Abstract
Objective:
The aim of this study was to compare the outcomes of 3 different levels of sympathectomy.
Summary Background Data:
Most surgeons still perform T2 or T2–3 sympathectomy for palmar hyperhidrosis, but both these treatments can cause severe side effects. Some recent articles have advocated T4 sympathectomy and obtained satisfactory results.
Methods:
Between January 2000 and August 2004, 234 records of patients treated for palmar hyperhidrosis were retrospectively reviewed. Of them, 86 patients were treated with endoscopic thoracic sympathectomy of T2 (ETS2), 78 patients with ETS3, and 70 patients with ETS4. Follow-up data were collected using a telephone questionnaire with a scoring system. Multiple linear regressions were used to model markers for degree of satisfaction and severity of compensatory sweating (CS), including descriptive data, level of sympathectomy, clinical outcomes, and postoperative complications.
Results:
Mean follow-up was 47.1 ± 17.2 months. All 3 levels of sympathectomy could have achieved comparable improvement of palmar hyperhidrosis (P = 0.162). However, 88.5% of the patients noticed CS. Patients with ETS4 presented the lowest incidence of CS (P = 0.030), had the least severity of CS (β = −1.537, P = 0.002), and felt the least palmar overdryness (P < 0.001). None expressed regret for the procedure in the ETS4 group (P = 0.022). Being obese did not increase the incidence of CS, but the severity of CS was directly related to body mass index (β = 0.917, P < 0.001). The patients would be more satisfied if the severity of CS was minimal (β = −0.185, P = 0.002). The degree of satisfaction may decrease with time (β = −0.025, P = 0.003) and was lower when their palms were overdry (β = −1.463, P < 0.001).
Conclusions:
Different from the current procedure of T2 or T3 sympathectomy for palmar hyperhidrosis, T4 sympathectomy would be a better and more effective procedure with minimal long-term complications.
The aim of this study was to analyze and compare the long-term outcome of palmar hyperhidrosis treated by endoscopic thoracoscopic sympathectomy at 3 different levels. T4 sympathectomy preserved the purpose in solving excessive palmar sweating and simultaneously caused the least compensatory sweating.
Endoscopic thoracic sympathectomy (ETS) has been widely accepted as a safer and more effective procedure for the treatment of palmar hyperhidrosis with higher success rates. However, the flagrant side effect mostly influencing the quality of life is the presence of compensatory sweating (CS). To reduce the incidence of severe compensatory symptoms, several authors limited the extent of resections for hyperhidrosis to a single level,1–4 whereas Lin and Telaranta introduced the classification of sympathetic disorder according to segmental distribution of sympathetic innervations.5 According to the classification, interruption of T2 ganglion may ameliorate facial blushing and vibration disorder, T3 ganglion for facial sweating and blushing, T4 for palmar sweating, and T5 for axillary sweating (bromidrosis). Previously, we also published the importance of classification in sympathetic surgery and offered a proposed mechanism for CS.6
As per most reports from 2005,7–9 most surgeons have performed T2 or T2–3 sympathectomy for palmar hyperhidrosis. Recently, several authors treated palmar hyperhidrosis following the modified Lin-Telaranta classification and obtained very good results.1,6,10–12 However, published details of any comparative method concerning long-term outcome of T2, T3, and T4 sympathectomy are still lacking. In the present study, we have analyzed the long-term follow-up of palmar hyperhidrosis treated by the 3 different levels of sympathectomy and we have also evaluated which level of ganglion interrupted is the best for palmar hyperhidrosis.
PATIENTS AND METHODS
This was a retrospective review at a single medical center between January 2000 and August 2004 by the same surgical team. During the 5-year period, 158 men and 176 women were treated for palmar hyperhidrosis. This study included some patients mentioned in previous articles.6,10 Mean age at operation of hyperhidrosis was 22.9 ± 7.7 years and mean body mass index (BMI) was 21.1 ± 3.2 kg/m2. One hundred and fifty patients were treated by ETS of T2 (ETS2), 92 patients by ETS3, and 92 patients by ETS4. The different procedures performed were based on the changes in practice inspiration from the reports in other centers.3–5,12 Indeed, most patients in group ETS2 were operated on earlier in the period and most patients in groups ETS3 and ETS4 underwent surgery later in the period.
