Abstract
Background
Advanced Access has been strongly promoted as a means of improving access to general practice. Key principles include measuring demand, matching capacity to demand, managing demand in different ways and having contingency plans. Although not advocated by Advanced Access, some practices have also restricted availability of pre-booked appointments.
Aim
This study compares the strategies used to improve access by practices which do or do not operate Advanced Access.
Design of study
Postal survey of practices.
Setting
Three hundred and ninety-one practices in 12 primary care trusts.
Method
Questionnaires were posted to practice managers to collect data on practice characteristics, supply and demand of appointments, strategies employed to manage demand, and use of Advanced Access.
Results
Two hundred and forty-five from 391 (63%) practices returned a questionnaire and 162/241(67%) claimed to be using Advanced Access. There were few differences between characteristics of practices operating Advanced Access or not. Both types of practice had introduced a wide range of measures to improve access. The proportion of doctors' appointments only available for booking on the same day was higher in Advanced Access practices (40 versus 16%, difference = 24%, 95% CI = 16% to 32%). Less than half the practices claiming to operate Advanced Access ((63/140; 45%) used all four of this model's key principles.
Conclusion
The majority of practices in this sample claim to have introduced Advanced Access, but the degree of implementation is very variable. Advanced Access practices use more initiatives to measure and improve access than non-Advanced Access practices.
Keywords: appointments and schedules, family practice, health services accessibility, primary health care
INTRODUCTION
Improving access to services is fundamental to UK government health policy. The NHS Plan includes the targets that all patients should be able to see a primary care professional within 24 hours and a GP within 48 hours. To achieve this target, the government created a Primary Care Access Fund of £168 million in 2002–2003, with £48 million dedicated to improving access to primary care.1 A National Primary Care Collaborative was established under the direction of the National Primary Care Development Team to support practices in introducing change. The organisational approach strongly promoted by the collaborative was that of ‘Advanced Access’.2
This approach originated in the US and is based on applying insights from queuing theory and industry about how to reduce delays and achieve change in organisations.3 General practices were offered implementation and incentive payments if they used Advanced Access. Similar approaches are also being promoted in several other countries including the US and Australia.3–5
Advanced Access is based on several key principles: understanding demand (by measuring requests for consultations on different days of the week), matching capacity to demand (which may include changes to skill-mix), shaping the handling of demand by providing alternatives to face-to-face consultations, and developing contingency plans to cope with issues such as staff holidays or flu epidemics.2
The primary care collaborative encouraged practices to perform ‘plan-do-study-act’ cycles in order to implement changes to improve access which were tailored specifically to local needs and also to involve patients in planning changes.2 Although not advocated by the proponents of the Advanced Access approach,6 some practices have also restricted the booking of advance appointments7 and this change in particular has generated considerable controversy.8,9 Other aspects of Advanced Access have also raised concern, including claims that the emphasis on rapid access would disadvantage people such as the elderly and those with chronic illnesses for whom seeing a particular health professional may be a higher priority.10,11
By March 2003 the collaborative was working with about 2000 practices serving almost 11 million patients in England.12 Despite this investment in Advanced Access, very little independent evaluation has been conducted of the impact of this approach.13 A rapid evaluation of the first-wave of practices involved in the collaborative indicated that they had introduced a wide range of strategies to improve access and reported several benefits, but this finding was limited by the absence of a control group.14 This evaluation also suggested that these ‘firstwave’ practices were not representative of all practices, as they were more likely to be involved in vocational training, less likely to serve urban or deprived populations and more likely to have been fundholders.
The study reported here forms part of a larger controlled evaluation of Advanced Access in general practice. This paper examines the characteristics of practices which had adopted Advanced Access, the degree of implementation and the strategies that practices of different types have adopted to meet the demand for improved access to care.
METHOD
The survey was conducted between July and November 2004 in 12 primary care trusts (PCTs) which were purposefully selected to be representative of England in terms of age structure, ethnicity, unemployment, morbidity, practice size, and achievement of NHS access targets (Table 1). These PCTs included 391 practices serving approximately 2.3 million patients. A questionnaire was sent to each practice manager with two reminders sent at two weekly intervals.
Table 1.
