Abstract
Runaway youth report a broader range and higher severity of substance-related, mental health and family problems relative to non-runaway youth. Most studies to date have collected self-report data on the family and social history; virtually no research has examined treatment effectiveness with this population. This study is a treatment development project in which 124 runaway youth were randomly assigned to 1) Ecologically-Based Family Therapy (EBFT) or 2) Service as Usual (SAU) through a shelter. Youth completed an intake, posttreatment, 6 and 12 month follow-up assessment. Youth assigned to EBFT reported greater reductions in overall substance abuse compared to youth assigned to SAU while other problem areas improved in both conditions. Findings suggest that EBFT is an efficacious intervention for this relatively severe population of youth.
Ecologically-Based Family Therapy Outcome with Substance Abusing Runaway Adolescents
This paper reports findings from the first randomized clinical trial examining treatment outcome for family therapy with substance abusing runaway youth. Overall, many researchers have concluded that family-based intervention for substance abuse is an effective therapeutic modality (Craig, 1993; Gurman, Kniskern, & Pinsof, 1986; Stanton & Shadish, 1997). It has been recognized as particularly effective with adolescent substance abusers and behavior problem youth (Bry, 1988; Joanning, Thomas, Quinn & Millen, 1992; Liddle, Dakof, & Diamond, 1991; Szapocznik, Kurtines, Foot, Perez-Vidal & Hervis, 1983; Szapocznik, Kurtines, Santisteban, & Rio, 1990). Reviews of formal clinical trials of family-based treatments consistently found that more drug-abusing adolescents enter, engage in, and remain in family therapy longer than in other modalities, and family therapy produces significant reductions in pre to posttreatment substance use (Liddle & Dakoff; 1995; Ozechowski & Liddle, 2000; Stanton & Shadish, 1997; Waldron, 1997).
Fifteen randomized trials have evaluated substance use outcomes for adolescents and their families (for reviews: Kaminer & Slesnick, in press; Ozechowski & Liddle, 2000; Stanton & Shadish, 1997). All adolescent family therapy studies showed significant pre to posttreatment reductions in substance use for the family-based intervention utilized, with eight of the twelve studies that used a non-family therapy control showing superior effects for those youth assigned to family therapy. In addition to substance use, recent studies have shown that family therapy positively impacts school performance and attendance, family functioning, delinquency and aggression (Liddle et al. 2001; Henggeler, Clingempeel, & Brondino, 2002; Henggeler, Pickrel & Brondino, 1999; Santisteban, Perez-Vidal, Coatsworth, & Kurtines, 2003).
Family Preservation Model
Ecologically-Based Family Therapy (EBFT), evaluated in this study, is based upon the Homebuilders family preservation model. In the early 1980s, a variety of family-based prevention and reunification programs called home-based, family preservation or family-based services were utilized in several states (Nelson & Landsman, 1992). The prototypical intensive family preservation service program, Homebuilders, was started by clinical psychologists in 1974 to provide an alternative to foster care and institutional placement of children in Washington state (Kinney, Haapala, Booth, & Leavitt, 1990). The Homebuilders family preservation services are based on crisis intervention theory which postulates that families are most open to change when they are faced with a crisis, and their normal modes of coping no longer work. The program was structured to provide immediate, intensive services over a brief time period. In most cases, the crisis is precipitated by the threat of removal of a child by Child Protective Services, a child’s running away, or a child’s ejection from the family (Barth, 1990; Kinney, Haapala, Madsen, & Fleming, 1991). In this model, families are seen by a single counselor and services include a wide range of behavioral, cognitive, and environmental interventions, depending on the family’s needs. The program does not require all family members to be present or involved, and both family and individual sessions are used.
Numerous studies have evaluated intensive family preservation services, but most have lacked a comparison group and limited their measures of change to whether out-of-home placement occurred (Nelson, 1994). In general, Homebuilders programs have found placement rates of 9% to 38% compared to 72% to 100% in comparison groups for samples of youth in juvenile justice, child welfare and mental health programs (Kinney et al., 1991; Nelson & Landsman, 1992). In a more controlled study, Feldman (1991) found that those in the family preservation program, compared to those in the service as usual control groups, showed significant improvement in family functioning, parental functioning and child performance at post-treatment.
Multisystemic Treatment Approach
The family preservation model has the same conceptual base as the multisystemic treatment model where severe behavior problems associated with runaway youth are considered to be multiply determined and best addressed in multiple areas (Jessor & Jessor, 1977; Pickrel & Henggeler, 1996). Whereas traditional forms of family therapy focus on the parent-adolescent interaction, intervention involving meeting with individuals alone, adolescent and parent together, extended family as well as intervening at the extrafamilial level are viewed as integral to change in home-based, multisystemic approaches (Henggeler et al., 2002; Liddle 2001). Treatment is directed toward assessing these multiple influences and intervening so that change is supported throughout all the systems affecting the problem behavior, including the intrapersonal system of the individual adolescent, the interpersonal systems of the family and peers, and the extrapersonal systems of the shelter, juvenile justice system, school and the community.
Risks Faced by Runaway Youth
Runaway youth are at high risk for health and psychological problems, highlighting the need for research efforts focused on intervention. These youth often have significant substance abuse problems and high levels of family conflict and chaos. In a recent review, Robertson and Toro (1999) report findings that 48% of a street sample of homeless youth met diagnostic criteria for alcohol disorder, and 39% met criteria for other drug disorders. In comparing a New York City sample of runaways to adolescents in general (using NIDA data, 1991), Koopman, Rosario, and Rotheram-Borus (1994) report that runaways are three times more likely to use marijuana (43% vs. 15%), seven times more likely to use crack/cocaine (19% vs. 2.6%), five times more likely to use hallucinogens (14% vs. 3.3%), and four times more likely to use heroin (3% vs. 0.7%). Studies document high rates of physical and sexual abuse (16–60%), depression, teen pregnancy, and prostitution (Johnson et al., 1996; Zimet et al., 1995). Several studies report high rates of comorbid diagnoses among runaway and homeless youth (Schweitzer & Hier, 1993; Unger, Kipke, Simon, Montgomery, & Johnson, 1997; Warhiet & Biagora, 1991).
Published interventions with runaway youth are sparse. To date, we are only aware of empirical evaluation of an HIV intervention with runaway, shelter residing youth (Rotheram-Borus, Koopman, Haignere, & Davies, 1991) and a case management intervention with street living youth (Cauce et al., 1994). No published study has examined outcome of a comprehensive substance use and mental health treatment intervention for youth residing at a runaway shelter. Because research suggests that family disturbance is highly correlated to the act of running away (Finkelhor, Hotaling, & Sedlak, 1990; Kufeldt, Durieux, Nimmo, & McDonald, 1992) family therapy is identified as the most important first treatment to evaluate with this population. Thus, this study expected that home-based Ecologically-Based Family Therapy (EBFT) would positively impact substance use, HIV risk, psychological and family functioning and diagnostic status over time compared to Service as Usual (SAU) through the runaway shelter.
Methods
Participants
Referrals to the study were obtained through two local runaway shelters in Albuquerque, NM who serve youth between the ages of 12–17. Inclusion criteria for adolescents were: youth between the ages of 12 to 17, residing within a 60-mile radius of the research site, youth has the legal option of returning to a home situation (including foster or other family member) and reports at least ten days of substance use in the past 90 days or meets DSM-IV criteria for a Psychoactive Substance Use Disorders. Also, youth must have had at least one parent, or surrogate parent willing to participate in therapy.
Exclusion criteria were: evidence that alcohol is the primary drug of abuse, evidence of unremitted psychosis or other condition which would impair his or her ability to understand and participate in the intervention or to consent for research participation. Teens without the option of returning home were not included in the study as their home situation would be unclear and an identified family for therapy would not be established.