Surgical Technique
The surgical technique of ETS was performed as previously described.7,10 Under general anesthesia with single lumen tracheal intubation, the patient's arms were extended slightly upward and the axillae were exposed. Either two 5-mm ports or a single-port approach was used. For the former method, 1 port at the axilla and 1 at the midaxillary line at the level of the nipple were inserted. For the latter method, a 10-mm port was inserted at the third intercostal space over the midaxillary line. Because the first rib was usually difficult to visualize through thoracoscopy (Karl Storz GmbH & Co, Tuttlingen, Germany), the second, third, fourth, and fifth ribs were identified according to the anatomic landmark of the first rib covered by an area of bright yellow fat at the costovertebral junction. At the level where the sympathetic chain crossed the ribs, the parietal pleura was opened with the diathermic hook. The upper and lower ends of the intended ganglion were completely coagulated by simple diathermy at the head of the upper and lower ribs, for example: the fourth and fifth ribs for T4 ganglion. After being separated from the surrounding tissue, the sympathetic chain was gently cauterized and transected completely but the ganglion was left in position without removal by manipulation. The lung was routinely inflated after the procedure to make sure that it was well-expanded. No stitches were required for the 5-mm port, whereas 1 or 2 stitches were necessary for the 10-mm port. The same procedure was performed on the contralateral side. Postoperative chest radiography was performed routinely.
Data Collection
First, case patients were analyzed for their descriptive variables (age at operation, gender, BMI, and family history) by reviewing the medical charts. Second, at least 1 outpatient clinic was visited routinely within 1 week and the patient immediate postoperative outcomes were recorded according to the medical files. Third, follow-up data (at least 20 months from the time of surgery) were collected using a standardized telephone questionnaire. The visual analog scale (VAS) graded between 0 (none at all) and 10 (worst possible symptoms and clothes needing to be changed frequently) was used to represent the sweating pattern. Patient satisfaction after sympathectomy was also assessed from VAS 0 (extreme dissatisfaction) to 10 (excellent satisfaction). The score of palmar sweating before sympathectomy was recorded in sum A (rest and emotional response) (min: 0; max: 20). The score of palmar sweating after sympathectomy was also recorded in sum B (0–20). The change of sweating pattern before and after sympathectomy was recorded in sum (A − B). Subjective outcomes included recurrence of palmar hyperhidrosis, presence of gustatory sweating, presence of CS, regions of CS, severity of CS, palmar overdryness after sympathectomy, and regret after sympathectomy. This questionnaire allowed the research team to obtain an accurate pattern of postoperative sweating and follow-up data.
Statistical Analysis
Before beginning our analysis, the available literature was reviewed to identify factors thought to be important in CS and patient's satisfaction. Student t tests and χ2 tests were used to compare continuous and categorical descriptive variables respectively between enrolled and nonenrolled patients. The differences in enrolled patients were compared across the 3 groups of various surgical interventions using analysis of variance (ANOVA) for continuous variables and χ2 tests for categorical variables. Further analysis with Scheffe post hoc test was planned when the ANOVA showed that there was a statistical difference between groups. Univariate and multivariate linear regression analyses were used to examine the relationships between the subjective clinical outcomes and degree of satisfaction. Linear regression analyses were also used to examine the risk factors of severity of CS among the patients. Using the binary coding, the relationships between CS and 3 different levels of sympathectomy were also evaluated in the linear regression. Potential confounders such as patient age, gender, BMI, duration of follow-up, and postoperative outcomes were adjusted in all multivariate analyses. Results were expressed as a mean with standard deviation or effect and 95% confidence interval where appropriate. A P value of less than 0.05 denoted statistical significance. SPSS for Windows version 12.0 was used for all statistics.
