Abstract
In this study of 360 low-income mother-child dyads, our primary goal was to disentangle risks linked with commonly co-occurring maternal diagnoses: substance abuse and affective/anxiety disorders. Variable- and person-based analyses suggest that, at least through children’s early adolescence, maternal drug use is no more inimical for them than is maternal depression. A second goal was to illuminate vulnerability and protective processes linked with mothers’ everyday functioning, and results showed that negative parenting behaviors were linked with multiple adverse child outcomes. Conversely, the other parenting dimensions showed more domain specificity; parenting stress was linked with children’s lifetime diagnoses, and limit setting and closeness with children’s externalizing problems and everyday competence, respectively. Results are discussed in terms of implications for resilience theory, interventions, and social policy.
Introduction
In the context of poverty, mothers with substance abuse problems often suffer from depressive or anxiety disorders, and our goal in this paper was to disentangle risks for children stemming from each set of disorders. Using both variable- and person-based analyses, we examined levels of psychopathology and competence among school-age and adolescent children of mothers with (1) cocaine or heroin abuse, (2) depressive or anxiety disorders, (3) both sets of diagnoses, and (4) neither of them. An additional aim was to discern salient vulnerability and protective influences in these high-risk children, focusing on different aspects of mothers’ everyday functioning.
Maternal Drug Abuse and Other Psychopathology: Disentangling Risks to Children
Thousands of American children are believed to be at high risk because of maternal drug abuse: An estimated 7.93 million women in this country (6.5% of the female population) regularly use illicit drugs such as cocaine and opioids (Substance Abuse and Mental Health Services Administration, 2003). As drug abuse compromises several aspects of mothers’ everyday functioning (Mayes, 1995; Mayes & Bornstein, 1997), this poses several risks for the adjustment of children.
Although maladjustment among drug abusers’ children can derive from their mothers’ substance use per se, coexisting psychiatric disorders, particularly those in the affective and anxiety domains, may also be implicated (cf. Hans, Bernstein, & Henson, 1999). Estimates of the prevalence of affective or anxiety disorders among individuals with histories of substance abuse range from 32% (Regier et al., 1990; Regier, Rae, Narrow, Kaelber, & Schatzeberg, 1998) to as high as 90% (Luthar, Cushing, Merikangas, & Rounsaville, 1998; Weissman et al., 1999). For many of these women, exposure to traumatic life experiences and chronic environmental stressors result in serious disturbances in everyday functioning (Kettinger, Nair, & Schuler, 2000), and evidence suggests that between 36 and 50% of treatment-seeking substance abusers suffer from posttraumatic stress disorder (PTSD; see Myrick & Kathleen, 2003, for a review).
Considerable research has demonstrated the negative consequences of maternal depression for children (Goodman & Gotlib, 2002; Hammen, 2003; Lyons-Ruth, Wolfe, & Lyubchik, 2000). In interactions with their offspring, depressed women are less attentive than others, show less reciprocity, and alternate between disengagement and intrusiveness. They are also more likely to express negative affect and aggression in parenting and make negative attributions about their children (Goodman, Adamson, Riniti, & Cole, 1994; Hammen, 2003). In parallel with these parenting problems, children of depressed mothers have been found to show poorer adjustment than comparison youth of similar socioeconomic backgrounds, with greater maladjustment across multiple domains (Hammen, 2003).
Although there have been fewer studies examining maternal anxiety disorders compared to depression, the comorbidity of the two disorders is so pronounced that it has led to theories of similar etiologies (Office of the Surgeon General, 1999). About one half of those with a primary diagnosis of major depression also have an anxiety disorder (Bargee, 1998; Regier et al., 1998). Extant evidence also suggests comparable risks to children (see Hirshfeld, Biederman, Brody, Faraone, & Rosenbaum, 1997; McClure, Brennan, Hammen, & Le Brocque, 2001). Based on their meta-analysis of 46 observational studies, Lovejoy, Graczyk, O’Hare, and Neuman (2000) argued that the behavior disturbances of depressed parents are best conceptualized not as correlates of their depression per se, but, rather, as stemming from generalized negative affect, that is, “aversive mood states including distress, anger, upset, guilt, and anxiety” (p. 564). Support for this argument is seen in studies on children of parents with anxiety disorders, depressive disorders, both depressive and anxiety disorders, and neither of these. The first three of these groups of children were no different from each other, and all were significantly more likely than the fourth to have diagnosable psychiatric disorders (Beidel & Turner, 1997).
In comparison to the strong evidence of risks linked with maternal negative affect, findings involving maternal substance abuse have been more equivocal. In contrasting drug-exposed children and nonexposed children of comparable socioeconomic status (SES), the former have shown more problems in specific neurological or cognitive domains (Mayes & Bornstein, 1997), but on psychological dimensions, group difference tend to be negligible. Summarizing the results of 46 studies on behavioral outcomes of young children prenatally exposed to drugs, Carta et al. (1994) reported significant effects for only half the outcomes examined, and the majority of these were among infants less than 1 month old, and were chiefly in the neurodevelopmental domain.
There are fewer studies examining school-age children of women who abuse drugs and comparison youth; those that exist suggest somewhat greater psychopathology among the former but interpretations are complicated due to possible confounds. Studies by Wilens, Biederman, Kiely, Bredin, and Spencer (1995) and Blanchard et al. (in press) showed higher symptom levels among children of substance abusers in comparison to children of non-users, but maternal depression and anxiety disorders were not controlled for in analyses. In addition, child symptoms were assessed solely by parent report, and thus, could have been inflated by the high distress commonplace among drug abusing parents (see Martin, Ford, Dyer-Friedman, Tang, & Huffman, 2004). Similarly, De Cubas and Field (1993) found that 6- to 13-year-old children of substance-abusing mothers scored higher than matched controls on most dimensions assessed by mothers’ reports, but for assessments conducted with the children themselves, differences were found on only 4 of the 16 group comparisons conducted.
The possibility that maternal substance abuse may be no more deleterious to children than maternal affective disturbances, in fact, may be even less so, is suggested by findings of research involving different types of parental problems. Johnson, Nusbausm, Bejarno, and Rosen (1999) found that adjustment problems did not differ as a function of drug exposure but did vary according to maternal stress and depression. In a 10-year study of low-income children first assessed at birth, concurrent maternal opioid abuse had nonsignificant links to child psychopathology at age 10, whereas maternal psychological symptoms other than substance abuse were linked to various child outcomes (Wakschlag & Hans, 1999). Several other studies have shown that among children of heroin or cocaine abusers, psychopathology tends to be particularly high among those whose parents have coexisting depressive problems (Hans, Bernstein, & Henson, 1999; Weissman et al., 1999).
Assessing Relative Risks: Maternal Drug Abuse Versus Affective/Anxiety Disorders
In our research, we appraised the relative risks linked with mothers’ drug abuse versus their depressive or anxiety diagnoses, via multiple analytic strategies. First, we simply compared levels of child maladjustment in groups defined by these sets of maternal diagnoses. Second, in variable-based (regression) analyses, we compared the magnitude of links between each maternal disorder and children’s adaptation levels in each of several adjustment domains, controlling for all other comorbid disorders in mothers. Third, we used person-based analyses to determine the likelihood of relatively resilient adaptation linked within each set of maternal diagnoses (by criteria described later; Luthar, 2006; Luthar, Cicchetti, & Becker, 2000).
Measurement of child outcomes involved multiple respondents and included aspects of both maladjustment and competence. As in our past work (Luthar & Cushing, 1999; Luthar et al., 1998) we considered lifetime psychiatric diagnoses of both a disruptive and an internalizing nature, with measurement based on reports by children and mothers. Symptom levels of recent internalizing problems were assessed by child report, as children are most privy to their inner distress (cf. Martin, Ford, Dyer-Friedman, Tang, & Huffman, 2004). Externalizing problems, often underreported by children (Martin et al., 2004), were assessed via mothers’ reports as were levels of social competence, capturing adults’ perspectives on children’s success at salient developmental tasks.
Proximal Protective and Vulnerability Processes
In addition to disentangling risks associated with maternal lifetime drug abuse versus affective diagnoses, we examined several aspects of maternal everyday functioning as potential vulnerability and protective factors, while controlling for group differences deriving from maternal diagnoses per se. There is much evidence that both drug abusing and depressed mothers experience high parenting stress and display problematic parenting, but there remain questions about which particular parenting behaviors carry the most pronounced ramifications. When mothers contend with urban poverty along with serious personal depression and high everyday stress, for example, it is plausible that the presence of harsh, maltreating behaviors will have greater prognostic significance for children than will the presence of positive behaviors such as interest in children’s everyday activities (cf. Crnic & Acevedo, 1995; Luthar, 2006). Accordingly, we examined mothers’ subjectively perceived parenting stress, negative parenting behaviors (by both mothers’ and children’s reports), as well as two positive parenting dimensions as reported by mothers, closeness (communication and involvement) and limit setting.