Procedure
Adolescents referred by the shelter were interviewed in-person by a project research assistant (R.A.). Adolescents passing quick-screen criteria continued with the intake or were scheduled for an intake within 24 hours. The intake evaluation, conducted at the shelter, also by an R.A., began with a review of the nature and conditions of the study, a formal review of the elements of informed consent, and signing of the consent statement. Effort was focused on developing and building trust and interest in the project. After the adolescent consented to participate in the study, the adolescent’s parent or legal guardian was contacted to engage into the study and also signed an informed consent statement upon their agreement. Individuals other than the parent or guardian (e.g. siblings) who were asked to participate in the family therapy condition signed treatment consent forms at the first therapy session, and were not contacted before the randomization procedure. Upon parental consent, the interviewer proceeded to administer the Computerized Diagnostic Interview Schedule for Children (CDISC, Shaffer, 1992), sections on drugs, alcohol, and psychosis to determine formal eligibility of the adolescent. Those not passing quick-screen or inclusion criteria during the diagnostic screening continued with treatment as usual through the shelter. Those meeting the criteria for participation in the study, continued with the assessment battery. Following completion of the assessment battery all youth were randomly assigned to EBFT (N = 65) or SAU through the shelter (N = 59).
Randomization procedures
Urn randomization has been used successfully in clinical trials ensuring pretreatment group equivalence (e.g., Project MATCH, 1993). Non-equivalent groups can emerge by chance especially given small samples. The urn procedure retains random allocation and balances groups on a priori continuous and categorical variables. The relative probabilities of assignment to treatment groups (urns) are computer adjusted based on previous randomizations to reduce the risk of nonequivalent groups. The variables included in the urn were: gender, age, primary drug of abuse, ethnicity, psychiatric severity, and number of previous runaway episodes.
Assessment
The adolescent was the only data source for all cases, as an entire family assessment was beyond the scope of this project. The pretreatment and follow-up evaluation for adolescents included a core of the same set of measures at each measurement point so that pretreatment assessments were comparable to later assessments. Five domains of interest were assessed, as it was expected that these areas would be positively influenced by the therapeutic intervention: Substance use, adolescent psychological functioning, family functioning, HIV risk behaviors, and diagnostic status. The pretreatment and follow-up assessments, including the diagnostic battery, required approximately 3 hours to complete. Assistance in completing forms was provided as needed. Participants were given the option of completing the assessment in one session or in two shorter sessions on separate days.
Three posttreatment follow-up points, at posttreatment (3 months post-intake), 6 and 12 months were chosen since more data points give a clearer picture of the client’s substance use patterns after treatment. Adolescents were paid $25 at the completion of the pretreatment evaluation and at the 3 month follow-up, and were paid $50 at the 6 and 12 month follow-ups. Adolescents missing follow-up assessment sessions were rescheduled. If clients were unable to conduct an in-person follow-up appointment at the research site, effort was made to arrange for transportation to the site. Otherwise, a home visit was arranged. We were relatively successful in tracking youth for their follow-up assessment. In the EBFT condition, follow-up rates were as follows: 60/65 (92%) at posttreatment, 58/65 (89%) at 6 months, and 58/65 (89%) at 12 months. In the SAU condition the rates were somewhat lower: 48/59 (81%) at posttreatment, 49/59 (83%) at 6 months, and 52/59 (88%) at 12 months. Attrition did not differ by treatment modality or time. The assessment battery included the measures described below.
Materials
A demographic questionnaire assessing a set of core variables used to characterize and compare samples included in the study was administered by the examiner. These demographic items include age, gender, self-identified ethnicity, parent and sibling information, education, income sources, number of previous runaway episodes, and homeless and victimization experiences.
Measures of Substance Use
The Form 90, developed for NIAAA funded Project Match (Miller & Delboca, 1994), was the primary measure of quantity and frequency of drug and alcohol use. This measure uses a combination of the timeline follow-back method (Sobell & Sobell, 1992) and grid averaging (Miller & Marlatt, 1984). Total number of days of substance use vary by client as the Form 90 instrument assesses substance use in the 90 days prior to the last alcohol or drug use up until the day prior to the assessment interview. Thus, alcohol/drug use days are reported as “percentage days of use.” This tool has shown excellent test-retest reliability for indices of drug use in major categories for adults (Tonigan, Miller, & Brown, 1997; Westerberg, Tonigan & Miller, 1998) and runaway adolescents (Slesnick & Tonigan, in press), with kappas for different drug classes ranging from .74 to .95.
As further validation of self-reported drug use, urine toxicology screens were collected for adolescents at pretreatment and the first post-treatment follow-up point. It was beyond the financial scope of this study to collect urine samples at each follow-up point. To address problem consequences associated with drug use, the POSIT (Rahdert, 1991) was utilized. Support for the psychometric properties of the POSIT, including convergent and discriminant validity, has been reported by McLaney, Delboca and Babor (1994).
HIV/AIDS Behaviors
The Health Risk Questionnaire is a modified version of the 1989 edition of the CDC Health Risk Survey (HRS; Kann, Nelson, Jones, & Kolbe 1989) and of the Homeless Youth Questionnaire (Johnson, Aschkenasy, Herbers, & Gillenwater, 1996). This instrument provides both HIV/AIDS knowledge and risk scores. Ashworth, Durant, Newman and Gaillard (1992) found pre-post test reliabilities of .76 and .81, respectively for items that address knowledge and attitudes about HIV.
Psychological Functioning
The Youth Self-Report of the Child Behavior Checklist (YSR; Achenbach & Edelbrock, 1982) elicits youth’s self-reported behavior across a wide range of problem areas (Achenbach & Edelbrock, 1982). The Beck Depression Inventory (BDI, Beck, Ward, Mendelson, Mock & Erlbaugh, 1961) and the National Youth Survey Delinquency Scale (NYSDS; Elliot, Huizina, & Ageton, 1985) were utilized to assess depression and self-reported delinquent behaviors.
Family Functioning
The Family Environment Scale (FES; Moos & Moos, 1986) was used to assess perceptions of the family environment. The Conflict Tactic Scale (CTS; Straus, 1979) was implemented to measure the occurrence of several methods of conflict resolution used by the youth and primary caretaker. CTS is a widely used measure of conflict resolution tactics (Wolfe, Toro, & McCaskill, 1999). The Parental Bonding Instrument (PBI, Parker, Tupling & Brown, 1979) is a measure of two dimensions of parent child relationship: perceived parental care versus rejection, and control versus autonomy.
Diagnostic Status
The Computerized Diagnostic Interview Schedule for Children (CDISC, Shaffer, 1992), is a computerized structured interview containing 263 items pertinent to a comprehensive psychiatric diagnostic interview based upon DSM-IV criteria.
Treatment
Therapist Training and Supervision
Several therapists conducted the family therapy but three therapists conducted therapy with the majority of the youth (80%). Therapists were primarily female (one male), master’s level licensed counselors with between two to five years experience in the field. All therapists were trained and experienced in substance abuse treatment using cognitive-behavioral and behavioral family systems approaches. Therapist differences were investigated between these three therapists. No differences were found for the number of completed treatment sessions (p = .58). Further, no overall main effects of therapist or interactions between therapist and time were found for substance use or any other variables of interest (all p’s > .20; using repeated measures ANOVAs).
As this project entailed the development and refinement of the family-based multisystemic treatment procedure, supervision and therapy modification meetings were ongoing. Audiotaped recordings of all therapy sessions were used for two purposes: treatment adherence checks and supervision. The therapists and Project Director met at least weekly throughout the treatment provision phase of the project. In these meetings, selected portions of audiotapes were reviewed, feedback was provided and problems were discussed. These meetings also provided the context to gather information for improving and modifying the therapy manual on an ongoing basis.