Characteristics of population in primary care trusts studied
| Characteristic | Population of 12 PCTs in study % | England % |
|---|---|---|
| Age (%) | ||
| 0–4 yearsa | 5.9 | 6.0 |
| ≥75 years overa | 8.6 | 7.5 |
| Ethnicity (%) | ||
| White Britisha | 88.2 | 87.0 |
| Unemployment (%) | ||
| Aged 16–74 years unemployeda | 3.29 | 3.35 |
| Morbidity (%) | ||
| Limiting long-term illnessa | 18.8 | 17.9 |
| Practice size (n) | ||
| GPs per practiceb | 3.6 | 3.1 |
| NHS access target (%) | ||
| Patients offered an appointment to see a GP within 2 working days.c | 87.9 | 88.2 |
2001 census: http://neighbourhood.statistics.gov.uk/ (accessed 30 Oct 2006).
National database for primary care groups & trusts. Data 2001. http://www.primary-care-db.org.uk/ (accessed 30 Oct 2006).
2002/2003 NHS performance ratings www.chi.nhs.uk/ratings (accessed 30 Oct 2006).
The questionnaires consisted of a total of 23 questions divided into five sections to collect data about practice characteristics, demand and supply of appointments, interventions used to improve access, dealing with a backlog of appointments, and implementation of Advanced Access. The final page was left blank for additional comments. The questionnaire was piloted among practices in a different PCT area.
How this fits in
General practices are being encouraged to improve access to primary care using the ‘Advanced Access’ approach. There has been concern that some practices are meeting access targets by restricting pre-booked appointments. Two-thirds of practices in England claim to be operating Advanced Access but the degree of implementation is variable. Practices are using a wide range of strategies to improve access, whether or not they use Advanced Access. Advanced Access practices embargo a higher proportion of appointments until the same day compared with practices not operating Advanced Access.
Analysis
Practices which responded to the questionnaire were compared with those not responding using routinely collected General Medical Services statistics and Quality and Outcomes Framework data.15
Practices replying positively or negatively to the question ‘Does the practice consider that it is operating Advanced Access?’ were compared for each of the other questions using differences in means or odds ratios as appropriate, 95% confidence intervals and P-values.
RESULTS
The overall response rate was 63% (245/391). Practices responding to the questionnaire were less likely to be single-handed and more likely to be training practices than those not responding. There was no evidence of difference in their scores under the Quality and Outcomes Framework, and, in particular, no difference in their scores for patient access (Supplementary Table 1).
Advanced Access
Practices were asked the extent to which they were operating Advanced Access, using a 4-point scale. Almost a third of practices (31%; 75/241) claimed to operate Advanced Access ‘completely’, 36% (87/241) claimed to operate it ‘mostly’, 23% (56/241) claimed not to operate Advanced Access but had ‘used some Advanced Access ideas’ and 10% (23/241) claimed they did not use Advanced Access ‘at all’. The remaining analyses compare practices in the first two categories combined (Advanced Access) with those in the last two categories combined (non-Advanced Access). Approximately two thirds of practices claimed to be using Advanced Access ‘completely’ or ‘mostly’ (67%;162/241).
Practice characteristics
Practice characteristics are summarised in Supplementary Table 2. No differences were found between Advanced Access and non-Advanced Access practices in terms of practice size, location, approach to doctor continuity, contractual status, deprivation, training practice or previous fundholding status. Advanced Access practices were more likely to receive extra payments to improve access under the Directed Enhanced Service scheme.16
Matching capacity with demand
Practices were asked whether they had measured demand for appointments in the last year and if so whether the number of available appointments matched demand. A higher proportion of Advanced Access practices (136/160;85%) than non-Advanced Access practices (55/77;71%) had measured demand (odds ratio = 2.27, 95% confidence interval [CI] 1.17 to 4.38). Of those who had measured demand, a similar proportion of Advanced Access practices (57/120; 47%) and non-Advanced Access practices (21/44; 48%) indicated demand for face-to-face consultations matched the number of available appointments each week (odds ratio = 0.99, 95% CI = 0.50 to 1.98). However, Advanced Access practices were slightly more likely to have altered the total number of appointments offered to match demand (66/116; 57% versus 17/43; 39%, odds ratio = 2.02, 95% CI = 0.99 to 4.12) and to have introduced measures to handle demand differently (91/115; 79% versus 27/43; 63%, odds ratio = 2.25, 95% CI = 1.05 to 4.83).