To summarize, our primary goal in this study was to illuminate the relative risks to children deriving from two sets of maternal diagnoses that commonly co-occur: substance abuse and affective/anxiety disorders, using both variable-based and person-based analyses. An additional goal was to determine the relative significance of both negative and positive parenting behaviors for children’s adjustment while controlling for group differences on the basis of maternal psychopathology.
Method
Sample
This study represents part of a larger longitudinal investigation of vulnerability and resilience among children of low-income mothers with major mental illness.1 To achieve variability on relevant maternal dimensions, we recruited women from outpatient treatment facilities for substance abuse and for other mental health problems (chiefly depression and anxiety), as well as from community settings such as churches, neighborhood stores, and primary health care facilities. The sample included 360 mother-child dyads. A cross tabulation of the presence or absence of diagnostic history for drug and for affective/anxiety diagnoses yielded the following: about 45% of these mothers (n = 163) had lifetime psychiatric diagnoses of abusing cocaine, opiates, or both, and the rest had no history of drug abuse (n = 197), and about 45% of the women had lifetime affective/anxiety diagnoses (n = 165). Within these overarching groups, about 60% of those women with drug histories also had lifetime affective/anxiety diagnoses (n = 94). Finally, about 35% of the sample had no history of affective/anxiety or drug diagnoses (n = 126). In analyses that follow, the following labels are used to refer to the four groups of mothers: drug only (substance abuse without affective/anxiety disorders); affective/anxiety only (depressive or anxiety diagnoses without substance abuse), comorbid (drug abuse and affective/anxiety diagnoses), and neither (neither drug abuse nor affective/anxiety diagnosis).
Regarding the relative prevalence of affective versus anxiety disorders and their comorbidity, an overwhelming majority of those in the affective/anxiety-only group (85.9%) and those in the comorbid group (72.3%) had a lifetime diagnosis of major depression disorder (MDD). The next most common diagnosis was PTSD, with 47.9% of those in the affective/anxiety-only group and 55.3% of those in the comorbid group meeting criteria. The percentage of women diagnosed with both an Anxiety disorder (generalized anxiety disorder, social phobia, panic disorder, or PTSD) and an affective disorder (MDD or dysthymia) was 50.7% in the affective/anxiety-only group and 40.4% in the comorbid group, respectively.
In each of the groups, the majority of the women (56.5% of the sample) heard about the study from a flyer posted in their community or in a mental health or drug and alcohol treatment clinic; 18.6% reported that they heard about it from a friend or study participant; 2.8% heard about it from a counselor. (The remainder reportedly could not recall where they heard about it or reported hearing about it from “other” sources.) Participants were told that they were participating in a study on family life and child development to better understand what helps mothers and children do well despite stress in their lives. Requirements were that the mother be the biological mother of a child between 8 and 17 years of age, be the child’s legal guardian, and live with the child. Women were screened for psychotic features and excluded if they were on antipsychotic medications and/or had a history of psychosis.
The majority of the measures were administered by oral interview by highly trained, master’s degree level interviewers. In addition, reading comprehension was assessed for both mothers and children as part of the administration of the Kaufman Brief Intelligence Test (Kaufman & Kaufman, 1990), and those participants with low reading levels were administered all instruments by oral interview. Upon completion of the interview, the child received a $40 gift certificate (if child was under 13) or $40 (if he/she was over age 13); the mother received $40 cash and a bonus of $20 if her child finished as well.
Descriptive data on the four subgroups are presented in Table 1. As shown there, approximately two-thirds of mothers were of ethnic minority backgrounds across the groups, and most were single parents. About half of the families received welfare (referred to as Aid for Dependent Families and Children at the time of the interview), and the mean monthly income (including welfare) for the sample was $1,147; about one-fourth of the state average for families during the time these data were collected.2 Education levels were approximately at the high school level across groups, though the Comorbid group had lower levels than the affective/anxiety-only and neither groups. Given these differences, we controlled for education levels in all statistical analyses.
Table 1.
Characteristics of mothers and children according to four groups based on mothers’ diagnoses: Drug only, affective/anxiety only, comorbid, and neither
| Groups of Mothers by Diagnoses
|
|
Groups of Mothers by Diagnoses
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternal Indices | Drug Only (n = 69) | Aff/Anx Only (n = 71) | Comorbid (Drug + Aff/Anx) (n = 94) | Neither (n = 126) | p | Child Indices | Drug Only (n = 69) | Aff/Anx Only (n = 71) | Comorbid (Drug + Aff/Anx) (n = 94) | Neither (n = 126) | p |
| Background variables | Background variables | ||||||||||
| Minority ethnicity | 48/69% | 42/59% | 57/61% | 90/71% | Gender: girls | 32/46% | 28/39% | 46/49% | 61/48% | ||
| Mean age | 39.30N | 39.90N | 37.96 | 36.88DA | .01 | Mean age | 12.19 | 12.39 | 12.18 | 11.79 | |
| Single parent status | 58/83%AN | 48/68%DC | 84/89%AN | 87/69%DC | .01 | Psychiatric diagnoses | |||||
| Mean years of education | 11.87AN | 13.23C | 11.68N | 12.93DC | .001 | Internalizing | 29/41% | 39/55%N | 48/5 1%N | 46/37%AC | .05 |
| Frequently unemployed | 47/67%N | 40/56% | 57/6 1%N | 54/43%DC | .01 | Disruptive | 15/21% | 23/28%N | 28/30%N | 17/14%AC | .01 |
| Receiving welfare | 39/56%C | 48/68%CN | 37/39%DA | 57/45%A | .01 | Substance use | 5/7% | 5/7% | 13/14%N | 3/2%c | .05 |
| Total monthly income | $1,282.11 | $1,006.01 | $951.01N | $1298.81C | .01 | Any disorder | 39/56% | 47/66%N | 59/63%N | 57/45%AC | .05 |
| Treatment seeking | Dimensional outcomes | ||||||||||
| Current drug/alc tx or counseling | 36/51%N | 38/54%N | 52/55%N | 19/15%DAC | .001 | Internalizing | 43.23 | 45.34 | 45.12 | 44.59 | |
| Psychiatric diagnoses | Externalizing | 52.80N | 54.63N | 55.32N | 46.10DAC | .001 | |||||
| Alcohol abuse/dependence | 14/20%CN | 10/14%CN | 38/40%DAN | 5/6%DAC | .001 | Competence | 46.32 | 46.87 | 45.34 | 48.77 | |
| Antisocial personality disorder | 52/74%N | 44/62%CN | 74/79%AN | 43/34%DAC | .001 | Parenting perceptions | |||||
| Any disorder | 70/100%N | 71/100%N | 94/100%N | 44/35%DAC | .001 | Negative parenting behavior | 97.83 | 99.56 | 97.35 | 96.83 | |
| Parenting perceptions | |||||||||||
| Negative parenting behavior | 91.15A | 101.15DN | 96.70N | 90.99AC | .001 | ||||||
| Total parenting stressa | 76.88AC | 86.85DN | 86.58DN | 70.16AC | .001 | ||||||
| Limit setting | 48.67N | 48.93N | 45.90N | 52.77DAC | .001 | ||||||
| Closeness | 54.10 | 51.96 | 53.14 | 54.27 | |||||||
Note: Entries in the table represent the numbers/percentages for categorical variables and group means for continuous variables; the significance for group differences is based on chi-square and univariate F tests, respectively. Subscripts indicate instances where means differed between groups and refer to the first letter of the group. Continuous variables in italics are based on child reports, and others are based on mother reports; child diagnoses are based on both mothers’ and children’s reports.
The PSI total score.
Maternal psychopathology
The presence of maternal psychiatric disorders was assessed based on the interviewer-administered computerized version (Erdman et al., 1992) of the Diagnostic Interview Schedule (DIS; Robins, 1995; Robins et al., 1989), and disorders were considered to be present only if they occurred during the lifetime of the child in the study. The C-DIS-IV is a structured interview that can be administered by lay interviewers and assesses for presence of a DSM-IV lifetime history of symptoms as well as current (past 12 months) symptoms. All responses are preceded, and the measure has demonstrated good reliability and criterion validity (Malgady, Rogler, & Tryon, 1992).
