Abstract
Objective:
To characterize the beneficial effects of perioperative systemic lidocaine on length of hospital stay, gastrointestinal motility, and the inflammatory response after colorectal surgery.
Summary Background Data:
Surgery-induced stimulation of the inflammatory response plays a major role in the development of several postoperative disorders. Local anesthetics possess anti-inflammatory activity and are thought to positively affect patients' outcome after surgery. This double-blinded, randomized, and placebo-controlled trial aimed to evaluate beneficial effects of systemic lidocaine and to provide insights into underlying mechanisms.
Methods:
Sixty patients undergoing colorectal surgery, not willing or unable to receive an epidural catheter, were randomly assigned to lidocaine or placebo treatment. Before induction of general anesthesia, an intravenous lidocaine bolus (1.5 mg/kg) was administered followed by a continuous lidocaine infusion (2 mg/min) until 4 hours postoperatively. Length of hospital stay, gastrointestinal motility, and pain scores were recorded and plasma levels or expression of pro- and anti-inflammatory mediators determined.
Results:
Lidocaine significantly accelerated return of bowel function and shortened length of hospital stay by one day. No difference could be observed in daily pain ratings. Elevated plasma levels of IL-6, IL-8, complement C3a, and IL-1ra as well as expression of CD11b, l- and P-selectin, and platelet-leukocyte aggregates were significantly attenuated by systemic lidocaine.
Conclusions:
Perioperative intravenous lidocaine not only improved gastrointestinal motility but also shortened length of hospital stay significantly. Anti-inflammatory activity modulating the surgery-induced stress response may be one potential mechanism. Systemic lidocaine may thus provide a convenient and inexpensive approach to improve outcome for patients not suitable for epidural anesthesia.
Stimulation of the inflammatory response plays a major role in patients' recovery and outcome after surgery. Perioperative systemic administration of lidocaine not only attenuates various pro-inflammatory mediators and accelerates return of gastrointestinal motility, but most importantly shortens length of hospital stay in patients undergoing colorectal surgery.
Major abdominal surgery elicits a broad variety of alterations in hemodynamic, endocrine-metabolic, and immune responses.1 Although inflammation is crucial for structural and functional repair of tissue damage, excessive stimulation of the inflammatory response has major impact on the development of several inflammatory disorders perioperatively, such as impaired gastrointestinal motility. Anesthetic interventions that modulate inflammatory responses might thus decrease frequency and severity of such complications, thereby minimizing morbidity and mortality.
Epidural administration of local anesthetics was initially designed to provide optimal perioperative anesthesia and analgesia, but numerous studies have shown that this anesthetic technique exerts far more effects than pain relief. As it attenuates the surgery-induced stress response and improves postoperative gastrointestinal function, epidural anesthesia has become a popular anesthetic strategy to improve outcome after major surgery.2 However, insertion of an epidural catheter is not without risks in certain patient populations. Especially patients after coronary stenting receive anticoagulant therapy and thus require careful assessment as to the risks and benefits of administering a regional anesthetic technique. Because of the strongly increasing numbers of these patients, alternative therapeutic interventions for optimal perioperative care are needed.
Local anesthetics, reabsorbed from the epidural space, may contribute to the beneficial nonanalgesic effects of epidural anesthesia. Originally known for inhibition of voltage-gated sodium channels, local anesthetics have significant anti-inflammatory properties and may allow modulation of excessive inflammatory responses without impairing the physiologic host defense.3 By characterizing the beneficial effects of intravenous lidocaine in patients undergoing colorectal surgery and identifying underlying mechanisms, systemic lidocaine may become a safe and alternative strategy for patients not willing or able to receive epidural anesthesia for improving perioperative outcome.4
METHODS
The study was carried out between September 2002 and December 2004 at the Departments of Anesthesiology and Surgery, University of Heidelberg, Germany, following ICH GCP guidelines. ELISA measurements of cytokines were conducted at the Department of Anesthesiology, University of Amsterdam, The Netherlands. After approval of the protocol by the Institutional review board of the University of Heidelberg and after obtaining written informed consent, we enrolled 60 patients of American Society of Anesthesiologists physical status I to III, and between 18 and 75 years of age, scheduled for elective colorectal surgery in this double-blinded, randomized, and placebo-controlled clinical trial. Inclusion criteria were refusal or contraindication for placement of an epidural catheter, whereas criteria for exclusion were known allergies to local anesthetics, chronic use of analgesics or corticosteroids, underlying inflammatory bowel disease (Crohn's disease or ulcerative colitis), prolonged postoperative ventilatory support, impaired liver function, and severe cardiac arrhythmia.
