Abstract
Objective:
The objectives of this study were to examine whether girls with attention-deficit/hyperactivity disorder (ADHD) are at increased risk of having histories of abuse and to assess whether the presence of an abuse history may constitute a distinct subgroup of youth with ADHD.
Method:
We examined rates and correlates of child abuse in an ethnically and socioeconomically diverse sample of girls with attention-deficit/hyperactivity disorder (ADHD; n = 140) and a matched comparison sample of girls without ADHD (n = 88), all aged 6-12 years. A thorough chart review reliably established documented rates of physical and sexual abuse in both samples.
Results:
There were significantly higher rates of abuse for girls with ADHD (14.3%) than for the comparison sample (4.5%), with most of the abuse found in girls with the Combined as opposed to the Inattentive type. Higher rates of externalizing behaviors (including objective observations in a research summer camp) and peer rejection (indexed through peer sociometric nominations) characterized the subgroup of girls with ADHD with abuse histories compared to the subgroup without such histories, with moderate to large effect sizes. Subgroup differences regarding internalizing problems and cognitive deficits did not emerge. Findings regarding peer rejection were explained, in part, by higher rates of observed aggressive behavior in the abused subgroup.
Conclusions:
The findings raise important questions about the possible etiologic and/or exacerbating role of abusive trauma in a subgroup of children with ADHD.
Keywords: ADHD, Child abuse, Physical abuse, Sexual abuse, Aggression, Peer rejection
Introduction
The behavioral sequelae of child abuse and the symptoms and outcomes of children with attention-deficit/hyperactivity disorder (ADHD) share many features, including aggression and externalizing behavior, depression, and cognitive difficulties (e.g., Ethier, Lemelin, & Lachorite, 2004; Mannuzza & Klein, 1999). This overlap has sparked a recent debate as to the possible association between ADHD and child abuse (Ford et al., 2000; Wozniak et al., 1999), which raises issues of (a) the possible etiologic and exacerbating role of abuse in the development of ADHD and (b) the potential for abuse-related post-traumatic responses being misdiagnosed as ADHD. Our key objectives were to examine whether girls with ADHD were at increased risk of having histories of abuse and to assess whether those with abuse histories may constitute a distinct subgroup. We focus on the understudied population of girls with ADHD, given the clinical and conceptual importance of this group (Hinshaw & Blachman, 2005). Our objective is not to investigate the prevalence of abuse within a normative sample (e.g., Finkelhor, Ormrod, Turner, & Hamby, 2005) but, within a clinical sample, to examine clinical presentation and levels of crucial impairments when abuse and ADHD co-occur. We examined girls with ADHD because of the underrepresentation of females in extant research and because of the availability of the large data base that we have gathered on a well-characterized female sample (Hinshaw, 2002).
Child abuse and its sequelae
Increased aggression and externalizing problems, including hostility, difficulty with anger management, impulsivity, and physical attacks (Widom, 1997) are clearly linked to abuse (Cicchetti, Rogosch, Lynch, & Holt, 1993; Deater-Deckard & Dodge, 1997; Margolin & Gordis, 2000; Osofsky, 2003; Widom, 1997). Physical abuse has been most strongly and specifically linked to externalizing problems (Margolin & Gordis, 2000); sexual abuse has been more directly linked to childhood PTSD symptoms and later internalizing symptoms (Kendall-Tackett, Williams, & Finkelhor, 1993; Whiffen & MacIntosh, 2005). Yet sexual abuse predicts such specific externalizing behaviors as sexualized talk, preoccupation with sexual themes, sexual aggression toward other peers, and provocative behaviors at early ages, collectively termed “sexual acting out,” (Gil & Johnson, 1993; Margolin & Gordis, 2000).
Next, abuse is often damaging to a child’s self-perceptions and perceptions of the world, resulting in learned helplessness, anxiety, and depression (Kazdin, 1985), even to the point of increased self-destructive and suicidal behavior (Widom, 1997). Abused children also show evidence of poor social interactions and peer relationships. They are rated by their peers as more rejected, less popular, and more disruptive than children who have not been abused. Parents and teachers also rate abused children as socially rejected. Finally, abuse (Osofsky, 2003; Widom, 1997) and neglect (Margolin & Gordis, 2000; Osofsky, 2003) have been linked to both poor academic functioning and delayed cognitive development. On tests of verbal ability and comprehension, both physically abused and neglected children tend to score lower than non-abused comparison children. In sum, abused children present with externalizing and internalizing difficulties, compromised peer relations, and academic/cognitive impairments, yet specific mediators of such associations have yet to be elucidated.