Child psychopathology and maladjustment
Child psychiatric diagnoses were assessed using the Computerized Diagnostic Interview Schedule for children (C-DISC-4.0; NIMH DISC-IV Editorial Board, 1995). The C-DISC-4.0 was designed to address more than 30 psychiatric diagnoses in children and adolescents (lifetime and in the past 12 months), and has parallel versions for parent and child informants: the DISC-P, for parents of 6- to 17-year-olds, and the DISC-Y, for direct administration to children and youths aged 9–17 years (Shaffer, Prudence, Lucas, Dulcan, & Schwab-Stone, 2000). Internalizing disorders were considered present if the child met the lifetime criteria for one or more of the following according to child or mother report: dysthymia, major depressive episode, posttraumatic stress, generalized anxiety, separation anxiety, panic, social phobia, and agoraphobia. Similarly, children’s lifetime externalizing disorders (conduct, oppositional defiant, and attention deficit) were considered in a single category, with the label of disruptive disorders and were based on child or mother report. The decision to use an “or” rule in computing final diagnoses was based on Grills and Ollendick’s (2002) recommendation that given the usually limited agreement between parents and children regarding children’s lifetime diagnoses and the likelihood that children may not be able to reliably recall symptoms that occurred in early childhood, the optimal approach is to combine information from both (see also Bird, Gould, & Staghezza, 1992).
Dimensional outcomes of current child adjustment were assessed via the Behavioral Assessment System for Children (BASC; Reynolds & Kamphaus, 1992), via the child (ages 6–11) and adolescent (ages 12–18) versions (Self-Report of Personality) and the parent version (Parent Rating Scale [PRS]). The T scores above 60 on these subscales indicate clinically significant scores (Reynolds & Kamphaus, 1992). Internalizing symptoms were assessed via children’s reports on a composite of the depression and anxiety BASC subscales. Composite PRS scores of externalizing symptoms (hyperactivity, aggression, and conduct problems) and on competence (adaptability, social skills, leadership) were used respectively to capture children’s disruptive behaviors and everyday competence. Both the child and parent versions of the BASC have good psychometric properties (Adams & Drabman, 1994; Flanagan, 1995; Kamphaus & Frick, 1996). For this sample, the Cronbach α coefficients were .97 for the C-BASC internalizing composite and .82 and .85 for the PRS externalizing and competence composites, respectively.
Parenting indices
The Parenting Stress Index Short Form (PSI/SF; Abidin, 1995) is a 36-item questionnaire with a 5-point scale, subsuming three subscales (Castaladi, 1990; Huenstein, Scarr, & Abidin, 1987): difficult child (which measures children’s self-regulatory capacity, including adaptability, demandingness, mood, and distractibility/hyperactivity), parent-child dysfunctional interaction (which measures the extent to which the parent does not derive satisfaction from interaction with the child), and parental distress (which signals role restriction, isolation, spousal relation problems, and depression), as well as a total stress score, which is a sum of the three. A raw total stress score of 90 (at or above the 90th percentile) represents a clinically significant score. For analyses predicting to child outcomes, an adapted parenting stress score was computed without the difficult child subscale to avoid confounding parenting stress with child outcomes particularly externalizing problems. Psychometric adequacy of PSI/SF has been well established (Abidin, 1995); for this sample, the Cronbach α coefficient was .89 for the adapted parenting stress score and .93 for the PSI total score.
The dimension of negative parenting was assessed via both mothers’ and children’s reports on the Parental Acceptance/Rejection Questionnaire (Rohner, 1991), a 60-item questionnaire with four subscales: low warmth/affection, aggression/hostility, neglect/indifference, and undifferentiated rejection. Each subscale contains 15 items rated on a 4-point scale and has good reliability and validity (Rohner, 1991). For this sample, the Cronbach α coefficients ranged from .69 to .82 for mothers and .76 to .91 for children, respectively, and values for the total negative parenting scores were .77 and .79.
Positive parenting behaviors were assessed via mothers’ report on the Parent–Child Relationship Inventory (PCRI; Gerard, 2000), a 78-item measure rated on a 4-point scale. The PCRI consists of seven subscales, and three of these measured positive interactions relevant to this study. The communication (capacity to talk and empathize with children), and involvement (expressed interest in children’s activities) subscales were used to assess parent-child closeness (as in other studies, these were highly correlated, r = .70, and thus combined; Luthar & Suchman, 2000). Limit setting was used to measure the effectiveness and character of mothers’ discipline techniques, with low scores indicating an inability to establish appropriate guidelines for children. On these subscales, T scores below 40 represent problems of clinical significance (Gerard, 2000). Good psychometric properties have been established for the PCRI (Gerard, 2000; Heinz & Grisso, 1996), and for this sample, the Cronbach α coefficients ranged between .74 and .82.
Results
Descriptive statistics
Table 1 provides profiles of adjustment of mothers and children, presented separately in the four groups defined according to the maternal disorders of central interest: drug only, affective/anxiety only, comorbid, and neither. In terms of other coexisting maternal diagnoses, the groups differed significantly with alcoholism being highest in the comorbid group (44.2%) and antisocial personality disorder highest in the drug-only followed by the comorbid group.
It should be noted that rates of antisocial personality disorder (ASPD) in this sample are probably inflated because antisocial problems often are confounded with (a) substance use and (b) poverty. To illustrate, in this study about 35% (n = 75) of those meeting ASPD criteria reported that their antisocial behaviors occurred only after drinking alcohol or doing drugs. (It is not surprising that the rates of antisocial behavior exclusively in relation to alcohol or drug abuse for those who met ASPD criteria were significantly higher in the drug-only and comorbid groups, 55.8 and 51.4%, respectively, vs. 9.1 and 9.3% in the affective/anxiety only and neither groups; χ2 = 47.01, p< .001.)
With regard to the second set of confounds, a defining feature of ASPD, “the failure to sustain good job performance over a period of several years” (Robins, 1995), characterized much of this low-income sample of women. Of the 213 women meeting criteria for anti-social problems, 98 (46.0%) reported that they had “made money illegally, including selling drugs or prostitution.” Again, this behavior was significantly higher among women in the drug-Only and comorbid groups (57.7 and 68.9%, respectively, in comparison to 7.1% in the affective/anxiety-only group and 23.8% in the neither group; χ2 = 42.8, p < .001). Regarding other evidence of financial problems, just under half of those in the sample who met antisocial personality criteria reported other behaviors commonly associated with poverty (with prevalence rates comparable across groups). Specifically, 98 reported that they “had times when they had no fixed address or were homeless,” 91 reported “trouble with debts,” 91 reported that they “did not work for several months when they were not caring for children,” 69 “quit a job without savings,” and 99 reportedly “borrowed more than $20 without giving it back.” In sum, illegal behaviors specifically related to substance use and high rates of unemployment and poverty in this sample contributed to unusually high rates of antisocial personality diagnoses.
With respect to children’s psychiatric disorders (see Table 1), children of affective/anxiety-only mothers had the highest percentage of “Any disorder,” with 66% meeting criteria for a disorder as reported by mother or child. Disruptive disorders also were highest among offspring of the affective/anxiety-only mothers (55%) followed by the comorbid and drug-only groups, while internalizing disorders were highest among offspring of the comorbid group (30%) followed by affective/anxiety-only and drug-only groups. Rates of substance use were highest for children in the comorbid group. Chi-square analyses indicated significant group differences in all instances, and post hoc chi-square comparisons of pairs indicated significant differences between the affective/anxiety-only and comorbid groups in relation to the neither group.
In comparing the groups on continuous variables, a multivariate analysis of variance was conducted, Wilks’ Λ = .85, F (7.08), p < .001, followed by univariate analyses of variance and post hoc comparisons of means. Similar to the pattern seen on categorical variables, on mothers’ self-reported parenting indices, the affective/anxiety-only and comorbid groups reflected the greatest impairment. Mothers’ reports of their children’s externalizing behavior was significantly higher across the maternal psychiatric groups in comparison to the Neither group, while the groups did not differ with respect to mother-reported child social competence. On child-reported internalizing symptoms, both the affective/anxiety-only and comorbid offspring reported significantly higher symptoms in comparison to the neither group, while group differences were nonsignificant with respect to negative parenting behaviors.
In sum, group comparisons generally showed that the comorbid and affective/anxiety-only (but not the drug-only) groups showed significantly more impairment than the neither group among both mothers and children.