Patients were randomly assigned to either lidocaine or placebo treatment using the following multistep protocol to minimize effects of type and length of surgery. Dependent on the surgical procedure performed, patients were allocated to 2 different groups (colectomy vs. rectum resection). Each group was subdivided into blocks consisting of 6 patients. According to numbers on a drawn lot, patients were assigned to the lidocaine or placebo groups subsequently. Both groups were randomized separately and blockwise.
The study medication was prepared by an anesthesiologist not involved in further treatment of the patients. The anesthesia team and all other staff involved in patient care were blinded to study group assignments.
One day before surgery, all patients were instructed how to use a patient controlled analgesia (PCA) pump and rate pain intensity on a visual analog scale (VAS), identifying 0 as “no pain” and 10 as “worst imaginable pain.” In addition, each patient was requested to record the first appearance of bowel sounds, flatus, and defecation postoperatively.
Perioperative Protocol
All anesthetic procedures were performed in a standardized fashion. For premedication, all patients received clorazepate dipotassium by mouth. Standard monitoring was applied and general anesthesia induced with fentanyl, propofol, and vecuronium. Anesthesia was maintained using sevoflurane and 40% oxygen in 60% nitrous oxide. Sevoflurane concentration was adjusted to keep blood pressure and heart rate within ±15% of baseline values. Mechanical ventilation facilitated normocapnia. Before surgical incision, a fentanyl bolus was administered and further analgesia was provided using continuous infusion of remifentanil individually adapted. Thirty minutes before the end of surgery, piritramide for postoperative analgesia was administered intravenously and all patients received dolasetron for postoperative nausea and vomiting prophylaxis. Train-of-four monitoring guided relaxation, facilitating extubation (train-of-four >90%) without using reversal agents. Normothermia was maintained during surgery using a warm touch warming system (Mallinckrodt Medical Inc., St. Louis, MO).
Study Drug Administration
Patients in the lidocaine group received 1.5 mg/kg lidocaine intravenously as a loading dose before induction of general anesthesia. Immediately after tracheal intubation, a continuous systemic lidocaine infusion (2 mg/min) was initiated and terminated 4 hours after skin closure. Patients in the control group were treated likewise using NaCl 0.9% in a double-blinded fashion.
PACU and Postoperative Care
After surgery, patients were transferred to the postoperative anesthesia care unit (PACU) and discharged not earlier than 30 minutes after completion of lidocaine/saline treatment. PCA devices were adjusted to a demand dose of 2 mg piritramide and a lockout period of 10 minutes without basal infusion. Additionally, after transfer to the ward, 1 g metamizol or in case of contraindications 1 g paracetamol was given every 6 hours. Diet was advanced according to the fast-track concept established at our institution, facilitating solid food intake as soon as possible.
Outcome Measures
The primary outcome measure was length of hospital stay. Secondary outcome measures included length of PACU stay, time until return of bowel function, postoperative pain and opioid consumption, plasma levels of several pro- and anti-inflammatory interleukins ([IL]-6, IL-8, IL-1β, TNF-α and IL-1ra, IL-10, respectively), complement C3a, leukocyte activation (CD11b, CD62L, CD62P) as well as platelet-leukocyte-interactions (PLAs).
Data Collection
Lidocaine plasma levels were determined at 5 minutes, 2 hours, and 4 hours after application of the loading dose, using high-pressure liquid chromatography.
Time until discharge from PACU was evaluated every 15 minutes by assessment of the Aldrete score.5 Aldrete ≥8 defined readiness for discharge. To determine return of gastrointestinal motility, bowel sounds were auscultated and patients asked twice daily if first flatus and defecation had occurred. Nausea, vomiting, type of diet, wound healing disturbances, and surgery-related complications were recorded. Pain intensities at rest and during coughing were measured using a VAS at 2 and 4 hours postoperatively as well as every 12 hours on the following days. Opioid demand by PCA was monitored daily. Length of hospital stay was determined as time until patients met standardized discharge criteria according to our surgeons' protocol to exclude social factors delaying real discharge times. Discharge criteria include: return to light diet without nausea and vomiting, ability to self-care and mobilize or to be able to be cared for by existing-home arrangements, no signs of wound healing disturbances, absence of increased infectious parameters in blood chemistry, pain control with oral analgesics, and as bowel movements before discharge.
Blood samples for measurement of inflammatory cells and mediators were taken immediately before induction of anesthesia, at the end of surgery, 2 hours postoperatively, and on postoperative day (POD) 3.