Interventions to improve access
Both Advanced Access and nonAdvanced Access practices used many different strategies to improve access, summarised in Table 2. Advanced Access practices were more likely than nonAdvanced Access practices to offer telephone advice for new consultations, plan telephone consultations for some followup consultations, use specific measures to reduce follow-up, triage requests for home visits and to re-direct workload from GPs to healthcare assistants. Other interventions that have been recommended to improve access to care such as email consultations or providing information about self-care on practice websites were not widely used by either group of practices. Overall, the Advanced Access practices implemented more of the strategies listed in Table 2 than non-Advanced Access practices (mean number of strategies = 5.1 and 4.2, respectively, mean difference = 0.92, 95% CI = 0.33 to 1.51).
Table 2.
Strategies used to improve access.
| Advanced Access? | Comparison between Advanced Access and non-Advanced Access practices | ||||||
|---|---|---|---|---|---|---|---|
| Yes (n = 162)a | No (n = 79)a | ||||||
| n | % | n | % | Odds ratio | 95% CI | P-value | |
| Interventions used to improve access | |||||||
| Telephone advice for some new consultations | 104 | 66.2 | 38 | 48.1 | 2.12 | 1.22 to 3.68 | 0.008 |
| Planned telephone consultations for some follow-up consultations | 97 | 92.9 | 35 | 44.3 | 2.07 | 1.19 to 3.58 | 0.010 |
| Specific measures to reduce follow-up | 76 | 52.8 | 24 | 32.0 | 2.38 | 1.32 to 4.26 | 0.004 |
| Telephone triage by GPs | 84 | 52.5 | 36 | 45.6 | 1.32 | 0.77 to 2.67 | 0.314 |
| Telephone triage by nurses | 58 | 36.3 | 26 | 33.3 | 1.14 | 0.64 to 2.01 | 0.659 |
| Telephone triage for home visits | 128 | 80.5 | 54 | 68.4 | 1.91 | 1.03 to 3.54 | 0.039 |
| Nurse practitioners provide initial consultations for minor illness | 45 | 28.8 | 20 | 26.3 | 1.14 | 0.61 to 2.10 | 0.687 |
| Redirect workload from GPs to nurses | 120 | 75.0 | 59 | 74.7 | 1.02 | 0.55 to 1.89 | 0.958 |
| Redirect workload from GPs to healthcare assistants | 85 | 54.5 | 26 | 33.8 | 2.35 | 1.33 to 4.14 | 0.003 |
| Email consultations | 2 | 1.3 | 2 | 2.5 | 0.49 | 0.07 to 3.57 | 0.484 |
| Advice about self-care on practice website | 25 | 16.1 | 9 | 11.5 | 1.47 | 0.65 to 3.33 | 0.351 |
| Other recommended aspects of Advanced Access | |||||||
| Documented contingency plans | 79 | 51.0 | 34 | 43.0 | 1.39 | 0.89 to 2.40 | 0.232 |
| Most appointments available on Monday | 91 | 59.1 | 29 | 37.7 | 2.39 | 1.36 to 4.19 | 0.002 |
| Collect appointment data monthly | 126 | 78.3 | 50 | 64.1 | 2.02 | 1.11 to 3.66 | 0.021 |
| Involve patients in planning changes | 40 | 25.6 | 10 | 12.8 | 2.34 | 1.10 to 4.99 | 0.027 |
| Use plan-do-study-act cycles | 93 | 59.6 | 21 | 26.9 | 4.01 | 2.21 to 7.26 | <0.001 |
| Provide extra appointments to clear backlog | 95 | 62.5 | 29 | 36.7 | 2.70 | 1.53 to 4.79 | 0.001 |
| Participate in primary care collaborative | 109 | 72.7 | 29 | 39.7 | 4.03 | 2.23 to 7.28 | <0.001 |
The number of observations differs for each question depending upon the number of missing answers. The percentage given relates to the observations excluding missing data.
Other recommended aspects of Advanced Access
Table 2 also provides data about other strategies which are related to the Advanced Access approach. Advanced Access practices were more likely to offer the highest number of ‘same day’ appointments on a Monday, to involve patients in planning changes to the appointment system and to have provided extra consultations for a period to clear a backlog. They are also more likely to participate in the primary care collaborative and use ‘plan-do-study-act’ cycles to assess and implement changes.
Appointment availability
Practices were asked to calculate the total number of appointments available each week with GPs, nurse practitioners or nurses, assuming no-one was on holiday, and to provide data about the number which could be booked in advance of the same day. They were also asked about unscheduled workload (‘open’ surgeries and ‘extra’ patients), where patients arrived and waited without a specific appointment.