Ecologically-Based Family Therapy (EBFT)
The EBFT manual (Slesnick, 2003) was developed during the project and is divided into four sections. The engagement procedure utilized with these youth and families is described in section one. Section two identifies common themes to the therapy with runaway youth and families, and organizes an approach to effectively intervene. Section three provides a four session HIV prevention intervention developed for the runaway youth and to be applied in individual meetings. The final section, Section four, outlines the sequence of clinical tasks for the therapy sessions. Preliminary intervention with the family consists of preparing parents and adolescents to come together to talk about issues that may have initiated the runaway episode. Sessions with parents alone utilize similar motivation and engagement procedures as those used with the adolescent. The sessions help develop parents’ readiness to develop a new kind of relationship with their youth and change parenting strategies. The therapist works towards fostering competency in parenting by supporting consistent and age-appropriate limit-setting and monitoring of activities. This may be especially salient for parents of runaway youth as they may have lost confidence in their ability to influence the adolescent.
Following completion of the individual sessions, family members are brought together to target specific dysfunctional interactions which correspond to the development and continuation of problem behaviors. Techniques utilized in these sessions include communication and problem-solving skills training where youth and parents become more confident and competent in their ability to communicate needs and expectations. Unlike the traditional family intervention, multisystemic intervention does not assume that changes in the parent-adolescent relationship is necessarily sufficient to alter drug and alcohol using behavior (Schmidt, Liddle, & Dakof, 1996). Hence, a framework is created in both the individual and family sessions for dealing with substance use in an overt way. The next level of intervention involves individuals who play a key role in the life of the adolescent (e.g., siblings, extended family members, etc.) who are encouraged to participate in family sessions. Sessions 14 and 15 focuses on issues of termination. Throughout the treatment phase, family members may need assistance obtaining community services such as medical care, job training, or self-help programs. Additionally, counselors may routinely meet with school personnel and probation officers. Overall, 29/65 (45%) of the youth and families assigned to EBFT completed all 15 sessions and 50/65 (77%) completed 5 or more sessions. The following reasons were documented for the 15 youth and families who completed 4 or fewer sessions: 1) youth was jailed or sent to residential treatment (N = 4), 2) youth moved to another city (N = 2), 3) youth went on the run and was not found until after the treatment window passed (N = 3), or 4) the family was unable to be engaged back into treatment (N = 6).
Service as Usual
Adolescents who were not randomized into the family therapy condition were assigned to SAU through the shelter. Typically, adolescents remained in the shelter system for a short time, 5 to 30 days. Adolescents in our study were in the shelter an average of 9 (SD = 17.5) days at the pretreatment assessment, and 14 (SD = 20.9) days at the posttreatment assessment, which did not differ between treatment groups. Some adolescents received treatment outside our program. At pretreatment, the average number of outside (non-EBFT) treatment sessions was 4 (SD = 13.6), which did not differ between treatment groups. However, at posttreatment the average number of outside treatment sessions was 3 (SD = 6.0), which did differ between groups; SAU received more a greater percentage of days of outside treatment (4%) than EBFT did (2%, F (1, 106) = 4.08, p <.05). Although it is likely that many of these reported outside treatment sessions were with shelter staff, the assessment did not differentiate which treatments were with shelter staff and which treatments were not with shelter staff. Counselors on staff and shelter workers were available for talking with the youth. In a report of the shelter mission, it is stated, “Our task as youth services providers is not correcting the ‘pathologies’ of troubled youth, but rather as providing for the successive ‘needs’ of young people.” The shelters primarily provided food, shelter, clothing, crisis intervention and assisted with placement.
Statistical analyses
Initial analysis were conducted to examine that the distributional characteristics of the variables of interest. The only variables that had distributional problems were from the National Youth Survey Delinquency Scale (NYSDS). To adjust for these problems, five cases were excluded that had scores greater than 4 standard deviations away from the mean for any of the 4 assessment periods. Any analyses reported with the NYSDS excluded these outliers. All other analyses included all clients with complete data.
To test for potential baseline differences between modality groups, t-tests and chi-square analyses were used. To test for the treatment differences, pre to post treatment analyses were conducted on all clients on the main variables of interest. Repeated measures analyses were conducted with treatment modality as the between-subjects factor, and number of treatment sessions as a covariate. First, intent to treat analyses were completed with all clients on all the main variables, then the treated vs. untreated groups were analyzed, using number of treatment sessions as a covariate.
Results
Sample Characteristics
Of the youth approached at the shelter, 98% agreed to participate in the program (2 refusals). The average age of youth was 14.8 years, and the sample includes 73 females (51 males). Reported adolescent ethnicity included Hispanic (N = 51), Anglo (N = 46), African American (N = 9), Native American (N = 5) and “other” (N = 13). Intravenous drug use was reported by 10.6% (N = 11) of the youth, and average number of reported runaway episodes in the last 90 days was 3.1. Overall, youth reported using alcohol or drugs on 50% of the assessments days. As this project only engaged those youth with a primary drug problem, the percent days of alcohol use in the assessment period was relatively low (6% days). Most often used substances are described in Table 1. Moreover, 31% of youth reported sexual abuse, 55% reported physical abuse and 21% reported both physical and sexual abuse. The majority (74.2%) of the youth met DSM IV criteria for one or more Axis I diagnoses other than substance abuse or dependence, and 37% of youth reported at least one suicide attempt. Only 48% of youth reported not being currently enrolled in school. Average BDI score (13.4) was in the mild to moderate depression range. Please see Table 2 for a summary of sample characteristics.
Table 1.
Means and Standard deviations of the most often used substances at pretreatment.
| Substance Used | Average Percent Days Use (SD) |
|---|---|
| Any drug use (not alcohol or tobacco) | 50% (34.4) |
| Alcohol | 6% (10.8) |
| Tobacco | 61% (44.3) |
| Marijuana | 44% (36.0) |
| Cocaine | 6% (17.6) |
| Opiates | 2% (10.12) |
Table 2.
Demographic characteristics by treatment modality at pretreatment.
| Variable | EBFT | SAU | Total | |
|---|---|---|---|---|
| Age | 14.8 (1.5) | 14.9 (1.3) | 14.9 (1.4) | |
| Gender (#, % Male) | 30, 46% | 21, 36% | 51, 41% | |
| Ethnicity (#,%) | Anglo | 25, 39% | 21, 36% | 46. 37% |
| Hispanic | 25, 39% | 26, 44% | 51, 42% | |
| Native Am | 4, 6% | 1, 2% | 5, 4% | |
| African Am | 6, 9% | 3, 5% | 9, 7% | |
| Other | 4, 6% | 8, 14% | 12, 10% | |
| # Lifetime Runs | 2.6 (3.9) | 3.8 (6.9) | 3.1 (5.0) | |
| # Arrests | 1.5 (2.2) | 2.3 (4.9) | 1.9 (3.7) | |
| Currently enrolled in school (#, %) | 34, 52% | 30, 51% | 64, 52% | |
| Family income | $27,972 (32,890) | $26,734 (29,321) | $27,384 (31,123) | |
Note. Means and Standard deviations unless otherwise specified.
Pretreatment Differences
Gender differences
Males and females differed significantly in the percentage who reported sexual abuse (χ2 = 21.19, p < .001), but did not differ in physical abuse (see Table 3). Males and females also did not differ in their report of at least one previous suicide attempt.
Table 3.