Maternal drug abuse versus affective/anxiety disorders: Variable-based analyses
To supplement these group comparisons (based on groups of children defined by maternal disorders), we conducted variable-based analyses to ascertain the degree to which maternal drug abuse and affective/anxiety disorders were linked with the five child outcomes: disruptive disorders, internalizing disorders, internalizing symptoms, externalizing symptoms, and competence. Logistic and multiple regressions were conducted for the categorical and continuous outcome variables, respectively. Controlling for demographics (minority status, mother’s education level, and child age and gender), we examined the unique contributions of maternal drug abuse and affective/anxiety disorders as well as the two other diagnoses that also tend to co-occur with maternal addiction: alcoholism and ASPD. The decision of which demographic variables was guided by evidence that among mostly single mothers in poverty, maternal education is a more stable predictor of SES than current income (Hoff-Ginsberg & Tardif, 1995; Suchman & Luthar, 2001).3
All of the models significantly predicted child outcomes. Findings showed that maternal drug abuse was not uniquely associated with any of the child outcomes (see Table 2). Conversely, maternal affective/anxiety diagnosis was associated with significant risk in four of the five domains: children’s disruptive and internalizing diagnoses, as well as both externalizing and internalizing symptoms. Of the other psychiatric conditions, only APSD was associated with child outcomes, linked with children’s disruptive diagnoses and externalizing symptoms.
Table 2.
Regression analyses with maternal diagnoses predicting child outcomes
| Disruptive Diagnosesa | Internalizing Diagnosesa | Externalizing Symptomsb | Internalizing Symptomsc | Competenceb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Demographic indices | ||||||||||
| Block 1 ΔR2/Δχ2 | 6.03 | 12.97* | .09*** | .05** | .09*** | |||||
| Child age | .08 | .09 | −.07 | −.08 | .05 | .06 | .06 | .05 | −.13* | −.13** |
| Child genderd | .33 | .40 | −.52* | −.52* | .27*** | .29*** | .12* | .13* | −.18* | −.19*** |
| Minority ethnicity | −.20 | −.09 | .18 | .25 | .01 | .04 | .16** | .17** | −.04 | −.05 |
| Mother education | −.05 | −.04 | −.08 | −.08 | −.13* | −.09 | −.08 | −.10 | .19*** | .18** |
| Maternal diagnoses | ||||||||||
| Block 2 ΔR2/Δχ2 | 16.73** | 8.93* | .09*** | .02* | .01 | |||||
| Drug diagnosis | −.09 | −.05 | .03 | −.10 | −.03 | |||||
| Affective/anxiety diagnosis | .69* | .66** | .16** | .13* | −.05 | |||||
| Alcoholism diagnosis | −.14 | .11 | −.01 | −.08 | .00 | |||||
| Antisocial personality diagnosis | .79* | −.15 | .20*** | .06 | −.11 | |||||
| Model ΔR2/Δχ2 | 22.77** | 21.90** | .18*** | .07*** | .10*** | |||||
Note: Logistic and multiple regressions were used in predicting categorical variables and continuous variables, respectively. Unstandardized coefficients are presented for logistic regressions and standardized coefficients are presented for multiple regressions.
Mother and child report.
Mother report.
Child report.
Girl = 0.
p < .05.
p < .01.
p < .001.
Group comparisons of resilient adaptation
To further explore child adjustment vis-à-vis maternal drug abuse versus affective/anxiety disorders, we conducted person-based analyses to determine the proportions of children manifesting relative resilience across different adjustment domains. Given the severity of risk factors facing this sample (poverty and maternal psychiatric disorders), children’s resilience was defined here as evasion of serious psychopathology (no psychiatric diagnoses and symptoms below clinical cutoffs) and presence of average social competence (see Luthar, 2006; Luthar et al., 2000).
Results of these analyses are presented in Figure 1, shown separately for children in the four groups of mothers (drug only, affective/anxiety only, comorbid, neither). For each group, the three contiguous bars represent, in turn (a) the proportion of youth who had no disruptive psychiatric diagnoses and had externalizing symptom levels below the clinical cutoff (T score = 60); (b) of this subset, the proportion who had no internalizing diagnoses and had depressive/anxiety symptom levels below the clinical cutoff (T score = 60); (c) of this subset, the proportion who showed at least average competence scores (as reported by mothers on the BASC; T score ≥ 50). Consistent with the previously discussed findings, the smallest proportion of manifestly resilient children (the final bar within each set) were in the comorbid and affective/anxiety-only groups (7.4 and 16.9%, respectively). Post hoc comparisons of pairs of groups showed two significant differences: the proportion of manifestly resilient children was lower in the comorbid group as compared to the drug-only, χ2 (1) 6.75, p < .01, and neither groups, χ2 (1) 9.54, p < .01.
Figure 1.
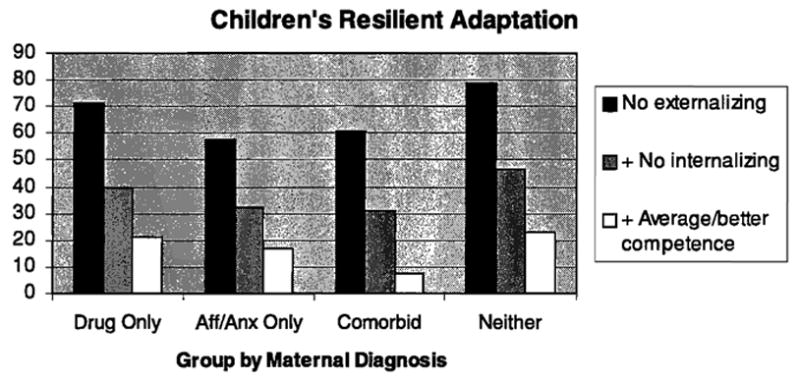
The percentage of children showing positive adaptation across multiple domains, by mothers’ psychiatric diagnoses of drug abuse and affective/anxiety disorders.
We reran the preceding analyses separately for boys and girls and then again separately for children under 12 years versus those 13 and older. Group differences were nonsignificant in these cases, possibly reflecting limited statistical power (several cell sizes became smaller than five).
Vulnerability and protective processes
The final analyses were on vulnerability and protective processes related to children’s adjustment levels. Multivariate regression analyses were conducted with controls for demographic predictors: child age, child gender, minority status, and maternal education. To fully explain any differences between the four groups and to identify any group-specific processes, potentially salient in one maternal psychiatric group more so than others, we used three orthogonal Helmert contrast codes to compare the mean of each level to the mean of all the succeeding levels (Wendorf, 2004). Contrast 1 compared the neither group to the average of the other three groups, Contrast 2 compared the comorbid group to the average of the affective/anxiety-only group and the drug-only group, and Contrast 3 compared the drug-only group with the affective/anxiety-only group (our primary research question).4 Next, the four parenting dimensions, stress, negative parenting behaviors (as an average of children’s and mother’s reports), closeness, and limit setting, were entered. Finally, interaction terms of Contrast 3 times each of the parenting indices were entered, to identify any differences in processes among children of drug abusers versus those whose mothers had affective or anxiety diagnoses.
As shown in Table 3, effects for the demographic indices showed that younger child age was associated with greater risk for internalizing diagnoses in the complete model. Boys had higher externalizing and internalizing symptoms than girls, while girls exhibited higher rates of internalizing diagnosis and competence levels. Maternal education was linked with relatively good child competence.
Table 3.
Vulnerability and protective indices: Maternal psychiatric group Helmert contrasts and parenting indices predicting child outcomes
| Disruptive Diagnosisa | Internalizing Diagnosisb | Externalizing Symptomsb | Internalizing Symptomsc | Competenceb | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographic indices | |||||||||||||||
| Block 1 ΔR2/Δχ2 | 5.14 | 12.85* | .09*** | .05** | .10*** | ||||||||||
| Child age | .06 | .05 | .01 | −.09* | −.10* | −.12** | .04 | .02 | −.05 | .03 | .03 | −.02 | −.15** | −.15** | −.01 |
| Child genderd | .29 | .33 | .47 | −.50* | −.47* | −.44* | .27*** | .28*** | .27*** | .13* | .14* | .10 | −.19*** | −.19*** | −.17*** |
| Minority ethnicity | −.31 | −.22 | −.26 | .15 | .24 | .13 | −.00 | .03 | .05 | .14*** | .15** | .10 | −.03 | −.04 | .01 |
| Mother education | −.05 | −.05 | .05 | −.07 | −.07 | −.07 | −.13* | −.11* | −.00 | −.08 | −.10 | −.04 | .20*** | 19*** | .13** |
| Maternal psychiatric contrasts | |||||||||||||||
| Block 2 ΔR2/Δχ2 | 8.27* | 9.75* | .06*** | .02 | .00 | ||||||||||
| Neither vs. aff/anx, comorbid, and drug | −.19* | −.05 | −.14* | −.09 | −.24*** | −.15** | .01 | .03 | .04 | −.01 | |||||
| Comorbid vs. aff/anx and drug | .01 | −.03 | .02 | .04 | .01 | −.03 | .04 | .06 | −.02 | −.01 | |||||
| Drug vs. aff/anx | .26 | .11 | .36* | .23 | .06 | −.03 | .12* | .08 | −.01 | .05 | |||||
| Parenting indices | |||||||||||||||
| Block 3 ΔR2/Δχ2 | 60.59*** | 9.62* | 22*** | .12*** | 20*** | ||||||||||
| Parenting stress | .05*** | .03** | .06 | −.08 | −.09 | ||||||||||
| Negative parenting behaviors | .12* | .04 | .10* | .38*** | −.19** | ||||||||||
| Closeness | .01 | .01 | −.01 | .09 | .27*** | ||||||||||
| Limit setting | −.06** | .02 | −.40*** | −.07 | .05 | ||||||||||
| C3 × parenting indicese | |||||||||||||||
| Block 4 ΔR2/Δχ2 | 5.63 | 3.36 | .01 | .01 | .00 | ||||||||||
| Model ΔR2/Δχ2 | 79.63*** | 35.57** | .38*** | .19*** | .30*** | ||||||||||
Note: Logistic and multiple regressions were used in predicting categorical variables and continuous variables, respectively. Unstandardized coefficients are presented for logistic regressions and standardized coefficients are presented for multiple regressions.