RESULTS
Descriptive Data
Response rate for the telephone questionnaire was 67.1% (Table 1). The data for 90 patients were not collected. Of these, 68 of them had incorrect phone numbers and 16 patients had gone abroad. Six patients who received ETS2 refused the telephone interview by reason of recurrence in 3, severe CS in 2, and left brachial plexopathy in 1. Of the 244 patients, data in 10 patients were incomplete and records of 234 patients were enrolled. A comparison of the 234 complete follow-up patients with those who were not included showed no significant differences in age, gender, and BMI (P = 0.654, 0.430, and 0.217).
TABLE 1. Descriptive Variables in Enrolled Patients
Of 234 participating patients, 112 of them (47.9%) were students. A family history was elicited in 113 of 234 patients (48.3%). The mean age of enrolled patients was 22.3 ± 7.2 years and mean BMI was 20.9 ± 3.4 kg/m2. Before operation, 26 patients (11.1%) had once tried topical antiperspirants as treatment but this did not produce satisfactory results. There were 86 patients of ETS2, 78 patients of ETS3, and 70 patients of ETS4 enrolled. Gender and the score of palmar sweating before sympathectomy (sum A) among 3 enrolled groups were comparable (P = 0.145 and 0.713). The average age (P < 0.001) and the body configurations (P = 0.430) of the patients were similar clinically, though there were statistically significant differences among the 3 groups. Mean follow-up was 47.1 ± 17.2 months.
Short-term Outcome
During operation, no patient died or developed Horner syndrome, no procedures were converted to thoracotomy, and adhesions were found in 3 patients (1.3%). Two hundred and twenty patients (94.0%) could be discharged within 24 hours after the operation. Immediate complications were usually mild and requiring at most a day or 2 of prolonged hospital stay. Seventy-six patients (32.5%) had subcutaneous emphysema and 33 patients (14.1%) had pneumothorax on follow-up x-ray. All of the pneumothorax cases were residual (not because of lung injury) and most of them were generally reabsorbed spontaneously and needed no further treatment. However, 6 patients (2.6%) required chest tube drainage. The other complications included 8 patients (3.4%) with pulmonary atelectasis, 7 patients (3.0%) with intercostal pain, 2 patients (0.9%) with pleural effusions, and 1 patient (0.4%) with hemothorax.
Long-term Follow-up
The length of mean follow-up in ETS2 was 60.9 ± 15.3 months, in ETS3 35.6 ± 13.5 months, and in ETS4 43.1 ± 10.3 months. The patients with ETS3 had the least degree of postoperative sweating in their hands (sum B) (P = 0.012), though the differences of palmar sweating before and after operations were comparable among the 3 groups [sum (A − B)] (P = 0.162) (Table 2). Up to 88.5% of the patients might notice CS in previously less affected regions of the body. There were usually multiple regions of CS, but group ETS4 had less areas involved (P = 0.015). The most common region of CS was the back, occurring in 56.3% of ETS2, 75% of ETS3, and 42.9% of ETS4 (Fig. 2). Compared with the back, CS affected less frequently the anterior aspect of the body and the lower legs. Group ETS4 also had lower incidence and lesser severity of CS when compared with the other 2 groups (P = 0.030, and <0.001). Patients (13.2%) may notice increased sweating while smelling or eating spicy food (gustatory sweating). Of those patients with recurrence of palmar hyperhidrosis, 22 patients (25.6%) were in group ETS2, 6 patients (7.7%) in group ETS3, and 16 patients (22.9%) in group ETS4. Sixty-nine patients (29.5%) complained about overdryness of their palms, especially groups ETS2 and ETS3 (P < 0.001). Most patients were satisfied with the results of surgery, especially in groups ETS3 and ETS4 (P < 0.001). Eleven patients (4.7%) regretted the surgical procedure, especially in group ETS2 (P = 0.022). No patient expressed regret in group ETS4.
