseudotyped with filoviral envelope glycoproteins transduce airway epithelia from the apical surface independently of folate receptor alpha. J. Virol. 77:5902-5910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takada, A., H. Feldmann, U. Stroeher, M. Bray, S. Watanabe, H. Ito, M. McGregor, and Y. Kawaoka. 2003. Identification of protective epitopes on Ebola virus glycoprotein at the single amino acid level by using recombinant vesicular stomatitis viruses. J. Virol. 77:1069-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takada, A., K. Fujioka, M. Tsuiji, A. Morikawa, N. Higashi, H. Ebihara, D. Kobasa, H. Feldmann, T. Irimura, and Y. Kawaoka. 2004. Human macrophage C-type lectin specific for galactose and N-acetylgalactosamine promotes filovirus entry. J. Virol. 78:2943-2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takada, A., S. Watanabe, H. Ito, K. Okazaki, H. Kida, and Y. Kawaoka. 2000. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology 278:20-26. [DOI] [PubMed] [Google Scholar]
- 30.Volchkov, V. E., H. Feldmann, V. A. Volchkova, and H. D. Klenk. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 95:5762-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang, G., V. Slepushkin, J. Zabner, S. Keshavjee, J. C. Johnston, S. L. Sauter, D. J. Jolly, T. W. Dubensky, Jr., B. L. Davidson, and P. B. McCray, Jr. 1999. Feline immunodeficiency virus vectors persistently transduce nondividing airway epithelia and correct the cystic fibrosis defect. J. Clin. Investig. 104:R55-R62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wool-Lewis, R. J., and P. Bates. 1998. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J. Virol. 72:3155-3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wool-Lewis, R. J., and P. Bates. 1999. Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J. Virol. 73:1419-1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang, Z. Y., H. J. Duckers, N. J. Sullivan, A. Sanchez, E. G. Nabel, and G. J. Nabel. 2000. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat. Med. 6:886-889. [DOI] [PubMed] [Google Scholar]