Number and percentage of adolescents reporting sexual abuse, physical abuse and suicide attempts by gender.
| Male (N = 51) | Female (N =73) | Total (N = 124) | ||
|---|---|---|---|---|
| Ever Sexually Abused?* | No | 47 (92%) | 39 (53%) | 86 (69%) |
| Yes | 4 (8%) | 34 (47%) | 38 (31%) | |
|
| ||||
| Ever Physically Abused? | No | 28 (55%) | 28 (38%) | 56 (45%) |
| Yes | 23 (45%) | 45 (62%) | 68 (55%) | |
|
| ||||
| Attempt Suicide Ever? | No | 37 (73%) | 41 (56%) | 78 (63%) |
| Yes | 14 (27%) | 32 (44%) | 46 (37%) | |
Note. Significant difference.
A number of gender differences were found at pretreatment for the main variables of interest. Females reported higher conflict and lower cohesion in their family. Further, they reported higher total conflict tactics scores for both themselves and their primary caretaker, which further revealed itself in the aggression subscale of the CTS with females with higher aggression scores. Females also had higher internalizing problems from the Youth Self Report. Further, females reported lower parental care on the PBI and scored almost twice as high on the Beck Depression Inventory. Females reported higher drug/alcohol problem consequences than males, but did not report greater use. Females had higher HIV risk scores, but did not differ in their HIV knowledge from males. No gender differences in delinquency from either the NYSDS or the YSR were found. See Table 4 for means, standard deviations, and t-values.
Table 4.
Means and standard deviations for the main variables by gender.
| Variable | Male | Female | t |
|---|---|---|---|
| Drug Use: | |||
| Percentage days of use | 51 % (35) | 46% (35) | 0.73 |
| # of categories of drugs used | 2.92 (1.38) | 3.22 (1.52) | −1.11 |
| # of problem consequences (POSIT) | 4.58 (3.40) | 6.67 (4.58) | −2.75* |
|
| |||
| HIV: | |||
| Knowledge (out of 17) | 14.76 (1.78) | 14.34 (2.14) | 1.16 |
| high-risk behaviors (out of 7) | 0.98 (0.79) | 1.70 (1.38) | −3.35* |
|
| |||
| Psychological Functioning: | |||
| number of psychiatric diagnoses | 0.78 (1.03) | 1.27 (1.61) | −1.92 |
| Depression from the BDI | 8.69 (7.91) | 16.63 (11.56) | −4.26* |
| internalization problems | 14.39 (7.61) | 22.36 (11.76) | −4.25* |
| externalizing problems | 25.39 (8.15) | 26.88 (11.74) | −0.78 |
| delinquent behaviors (total) | 177.79 (312.16) | 224.44 (364.91) | 0.78 |
|
| |||
| Family Functioning: | |||
| verbal aggression - youth (CTS) | 0.37 (0.24) | 0.50 (0.25) | −2.91* |
| family violence - youth (CTS) | 0.07 (0.08) | 0.09 (0.10) | −0.96 |
| family cohesion | 4.61 (2.62) | 3.34 (2.29) | 2.18* |
| family conflict | 4.71 (2.31) | 5.90 (2.50) | −2.70* |
| parental care | 22.41 (8.67) | 18.47 (7.64) | −2.66* |
| parental overprotectiveness | 18.82 (8.63) | 20.60 (9.00) | −1.10 |
Note. Significant gender differences (p < .05)
Ethnicity differences
Since the ethnic distribution was not equal across all ethnic categories, only Anglo and Hispanic youth were used in tests for group differences, however all ethnicities are represented in Table 5. Anglo and Hispanic youth reported no differences in sexual or physical abuse reports, however, Anglo youth were more likely to report at least one previous suicide attempt as compared to Hispanic youth (χ2 = 4.30, p < .05). Hispanic youth were about a year older than Anglo youth (t (95) = −2.04, p < .05). Few differences were found between Anglo and Hispanic youth in the main variables (see Table 6). Anglo youth had greater HIV risk knowledge than Hispanic youth (t (95) = −2.22, p <.05). No other ethnicity differences were found.
Table 5.
Number and percentage of adolescents reporting sexual abuse, physical abuse, and suicide attempts by ethnicity.
| Hispanic (N = 51) | Anglo (N = 46) | African Am. (N = 9) | Native Am. (N = 5) | Other (N = 13) | ||
|---|---|---|---|---|---|---|
| Ever Sexually Abused? | No | 35 (69%) | 30 (65%) | 6 (67%) | 5 (100%) | 10 (77%) |
| Yes | 16 (31%) | 16 (35%) | 3 (33%) | 0 (0%) | 3 (23%) | |
|
| ||||||
| Ever Physically Abused? | No | 21 (41%) | 21 (46%) | 5 (56%) | 2 (40%) | 7 (54%) |
| Yes | 30 (59%) | 25 (54%) | 4 (44%) | 3 (60%) | 6 (46%) | |
|
| ||||||
| Attempt Suicide Ever? | No | 37 (73%) | 24 (52%) | 5 (56%) | 4 (80%) | 8 (62%) |
| Yes | 14 (27%) | 22 (48%) | 4 (44%) | 1 (20%) | 5 (38%) | |
Table 6.
Differences between Anglo and Hispanic adolescents on the main variables.
| Variable | Anglo (N = 46) | Hispanic (N = 51) |
|---|---|---|
| Drug Use: | ||
| Percentage days of use | 48% (37) | 47% (34) |
| # of categories of drugs used in past 90 days | 3.41 (1.55) | 2.96 (1.48) |
| number of problem consequences (POSIT) | 6.14 (4.59) | 5.13 (3.95) |
|
| ||
| HIV: | ||
| Knowledge (out of 17) * | 14.33 (2.07) | 15.13 (1.36) |
| high-risk behaviors (out of 7) | 1.48 (1.12) | 1.46 (1.46) |
|
| ||
| Psychological Functioning: | ||
| number of psychiatric diagnoses | 1.61 (0.96) | 1.63 (0.92) |
| Depression from the BDI | 14.92 (12.08) | 12.43 (10.22) |
| internalization problems | 20.10 (11.65) | 18.48 (11.22) |
| externalizing problems | 24.84 (10.00) | 28.85 (10.40) |
| delinquent behaviors (total) | 173.45 (347.38) | 305.43 (466.42) |
|
| ||
| Family Functioning: | ||
| verbal aggression - youth (CTS) | 0.42 (0.24) | 0.48 (0.25) |
| family violence - youth (CTS) | 0.07 (0.09) | 0.09 (0.10) |
| family cohesion | 3.90 (2.41) | 3.69 (2.64) |
| family conflict | 5.65 (2.43) | 5.67 (2.60) |
| parental care | 18.82 (7.82) | 19.67 (8.60) |
| parental overprotectiveness | 20.75 (8.76) | 20.39 (8.81) |
Note. Significant ethnicity differences.
Treatment differences
No differences were found for any of the main variables (substance use, HIV risk, psychological functioning, or family functioning), indicating that the treatment groups were relatively equal in baseline performance (all p’s > .10).
Correlation with Urine Screens
Urine screens were conducted at pretreatment and posttreatment. Cannabis was the drug that was most commonly found on the urine screens. All other drugs were found in 4 or less youths’ drug screens. Point-biseral correlations were conducted between percentage days use of marijuana and the drug screen (positive or negative). Significant positive correlations were found both at pretreatment (r = .49, p < .001) and posttreatment (r = .62, p < .001) indicating that the adolescent’s self-reported substance use is largely valid.
Pre to Post Treatment Differences
Intent to treat analyses
For the intent to treat analyses, repeated measures analyses were conducted with treatment modality as the between-subjects factor, and number of treatment sessions as a covariate. The key effect sought was an interaction between time and modality. Fifty-three subjects assigned to EBFT competed all 4 assessment points, and 44 SAU subjects completed all 4 assessments points, and were included in the intent to treat analyses. No significant interactions were found for any of the main variables of interest.