TABLE 2. Clinical Feature of the Patients With Long-term Follow-up
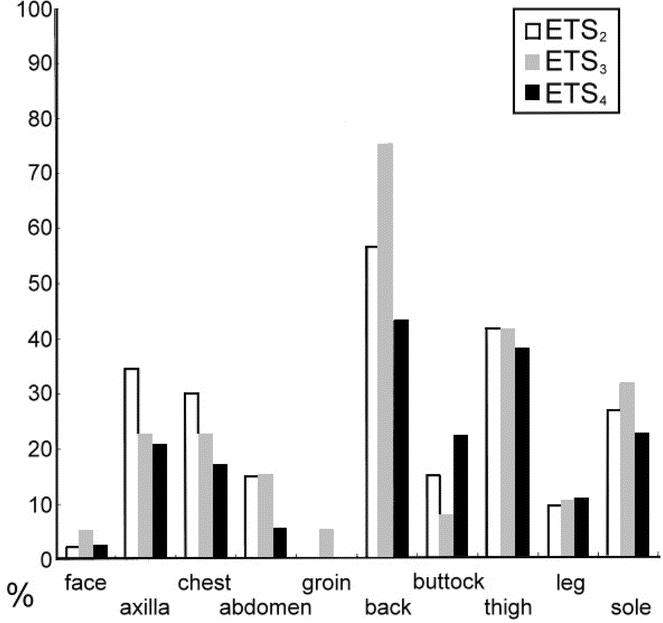
FIGURE 2. Regions of compensatory sweating of the 3 groups.
The results of factors influencing the extent of CS are shown in Table 3. In the univariate analysis, the extent of CS was directly related to the BMI and regions of CS, while being independent of age, gender, presence of gustatory sweating, positive family history, and duration of follow-up. In the multivariate analysis, the severity of CS was still significantly directly related to the BMI and regions of CS in total patients (β = 0.132, P = 0.021 and β = 0.917, P < 0.001). Group ETS4 presented with a lesser extent of CS than group ETS2 in both univariate and multivariate analysis (β = −2.409, P < 0.001 and β = −1.537, P = 0.002). The patients with ETS3 were found to have a greater extent of CS than the patients with ETS2 in univariate analysis (β = 1.113, P = 0.007), but this was not significant after additional adjustment (β = 0.325, P = 0.533).
TABLE 3. Factors Influencing the Extent of CS Estimated by Univariate and Multivariate Linear Regression
The results of factors influencing postoperative satisfaction are shown in Table 4. In the univariate analysis, the degree of satisfaction was directly related to age and the difference of palmar sweating before and after operation [sum (A − B)], but was inversely related to the regions of CS, the severity of CS, the score of palmar sweating after sympathectomy (sum B), the duration of follow-up, palmar overdryness, and recurrence of palmar hyperhidrosis. Patient satisfaction was independent of gender, BMI, presence of gustatory sweating, presence of CS, and positive family history. In the multivariate analysis, the degree of satisfaction in patients was significantly inversely related to the severity of CS, the score of palmar sweating after sympathectomy (Sum B), duration of follow-up, and palmar overdryness (β = −0.185, P = 0.002; β = −0.159, P = 0.011; β = −0.025, P = 0.003 and β = −1.463, P < 0.001), whereas age, regions of CS, the difference of palmar sweating before and after operation [sum (A − B)], and recurrence were not significant after additional adjustment (P = 0.382, 0.371, 0.691, and 0.169).
TABLE 4. Factors Influencing Postoperative Satisfaction Estimated by Univariate and Multivariate Linear Regression
DISCUSSION
ETS is currently recognized as the best method of treatment for palmar hyperhidrosis. However, it is difficult to say whether the operation is successful or not,11 being totally based on the patient's subjective feelings.13 To date, there are 2 quality-of-life instruments that examine the physical and psychologic condition of patients after ETS.1,13 We considered that telephone visits might fail or be incomplete if the questions asked were excessively long or complex. In the present series, these patients were followed up by a simplified telephone questionnaire with VAS under the following issues: degree of palmar sweating before and after operation, severity of CS, degree of satisfaction, and regret after operation. Because 84 patients never received the questionnaire because they had emigrated, the actual response rate may be calculated as 93.6%. According to the visiting results, both ETS3 and ETS4 could provide comparable satisfaction and were significantly different from what ETS2 provided (P < 0.001).