Mother report.
Mother and child report.
Child report.
Girl = 0.
Coefficients for this block are not presented, given that the block was nonsignificant for all outcomes. Betas for the other predictors did not change significantly as a result of this block; thus, the coefficients presented in block 3 (column 3) represent those for the final model.
p < .05.
p < .01.
p < .001.
For the block involving contrasts among different maternal psychiatric groupings, results showed that when these were considered without parenting indices in the model, Contrast 1 (comparing the neither group to the others) was linked to both sets of child diagnoses and with externalizing problems. Similarly, Contrast 3 (comparing the drug only to the affective/anxiety only) was associated with internalizing diagnosis and internalizing symptoms (as Table 1 shows, the affective/anxiety-only group demonstrated higher levels of both of these outcomes). However, once the parenting indices were also considered in the full model, the only effect remaining significant was for Contrast 1 in relation to externalizing symptoms, suggesting that differences in parenting behaviors mediated the previously established differences of higher disruptive and internalizing diagnoses and internalizing symptoms among children of diagnosed mothers.
Of the parenting dimensions examined as vulnerability or protective indices, the strongest associations were for mothers’ negative parenting behaviors; these had significant unique links with all outcomes except internalizing diagnoses. With regard to positive parenting, mothers’ reports of their own limit setting were inversely linked with child externalizing symptoms and children’s disruptive disorder diagnoses, and reports of closeness were associated with high everyday competence. Finally, parenting stress had significant unique links with the both disruptive and internalizing diagnoses, but with none of the dimensional indices of current functioning.
The block of interaction effects involving Contrast 3 and each parenting dimension was not statistically significant in relation to any outcome. Thus, component interactions were not considered any further.
Vulnerability effects, promotive effects, or both?
To explore the degree to which the associations listed above reflected vulnerability processes (connoting child adjustment poorer than average) as opposed to promotive ones (connoting exceptionally positive child adjustment), we followed procedures to graph outcomes, for all continuous dimensions, as suggested by resilience researchers (e.g., Luthar & Latendresse, 2005; Luthar & Zelazo, 2003). (This was not done for categorical outcomes as “normative” rates of diagnoses are not clearly defined.) The graphs involved computing, for high, medium, and low levels of the significant predictor variables, or for boys as opposed to girls, mean scores on the outcome domain in question, with these outcome scores considered as standardized predicted values having controlled for all other predictors (including all possible differences between maternal psychiatric groups) in the regression equation in Table 3. These values are depicted in Figure 2, relative to national normative T scores of 50. Deviations of ±10 from 50 represent clinically significant levels.
Figure 2.
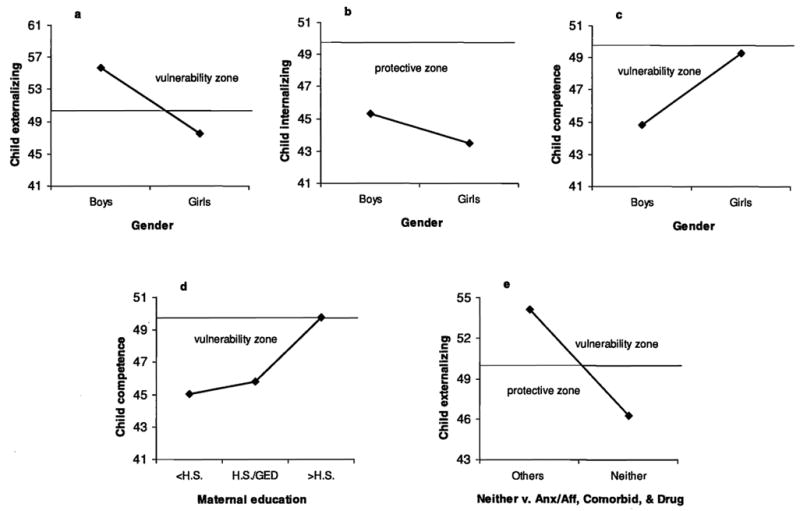
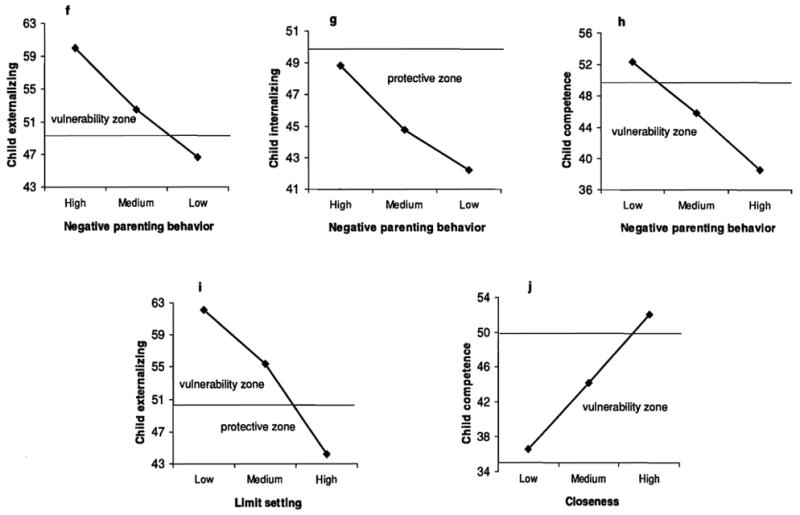
The associations of maternal psychiatric contrasts and vulnerability and protective indices with child adjustment outcomes. Lines indicate average symptom levels according to clinically established norms (T score = 50); SD = 10.
As shown in these figures, externalizing problems were somewhat above the national average for boys, and their competence below average, connoting modest vulnerability (mean T scores = 56 and 44 in Figure 2a and c, respectively). Both gender groups had internalizing symptoms below normative averages, with girls reporting particularly low symptoms (Figure 2b). In addition, maternal education at the high school level or less was linked with modest child vulnerability in everyday competence (mean T scores = 45, Figure 2d). Finally, externalizing symptoms were above average for the three maternal psychiatric groups (drug only, affective/anxiety only, and comorbid), with mean T scores of about 53; the absence of these maternal mental illnesses was modestly protective (T scores = 46, Figure 2e).
Contrasting with these findings involving the “global” predictor indices (demographics and maternal psychiatric illness) on the various parenting dimensions, extremes of continua placed children more clearly in clinically significant ranges. Specifically, when negative parenting behaviors were high (at or above the clinical cutoff of 110), child externalizing symptoms fell above clinically significant levels (mean T score = 60, Figure 2f) and significant vulnerability was also seen in relation to everyday competence (mean T score = 38, Figure 2h). Conversely, when mothers showed low negative parenting behaviors (below the “normal” range of 90–110), their children reported unusually low internalizing symptoms (T score = 42, Figure 2g). On the positive parenting indices, similarly, low limit setting represented vulnerability to clinically significant externalizing problems (mean T score = 62, Figure 2i) as low levels of closeness connoted significant vulnerability in everyday competence (mean T score = 36, Figure 2j).