Treated analyses
The same analyses were completed with the clients that received a dose of treatment (defined as more than 4 treatment sessions completed; EBFT N = 42; SAU N = 44). Interactions were found in percentage days of overall substance use (tobacco use not included; F (3,81) = 2.91, p < .05; η2 = .10; see Figure 1 for amount of change), for use excluding tobacco and alcohol (F (3,81) = 2.89, p < .05; η2 = .10), and for percentage days of marijuana use (F (3,81) = 2.84, p < .05; η2 = .10). The same pattern is found for all three of these measures of use.
Figure 1.
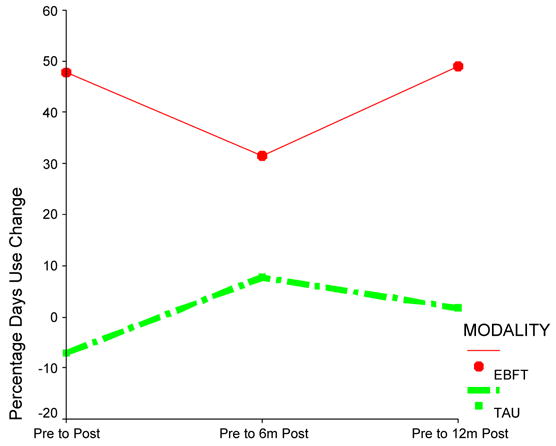
Percentage change in days use of all drug classes (except tobacco) from pretreatment levels to each posttreatment assessment point by treatment modality.
Overall, both groups get better on many different areas of functioning (main effect of time), but few interactions are found between the two groups. Table 7 shows the means and standard deviations for each of the main variable at each of the assessment points.
Table 7.
Means and standard deviations for the main variables of interest over time.
| Variables | Pretreatment | Posttreatment | 6 months posttreatment | 12 months posttreatment |
|---|---|---|---|---|
| Drug Use: | ||||
| percentage days of use* | 50% (33.91) | 31% (35.25) | 31% (36.29) | 25% (32.08) |
| # of categories of drugs used in past 90 days * | 3.04 (1.49) | 2.27 (1.70) | 2.53 (1.87) | 1.96 (1.61) |
| number of problem consequences (POSIT) * | 5.63 (4.11) | 4.31 (3.63) | 3.42 (3.56) | 2.80 (3.31) |
|
| ||||
| HIV: | ||||
| knowledge (out of 17) * | 14.54 (2.03) | 15.21 (1.67) | 15.49 (1.41) | 15.51 (1.80) |
| high-risk behaviors (out of 7) | 1.43 (1.24) | 1.36 (1.30) | 1.33 (1.10) | 1.53 (1.27) |
|
| ||||
| Psychological functioning: | ||||
| # of psychiatric dx * | 1.55 (0.97) | 1.32 (1.31) | 1.03 (1.16) | 0.76 (1.13) |
| depression from the BDI * | 13.21 (10.33) | 8.01 (8.00) | 6.76 (7.28) | 5.48 (6.38) |
| internalization problems * | 19.47 (11.01) | 15.89 (9.25) | 14.11 (8.42) | 12.59 (7.59) |
| externalizing problems * | 26.48 (10.13) | 22.78 (9.88) | 20.03 (9.67) | 17.69 (9.03) |
| delinquent behaviors (total) * | 255.9 (463.5) | 93.27 (486.7) | 56.01 (208.1) | 37.27 (116.8) |
|
| ||||
| Family functioning: | ||||
| verbal aggression - youth (CTS)* | 0.46 (0.25) | 0.27 (0.25) | 0.26 (0.24) | 0.19 (0.22) |
| family violence - youth (CTS)* | 0.08 (0.09) | 0.04 (0.11) | 0.03 (0.06) | 0.03 (0.07) |
| family cohesion * | 4.06 (2.41) | 5.21 (2.63) | 5.31 (2.53) | 6.15 (2.36) |
| family conflict * | 5.45 (2.47) | 4.27 (2.54) | 3.76 (2.61) | 3.48 (2.59) |
| parental care * | 19.91 (8.23) | 23.51 (8.40) | 23.65 (8.43) | 26.91 (7.69) |
| parental overprotectiveness * | 19.67 (9.18) | 18.09 (9.00) | 17.74 (9.39) | 14.68 (8.94) |
Note. Significant time main effects.
Treatment interactions by gender
No interactions of gender and modality were found in the intent to treat repeated measures analyses of main variables, or in the treated analyses.
Treatment interactions by ethnicity
Only Anglo and Hispanic ethnicities were used in the following analyses, since these were the two ethnicities represented by the majority of the clients. Intent to treat repeated measures analyses with ethnicity as a between subjects variable did not reveal any interactions of group over time, nor any overall ethnicity differences. Treated analyses were conducted with ethnicity and modality as between subjects variables. A three way interaction between time, modality and ethnicity was found for the number of Axis I diagnoses (F (3,64) = 3.09, p < .05). Figure 2 shows the different patterns demonstrated by Hispanic and Anglo youth in the two modalities.
Figure 2.
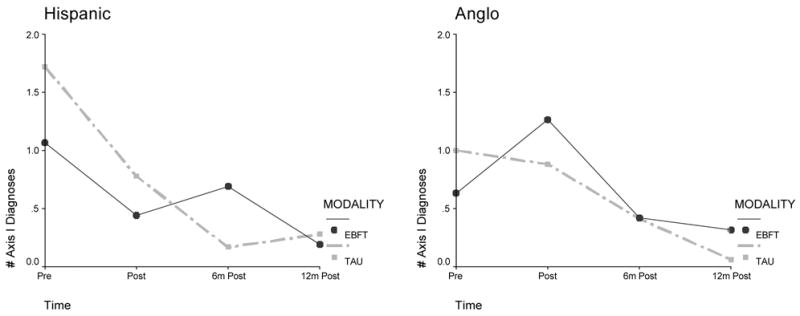
Interaction between ethnicity, treatment modality, and time for the number of Axis I diagnoses.
Treatment interactions with age
A median split of age was conducted so that the younger group’s mean age was 13 and the older group’s mean age was 16. Repeated measures analyses were conducted using this age variable and modality as between subjects variables on the main variables of interest. No interactions of age, modality and time were found for either intent to treat analyses or treated analyses.
Treatment interactions with abuse
The measures of sexual and physical abuse were combined to create a measure that evaluated whether adolescents reported neither sexual or physical abuse (coded 0), either sexual or physical abuse (coded 1), and both sexual and physical abuse (coded 2). This measure was used in the repeated measures analyses as a between subjects’ variable along with modality. Two measures showed a three way interaction with time, modality, and abuse: problem consequences of use (F (6, 180) = 2.85, p < .05) and number of drugs used in the past 90 days (F (6, 176) = 2.25, p < .05). From these analyses, both variables indicate that youth with both sexual and physical abuse do better with EBFT than with TAU (less problem consequences, fewer drugs used), and youth with neither sexual or physical abuse do not differ between modalities (see Figure 3).
Figure 3.