Quantitative measurements of plasma cytokine levels were made using commercial “sandwich” enzyme-linked immunosorbent assay kits according to the manufacturer's instructions. IL-6, IL-8, IL-10, TNF-α, IL-1β (Quantikine, R&D Systems GmbH, Wiesbaden, Germany), IL-1ra (BioSource Deutschland, Solingen, Germany), and C3a (Quidel Deutschland, Marburg, Germany). Sensitivities of the assays used were 0.7, 4.4, 3.9, 0.5, 0.3, 4.0 pg/ml and 1.0 ng/ml, respectively. Intraassay and interassay coefficients of variation were all less than 10% in each measurement. Cross reactivity with other factors was negligible. Activation of leukocytes and PLAs was analyzed with a three-color FACSCalibur flow cytometer and CellQuestPro software (BD Bioscience, Heidelberg, Germany), using the following antibodies: anti-CD11b-FITC, anti-CD45-PE, anti-CD42b-FITC, anti-CD62L-FITC, anti-CD62P-PE: all Dako, Heidelberg, Germany, except anti-CD11b-FITC (Dianova, Hamburg, Germany) and anti-CD62P-PE (BD Bioscience). PLA formation is expressed as percentage of platelet-bound leukocytes. All samples and standards were run in duplicate.
Statistics
Statistical analysis was performed using SPSS version 12.0.2 for Windows (SPSS Inc., Chicago, IL). With respect to our primary endpoint, length of hospital stay, sample size analysis revealed a required number of patients of 28 per group (expected mean difference 1.0 day, expected standard deviation 1.3 days, based on data of Groudine et al,6 and our own pilot study; power 80%, P < 0.05). Baseline values were compared using Student t test, Wilcoxon test, and Fisher exact test. The effect of treatment on gastrointestinal motility, piritramide consumption, and length of hospital stay was analyzed by Student t test or Mann-Whitney U test, depending on distributional properties. Differences in cytokine plasma levels were assessed using repeated-measures analysis of variance and corrected with a post hoc Bonferroni test. Linear mixed modeling was performed to study the overall and time-dependent influence of lidocaine treatment on CD11b, CD62P/L, and PLA (relative to baseline). Akaike's information criterion was used to decide upon the best model fit. A P value <0.05 was considered to represent a significant difference. Data are mean ± SD or median with interquartile ranges, unless otherwise indicated.
RESULTS
Demographic Data
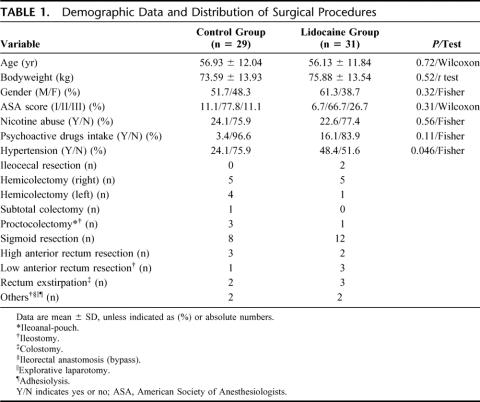
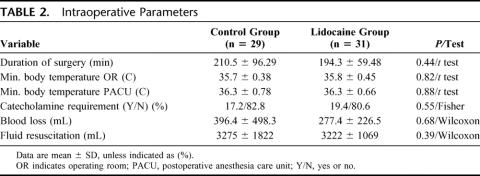
Seventy-seven patients undergoing elective colorectal surgery met our study criteria. Nine patients refused to participate, whereas delay of surgery led to exclusion of 2 patients. Thus, 66 patients were randomized and assigned equally to both groups. Because of intraoperative hypothermia, 2 patients in each group required prolonged ventilatory support and had to be excluded during the postoperative course. In addition, 2 patients of the control group dropped out because of preoperative unrecognized chronic drug abuse (analgesics). Altogether, 60 patients (29 in the control and 31 in the lidocaine group) completed the study and were analyzed (Fig. 1). The relevant demographic and intraoperative data are given in Tables 1 and 2, respectively. A significant proportion of patients in the lidocaine group presented with preexisting hypertension (P = 0.046), whereas in other aspects no significant differences between the groups could be observed. Colectomies and rectum resections were equally distributed, and one patient of each group underwent an additional hemihepatectomy.
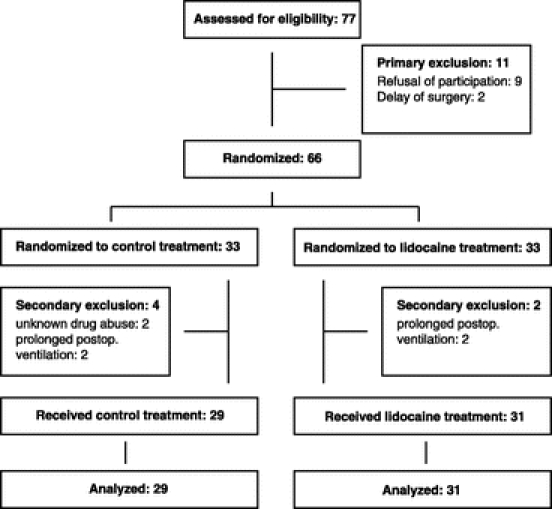
FIGURE 1. Study design according to the CONSORT statement.