ADHD and its sequelae
ADHD is a childhood disorder characterized by impairing and developmentally extreme levels of inattention, impulsivity, and hyperactivity and yielding a prevalence of 3-7% (American Psychiatric Association, 2000). It is predominantly a male disorder, with male to female ratios approximating 3:1 in the population at large (Hinshaw & Blachman, 2005). The study of ADHD has been overwhelmingly based on male samples, with focus on girls emerging relatively recently (Arnold, 1996; Gaub & Carlson, 1997; Hinshaw & Blachman, 2005).
ADHD affects children in many domains, including those that closely parallel the above-noted examples related to abuse: externalizing difficulties (Hinshaw, 1987), internalizing problems (Jensen, Martin, & Cantwell, 1997), compromised peer relationships (Hinshaw & Melnick, 1995), and problems in cognitive ability/academic performance (Hinshaw, 1992). The extensive literatures on each of these domains of impairment are vast. Indeed, the impairments related to ADHD are substantial and rates of comorbidity with both disruptive and internalizing disorders are far above chance (Angold, Costello, & Erkanli, 1999). Furthermore, peer rejection places children at substantial risk for continued social problems, academic underachievement, and behavioral problems (Parker & Asher, 1987), meaning that the impairments related to ADHD are probably overdetermined.
ADHD, parenting, and risk of abuse
ADHD is a condition for which high rates of heritability and evidence of neurobiological underpinnings strongly suggest neurodevelopmental origins (Tannock, 1998). This assertion is not meant to imply that school and family environments are unimportant in the development or maintenance of ADHD (Hinshaw, 1999); rather, it indicates that parenting is not likely to be a primary cause of ADHD. In addition, given the genetic underpinnings of many cases of ADHD, biological parents of children with ADHD are likely to show impulse control and attentional problems themselves (see review in Johnston & Mash, 2001), possibly increasing the likelihood of abusive behavior.
A substantial literature reveals that parents of children with ADHD experience more stress and more dysfunctional parent/child interaction styles than do parents of children without ADHD (Anastopoulos, Guevremont, Shelton, & DuPaul, 1992; Anderson, Hinshaw, & Simmel, 1994; Fischer, 1990; see review in Johnston & Mash, 2001). Furthermore, parents of children with ADHD report increased feelings of self-blame, incompetence, depression, and isolation (e.g., Nigg & Hinshaw, 1998). Not surprisingly, mothers of hyperactive children are separated or divorced more frequently than mothers of children without ADHD (Fischer, 1990).
Empirical link between ADHD and abuse
We have asserted that abuse and ADHD share the common features of externalizing and internalizing behavior problems, peer rejection, and cognitive difficulties. Furthermore, child abuse is defined by inappropriate reactions on the part of adults (often parents) against children, and families of children with ADHD are marked by dysfunctional interactional patterns. These similarities raise the question of a possible link between these two phenomena as well concerns about the differential diagnosis and treatment of each problem.
Wozniak et al. (1999) investigated whether children with ADHD are at increased risk of suffering from trauma as well as PTSD and related psychopathology. Their definition of trauma included child abuse as well as other traumatic events like accidents, combat, medical catastrophes, and physical attacks. They concluded that there were no meaningful associations between ADHD, trauma, and PTSD. However, they did not disaggregate their data by category of traumatic events, yet our examination of their tabulated data reveals that that 7% of their ADHD population had suffered from child abuse (including sexual abuse, physical abuse, and witnessing domestic violence) compared to 0.1% of their comparison sample. Also, they excluded adopted children, possibly leading to lowered rates of abuse Thus, their methods may have limited chances for finding links between abuse and ADHD.