Discussion
Whereas maternal drug abuse is widely seen as highly inimical to children, this study showed that it did not connote significantly more risk than did maternal depressive and anxiety diagnoses. Three sets of analyses converged in pointing to the same conclusion: those involving (a) comparisons of child maladjustment across four groups of mothers (with diagnoses of drug-only, affective/anxiety disorder only, comorbid, and neither), (b) variable-based analyses where maternal diagnoses predicted to different child outcomes, and (c) comparisons of manifestly resilient children of mothers in the drug-only, affective/anxiety-only, comorbid, and neither groups. In all instances, children of drug-abusing mothers fared no worse than did those of mothers with affective or anxiety disorders.
Maternal drug abuse and other psychopathology: Specificity of effects
In comparing child maladjustment across maternal diagnostic groups, rates of at least one lifetime psychiatric diagnosis were one and a half times as high among children in the maternal affective/anxiety-only group (66%) as well as in the comorbid group (63%) in comparison to the neither group (45%). Conversely, rates in the drug-only group did not differ significantly from those in the neither category (56 vs. 45%).
Similarly, results of our variable-based analyses showed no evidence of maternal drug abuse as a risk factor when examined concurrently with other comorbid diagnoses. Hierarchical multiple regression analyses, with controls for demographic characteristics and other comorbid diagnoses, showed that maternal drug abuse did not have any unique links with the child outcomes considered. By contrast, a maternal depression or anxiety diagnosis was associated with risk in four of the five outcomes: children’s diagnoses both in the disruptive and internalizing categories (based on mothers’ and children’s reports) as well as children’s self-report of internalizing symptoms and mothers’ perception of externalizing symptoms.
Finally, person-based analyses of resilient adaptation among children were consistent. Findings showed that the evasion of serious externalizing and internalizing psychopathology, along with at least average social competence (or the maintenance of “cross-domain resilience”) was lower among children whose mothers had affective anxiety disorders: 7% for comorbid and 17% for affective/anxiety only, as opposed to 21% for drug only and 23% for neither, with significant differences in post hoc comparisons of pairs of groups for the comorbid group in relation to the drug-only and neither groups.
These results substantiate prior findings on parental substance abuse coexisting with depression, while also providing new insights. In their family-genetic research, Weissman and colleagues (1999) have shown that children of opioid abusers display greater psychopathology in the presence, versus the absence, of comorbid depression in their parents. Building on this work, the present findings suggest that, within the combination of parental substance abuse and depression, it is the latter more than the former that seems to be the more “active ingredient” in conferring risks to children.
The apparently differential vulnerability conferred by maternal negative affect disorders compared to substance abuse might partly reflect genetic factors, unmeasured in this study. To illustrate, the presence of a short form (“s” allele) of the gene coding, implicated in the inefficient transportation of serotonin, has been linked to relatively high rates of depression among maltreated children lacking in adult supports (Kaufman et al., 2004), and also among previously maltreated adults who experience high life stress (Caspi et al., 2003). In parallel, it is plausible that in this study, maternal affective and anxiety disorders might have been more likely than maternal drug abuse to confer genotypes connoting relatively high child reactivity to external, environmental stressors.
It is also possible that affective disturbances have particularly pervasive and enduring effects on mothers’ everyday functioning. As noted by Lovejoy and colleagues (2000), negative emotion states can result in a variety of adverse maternal behaviors ranging from irritability and aggression to withdrawal and general lack of responsiveness. Moreover, the authors point out that parenting that is harsh and low in warmth can endure even when a mother’s depression is in remission. To date, there is no comparable evidence, to our knowledge, establishing such ubiquitous, robust ill effects on parenting as a result of a substance abuse diagnosis at some prior point in a mother’s life.
The apparently greater psychopathology among children in the affective/anxiety and comorbid groups may also partly derive from relatively negative, or relatively realistic, perceptions among mothers. Self-criticism and a low threshold for tolerating stress are hallmarks of internalizing disorders, such that slight “transgressions” by the children (disruptiveness) or the mothers themselves (e.g., harsh parenting) could come to assume large proportions in the mothers’ minds. As Rogosch and colleagues have demonstrated, depressed mothers express more negative emotion and criticism not only in relation to their children but also toward themselves (Rogosch, Cicchetti, & Toth, 2004). Effect sizes of group comparisons in this study are consistent with this suggestion: group differences were far greater when it was mothers rather than their children who were rating their negative parenting behaviors.
Vulnerability and protective processes
Our findings showed that far more than their histories of particular psychiatric illnesses, mothers’ contemporaneous parenting behaviors had strong links with child outcomes. For the contrasts involving various maternal psychiatric groupings, significant effects with child outcomes were found for the neither versus the three other maternal groups (drug abuse and affective/anxiety disorders, alone or in combination) and for the drug only versus affective/anxiety only. Once aspects of the mothers’ current functioning were considered, however, all associations for this psychiatric status contrast but one, the neither versus others predicting to child externalizing symptoms, became nonsignificant, and even in this case, the variance explained by the contrast was much lower than that explained by the four parenting dimensions (R2 change of .06 vs. .22). These findings corroborate prior suggestions that more than a mother’s history of particular mental illnesses, it is the current context of the child’s environment, including their caregivers’ negative and positive behaviors, that is likely to be reflected in children’s outcomes (Sameroff, 2000).
Of the four parenting dimensions we examined, effects were most pronounced for negative parenting, which encompasses mothers’ hostility, rejection, neglect, and lack of warmth. This dimension had significant unique links with children’s disruptive diagnoses and with all three dimensional child outcomes, self-reported internalizing symptoms and mothers’ reports of externalizing problems and low competence. In addition, on the last two of these three continuous outcomes, high negative parenting clearly connoted significant vulnerability, with children’s falling in clinically significant ranges of maladjustment. Collectively, these findings resonate with Cicchetti’s (2002) caution that caregivers’ harsh, rejecting behaviors can be highly inimical for child well-being, impairing children’s coping, and competence across multiple domains.
Also connoting significant vulnerability for externalizing and lack of everyday competence were low levels of maternal limit setting and low closeness to children, respectively. Mothers’ self-reported effectiveness at limit setting was linked with their reports of low externalizing problems, as was high levels of closeness in relation to child competence. Conceptually, the domain specificity of these links makes sense; it is reasonable that children’s externalizing behaviors (but not everyday competence) would vary substantially on the adequacy of parent discipline, whereas children’s leadership and everyday social competence would be promoted by mothers’ closeness with their children (more so than by adequacy of discipline). At the same time, these links could reflect mothers’ modifications in their parenting behaviors in response to children’s adjustment. For example, mothers could have relinquished limit-setting efforts, to some degree, when children’s behaviors reached inordinately high levels, or conversely, they could have felt increasing warmth and involvement toward children who displayed high everyday competence. In the future, longitudinal analyses will be critical to tease apart the relative strengths of these directional links between mothers and their children.
Mothers’ self-reported parenting stress showed links with children’s disruptive and internalizing lifetime diagnoses but not with their current symptoms. One possible explanation for this discrepancy is that children are most affected by maternal stress early in their development, and that maturation facilitates a better understanding of a mother’s struggle to balance economic and emotional responsibilities to her children. Supporting this contention is that, whereas age effects were not evident in relation to any of the continuous outcomes measuring current behavior, analyses indicated higher risks for internalizing diagnosis among younger children. An alternative explanation for the differential results across outcomes involves causal links in the opposite direction. Mothers themselves may have experienced much more stress in the parenting role when their children had serious adjustment problems, extreme enough to meet diagnostic criteria, rather than when the latter manifested some elevations in contemporaneous symptom levels. Again, longitudinal analyses will be critical in disentangling these links.
One surprising finding in this study was the relatively low levels of current internalizing symptoms reported by children across maternal psychiatric groups. It is possible that children in this sample had difficulty in articulating inner distress, either due to developmental limitations or as a result of difficulty confronting their true feelings (see Schneider & Phares, 2005). Consistent with this suggestion, 15.2% of the child sample fell into the range of potentially positively biased responses according to the L-Index of the BASC (Adams & Drabman, 1994). Such defenses may represent a useful part of children’s self-regulatory strategies during middle childhood but do not necessarily protect them from internalizing problems later in life. Longitudinal research is needed to examine whether children’s reports of depressive and anxiety symptoms increase over time, particularly during adolescence and young adulthood.
Caveats, limitations, and implications
It is worthwhile to emphasize two important caveats surrounding our findings on maternal drug abuse, the first of which is that they do not by any means suggest that this is a “low-risk” parental problem. More than half of the drug abusers’ children (56%) in this sample had at least one lifetime psychiatric diagnosis themselves by the average age of 12 years, a statistic far from trifling. In addition, many of the children had not yet reached midadolescence, a period of sharp escalation in many problems including conduct disturbances, depressive disorders, and (most significantly from the standpoint of this sample) substance use. Finally, our comparison group was also clearly a troubled one, comprised mostly of poor mothers in inner-city neighborhoods, 45% of whom also had at least one psychiatric disorder. Similarity to children of these mothers is in no way reassuring about the levels of disturbance we documented among children in the drug-only group.