TABLE 1. Demographic Data and Distribution of Surgical Procedures
TABLE 2. Intraoperative Parameters
Length of Hospital Stay
Analysis of the primary endpoint showed a significant difference (P = 0.004) in length of hospital stay; lidocaine-treated patients were discharged home 1 day earlier than their control counterparts: 7 days [6, 8] versus 8 days [7, 11] respectively (Fig. 2).
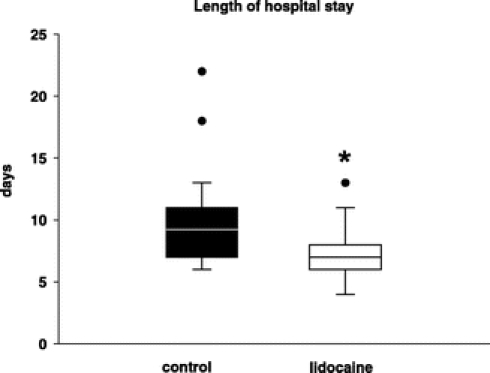
FIGURE 2. Effects of continuous administration of systemic lidocaine on length of hospital stay. Data are shown as median with 25th and 75th percentiles. *Statistical significance (P = 0.004) compared with control (Mann-Whitney U test).
Length of PACU Stay
There was no difference regarding length of PACU stay between groups (76 ± 74 and 84 ± 77 minutes for control and lidocaine patients, respectively).
Gastrointestinal Motility
Return of bowel function was significantly accelerated in patients receiving intravenous lidocaine. Bowel sounds and first flatus occurred approximately 8 hours earlier (Fig. 3a) compared with control and time until first defecation was significantly decreased in patients after administration of lidocaine (66.6 ± 26.4 vs. 82.1 ± 33.8 hours for control patients after surgery, P < 0.05, Fig. 3b). Time until tolerating solid food differed significantly between both groups (74.3 ± 23.2 hours for lidocaine-treated patients vs. 98.7 ± 27.1 hours for control patients; P < 0.001).
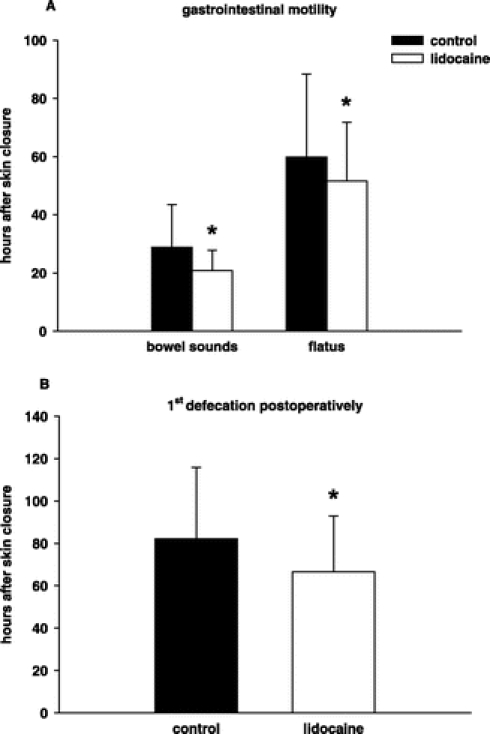
FIGURE 3. First occurrence of bowel sounds and flatus (A) and defecation (B) postoperatively. Data are mean ± SD. *Statistical significance (P < 0.05) compared with control (unpaired Student t test). Black bars, control patients; white bars, lidocaine-treated patients.
Pain Scores and Opioid Consumption
Pain intensities during rest and coughing did not differ between the groups, although a trend toward lower VAS scores was observed in lidocaine-treated patients (Fig. 4). The demand for piritramide in the postoperative period did not show any significant differences either, resulting in a similar overall piritramide consumption (106.4 ± 80.4 mg vs. 105.3 ± 101.9 mg for control and lidocaine group, respectively).