Ford et al. (2000) examined the relationship between trauma exposure and both ADHD and oppositional defiant disorder (ODD). After screening admissions in an outpatient psychiatric facility for ADHD and ODD, they assessed children’s exposure to trauma and PTSD-related symptoms. Trauma was strongly linked to ODD: 45-73% of the ODD sample had been exposed to physical maltreatment, and 18-31% had been sexually maltreated. In contrast, 25% of the ADHD children were exposed to physical abuse and 11% exposed to sexual abuse. Tellingly, 91% of children with comorbid ADHD and ODD had a history of trauma (Ford et al., 2000). Thus, comorbidity of ADHD and disruptive behavior disorders may be a particularly strong correlate of abuse histories.
Objectives
Our first purpose was to extend a preliminary, descriptive finding of Hinshaw (2002) by examining whether a carefully diagnosed sample of preadolescent girls with ADHD showed higher rates of documented abuse than a matched comparison sample. Our second and more crucial objective was to document whether the subgroup of girls with ADHD and documented abuse was more impaired, in terms of externalizing and internalizing behavior problems, peer relations, and cognitive functioning, than the non-abused ADHD subgroup. We hypothesized that the ADHD-abused subgroup would display substantial impairments in each domain. A key feature of this investigation is the availability of multi-informant and multi-method data on key impairments. In addition to parent, teacher, and staff ratings, these included objective observations of externalizing behavior, validated self-reports and observations of internalizing behavior, peer sociometrics (as an indictor of social relations), and standardized cognitive tests. Finally, to elucidate relevant interactive processes and mechanisms, we examined whether any established linkages between abuse and peer rejection were mediated by tendencies of the abused subgroup to display aggressive behavior patterns. Because aggressive behavior has been causally linked to the development of peer rejection (e.g., Erhardt & Hinshaw, 1994), we tested whether aggressive behavior might account for association between abuse and negative peer status.
Method
Overview of procedures
The present research was conducted as part of a 3-year, National Institute of Mental Health (NIMH)-funded, series of summer camp investigation of girls with ADHD, held in 1997, 1998, and 1999 (see Hinshaw, 2002, for details). After initial recruitment and screening of participants, written consent was obtained and families came to campus for an extensive in-person assessment, during which assessments of IQ and academic achievement, as well as interviews and checklists of internalizing and externalizing behavior, were gathered (see Hinshaw, 2002, for details of recruitment and consent issues). The research summer camps were 5 weeks in length, conducted in 1997, 1998, and 1999. Each cohort had a total of 75-80 girls, approximately 60% with ADHD and 40% comparison girls. The girls were divided into three groups/classes according to ages (younger 6-8, middle 8.5-10 and older 11-12.5 years old) for all activities, with ADHD and comparison participants intermixed; daily events included classroom, physical education, drama, and art-periods. The full protocol for these programs was approved by the University of California, Berkeley, Committee for Protection of Human Subjects. Observations of the girls (while unmedicated) by trained observers, blind to diagnostic status, yielded additional, objective measures of internalizing and externalizing behaviors. Sociometric interviews were also conducted (Blachman & Hinshaw, 2002). Hinshaw, Carte, Sami, Treuting, and Zupan (2002) describe salient neuropsychological findings, but this is the first examination of the correlates of abuse status.
Participants
Two hundred and twenty eight girls (140 girls with ADHD and 88 without ADHD) between the ages of 6 and 12 were recruited through letters to pediatricians, mental health resources in the community, contacts with principals, guidance counselors, parent support groups, and advertisements in local newspapers and periodicals. For the ADHD group, an initial eligibility requirement was suspicion (if not documentation) of attentional problems. All girls received a full clinical workup to confirm the diagnosis of ADHD. Specifically, girls initially had to surpass cutoff scores on two highly reliable and widely used rating scales of ADHD---Child Behavior Checklist (CBCL) and Swanson, Nolan, and Pelham Rating Scale (SNAP)---and then meet full criteria for ADHD on the parent-administered Diagnostic Interview Schedule for Children, Version IV (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The sample included 93 girls with ADHD-combined type and 47 with ADHD-inattentive type. However, given the small sample sizes of abused children in the Inattentive subtype, we performed our primary ADHD versus comparison analyses merging the ADHD types. For complete details of screening and diagnostic procedures, see Hinshaw (2002). Although 50% of the girls with ADHD had previously received medication for their behavioral problems, all participated for most of the summer camp periods off medication. For those who participated in a medication trial during the program, all observations and ratings reported herein reflect unmedicated behavior patterns only. Comparison girls were required to be between the same ages and could not meet criteria for ADHD on the above-noted ratings scales and structured interview. All children had IQ scores over 70.