In the present study, different levels of sympathectomy all brought about good effects in reducing palmar hyperhidrosis [sum (A − B), P = 0.162]. However, a large discrepancy of satisfaction was noted among patients, and postoperative complications nearly accounted for all the disparity in satisfaction. The multivariate logistic regression showed that the most important variable influencing satisfaction after the operation was the presence of palmar overdryness (β = −1.463, P < 0.001) (Table 4) and the most important variable associated with the severity of CS was the number of regions of CS (β = 0.917, P < 0.001) (Table 3). In Table 2, the patients with ETS4 had the lowest incidence of CS, the least regions of CS and their palms were simultaneously the least suffering from overdryness (P = 0.030, 0.015, and <0.001). None of the patients with ETS4 regretted having the operation. Compared with ETS3, it seemed that ETS4 for palmar hyperhidrosis was a more effective approach, which could minimize postoperative complications, including palmar overdryness, presence of CS, and regions of CS.
Generally, the more sympathetic segments excised, the greater the incidence of severe compensatory symptoms.2,14 Several authors limited the extent of resections for hyperhidrosis to a single level to reduce the incidence of severe compensatory symptoms.1–4 However, the correlation between the level of the sympathetic trunk interrupted and severity of CS was reported (Fig. 1). 2,15 Inclusion of the T2 lesion results in significantly more severe CS than other levels not having T2 removed.2,16 In the present series, different degrees of CS were found after different level of sympathectomy (P < 0.001). Compared with ETS2, the severity of CS was directly related to ETS3 (β = 0.325, P = 0.533) and significantly inversely related to ETS4 (β = −1.537, P = 0.002) in the multivariate analyses.

FIGURE 1. The schematic drawing showing T4 sympathectomy was performed by simple diathermic severance of the sympathetic trunk.
Compensatory sweating seems to be a permanent side effect and occurred in 88.5% of our patients and the detailed distribution is shown in Figure 2. The distributions of the preferential location among the 3 groups were comparable, and back and lower extremities were the common regions. When compared with groups ETS2 and ETS3, group ETS4 had less areas involved (P = 0.015). However, the highest incidence in the back and the lowest in the buttock were presented in group ETS3. Perhaps we should have asked our patients more clearly whether their CS occurred in the upper, middle, or lower back. Besides, patients may confuse the area “lower back” or “buttock.” In general, several authors have described that the most common region was the posterior aspect of the trunk.17,18 The authors believe that postoperative sweating is “reflex sweating” instead of CS because the positive feedback mechanism (reflex sweating) of the autonomic nervous system is induced by blocked negative feedback signal (sympathectomy).6 T2 interruption stops negative feedback signals from T2 and below and provides the strongest positive feedback signal. T3 interruption preserves some negative feedback signals (from T2) whereas T4 interruption preserves more (from T2 and T3). Therefore, the positive feedback signals are much weaker in T4 interruption than in T2 interruption. The severest form of CS was observed more frequently in the T2 group than in the T3 group.15,16,19 The detailed mechanism of reflex sweating has been described in our previous publication.6
Patient satisfaction would not be affected by the presence of CS or a lot of regions of CS (P = 0.569 and 0.371). The above results illustrated that these patients all have a certain cognition regarding CS, which seems inevitable. However, the degree of satisfaction would drop if the degree of CS was too serious (β = −0.185, P = 0.002). Panhofer et al1 also reported that the quality of life in patients who developed severe CS was worse than before surgery. Therefore, those patients should be excluded from surgery if risk factors could be identified for the development of CS. Because the triggering factors of hyperhidrosis are emotion and anxiety rather than a hot environment,20 obesity was not a risk factor of presence of CS (BMI >24 vs. ≦24 kg/m2; odds ratio 2.28; 95% confidence interval (CI), 0.52–10.14; P = 0.276). However, CS was actually more serious in obese individuals (β = 0.132, P = 0.021) although no statistically significant association was found between BMI and the degree of satisfaction (P = 0.198). The same results were described by de Campos et al.19 That is to say, when facing a broader-in-stature patient who seeks surgery for palmar perspiration, the surgeon must inform him/her that the degree of CS after operation might be more serious than that of the average person.