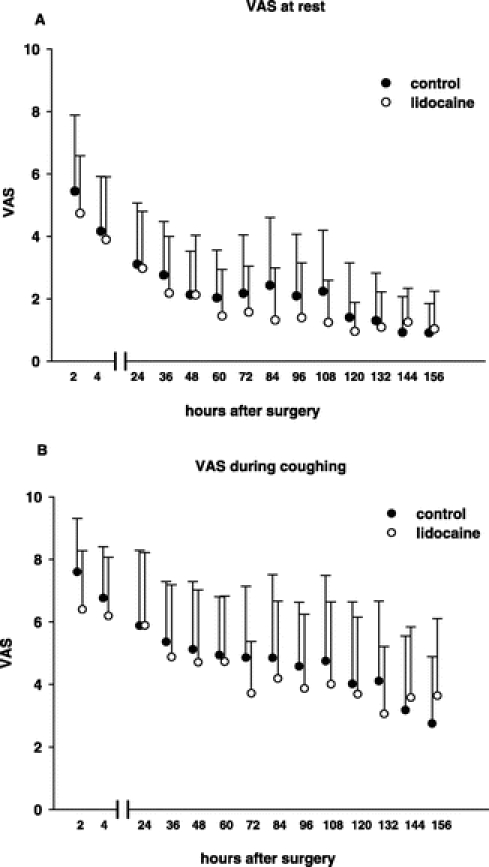
FIGURE 4. Visual analog scale (VAS) pain scores at rest (A) and during coughing (B). Data are mean ± SD. Black dots, control patients; white dots, lidocaine-treated patients.
Surgery-Related Complications
Hospital mortality was 0% in both groups, whereas morbidity was 34.5% (10 of 29) and 9.7% (3 of 31) for control and lidocaine-treated patients, respectively. Anastomotic leak occurred in one control patient but in none of the lidocaine-treated patients. Gastrointestinal atonia, defined as postoperative ileus >5 days, was found in 8 control patients compared with 2 patients in the lidocaine group. Wound healing disturbances occurred in 2 cases. One control patient developed a subphrenic abscess, whereas one patient receiving lidocaine showed minor signs of skin wound irritation, which did not require any surgical intervention.
Lidocaine Plasma Levels
Mean plasma levels of lidocaine were in the range of 1.1 to 4.2 μg/mL, with the exception of one patient presenting with a peak value of 5.8 μg/mL after lidocaine bolus administration. All patients started on the lidocaine infusion finished their full course of drug and did not experience any adverse events, such as arrhythmias or neurologic symptoms, related to the local anesthetic.
Cytokines, Integrins, and PLAs
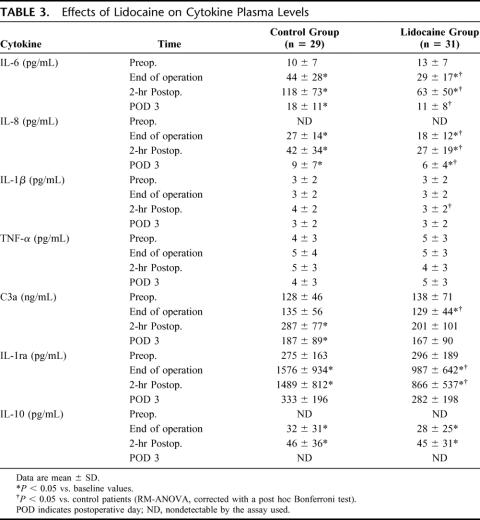
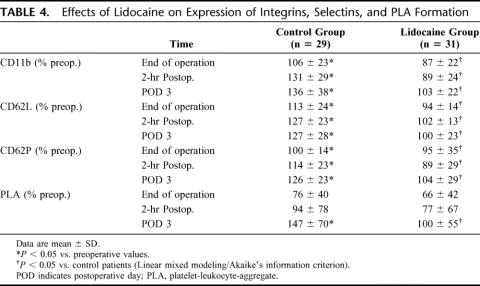
Systemic lidocaine significantly attenuated plasma levels of IL-6, IL-8, IL-1ra, complement C3a, as well as expression of CD11b, CD62L, CD62P and formation of PLAs. Plasma levels of TNF-α and IL-1β, however, did not increase in response to surgery, whereas IL-10 was not affected by the local anesthetic at any time point (Tables 3 and 4).
TABLE 3. Effects of Lidocaine on Cytokine Plasma Levels
TABLE 4. Effects of Lidocaine on Expression of Integrins, Selectins, and PLA Formation
DISCUSSION
Our study demonstrates that perioperative systemic administration of lidocaine significantly shortened length of hospital stay by 1 day in patients undergoing colorectal surgery.