The second caveat is that our data pertain only to women’s substance abuse at some period during the lifetimes of their children, and not to their current abuse of cocaine or heroin. Over half of the women in each of the psychiatric groups were in treatment, and many, if not most, had achieved some level of abstinence. It is quite plausible that if we had a sample of women with contemporary problems of drug abuse, their children would in fact have shown more problems than SES-matched others.
Among the limitations that qualify the conclusiveness of our findings, the first lies in their cross-sectional nature. Reports of both mothers and children’s diagnoses were based on retrospective reports of lifetime problems, which can be subject to recall biases. Inferences about causality are also precluded; in additional to bidirectional links such as those suggested earlier (between maternal and child distress), third variables, such as family life in chronic poverty, could account for variations in levels of each. Finally, although all of the groups were of generally low SES, the comorbid group had the lowest level of education; this difference constitutes another limitation, notwithstanding the statistical controls we employed in the analyses reported.
In terms of implications for future research, our findings support arguments that in studies of resilience, “main effect” findings involving risk modifiers should not be arbitrarily described as reflecting vulnerability versus protective (or promotive) effects. To illustrate, boys in this low-income sample did, in fact, fare more poorly than girls on several dimensions in this study, but being male did not imply clinically significant levels of problems relative to national norms. Conversely, extremes of parenting behaviors did in fact connote significant child vulnerability. Unusually high negative parenting represented clear dysfunction in terms of children’s externalizing behaviors and their poor everyday competence, as low parent limit-setting and closeness, respectively, represented vulnerability for externalizing problems and competence. To have described the latter findings as suggesting protective or promotive effects for inner-city mothers’ effective limit-setting, or their high closeness with children, would have been both erroneous and misleading. In sum, our findings underscore the dangers of using the terms vulnerability and protection interchangeably, without first exploring the distributions of outcomes, at the respective extremes of predictors, in relation to average or normative scores on adjustment.
In terms of treatment implications, the most substantive message from this study is that there must be concerted attention to parenting problems among women in poverty. The non-trivial effect sizes for these constructs within our analyses, and their potential to become implicated in mutually aggravating cycles with child psychopathology jointly point to the urgency of this need. Service providers must directly address the distress and despair that afflict many mothers in poverty, many of whom are primarily responsible for the welfare of minor children in their care.
Our findings also have implications for policies surrounding maternal drug abuse. Perhaps more than any other psychiatrically disordered group, poor, single mothers with histories of drug abuse confront exceptionally negative attitudes from service providers, policy representatives, and the lay public (Garrity-Rokous, 1994; Luthar & Suchman, 2000). Typically perceived as having willfully jeopardized their families’ well-being, they are often subject to punitive measures such as mandatory drug testing when pregnant with subsequent children, and risk revocation of parental rights if drug abuse is confirmed. In comparison, mothers with histories of depression tend more often to be seen as victims of genetic predisposition or life circumstances, and rarely confront such punitive measures, notwithstanding any evidence (such as that reported here) that this disorder can be at least as deleterious for children as is prior maternal addiction. As we weigh such disparities in attitudes, it is worthwhile to consider that drug dependence is not a lifestyle that would be volitionally chosen by anyone. This is a psychiatric condition that, among many mothers, emerges in response to years of trauma, distress, and alienation. By the same token, it is also an illness, like depression, that can potentially show improvement with therapeutic attention to the woman’s personal well-being (e.g., Luthar & Suchman, 2000; Luther, Suchman, & Altomere, 2007).
Conclusion
In conclusion, findings of this study indicate that among economically disadvantaged families, mothers with prior histories of drug abuse can be no more inimical for their children’s well-being than their counterparts who have been drug free, at least through their children’s middle childhood and early adolescent years. More than maternal histories of particular psychiatric illnesses, disturbances in everyday parenting can seriously compromise the well-being of children in poverty, and conversely, resource-poor, disenfranchised mothers can report alarmingly high levels of parenting stress when their children have a psychiatric diagnosis.
Implications for future health care policies are clear: there must be concerted attention to mental health and parenting needs of mothers in urban poverty. From the standpoints of reducing emotional suffering among both mothers and their children, fostering resilient adaptation, and maximizing cost-efficacy of social programs, there is an urgent need for interventions targeting what is essential to maximize children’s potential: the emotional well-being of their primary caretakers and these women’s capacities to maintain supportive, engaged parenting.
Footnotes
The data presented here encompass the entire baseline sample of 360 mother-child dyads in a larger longitudinal project on vulnerability and resilience among children of low-income mothers with major mental illnesses. Preliminary, exploratory analyses of some of the questions addressed here were reported by Luthar, D’Avanzo, and Hites (2003), involving a subset of the baseline sample (i.e., those on whom data had been collected midway into the initial 5-year funding period).
The median monthly income for families in this state in 2000, which was around the time these data were collected (1998-2000), was approximately $5,029.17 (The Annie E. Casey Foundation, 2006).
Subsequent analyses included single parent status, maternal unemployment, and welfare receipt as controls, none of which was shown to have significant associations with child outcomes or to affect the results described here. We also explored effects of various treatment experiences (e.g., methadone maintenance and 12-step programs, length of psychiatric treatments), and again, considering these did not change the results from those reported here.
Inclusion of maternal alcoholism and antisocial personality disorder, and of maternal single-parent family status, did not change the results reported in Table 3.
Preparation of this manuscript was funded in part by grants from the National Institutes of Health (RO1-DA10726, RO1-DA11498, and R01-DA14385).
References
- Abidin RR, editor. Parenting Stress Index: Third edition professional manual. Lutz: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Adams CA, Drabman RS. BASC: A critical review. Child Assessment News. 1994;4:1–5. [Google Scholar]
- Bargee JG. Mixed symptoms and syndromes of anxiety and depression: Diagnostic, prognostic, and etiologic issues. Annals of Clinical Psychiatry. 1998;10:15–29. doi: 10.1023/a:1026198512361. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM. At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Medical Association. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Sexton CC, Morgenstern J, McVeigh KH, McCrady BS, Morgan TJ, et al. Children of substance abusing women on federal welfare: Implications for child well-being and TANF policy. Journal of Human Behavior in the Social Environment in press. [Google Scholar]
- Carta JJ, Sideridis G, Rinkel P, Guimaraes S, Greenwood C, Baggett K, et al. Behavioral outcomes of young children prenatally exposed to illicit drugs: Review and analysis of experimental literature. Topics in Early Childhood Special Education. 1994;14:184–216. [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig lW, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Castaladi J. Affective and cognitive patterns in the mother-child relationship during the second year of life. University of Virginia; Charlottesville: 1990. Unpublished doctoral dissertation. [Google Scholar]
- Cicchetti D. The impact of social experience on neurobiological systems: Illustration from a constructivist view of child maltreatment. Cognitive Development. 2002;17:1407–1428. [Google Scholar]
- Crnic K, Acevedo M. Everyday stress and parenting. In: Bornstein MH, editor. Handbook of parenting. Vol. 4. Mahwah, NJ: Erlbaum; 1995. pp. 277–297. [Google Scholar]
- De Cubas MM, Field T. Children of methadone-dependent women: Developmental outcomes. American Journal of Orthopsychiatry. 1993;63:226–276. doi: 10.1037/h0079429. [DOI] [PubMed] [Google Scholar]
- Erdman HP, Klein MH, Greist JH, Skare SS, Justed JJ, Robins LN, et al. A comparison of two computer-administered versions of the NIMH Diagnostic Interview Schedule. Journal of Psychiatric Research. 1992;26:85–95. doi: 10.1016/0022-3956(92)90019-k. [DOI] [PubMed] [Google Scholar]
- Flanagan R. A review of the Behavior Assessment System for Children (BASC): Assessment consistent with the requirements of the Individuals with Disabilities Education act (IDEA) Journal of School Psychology. 1995;33:177–186. [Google Scholar]