The sample was ethnically diverse: 53% White, 27% Black, 11% Latina, and 9% Asian-American/Pacific Islander. The ADHD and comparison groups did not differ significantly on any demographic variable except for rates of adoption (higher in the ADHD group; see Table 1 for demographics).
Table 1.
Demographic and Background Variables for ADHD and Comparison Groups
| Variable | ADHD(N=140)M (SD) | Comparison(N=88)M (SD) | p |
|---|---|---|---|
| Age (Months) | 116.0 (20.2) | 113.2 (19.8) | Ns |
| Income (1-9) | 6.2 (2.7) | 6.7 (2.5) | Ns |
| Maternal Education | 4.7 (1.0) | 4.9 (1.0) | Ns |
| White (%) | 56.7 | 46.6 | Ns |
| Public assistance (%) | 15.0 | 11.4 | Ns |
| Two-parent household (%) | 66.3 | 77.3 | Ns |
| Adopted (%) | 21.9 | 4.5 | <.01 |
Note: Comparisons made by independent-sample t-tests for continuous variables or X2 tests for categorical variables.
Abuse determination
Six trained raters examined the charts of all participants to probe for indications of abuse. The charts contained basic background information on the child and her family, as well as the CBCL and Teacher Report Form (TRF). All parents had been asked about significant or concerning events in the child’s life, such as out-of-home placement or indications of abuse; these data were documented in the chart. The CBCL and TRF each contain one specific question regarding sexualized behavior, as well as an open-ended question for parents and teachers to address concerns about the child. The raters examined only the sexualized behavior questions and the open-ended questions of the CBCL and TRF. Note that the charts did not include staff ratings, behavioral observations, self-report measures from the girl, cognitive tests, or peer sociometrics, all of which are used as the criterion variables in this investigation. Furthermore, the charts did not distinguish the ADHD versus comparison status of the participants. For all girls with ADHD and most of the comparison girls, the charts included a psychological report written by camp staff that noted impressions of the child’s behavior, some background history of the child, and recommendations for the family. The charts also included clinically relevant information (e.g., other psychological reports or Child Protective Services reports).
Raters were trained to look specifically for (a) statements indicating that the child had been abused, (b) any CPS reports, and (c) clinical notes from staff. Each rater completed a “hotsheet” for each participant designed to serve as a sensitive measure of abuse. If raters came across information in the chart such as a clinical report or staff notes about disturbing behavior, the rater would document the information, noting what was said and where that information was found.
The rater would also document any information regarding when abuse occurred (age of the child), who committed the abuse, and the type of abuse. The hotsheet ratings (presence of abuse, type of abuse, perpetrator, and age when the abuse occurred) were reliably scored across independent raters, with kappas ranging from .61-.82.
Next, the principal investigator and project director conducted a blind clinical consensus review of (a) the charts found to have any indications of abuse and (b) other, randomly selected charts not so designated. From this chart review, those cases containing only behavioral indications of abuse (i.e., extreme sexual acting out, or aggression) were eliminated from consideration. Thus, none of the cases designated as positive for abuse was defined solely on the basis of behavioral manifestations, to avoid conflating abuse and externalizing symptomatology (one of the key criterion variables). Substantiation of abuse could occur for the following reasons: (a) Child Protective Services reports (5 cases), (b) substantiated parent reports (15 cases), or (c) reports of abuse from psychological reports from school districts or prior treating clinicians (4 cases) (N = 24). Eight of the 24 girls with documented abuse were exposed to trauma before the age of 3 years, eight between 3-5 years, and the remaining eight between 6-10 years.
Criterion measures
We sampled four domains of functioning---externalizing behavior, internalizing behavior, peer appraisal, and cognitive/achievement scores---via multiple methods and informants. Objective information (direct observation, peer report, test data) supplemented adult informant report when possible, an important feature given that the independent variable of abuse status was generated largely through parental report.
Externalizing.