The mean proportion of doctors' appointments that could only be booked on the same day was much higher in the Advanced Access group than the non-Advanced Access group (41% versus 16%, difference 24%,16% to 32%) and 7% (10/144) of the Advanced Access practices did not offer any appointments with doctors which could be booked in advance of the same day, compared with none (0/77) of the non-Advanced Access practices (P = 0.033, Fisher's Exact test). Figure 1 shows the proportion of appointments with a doctor which could only be booked on the same day for the two types of practices. The total number of appointments available with doctors and with nurse practitioners was similar in the two groups of practices but non-Advanced Access practices offered a higher number of appointments with other types of nurses (Table 3).
Figure 1.
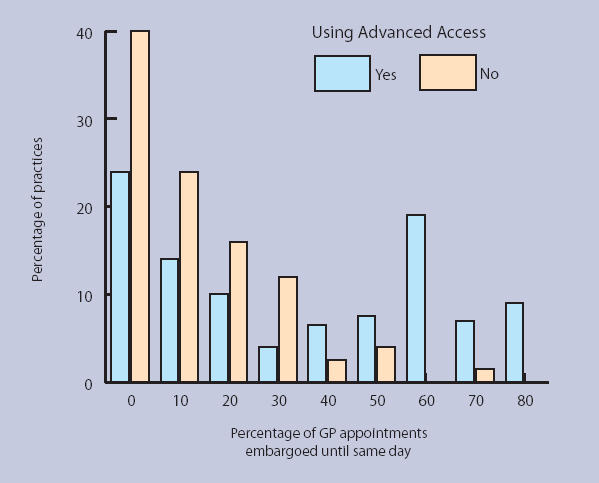
Percentage of doctors' appointments which could only be booked on the same day.
Table 3.
Appointments offered.
| Advanced Access? | |||||
|---|---|---|---|---|---|
| Yes (n = 162)b | No (n = 79)b | ||||
| Staff member | Mean number of appointments | Mean number of appointments | Difference | 95% CI | P-value |
| GP Appointments | |||||
| Pre-bookable | 34.4 | 51.7 | −17.32 | −25.13 to −9.51 | <0.001 |
| Same day | 24.3 | 10.2 | 14.12 | 8.61 to 19.64 | <0.001 |
| Total | 59.1 | 61.8 | −2.72 | −10.31 to 4.87 | 0.481 |
| Nurse practitioners | |||||
| Pre-bookable | 5.7 | 5.7 | −0.03 | −4.14 to 4.07 | 0.907 |
| Same day | 0.7 | 0.6 | 0.04 | −0.66 to 0.75 | 0.867 |
| Total | 6.4 | 6.4 | −0.03 | −4.49 to 4.42 | 0.988 |
| Other nurse | |||||
| Pre-bookable | 25.5 | 36.3 | −10.83 | −17.55 to −4.12 | 0.002 |
| Same day | 3.4 | 1.2 | 2.16 | 0.33 to 4.00 | 0.021 |
| Total | 29.3 | 37.5 | −8.19 | −15.38 to −1.01 | 0.026 |
| Same-day appointments | 28.3 | 12.0 | 16.32 | 10.05 to 22.58 | <0.001 |
| Total appointments offered | 97.6 | 106.3 | −8.76 | −21.28 to 3.75 | 0.169 |
| Unscheduled consultations | 7.6 | 5.7 | 1.84 | −2.00 to 5.68 | 0.345 |
Denominators vary because of missing data. In calculating same day appointments and total appointments practices were only included if they provided data for all relevant variables.
Four practices did not respond to the question about use of Advanced Access. Figures are mean number (SD) of appointments per 1000 registered patients.
Implementation of Advanced Access principles
The extent to which practices had implemented the key principles of Advanced Access varied for both groups of practices. As previously described, practices describing themselves as operating Advanced Access were more likely to measure demand for appointments (odds ratio = 2.27, 95% CI = 1.17 to 4.38). They were also more likely to have attempted to match capacity with demand either by making changes to the number of appointments or the ways in which care was delivered (odds ratio = 2.77, 95% CI = 1.44 to 5.32). Only half (79/154; 51%) of Advanced Access practices had explicit contingency plans, compared with 43% (34/79) of control practices (odds ratio = 1.39, 95% CI = 0.89 to 2.40), and almost all practices in both groups used a wide range of interventions to improve access (156/161 (97%) and 76/79 (96%) of practices respectively used at least one of the interventions listed in the top section of Table 4 (odds ratio = 1.23, 95% CI = 0.29 to 5.29). Fewer than half (63/140; 45%) the practices claiming to operate Advanced Access practices used all four of these key principles which are central to this approach, and a quarter (18/66; 27%) of the non-Advanced Access used all four principles (odds ratio = 2.18, 95% CI = 1.15 to 4.12).