The underlying mechanisms might be multifactorial. However, the accelerated return of bowel function seems to be a major contributor. Abdominal surgery is often accompanied by postoperative ileus; and despite its normally benign and self-limiting character, it is associated with patient discomfort, prolonged hospitalization, and increased postoperative morbidity. Prevention and/or treatment are difficult; thus, management remains mainly supportive.7 Postoperative ileus also has a significant economic impact since it results in additional costs of approximately $1 billion in the United States each year.8 Its etiology is complex and involves different mechanisms for initiation and prolongation. The acute phase is neurally mediated, whereas the late phase depends upon both leukocyte migration into the manipulated segment and subsequent activation of an inhibitory adrenergic pathway.7,9–11 Since inflammation plays a crucial role in sustaining postoperative ileus, intravenous local anesthetics may mediate their beneficial effects on promoting gastrointestinal motility by targeting different steps within this inflammatory cascade. Perioperative administration of lidocaine significantly attenuated the surgery-induced increase of complement and pro-inflammatory cytokines, such as IL-8 and IL-6. The latter is well known for its role in maintaining postoperative ileus and intestinal permeability disorders.12,13 Absence of an expected increase of IL-1β and TNF-α may have different reasons. Plasma levels of IL-1β may be low, although tissue damage is severe and the predefined schedule for sample measurements may have covered different cytokine peaks. However, in various studies, both cytokines have not been found to be elevated in patients undergoing different types of surgery.14–17 Lidocaine did not affect generation of the anti-inflammatory cytokine IL-10, but significantly attenuated plasma levels of IL-1ra. Since IL-1ra is an assumed marker for the presence of IL-1β, it may reflect otherwise nondetectable changes in IL-1β plasma levels due to lidocaine treatment. Yet, a direct effect of the local anesthetic on IL-1ra generation cannot be excluded. Recruitment of leukocytes to sites of inflammation requires multistep adhesive events that depend on the coordinated interactions of selectins, integrins, and adhesion molecules.18 Surgery-induced increased expression of L (CD62L)- and P (CD62P)-selectin as well as CD11b, the α subunit of leukocyte integrin MAC-1, was completely prevented by lidocaine. However, effects of local anesthetics on selectin expression remain controversial up to now.19,20 Inhibition of fMLP- or Staphylococcus aureus-induced CD11b expression in neutrophils has been documented more definitely, but concentrations required to achieve these effects exceed systemic concentrations at least 10- to 100-fold.21 Length of exposure (10–60 minutes in most in vitro studies19,21) might explain this difference since local anesthetics in the micromolar range are known to exert their anti-inflammatory properties in a time-dependent manner.22,23 Hence, the effect of low concentrations of local anesthetics on selectin and integrin expression in our study may result from the fact that lidocaine was administered continuously for at least 7 hours. Functional interactions of platelets and leukocytes play an important role in inflammation and thrombosis and could be detected in myocardial infarction or sepsis. Lidocaine treatment significantly reduced PLA formation. Underlying mechanisms may be many, but attenuated expression of P-selectin as one major contributor by lidocaine might be a promising candidate.24 If inflammation was severely disturbed, repair of tissue damage might be delayed and the incidence of postoperative complications potentially increased. In line with findings obtained in several in vivo studies, patients receiving lidocaine did not show seriously impaired wound healing in this trial.25 Altogether, lidocaine indeed may exert its beneficial effects on postoperative ileus by diminishing the inflammatory response, although our data have to be considered associative and additional mechanisms of action may exist.
Epidural anesthesia, using local anesthetics, is thought to promote gastrointestinal motility by inhibition of thoracolumbar sympathetic fibers and its opioid-sparing effects.26,27 It is unlikely, however, that sympathetic blockade is the main underlying mechanism for the effects of intravenous lidocaine. Concentrations of lidocaine required for inhibition of nerve conduction were shown to range between 60 and 100 μmol/L, whereas mean lidocaine plasma levels did not exceed 4.2 μg/mL (∼10 μM3) in the present study. An effect on opioid consumption cannot explain the findings either because VAS pain scores, rated at rest and during coughing, as well as piritramide consumption did not differ between both groups. This is in contrast to findings of Koppert et al, who showed attenuated postoperative pain and decreased morphine consumption after major abdominal surgery due to prevention of central hyperalgesia by intravenous lidocaine.28 There are obviously some limitations of the present study. Patients in this study underwent conventional colorectal surgery, although laparoscopy is frequently used for the surgical treatment of colorectal diseases and thought to better preserve immunity than open surgery.29 However, perioperative lidocaine is still able to positively affect postoperative ileus and outcome even if inflammation is less pronounced. Kaba et al found intravenous lidocaine to have similar beneficial effects on outcome as epidural anesthesia after laparoscopic colectomy.30 In this regard, length of hospital stay after colorectal surgery is of interest. Days spent in hospital after conventional surgery vary from 5 to 6 days in the United States and Scandinavia to 8 days and more in Germany and other European countries.31–34 Explanations for this difference may include a less stringent recovery program patients adhere to or organizational differences in postoperative care after discharge. Nevertheless, on the basis of available literature, lidocaine positively affects recovery and outcome data, even if hospital stay is shortened per se.6,30 Most recently, Kuo et al failed to find a difference regarding length of hospital stay in patients undergoing colorectal surgery, when comparing the effects of thoracic epidural anesthesia and intravenous lidocaine, though.35 As this study was powered for observing differences in postoperative opioid consumption, study groups may have been simply too small. Administration of lidocaine limited to the intraoperative period or weak exclusion criteria, such as permission of patients on corticosteroids, may have affected lidocaine's potential benefit additionally.