Parent:
Parents in the initial pre-camp assessment reported on their children’s internalizing and externalizing behavior patterns as well as other psychopathology. The CBCL is a widely used, well-established psychometric tool used to assess child internalizing and externalizing behavior problems (Achenbach, 1991). This measure contains 113 items and yields broad-band Externalizing (and Internalizing) dimensions. The Externalizing scale reflects impulsive, delinquent, aggressive, and disruptive behaviors; it incorporates the narrow-band Aggressive Behavior and Delinquent Behavior scales. The narrow-band Sex Problems scale was also used to assess sexualized behaviors such as talking about sex too much, knowing more than age appropriate about sex, and preoccupation with sexual themes. The psychometric properties of these scales are excellent (Achenbach, 1991).
Teacher:
Teachers reported on children’s behavior using a parallel measure to the above CBCL, the Teacher Report Form (TRF) Externalizing scale. (There is no parallel Sex Problems scale for the TRF.) This scale has been found to have a test-retest reliability of .91, and high convergent validity with alternative rating scales for externalizing behavior (Achenbach, 1991).
Observation:
Teams of trained raters, blind to medication and diagnostic status, observed 1 hour periods of class or playground activities multiple times per week during each summer camp (see Hinshaw, 2002). The raters were linked by headphones and were cued by a tape that would indicate when to find, observe, and record child behavior. The child’s behavior, observed in 5-second intervals, was coded into six mutually exclusive categories: noncompliance, verbal or physical aggression, social isolation, compliance, and prosocial behavior. The two categories used in this study were noncompliance and the combined category of verbal and physical aggression, for which occurrence-only agreement percentages ranged from .65-.72 (Hinshaw, 2002; Hinshaw, Zupan, Simmel, Nigg, & Melnick, 1997). Noncompliance behavior was defined as annoying, rule-violating, and intrusive behavior. Verbal aggression included taunts, swearing, or harsh words directed at peers or adults; physical aggression by hitting, kicking, shoving behaviors, or threats of the same. Both categories were proportion scores (i.e., number of instances divided by total of intervals).
Internalizing behavior.
Parent and teacher report:
The Internalizing broadband scale from the CBCL and TRF comprised the adult informant measures of this domain. This broadband scale is composed of the narrowband Withdrawn behavior, Somatic Concerns, and Anxiety/Depression scales. Excellent psychometric properties are associated with the Internalizing scale (Achenbach, 1991).
Self report:
The Children’s Depression Inventory (CDI) is a widely used and well-established self-report measure for children, which was developed to tap into children’s depressive symptomatology. This measure consists of 27 items, each rated on a 0-2 metric, spanning school failure, peer relationship difficulties, suicidal ideation, self worth and other aspects of depression. This is a sound psychometric instrument, with established test-retest reliability, construct validity, and long-term predictive validity (Kovacs, 1992).
Observation:
From the observation system described above, the relevant category is termed social isolation, defined as intervals during which a girl was not engaged in ongoing activities, through being on the periphery or wandered away from the activity. There was marginal interobserver agreement for this observation code (r = .5; Hinshaw, 2002).
Peer status.
At the end of the first, third, fifth weeks of camp, private interviews were held in which each girl was individually asked to nominate three classmates who fit certain behavioral descriptions or who were particularly valued or disliked (see Blachman & Hinshaw, 2002, for details). To facilitate these sociometric procedures, participants were shown picture boards with head and shoulders pictures of each classmate. The two scores used to index peer status were (a) positive nominations (the three children nominated as “liked”) and (b) negative nominations (the three children nominated as “disliked”). Because of the slightly different numbers of girls in each classroom, we calculated proportion scores (number of girls nominated divided by total number of classmates). These scores were stable, with a correlation between Week 1 and Week 5 of r = .51 for positive nominations and r = .85 for negative nominations (Blachman & Hinshaw, 2002).
Cognitive performance and academic achievement.
The Wechsler Intelligence Scale for Children (WISC) is the most widely used and psychometrically sound assessment of children’s IQ. We administered the third edition (WISC-III; Wechsler, 1991) and use the two key subscales of Verbal IQ (VIQ) and Performance IQ (PIQ). For academic achievement we analyzed the math and reading subscales of the screener version of the Wechsler Individual Achievement Test (WIAT; Wechsler, 1992). This test is also widely used, shares the same standardization sample as the WISC-III, and has sound psychometric properties.