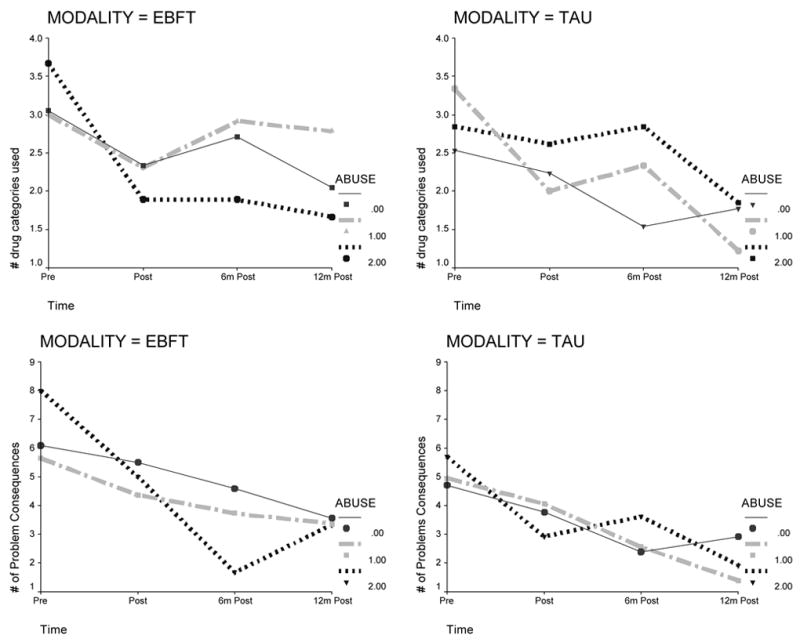
Interaction between abuse, treatment modality, and time for number of drug categories used and number of problem consequences reported (POSIT).
Discussion
This treatment development project examined outcome of Ecologically-Based Family Therapy (EBFT) versus Service as Usual (SAU) for substance abusing runaway youth residing at a local runaway shelter. Overall, youth receiving EBFT showed a greater reduction in overall substance use compared to those assigned to SAU. Gender and ethnicity did not differentially influence outcome. However, an interaction was found between abuse history, time and modality. Among youth who reported physical and sexual abuse, those assigned to EBFT reported fewer problem consequences and reported a reduction in the number of different drugs used over time compared to those in SAU. Both EBFT and SAU showed significant improvements over time on measures of psychological and family functioning and HIV knowledge. Overall, youth maintained the same relatively low levels of high-risk behaviors throughout the follow-up period with an average of 1.4 out of 7 potential high risk behaviors.
The findings showed several pretreatment differences between males and females. Females reported more verbal aggression in problem resolution tasks compared to males. This finding is similar to the adult marital and family research which has shown that women express more negative affect (hostility and aggression) during problem resolution communication tasks (e.g., Flaherty, & Richman, 1989; Gruen et al., 1994). The finding that females reported more family problems including less family cohesion, parental care and greater family conflict at pretreatment compared to males is perplexing, as these findings were unrelated to reported physical and sexual abuse. Possibly, the findings are a result of reporting bias in which females report the family environment as more negative than males. Alternatively, since our findings show that females are behaving similarly to males (delinquency, externalizing behaviors), it is possible that parents have less tolerance for female misbehavior. Without corroborating reports from other family members, we cannot evaluate these hypotheses.
Implications
These findings have several implications. First, the findings suggest that family therapy with this subpopulation of substance abusing adolescents is an effective treatment modality. Runaway youth and their parents have been described as difficult to engage and maintain in treatment (Morrissette, 1992; Smart & Ogborne, 1994) and have been considered “difficult to work with” (Kufeldt & Nimmo, 1987). This study showed that these families, similar to non-runaway families, can be effectively engaged and maintained into family treatment. Researchers have concluded that family-based interventions show higher rates of engagement and treatment retention compared to non-family based interventions (Stanton & Shadish, 1997). For example, Liddle et al. (2001) had a 16% treatment refusal rate and both Liddle et al. (2001) and Santisteban et al. (2003) reported a 70% treatment retention rate. Findings from this study are similar: 2/65 (3%) did not attend 1 session, 51/65 (77%) attended 5 or more sessions.
EBFT showed a differential positive impact on youth’s substance abuse. These findings are in line with other family intervention studies (see reviews Kaminer & Slesnick, in press; Ozechowski & Liddle, 2001) that found a differential impact of family therapy on substance use compared to non family-based therapy. This study extends previous findings to a subpopulation of substance abusing youth who often report significantly greater substance use, (as well as greater individual and family problems) compared to matched, housed youth (Forst & Crim, 1994; Koopman, Rosario, & Rotheram-Borus, 1994). In addition, EBFT had a significantly greater impact on reducing substance related problems and number of drugs used for physically and sexually abused youth. Given the role of the family in precipitating the runaway episode, it follows that inclusion of all those involved should increase the opportunity to resolve family problems and facilitate family members’ movement forward in seeking new ways of coping with difficult family stressors.
We did not find interactions between treatment modality and time for non-substance related variables (including family functioning), as these variables improved for all youth (those assigned to EBFT and SAU). In general, prior reviews (e.g. Stanton & Shadish, 1997) noted that family therapy studies found no significant difference in the reduction of adolescent problem behaviors (other than substance use) or family functioning between family and non-family-based interventions at post treatment or follow-up. Proposed reasons for the lack of significant group x time interactions in these domains include treatment effects in the comparison conditions, measurement instruments that are inadequately sensitive to change, or lack of sufficient statistical power. As Liddle and Dakof (1995) noted, measures of family functioning (a hypothesized mechanism of change in family therapy) across studies have primarily been based upon self-report measures. Utilizing observational measures may more sensitively assess changes in family interaction. Recently, in an exploratory analysis using observer ratings of family functioning, Santisteban et al. (2003) found differential improvement in family cohesion for family compared to group therapy. These findings further support the notion that observational methods may more sensitively assess family interactional change.
Second, our findings suggest that youth’s involvement in the shelter system has a positive impact on his or her behavior across a variety of domains even at one year post shelter stay. Few studies have examined long-term impact of a shelter stay on youth’s functioning across a range of domains. Our findings echo those of one study that examined the short-term impact of a shelter-stay on runaway youths’ behaviors (Thompson, Pollio, Constantine, Reid, & Nebbitt, 2002). Thompson et al. (2002) compared short term outcomes (6 weeks postdischarge) of 261 youth using runaway shelters from four midwestern states compared to 47 youth in longer term day treatment programs. Both groups showed significant improvement on 10 broad outcome variables, with no significant differences between the two groups.
Limitations
Limitations of the study should be noted. We did not conduct independent ratings of treatment fidelity for EBFT as the manual was a work in progress that evolved over the course of the project. However, the clinical supervisor reviewed audiotapes and provided intensive supervision with project therapists to ensure that the core elements of EBFT were being utilized by therapists. Our sample of runaway youth and families is based upon a sample of convenience and may not represent runaway youth in other parts of the country that have different ethnic and racial compositions, and perhaps different environmental/social influences. Another limitation is that findings were based solely upon youths’ self-report of their family environment and their own behavior. However, over nineteen studies have noted that by age ten, youths are considered reliable and valid informants of their own behaviors and feelings and that parents are not always the most reliable informants about the behavior of their children (see Meyers et al., 1999).
This study is an additional step towards developing and identifying effective treatments for this underserved population and much more work is needed. Longitudinal research to identify critical periods for intervention to prevent family disintegration leading to chronic running away and homelessness is necessary. Identification of high risk youth and having interventions available prior to them entering the shelter system can reduce disruption to the family associated with the youth being removed from the home. Alternatively, the youth’s stay at a shelter might provide needed respite to the family and create a context by which reunification and problem resolution can be most successful. That is, intervening when the family is “at its wit’s end” can be the crisis that facilitates participation and motivation for adjusting family interaction processes. In fact, Post and McCoard (1994) found that during a crisis (when the youth is at the shelter), these youths and families may be more amenable than usual to counseling.