Although never reported for its intended use, systemic lidocaine may have undesired effects on several organ functions as it inhibits voltage-gated sodium channels, thereby interrupting nerve conduction. Proportional to its plasma levels, it may cause central nervous system stimulation, producing drowsiness and tremor or depresses myocardial function by decreasing electrical excitability and conduction rate. First clinical signs of toxicity, however, occur at considerably high concentrations (>5 μg/mL), not even achieved when intravenous lidocaine was given continuously over 14 days in case of severe migraine.36
CONCLUSION
Our results show that perioperative intravenous administration of lidocaine provides an inexpensive and convenient approach to attenuate the initiation of the excessive inflammatory response during colorectal surgery. Associated with a shortened hospital stay and improved patient comfort, systemic lidocaine may be of clinical interest with respect to economics and optimal perioperative management. The growing number of patients not suitable for neuraxial anesthesia could still benefit from the protective effects of local anesthetics but would not have to face the potential risks of epidural anesthesia.
ACKNOWLEDGMENTS
The authors thank Prof. Dr. Wolfgang S. Schlack (Department of Anesthesiology, Academic Medical Center Amsterdam, The Netherlands) for critically reviewing the manuscript, Ute Krauser for expert technical assistance, and Prof. Dr. Eike Martin (Department of Anesthesiology, University of Heidelberg, Germany) for his support.
Footnotes
Supported in part by the Medical Faculty, University of Heidelberg, Germany (F203699 to S.P. and M.W.H; F206639 to S.H. and M.W.H.) and by institutional money from the Department of Anesthesiology, University of Heidelberg, Germany.
Reprints: Markus W. Hollmann, MD, PhD, Department of Anesthesiology, Academic Medical Center Amsterdam, P.O. Box 22600, 1105 DD Amsterdam, The Netherlands. E-mail: M.W.Hollmann@amc.uva.nl.
REFERENCES
- 1.Herroeder S, Durieux ME, Hollmann MW. Inflammatory responses after surgery. Hosp Med. 2002;63:99–103. [DOI] [PubMed] [Google Scholar]
- 2.Kozian A, Schilling T, Hachenberg T. Non-analgetic effects of thoracic epidural anaesthesia. Curr Opin Anaesthesiol. 2005;18:29–34. [DOI] [PubMed] [Google Scholar]
- 3.Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: a new therapeutic indication? Anesthesiology. 2000;93:858–875. [DOI] [PubMed] [Google Scholar]
- 4.Hollmann MW, Strumper D, Durieux ME. The poor man's epidural: systemic local anesthetics for improving postoperative outcomes. Med Hypotheses. 2004;63:386–389. [DOI] [PubMed] [Google Scholar]
- 5.Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–934. [PubMed] [Google Scholar]
- 6.Groudine SB, Fisher HAG, Kaufman RP, et al. Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg. 1998;86:235–239. [DOI] [PubMed] [Google Scholar]
- 7.Bauer AJ, Boeckxstaens GE. Mechanisms of postoperative ileus. Neurogastroenterol Motil. 2004;16(Suppl 2):54–60. [DOI] [PubMed] [Google Scholar]
- 8.Prasad M, Matthews JB. Deflating postoperative ileus. Gastroenterology. 1999;117:489–492. [DOI] [PubMed] [Google Scholar]
- 9.de Jonge WJ, van den Wijngaard RM, The FO, et al. Postoperative ileus is maintained by intestinal immune infiltrates that activate inhibitory neural pathways in mice. Gastroenterology. 2003;125:1137–1147. [DOI] [PubMed] [Google Scholar]
- 10.Collins SM. The immunomodulation of enteric neuromuscular function: implications for motility and inflammatory disorders. Gastroenterology. 1996;111:1683–1699. [DOI] [PubMed] [Google Scholar]
- 11.The FO, de Jonge WJ, Bennink RJ, et al. The ICAM-1 antisense oligonucleotide ISIS-3082 prevents the development of postoperative ileus in mice. Br J Pharmacol. 2005;146:252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cruickshank AM, Fraser WD, Burns HJ, et al. Response of serum interleukin-6 in patients undergoing elective surgery of varying severity. Clin Sci (Lond). 1990;79:161–165. [DOI] [PubMed] [Google Scholar]
- 13.Wang W, Smail N, Wang P, et al. Increased gut permeability after hemorrhage is associated with upregulation of local and systemic IL-6. J Surg Res. 1998;79:39–46. [DOI] [PubMed] [Google Scholar]