Thirty-six percent of patients with ETS2 felt overdryness in their hands whereas only 8.6% of the patients with ETS4 felt the same (P < 0.001). In the multivariate analysis, the degree of satisfaction may be significantly lower when their palms were quite dry (β = −1.463, P < 0.001). On the contrary, group ETS4 usually had satisfyingly mildly moist rather than fissured palms. We believe that the nerves to sweat glands of the hands center on the upper part of the sympathetic trunk although the routes may originate from T2 to T10. That is to say, the more uppermost the ganglion interrupted, the drier the palms present. Much drier hands should be observed in the T2 group than those of the T3 group theoretically. However, the least degree of postoperative palmar sweating was presented in group ETS3. Because the incidence of recurrence may increase with time no matter which level was transected,8,21 the differences in the follow-up period among the 3 groups interfered in the analysis of the outcomes. The shortest duration of follow-up in group ETS3 accounted for the preponderance of the least degree of palmar sweating and the lowest recurrence after sympathectomy.
We did not specifically ask our patients whether their CS had improved during long-term follow-up, but their satisfaction decayed gradually with time (β = −0.025, P = 0.003). Patient satisfaction is not only related to the result (reduction of palmar sweating), but also to patient tolerance to complications (recurrence, palmar overdryness, and CS). Once the euphoria over improvement in their hyperhidrosis dissipates, the patient's unsatisfied perception about postoperative side effects will be amplified.
Several authors have described greater prevalence of palmar hyperhidrosis among women than men,1,2,8,13,17 and the present study showed a balance between men and women. However, the conclusion of the present series is still appropriate for the general population because the outcome factors such as the severity of CS and degree of satisfaction were unrelated to gender in the multivariate analyses (P = 0.463 and 0.983). Other predictive factors such as age, family history, and presence of gustatory sweating were also studied; no relationships to the severity of CS and degree of satisfaction were found. Considering the limitations of a retrospective study such as ours, we strongly advocate the organization of a randomized prospective trial and quality-of-life protocols on this topic because ETS4 was a viable option in our present series and past studies.1,6,10–12
CONCLUSIONS
We consider that T4 level is now the level most indicated for treating palmar hyperhidrosis. When compared with ETS2 and ETS3, ETS4 serves the purpose in solving excessive palmar sweating. Furthermore, ETS4 reduces the occurrence and severity of CS, provides mildly moist rather than fissured palms, minimizes regret after the operation, and results in general satisfaction about quality of life. Meanwhile, palmar overdryness was an important factor that affects the degree of satisfaction after sympathectomy. There was no association between obesity and presence of CS; however, obese individuals who are scheduled for sympathectomy should be informed of the likelihood of increased severity of CS. Patient satisfaction might decrease gradually as time goes on no matter which level of sympathetic ganglion was transected.
ACKNOWLEDGMENTS
The authors thank the Statistical Analysis Laboratory, Department of Clinical Research, Kaohsiung Medical University Hospital for their help.
Footnotes
Reprints: Shah-Hwa Chou, MD, Division of Thoracic Surgery, Department of Surgery, Kaohsiung Medical University Hospital, Kaohsiung Medical University,100 Tzyou 1st Road, Kaohsiung 80708, Taiwan. E-mail: shhwch@cc.kmu.edu.tw.