Future Directions
Successful intervention at the point when the family has not disintegrated beyond the point of reunification might prevent future homelessness, though future research will need to examine this possibility. That is, most street living, homeless youth do not reach the shelter system (U.S. House of Representatives, 1992) which is in part because they do not want their families contacted as required by shelters, and because they have great difficulty maintaining in shelters – due to the behavioral requirements. Most street living youth no longer tolerate the possibility of reuniting with their families and in general, street youth have more severe substance abuse and related problems than do youth who reside at a runaway shelter (Finkelhor, Hotaling, & Sedlak, 1990).
Family reunification, when it is still possible and feasible, is significant not only because it might reduce the possibility of chronic running away and homelessness, but also because it can reduce related problems including the potential for suicide. Teare, Furst, Peterson, and Authier (1992) found that in their sample of shelter youths, those not reunified with their family were at greater risk of suicide, had more overall dissatisfaction with life, greater hopelessness, more generalized negative expectations about the future and more family problems compared to those who were reunified. Thus, attention towards reunifying families whose child resides at a shelter (when appropriate), or addressing problematic family interaction patterns prior to the youth leaving home, is worthy of future research focus.
Footnotes
This work has been supported by NIDA grant (R29 DA 11590).
Contributor Information
Natasha Slesnick, Department of Human Development and Family Science, The Ohio State University.
Jillian L. Prestopnik, Center on Alcoholism, Substance Abuse and Addictions, University of New Mexico
References
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Child Behavior Profile. Burlington, VT: Child Psychiatry, University of Vermont; 1982. [Google Scholar]
- Ashworth CS, Durant RH, Newman CC, Gaillard G. An evaluation of a school-based AIDS/HIV education program for high school students. Journal of Adolescent Health. 1992;13:582–588. doi: 10.1016/1054-139x(92)90372-i. [DOI] [PubMed] [Google Scholar]
- Barth RP. Theories guiding home-based intensive family preservation services. In: Whittaker JK, Kinney J, Tracy EM, Booth C, editors. Reaching high-risk families: Intensive preservation services in human services. New York: Aaldine; 1990. pp. 89–112. [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, Erlbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bry BH. Family-based approaches to reducing adolescent substance use: Theories, techniques, and findings. National Institute on Drug Abuse: Research Monograph Series. 1988;77:39–68. [PubMed] [Google Scholar]
- Cauce AM, Morgan CJ, Wagner V, Moore E, Sy J, Wurzbacher K, Weeden K, Tomlin S, Blanchard T. Effectiveness of intensive case management for homeless adolescents: Results of a 3-month follow-up. Special Series: Center for Mental Health Services Research Projects. Journal of Emotional and Behavioral Disorders. 1994;2:219–227. [Google Scholar]
- Craig RJ. Contemporary trends in substance abuse. Professional Psychology: Research and Practice. 1993;24:182–189. Substance Abuse, 8, 1–13. [Google Scholar]
- Elliot DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills, CA: Sage; 1985. [Google Scholar]
- Feldman LH. Evaluating the impact of intensive family preservation services in New Jersey. In: Wells K, Biegel DA, editors. Family preservation services: Research and evaluation. Newbury Park, CA: Sage; 1991. pp. 47–71. [Google Scholar]
- Finkelhor D, Hotaling G, Sedlak A. Missing, abducted, runaway and thrownaway children in America: First report. Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 1990. [Google Scholar]
- Flaherty J, Richman J. Gender differences in the perception and utilization of social support: Theoretical perspectives and an empirical test. Social Science Medicine. 1989;28:1221–1228. doi: 10.1016/0277-9536(89)90340-7. [DOI] [PubMed] [Google Scholar]
- Forst ML, Crim D. A substance use profile of delinquent and homeless youths. Journal of Drug Education. 1994;24:219–231. doi: 10.2190/K7VM-P8KN-P2FD-W9C3. [DOI] [PubMed] [Google Scholar]
- Gruen RJ, Gwadz M, Morrobel D. Support, criticism, emotion and depressive symptoms: Gender differences in the stress-depression relationship. Journal of Social and Personal Relationships. 1994;11:619–24. [Google Scholar]
- Gurman AS, Kniskern DP, Pinsof WM. Research on the process and outcome of marital and family therapy. In: Garfield SL, Bergin AE, editors. Handbook of psychotherapy and behavior change. 3. New York: Wiley; 1986. pp. 565–624. [Google Scholar]
- Henggeler SW, Clingempeel WG, Brondino MJ. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:868–874. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance-abusing and dependent delinquents: Outcomes, treatment, fidelity, and transportability. Mental Health Services Research. 1999;1:171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- Jessor R, Jessor SL. The social-psychological framework. In: Jessor R, Jessor SL, editors. Problem behavior and psychosocial development: A longitudinal study of youth. New York: Academic Press; 1977. pp. 17–42. [Google Scholar]
- Joanning H, Thomas F, Quinn W, Millen R. Treating adolescent drug abuse: A comparison of family systems therapy, group therapy, and family drug education. Journal of Marital and Family Therapy. 1992;18:345–356. [Google Scholar]
- Johnson TP, Aschkenasy JR, Herbers MR, Gillenwater SA. Self-reported risk factors for AIDS among homeless youth. AIDS Education and Prevention. 1996;8:308–322. [PubMed] [Google Scholar]
- Kaminer Y, Slesnick N. Evidence-based cognitive-behavioral and family therapies for adolescent alcohol and other substance use disorders. In: Galanter M, editor. Recent developments in alcoholism, Vol. XVII: Research on alcohol problems in adolescents and young adults. In press. [DOI] [PubMed] [Google Scholar]
- Kann L, Nelson GD, Jones JT, Kolbe LJ. Establishing a system of complementary school-based surveys to annually assess HIV-related knowledge, beliefs, and behaviors among adolescents. Journal of School Health. 1989;59:55–58. doi: 10.1111/j.1746-1561.1989.tb05392.x. [DOI] [PubMed] [Google Scholar]
- Kinney J, Haapala D, Madsen B, Fleming T. Keeping families together: The Homebuilders model. Hawthorne, NY: Aldine de Gruyter; 1991. [Google Scholar]
- Kinney J, Haapala DA, Booth C, Leavitt S. In: Reaching high-risk families: Intensive family preservation in human services. Whittaker JK, Tracy EM, Booth C, Kinney J, editors. Hawthorne, NY: Aldine de Gruyter; 1990. pp. 31–36. [Google Scholar]
- Koopman C, Rosario M, Rotheram-Borus MJ. Alcohol and drug use and sexual behaviors placing runaways at risk for HIV infection. Addictive Behaviors. 1994;19:95–103. doi: 10.1016/0306-4603(94)90055-8. [DOI] [PubMed] [Google Scholar]
- Kufeldt K, Durieux M, Nimmo M, McDonald M. Providing shelter for street youth: Are we reaching those in need? Child Abuse and Neglect. 1992;16:187–199. doi: 10.1016/0145-2134(92)90027-o. [DOI] [PubMed] [Google Scholar]
- Kufeldt K, Nimmo M. Youth on the street: Abuse and neglect in the eighties. Child Abuse and Neglect. 1987;11:531–543. doi: 10.1016/0145-2134(87)90079-2. [DOI] [PubMed] [Google Scholar]
- Liddle HA. Cannabis Youth Treatment (CYT) Manual series. Vol. 5. Rockville, MD: CSAT, SAMHSA; 2001. Multidimensional Family Therapy Treatment (MDFT) for the adolescent cannabis users. [Google Scholar]
- Liddle HA, Dakof G, Diamond G. Adolescent substance abuse: Multidimensional family therapy in action. In: Kaufman E, Kaufman P, editors. Family therapy with drug and alcohol abuse. Boston: Allyn & Bacon; 1991. pp. 120–171. [Google Scholar]