- 14.Wu CT, Jao SW, Borel CO, et al. The effect of epidural clonidine on perioperative cytokine response, postoperative pain, and bowel function in patients undergoing colorectal surgery. Anesth Analg. 2004;99:502–509. [DOI] [PubMed] [Google Scholar]
- 15.Slotwinski R, Olszewski WL, Chaber A, et al. The soluble tumor necrosis factor receptor I is an early predictor of local infective complications after colorectal surgery. J Clin Immunol. 2002;22:289–296. [DOI] [PubMed] [Google Scholar]
- 16.Pruitt JH, Welborn MB, Edwards PD, et al. Increased soluble interleukin-1 type II receptor concentrations in postoperative patients and in patients with sepsis syndrome. Blood. 1996;87:3282–3288. [PubMed] [Google Scholar]
- 17.Keel M, Ecknauer E, Stocker R, et al. Different pattern of local and systemic release of proinflammatory and anti-inflammatory mediators in severely injured patients with chest trauma. J Trauma. 1996;40:907–912. [DOI] [PubMed] [Google Scholar]
- 18.von Andrian UH, Mackay CR. T-cell function and migration: two sides of the same coin. N Engl J Med. 2000;343:1020–1034. [DOI] [PubMed] [Google Scholar]
- 19.Martinsson T, Oda T, Fernvik E, et al. Ropivacaine inhibits leukocyte rolling, adhesion and CD11b/CD18 expression. J Pharmacol Exp Ther. 1997;283:59–65. [PubMed] [Google Scholar]
- 20.Chen Y, Ke Q, Xiao YF, et al. Cocaine and catecholamines enhance inflammatory cell retention in the coronary circulation of mice by upregulation of adhesion molecules. Am J Physiol Heart Circ Physiol. 2005;288:H2323–H2331. [DOI] [PubMed] [Google Scholar]
- 21.Kiefer RT, Ploppa A, Krueger WA, et al. Local anesthetics impair human granulocyte phagocytosis activity, oxidative burst, and CD11b expression in response to Staphylococcus aureus. Anesthesiology. 2003;98:842–848. [DOI] [PubMed] [Google Scholar]
- 22.Hollmann MW, Herroeder S, Kurz KS, et al. Time-dependent inhibition of G protein-coupled receptor signaling by local anesthetics. Anesthesiology. 2004;100:852–860. [DOI] [PubMed] [Google Scholar]
- 23.Kohrs R, Hoenemann CW, Feirer N, et al. Bupivacaine inhibits whole blood coagulation in vitro. Reg Anesth Pain Med. 1999;24:326–330. [DOI] [PubMed] [Google Scholar]
- 24.Rinder HM, Bonan JL, Rinder CS, et al. Dynamics of leukocyte-platelet adhesion in whole blood. Blood. 1991;78:1730–1737. [PubMed] [Google Scholar]
- 25.Drucker M, Cardenas E, Arizti P, et al. Experimental studies on the effect of lidocaine on wound healing. World J Surg. 1998;22:394–397. [DOI] [PubMed] [Google Scholar]
- 26.Bonnet F, Marret E. Influence of anaesthetic and analgesic techniques on outcome after surgery. Br J Anaesth. 2005;95:52–58. [DOI] [PubMed] [Google Scholar]
- 27.Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362:1921–1928. [DOI] [PubMed] [Google Scholar]
- 28.Koppert W, Weigand M, Neumann F, et al. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004;98:1050–1055. [DOI] [PubMed] [Google Scholar]
- 29.Buunen M, Gholghesaei M, Veldkamp R, et al. Stress response to laparoscopic surgery: a review. Surg Endosc. 2004;18:1022–1028. [DOI] [PubMed] [Google Scholar]
- 30.Kaba A, Detroz BJ, Laurent SR, et al. Acute rehabilitation program after laparoscopic colectomy using intravenous lidocaine. Acta Chir Belg. 2005;105:53–58. [PubMed] [Google Scholar]
- 31.Moiniche S, Bulow S, Hesselfeldt P, et al. Convalescence and hospital stay after colonic surgery with balanced analgesia, early oral feeding, and enforced mobilisation. Eur J Surg. 1995;161:283–288. [PubMed] [Google Scholar]
- 32.Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. [DOI] [PubMed] [Google Scholar]
- 33.Braga M, Vignali A, Gianotti L, et al. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002;236:759–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alves A, Panis Y, Slim K, et al. French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg. 2005;92:1520–1525. [DOI] [PubMed] [Google Scholar]
- 35.Kuo CP, Jao SW, Chen KM, et al. Comparison of the effects of thoracic epidural analgesia and i. v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006;97:640–646. [DOI] [PubMed] [Google Scholar]
- 36.Williams DR, Stark RJ. Intravenous lignocaine (lidocaine) infusion for the treatment of chronic daily headache with substantial medication overuse. Cephalalgia. 2003;23:963–971. [DOI] [PubMed] [Google Scholar]