DISCUSSION
Summary of main findings
In this large and representative sample of English general practices, the majority have adopted at least some elements of the ‘Advanced Access’ approach. These practices are working in a range of settings and have similar characteristics to practices not operating Advanced Access. This survey also demonstrates the wide range of innovative measures that practices, whether or not they operate Advanced Access, have introduced in an attempt to improve access to care for patients.
Although most practices claim to operate Advanced Access, fewer than half of these appear to be following all of the principles and strategies that are central to the Advanced Access approach. The concept of Advanced Access was clearly explained and disseminated through regional collaboratives, supported by facilitators in each primary care trust, but this study illustrates the way in which a clear centrally driven model can become diluted when it is widely implemented. Conversely, diffusion has also occurred, with many of the practices which are not operating Advanced Access using some of the same ideas (not necessarily as a result of the Advanced Access initiative). It is notable that some of the strategies that have been promoted to improve access have not been widely implemented. Surprisingly, practices operating Advanced Access did not appear to make greater use of skill mix. Technological approaches to improve access such as email consultations and advice on practice websites were rarely used, possibly because of concerns about medicolegal issues or increasing patient demand.17
There has been concern about the way in which some practices claiming to operate Advanced Access have embargoed future appointments.7–9,18 Despite official statements that this forms no part of the Advanced Access model,6 free-text comments on the questionnaire and our interviews with practice staff (not reported here) suggest there is widespread uncertainty about what ‘Advanced Access’ means, and confusion between Advanced Access and the 48-hour access target. In addition, the Advanced Access slogan of ‘doing today's work today’2,3 may have reinforced the perception that most appointments should be made on the day of request. In this study Advanced Access practices embargoed a higher proportion of doctors' appointments until the same day than non-Advanced Access practices, but relatively few practices embargoed all appointments and most appointments were available for booking in advance.
Concerns have been expressed that placing priority on seeing patients on the day of their choice under Advanced Access would fuel demand, increase practice workload and reduce continuity of care.19,20 There was no evidence in this study that practices operating Advanced Access offered more appointments or placed less emphasis on encouraging patients to see the same doctor.
Strengths and limitations of the study
This is the first study to explore the use of Advanced Access by a large and representative sample of general practices in England. The response rate of 63% is reasonably high for a survey of general practice staff, but the differences identified in the characteristics of practices which did or did not respond raises the possibility of bias if non-responding practices had a different approach to patient access. The fact that responding and non-responding practices had similar scores for patient access in the Quality and Outcomes Framework provides some reassurance in this regard.
Although the size of the survey was sufficient to detect large differences between practices there may be differences in other characteristics (such as the proportion of training practices) for which the power in this study, and hence the precision around the estimates, was insufficient to exclude the null. The study was not based on a formal power calculation, as it included all the practices which were available in the participating PCTs. Finally, some of the issues covered in the questionnaire, such as ‘triage’ and ‘measuring demand’ are hard to define and may have been interpreted differently by different participants.
This survey is based on the reports of practice managers and describes differences in the process of care and strategies used at different types of practice. We need to know whether these differences have an impact on important outcomes such as patients' experience of access to care, continuity, and practice workload, measured objectively. This will be addressed in future phases of this programme of research.
Implications for future research
The majority of practices have now introduced Advanced Access as an approach to improving access to primary health care. However, there has been both dilution and diffusion of the concept, with many of those claiming to operate Advanced Access not doing so fully, and many of those not operating Advanced Access applying similar ideas. Both types of practices are using a wide range of strategies to improve access to care. Future research will explore whether these changes are associated with improved access to care as well as the effect on other important outcomes.
Supplementary Material
Acknowledgments
We would like to thank the other members of the Advanced Access Evaluation Team: M. Wallace (University of Bristol), L. Simons, V. Lattimer, S. George, K. Gerard, C. Pope (University of Southampton), S. Edwards, H. Smith (University of Brighton), and M. Boudioni (London South Bank University) for their contribution to this part of the study. We are also grateful to Susan Hamilton for help with analysis of data to select study areas, all the practice managers who gave their time to complete the survey, and Andrew Wagner for access to GMS statistics about general practices.
Supplementary Information
Additional information accompanies this article at http://www.rcgp.org.uk/bjgp-suppinfo
Funding body
This project is funded by the NHS Research and Development Programme on Service and Delivery Organisation (SDO/70/2004). The views expressed in this publication are those of the authors and not necessarily those of the funders.