- Liddle HA, Dakof GA. Efficacy of family therapy for drug abuse: promising but not definitive. Journal of Marital and Family Therapy. 1995;21:511–543. [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. American Journal of Drug Alcohol Abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- McLaney MA, DelBoca FK, Babor TF. A validation study of the Problem Orientated Screening Instrument for Teenagers (POSIT) Journal of Mental Health. 1994;3:363–376. [Google Scholar]
- Meyers K, Hagan TA, Zanis D, Webb A, Franz J, Ring-Kurtz S, Rutherford M, McLellan AT. Critical issues in adolescent substance use assessment. Drug and Alcohol Dependence. 1999;55:235–246. doi: 10.1016/s0376-8716(99)00019-8. [DOI] [PubMed] [Google Scholar]
- Miller WR, DelBoca FK. Measurement of drinking behavior using the Form-90 family of instruments. Journal of Studies on Alcohol. 1994;(Supplement No 12):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Marlatt GA. Manual for the Comprehensive Drinker Profile. Odessa, FL: Psychological Assessment Resources; 1984. [Google Scholar]
- Moffit TE. Accommodating self-report methods to a low-delinquency culture: Experience from New Zealand. In: Klien MW, editor. Cross-national research in self-reported crime and delinquency. Norwell, MA: Kluwer Academic; 1989. pp. 43–66. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Morrissette P. Engagement strategies with reluctant homeless young people. Psychotherapy. 1992;29:777–451. [Google Scholar]
- Nelson K. Innovative delivery models in social services. Journal of Clinical Child Psychology. 1994;23:26–31. [Google Scholar]
- Nelson KE, Landsman MJ. Alternative models of family preservation: Family-based services in context. Springfield, IL: Thomas; 1992. [Google Scholar]
- Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: Knowns and unknowns. Clinical Child and Family Psychology Review. 2000;3:269–298. doi: 10.1023/a:1026429205294. [DOI] [PubMed] [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Pickrel SG, Henggeler SW. Multisystemic therapy for adolescent substance abuse and dependence. Adolescent Substance Abuse and Dual Disorders. 1996;5:201–211. [Google Scholar]
- Post P, McCoard D. Needs and self-concept of runaway adolescents. The School Counselor. 1994;41:212–219. [Google Scholar]
- Project MATCH Research Group; National Institute on Alcohol Abuse and Alcoholism. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical and Experimental Research. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Rahdert E, editor. The adolescent assessment and referral system manual DHHS Publication No. (ADM) 91-1735. Rockville, MD: National Institute on Drug Abuse; 1991. [Google Scholar]
- Robertson MJ, Toro PA. Homeless youth: Research, intervention, and policy. In: Fosburg LB, Dennis DL, editors. Practical lessons: The 1998 National Symposium on Homelessness Research. Washington DC: US Department of Housing and Urban Development and US Department of Health and Human Services; 1999. pp. 3-1–3-32. [Google Scholar]
- Rotheram-Borus MJ, Koopman C, Haignere C, Davies M. Reducing HIV sexual risk behaviors among runaway adolescents. Journal of the American Medical Association. 1991;266:1237–1241. [PubMed] [Google Scholar]
- Santisteban DA, Perez-Vidal A, Coatsworth JD, Kurtines WM. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. Journal of Family Psychology. 2003;17:121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt SE, Liddle HA, Dakof GA. Changes in parenting practices and adolescent drug abuse during multidimensional family therapy. Journal of Family Psychology. 1996;10:12–27. [Google Scholar]
- Schweitzer RD, Hier SJ. Psychological maladjustment among homeless adolescents. Australian and New Zealand Journal of Psychiatry. 1993;27:275–280. doi: 10.1080/00048679309075777. [DOI] [PubMed] [Google Scholar]
- Shaffer D. The Diagnostic Interview Schedule for Children-2.3 Version. New York: Columbia University; 1992. [Google Scholar]
- Slesnick N. Treatment Manual: Ecologically-Based Family Therapy For Substance Abusing Runaway Youth. 2003. Unpublished manuscript. [Google Scholar]
- Slesnick N, Tonigan JS. A test-retest study of Form 90 assessment of runaway youth’s substance use. Alcoholism Treatment Quarterly. 22(2) doi: 10.1300/J020v22n02_03. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart RG, Ogborne AC. Street youth in substance abuse treatment: Characteristics and treatment compliance. Adolescence. 1994;29:733–745. [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litten R, Allen J, editors. Measuring alcohol consumption. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stanton MD, Shadish WR. Outcome, attrition, and family—Couples treatment for drug abuse: A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin. 1997;122:170–191. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage & the Family. 1979;41:75–88. [Google Scholar]
- Szapocznik J, Kurtines WM, Santisteban DA, Rio AT. The interplay of advances among theory, research, and application in treatment interventions aimed at behavior problem children and adolescents. Journal of Consulting and Clinical Psychology. 1990;58:696–703. doi: 10.1037//0022-006x.58.6.696. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Kurtines WM, Foote F, Perez-Vidal A, Hervis O. Conjoint versus one-person family therapy: Further evidence for the effectiveness of conducting family therapy through one person with drug abusing adolescents. Journal of Consulting and Clinical Psychology. 1983;54:395–397. doi: 10.1037//0022-006x.54.3.395. [DOI] [PubMed] [Google Scholar]
- Teare JF, Furst DW, Peterson RW, Authier K. Family reunification following shelter placement: Child, family, and program correlates. American Journal of Orthopsychiatry. 1992;62:142–146. doi: 10.1037/h0079314. [DOI] [PubMed] [Google Scholar]
- Thompson SJ, Pollio DE, Constantine J, Reid D, Nebbitt V. Short-term outcomes for youth receiving runaway and homeless shelter services. Research on Social Work Practice. 2002;12:589–604. [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Unger JB, Kipke MD, Simon TR, Montgomery SB, Johnson CJ. Homeless youths and young adults in Los Angeles: Prevalence of mental health and substance abuse disorders. American Journal of Community Psychology. 1997;25:371–394. doi: 10.1023/a:1024680727864. [DOI] [PubMed] [Google Scholar]
- U. S. House of Representatives, Education and Labor Committee. U.S. Code of Law and Administrative News, House Report No. 102–756. 1992. Legislative history, juvenile justice and delinquency amendments. [Google Scholar]
- Waldron HB. Adolescent substance abuse and family therapy outcome: A review of randomized trials. In: Ollendick TH, Prinz RJ, editors. Advances in clinical child psychology. New York, NY: Plenum Press; 1997. pp. 199–234. [Google Scholar]
- Warheit GJ, Biafora F. Mental health and substance abuse patterns among a sample of homeless post-adolescents. International Journal of Adolescents and Youth. 1991;3:9–27. [Google Scholar]
- Westerberg VS, Tonigan JS, Miller WR. Reliability of Form 90D: An instrument for quantifying drug use. Substance Abuse. 1998;19(4):179–189. doi: 10.1080/08897079809511386. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD. Current issues and future needs in the assessment of adolescent drug abuse. NIDA Research Monograph. 1995;156:146–171. [PubMed] [Google Scholar]
- Wolfe SM, Toro PA, McCaskill PA. A comparison of homeless and matched housed adolescents on family environment variables. Journal of Research on Adolescence. 1999;9:53–66. [Google Scholar]
- Zimet GD, Sobo EJ, Zimmerman T, Jackson J, Mortimer J, Yanda CP, Lazebnik R. Sexual behavior, drug use, and AIDS knowledge among midwestern runaways. Youth and Society. 1995;26:450–462. [Google Scholar]