- Garrity-Rokous FE. Punitive legal approaches to the problem of prenatal drug exposure. Infant Mental Health Journal. 1994;15:218–237. [Google Scholar]
- Gerard AB. Parent-Child Relationship Inventory: Manual. Los Angeles: Western Psychological Services; 2000. [Google Scholar]
- Goodman SH, Adamson LB, Riniti J, Cole S. Mothers’ expressed attitudes: Association with maternal depression and children’s self-esteem and psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1265–1274. doi: 10.1097/00004583-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Grills AE, Ollendick TH. Issues in parent-child agreement: The case of structured diagnostic interviews. Clinical Child and Family Psychology Review. 2002;5:57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- Hammen C. Risk and protective factors for children of depressed parents. In: Luthar SS, editor. Resilience and vulnerability: Adaptation in the context of childhood adversities. Cambridge: Cambridge University Press; 2003. pp. 50–75. [Google Scholar]
- Hans SL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development and Pyschopathology. 1999;11:957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Heinz MC, Grisso T. Review of instruments assessing parenting competencies used in child custody evaluations. Behavioral Sciences and the Law. 1996;14:293–313. [Google Scholar]
- Hirshfeld DR, Biederman J, Brody L, Faraone SV, Rosenbaum JF. Expressed emotion toward children with behavioral inhibition: Associations with maternal anxiety disorder. Journal of American Academy of Child & Adolescent Psychiatry. 1997;36:910–917. doi: 10.1097/00004583-199707000-00012. [DOI] [PubMed] [Google Scholar]
- Hoff-Ginsberg E, Tardif T. Socioeconomic status and parenting. Handbook of Parenting. In: Bornstein MH, editor. Biology and ecology of parenting. Vol. 2. Mahwah, NJ: Erlbaum; 1995. pp. 161–188. [Google Scholar]
- Huenstein E, Scarr S, Abidin RR. Detecting children at risk for developmental delay: Efficacy of the Parenting Stress Index in non-American culture. University of Virginia; Charlottesville: 1987. Unpublished manuscript. [Google Scholar]
- Johnson HL, Nusbausm BJ, Bejarno A, Rosen TS. An ecological approach to development in children with prenatal drug exposure. American Journal of Orthopsychiatry. 1999;69:448–456. doi: 10.1037/h0080393. [DOI] [PubMed] [Google Scholar]
- Kamphaus RW, Frick PJ. Clinical assessment of child and adolescent personality and behavior. Needham Heights, MA: Allyn & Bacon; 1996. [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test. Circle Pines, MN: ACS; 1990. [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal JH, et al. Social supports and serotonin transporter gene moderate depression in maltreated children. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kettinger LA, Nair P, Schuler ME. Exposure to environmental risk factors and parenting attitudes among substance abusing women. American Journal of Drug and Alcohol Abuse. 2000;26:1–11. doi: 10.1081/ada-100100586. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. 2. New York: Wiley; 2006. pp. 739–795. [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Cushing G. Neighborhood influences and child development: A prospective study of substance abusers’ offspring. Developmental Psychology. 1999;11:763–784. doi: 10.1017/s095457949900231x. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cushing G, Merikangas K, Rounsaville BJ. Multiple jeopardy: Risk/protective factors among addicted mothers’ offspring. Developmental Psychology. 1998;11:117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, D’Avanzo K, Hites S. Parental substance abuse. Risks and resilience. Resilience and vulnerability. In: Luthar SS, editor. Adaptation in the context of adversities. New York: Cambridge University Press; 2003. pp. 104–129. [Google Scholar]
- Luthar SS, Latendresse SJ. Comparable “risks” at the socioeconomic status extremes: Pre-adolescents’ perceptions of parenting. Development and Pyschopathology. 2005;17:207–230. doi: 10.1017/s095457940505011x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Relational Psychotherapy Mothers’ Group: A developmentally informed intervention for at-risk mothers. Development and Pyschopathology. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE, Altomere M. Relational Psychotherapy Mothers Group: A randomized clinical trial for substance abusing mothers. Development and Psychopathology. 2007;19:243–261. doi: 10.1017/S0954579407070137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Zelazo LB. Research on resilience: An integrative review. In: Luthar SS, editor. Resilience and vulnerability: Adaptation in the context of childhood adversities. New York: Cambridge University Press; 2003. pp. 510–549. [Google Scholar]
- Lyons-Ruth K, Wolfe R, Lyubchik A. Depression and the parenting of young children: Making the case for early preventive mental health services. Harvard Review of Psychiatry. 2000;8:148–153. [PubMed] [Google Scholar]
- Malgady RG, Rogler LH, Tryon WW. Issues of validity in the Diagnostic Interview Schedule. Journal of Psychiatric Research. 1992;26:59–67. doi: 10.1016/0022-3956(92)90016-h. [DOI] [PubMed] [Google Scholar]
- Martin JL, Ford CB, Dyer-Friedman J, Tang J, Huffman LC. Patterns of agreement between parent and child ratings of emotional and behavioral problems in an outpatient clinical setting: When children endorse more problems. Journal of Developmental and Behavioral Pediatrics. 2004;25:150–155. doi: 10.1097/00004703-200406000-00002. [DOI] [PubMed] [Google Scholar]
- Mayes LC. Substance abuse and parenting. In: Bornstein MH, editor. Handbook of parenting: Applied and practical parenting. Vol. 4. Mahwah, NJ: Erlbaum; 1995. pp. 101–126. [Google Scholar]
- Mayes LC, Bornstein MH. The development of children exposed to cocaine. In: Luthar SS, Burack J, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 166–188. [Google Scholar]
- McClure EB, Brennan PA, Hammen C, Le Brocque RM. Parental anxiety disorders, child anxiety disorders, and the perceived parent-child relationship in an Australian high-risk sample. Journal of Abnormal Child Psychology. 2001;29:1–10. doi: 10.1023/a:1005260311313. [DOI] [PubMed] [Google Scholar]
- Myrick H, Kathleen B. Current review of the comorbity of affective, anxiety, and substance use disorders. Current Opinion in Psychiatry. 2003;16:261–270. [Google Scholar]
- NIMH DISC-IV Editorial Board. The NIMH Diagnostic Interview Schedule for Children. New York: 1995. Unpublished manuscript. [Google Scholar]
- Office of the Surgeon General. Mental health: A report of the Surgeon General. Washington, DC: Author; 1999. [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzeberg AF. Prevalence of anxiety disorders and their comorbidity with mood addictive disorders. British Journal of Psychiatry. 1998;34 (Suppl):24–28. [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavioral Assessment System for Children (BASC) Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Robins LN. Announcing DIS IV: A major revision. St. Louis, MO: Washington University School of Medicine; 1995. [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The Composite International Diagnostic Interview: An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1989;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Cicchetti D, Toth SL. Expressed emotion in multiple subsystems of the families of toddlers with depressed mothers. Development and Psychopathology. 2004;16:689–706. doi: 10.1017/s0954579404004730. [DOI] [PubMed] [Google Scholar]
- Rohner RP. Handbook for the study of parental acceptance and rejection theory. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Sameroff AJ. Developmental systems and psychopathology. Development and Psychopathology. 2000;12:297–312. doi: 10.1017/s0954579400003035. [DOI] [PubMed] [Google Scholar]
- Schneider KM, Phares V. Coping with parental loss because of termination of parental rights. Child Welfare. 2005;84:819–842. [PubMed] [Google Scholar]
- Shaffer D, Prudence MS, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2003 National Survey on Drug Use and Health. Washington, DC: US Department of Health and Human Services; 2003. [Google Scholar]
- Suchman NE, Luthar SS. The mediating role of parenting stress in methadone-maintained mothers’ parenting. Parenting: Science and Practice. 2001;1:285–315. doi: 10.1207/s15327922par0104_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Annie E. Casey Foundation. Kids count state-level data online. 2006 Retrieved February 2, 2006, from http://www.aecf.org/kidscount/sld/profile.jsp.
- Wakschlag LS, Hans SL. Relation of maternal responsiveness during infancy to the development of behavior problems in high-risk youths. Developmental Psychology. 1999;35:569–579. doi: 10.1037//0012-1649.35.2.569. [DOI] [PubMed] [Google Scholar]
- Weissman MM, McAvay G, Goldstein RB, Nunes EV, Verdeli H, Wickramaratne PJ. Risk/protective factors among addicted mothers’ offspring: A replication study. American Journal of Drug and Alcohol Abuse. 1999;25:661–679. doi: 10.1081/ada-100101885. [DOI] [PubMed] [Google Scholar]
- Wendorf CA. Primer on multiple regression coding: Common forms and the additional case of repeated contrasts. Understanding Statistics. 2004;3:47–57. [Google Scholar]
- Wilens TE, Biederman J, Kiely K, Bredin E, Spencer TJ. Pilot study of behavioral and emotional disturbance in the high-risk children of parents with opioid dependence. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:779–785. doi: 10.1097/00004583-199506000-00019. [DOI] [PubMed] [Google Scholar]