Ethics committee
The study had ethical approval from Thames Valley Multicentre Research Ethics Committee (04/12/024)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Department of Health. Achieving and sustaining improved access to Primary Care. London: Department of Health; 2002. http://www.dh.gov.uk/PolicyAndGuidance/OrganisationPolicy/PrimaryCare/PrimaryCareTrusts/PrimaryCareTrustsArticle/fs/en?CONTENT_ID=4016138&chk=gvOn07 (accessed 26 October 2006) [Google Scholar]
- 2.Oldham J. Advanced Access in primary care. Glossop: National Primary Care Development Team; 2001. http://www.npdt.org/AccesstoPrimaryCare/advancedaccess.pdf (accessed 10 Nov 2006) [Google Scholar]
- 3.Murray M, Berwick DM. Advanced Access. Reducing waiting and delays in primary care. JAMA. 2003;289(8):1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 4.Knight AW, Padgett J, George B, Datoo MR. Reduced waiting times for the GP: two examples of ‘advanced access’ in Australia. Med J Aust. 2005;183(2):101–103. doi: 10.5694/j.1326-5377.2005.tb06941.x. [DOI] [PubMed] [Google Scholar]
- 5.Solberg LI, Hroscikoski MC, Sperl-Hillen JM, et al. Key issues in transforming health care organizations for quality: the case of advanced access. Jt Comm J Qual Safety. 2004;30(1):15–24. doi: 10.1016/s1549-3741(04)30002-x. [DOI] [PubMed] [Google Scholar]
- 6.National Primary Care Development Team. Pre-bookable appointments. Manchester: NPDT; 2004. http://www.npdt.org/PreBookable.pdf (accessed 10 Nov 2006) [Google Scholar]
- 7.Health Commission. Survey of patients 2005: primary care trust. London: Healthcare Commission; 2005. [Google Scholar]
- 8.Anonymous. Patients denied advance bookings. http://news.bbc.co.uk/1/hi/health/4112390.stm (accessed 26 Oct 2006)
- 9.Department of Health. Patients get booking ‘guarantee’ on NHS GP appointments. http://www.dh.gov.uk/PublicationsAndStatistics/PressReleases/PressReleasesNotices/fs/en?CONTENT_ID=4118856&chk=PUcZZF (accessed 26 Oct 2006)
- 10.Rubin G, Bate A, George A, et al. Preferences for access to the GP: a discrete choice experiment. Br J Gen Pract. 2006;56:743–748. [PMC free article] [PubMed] [Google Scholar]
- 11.Nutting PA, Goodwin MA, Flocke SA, et al. Continuity of primary care: to whom does it matter and when? Ann Fam Med. 2003;1(3):149–155. doi: 10.1370/afm.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The National Primary Care Collaborative. National Primary Care Development Team. http://www.npdt.org/scripts/default.asp?site_id=5 (accessed 16 Jan 2006-no longer available)
- 13.Salisbury C. Does advanced access work for patients and practices? Br J Gen Pract. 2004;54(502):330–331. [PMC free article] [PubMed] [Google Scholar]
- 14.Pickin DM, O'Cathain A, Sampson F, Dixon S. Evaluation of ‘Advanced Access’ in the National Primary Care Collaborative. Br J Gen Pract. 2004;54:334–340. [PMC free article] [PubMed] [Google Scholar]
- 15.Health and Social Care Information Centre. Quality and Outcomes Framework 2004/05. http://www.ic.nhs.uk/services/qof/data/ (accessed 26 Oct 2006)
- 16.British Medical Association. Access to general medical services, Specification for a directed enhanced service. London: British Medical Association; 2003. [Google Scholar]
- 17.Car J, Sheikh A. Email consultations in health care: 2 — acceptability and safe application. BMJ. 2004;329(7463):439–442. doi: 10.1136/bmj.329.7463.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Windridge K, Tarrant C, Freeman GK, et al. Problems with a ‘target’ approach to access in primary care: a qualitative study. Br J Gen Pract. 2004;54(502):364–366. [PMC free article] [PubMed] [Google Scholar]
- 19.Craighead IB. Redesigning health care. Practices in UK are working harder, not more efficiently. BMJ. 2001;323:804. [PubMed] [Google Scholar]
- 20.Lamb A. Why ‘Advanced Access’ is a retrograde step. Br J Gen Pract. 2002;52:1035. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