REFERENCES
- 1.Panhofer P, Zacherl J, Jakesz R, et al. Improved quality of life after sympathetic block for upper limb hyperhidrosis. Br J Surg. 2006;93:582–586. [DOI] [PubMed] [Google Scholar]
- 2.Dewey TM, Herbert MA, Hill SL, et al. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg. 2006;81:1227–1232. [DOI] [PubMed] [Google Scholar]
- 3.Yoon SH, Rim DC. The selective T3 sympathicotomy in patients with essential palmar hyperhidrosis. Acta Neurochir (Wien). 2003;145:467–471. [DOI] [PubMed] [Google Scholar]
- 4.Yoon DH, Ha Y, Park YG, et al. Thoracoscopic limited T-3 sympathicotomy for primary hyperhidrosis: prevention for compensatory hyperhidrosis. J Neurosurg. 2003;99(1 suppl):39–43. [DOI] [PubMed] [Google Scholar]
- 5.Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol. 2001;90:161–166. [PubMed] [Google Scholar]
- 6.Chou SH, Kao EL, Lin CC, et al. The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc. 2006;20:1749–1753. [DOI] [PubMed] [Google Scholar]
- 7.Arnold WS, Daniel TM. Thoracoscopic sympathectomy. In: Shields TW, LoCicero J III, Ponn RB, et al, eds. General Thoracic Surgery. Philadelphia: Lippincott Williams and Wilkins; 2005;698–702. [Google Scholar]
- 8.Chiou TS, Chen SC. Intermediate-term results of endoscopic transaxillary T2 sympathectomy for primary palmar hyperhidrosis. Br J Surg. 1999;86:45–47. [DOI] [PubMed] [Google Scholar]
- 9.Chou SH, Lee SH, Kao EL. Thoracic endoscopic T2–T3 sympathectomy in palmar hyperhidrosis: experience of 112 cases. Surg Today. 1993;23:105–107. [DOI] [PubMed] [Google Scholar]
- 10.Chou SH, Kao EL, Li HP, et al. T4 sympathectomy for palmar hyperhidrosis: an effective approach that simultaneously minimizes compensatory hyperhidrosis. Kaohsiung J Med Sci. 2005;21:310–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neumayer C, Zacherl J, Holak G, et al. Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb: reduction of compensatory sweating by clipping T4. Surg Endosc. 2004;18:152–156. [DOI] [PubMed] [Google Scholar]
- 12.Choi BC, Lee YC, Sim SB. Treatment of palmar hyperhidrosis by endoscopic clipping of the upper part of the T4 sympathetic ganglion. Preliminary results. Clin Auton Res. 2003;13:S48–S51. [DOI] [PubMed] [Google Scholar]
- 13.de Campos JR, Kauffman P, Werebe Ede C, et al. Quality of life, before and after thoracic sympathectomy: report on 378 operated patients. Ann Thorac Surg. 2003;76:886–891. [DOI] [PubMed] [Google Scholar]
- 14.Licht PB, Pilegaard HK. Gustatory side effects after thoracoscopic sympathectomy. Ann Thorac Surg. 2006;81:1043–1047. [DOI] [PubMed] [Google Scholar]
- 15.Reisfeld R. Sympathectomy for hyperhidrosis: should we place the clamps at T2–T3 or T3–T4? Clin Auton Res. 2006;16:384–389. [DOI] [PubMed] [Google Scholar]
- 16.Yazbek G, Wolosker N, de Campos JR, et al. Palmar hyperhidrosis—which is the best level of denervation using video-assisted thoracoscopic sympathectomy: T2 or T3 ganglion? J Vasc Surg. 2005;42:281–285. [DOI] [PubMed] [Google Scholar]
- 17.Dumont P, Denoyer A, Robin P. Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg. 2004;78:1801–1807. [DOI] [PubMed] [Google Scholar]
- 18.Adar R, Kurchin A, Zweig A, et al. Palmar hyperhidrosis and its surgical treatment: a report of 100 cases. Ann Surg. 1977;186:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Campos JR, Wolosker N, Takeda FR, et al. The body mass index and level of resection: predictive factors for compensatory sweating after sympathectomy. Clin Auton Res. 2005;15:116–120. [DOI] [PubMed] [Google Scholar]
- 20.Vetrugno R, Liguori R, Cortelli P, et al. Sympathetic skin response—basic mechanisms and clinical applications. Clin Auton Res. 2006;13:256–270. [DOI] [PubMed] [Google Scholar]
- 21.Reisfeld R, Nguyen R, Pnini A. Endoscopic thoracic sympathectomy for hyperhidrosis: experience with both cauterization and clamping methods. Surg Laparosc Endosc Percutan Tech. 2002;12:255–267. [DOI] [PubMed] [Google Scholar]