Data analytic plan
To address the first hypothesis, that girls with ADHD would have stronger likelihood of abuse histories than the comparison sample, we performed a chi-square test on the cross-classification of ADHD diagnostic status with abuse status. For the second hypothesis, that the ADHD and abuse subgroup would display substantial impairments in key domains of functioning, we performed a series of multivariate analyses of variance (MANOVAs) for each of the four domains of criterion variables (externalizing behavior, internalizing behavior, peer status, and cognitive functioning). The dichotomous independent variable was the ADHD and abuse subgroup versus the ADHD without abuse subgroup. A significant multivariate group difference afforded independent-sample t-tests (or Fisher exact tests for categorical variables) for each of the separate measures within a domain, in order to ascertain the specific differences between abused and non-abused subgroups of girls with ADHD. We retained an alpha of .05 but we emphasize effect sizes (ES, calculated as Cohen’s d; Cohen, 1988) for all contrasts.
Results
Of the 24 cases with abuse histories, four were comparison girls (4.5% of comparison sample) and 20 were girls with ADHD (14.4% of the ADHD sample). The chi-square test of this difference was significant, p < .05. The odds ratio was 3.5. As shown in Table 2, the ADHD sample had numerically higher rates of all types of abuse, most notably neglect and sexual abuse.
Table 2.
Rates of Abuse by ADHD and Comparison Groups
| Type of Abuse | ADHD (n=140) | Comparison (n=88) | Total (N=228) |
|---|---|---|---|
| Physical | 3 | 1 | 4 |
| Neglect | 4 | 0 | 4 |
| Sexual | 10 | 2 | 12 |
| Witnessed | |||
| domestic violence | 1 | 1 | 2 |
| Combination | 2 | 0 | 2 |
| Total | 20 | 4 | 24 |
The focus, therefore, shifts to how the abused group of girls with ADHD differs from the girls with ADHD without histories of abuse. Table 3 presents information on the two subgroups. First, in terms of demographics, the ADHD and abuse subgroup did not differ from their peers in terms of racial background, income, or adoptive status. (Note that among the 7 cases of adoption in the ADHD and abuse group, in each instance the abuse preceded the adoption, allowing us to assert temporal primacy of the abuse.) A higher percentage of the ADHD and abuse subgroup lived in single parent homes, Π2 (1, N = 140) = 4.44, p < .05. All girls in the ADHD and abuse subgroup had comorbid diagnoses of Oppositional Defiant Disorder (ODD), ascertained from the DISC-IV, whereas only about half of the ADHD girls without abuse had this diagnosis (p < .001).
Table 3.
Mean Scores of ADHD and Abuse and ADHD Non-abused Subgroups on Criterion Measures
| Variable | ADHD and abuse (N = 20) M (SD) | ADHD without abuse (N = 120) M (SD) | t/ Fisher exact test | p | d |
|---|---|---|---|---|---|
| Demographics1 | |||||
| White (%) | 50 | 57 | .63 | ||
| Two-parent household (%) | 45 | 69 | .04 | .04 | |
| Adopted (%) | 35 | 20 | .15 | .15 | |
| Income (1-9 scale) | 5.6 (2.6) | 6.3 (2.7) | -1.04 | .30 | |
| Externalizing | |||||
| % ODD1 | 100 | 57 | .00 | .00 | |
| Father CBCL Externalizing T | 68.15 (8.78) | 62.09 (10.78) | 1.93 | .06 | .58 |
| Mother CBCL Externalizing T | 71.75 (10.08) | 64.21 (10.02) | 3.11 | .00 | .75 |
| TRF Externalizing T | 71.32 (12.33) | 65.22 (9.94) | 2.40 | .02 | .59 |
| Father CBCL Sex Problems T | 61.73 (12.85) | 54.61 (8.21) | 1.79 | .10 | .81 |
| Mother CBCL Sex Problems T | 63.33 (13.59) | 56.58 (8.81) | 2.04 | .06 | .71 |
| Observed noncompliance (proportion) | .15 (.13) | .12 (.08) | 1.27 | .22 | .41 |
| Observed verbal + physical aggression (proportion) | .02 (.02) | .009 (.01) | 2.13 | .04 | .52 |
| Internalizing | |||||
| Dad CBCL Internalizing T | 65.85 (9.79) | 57.13 (11.15) | 2.67 | .01 | .79 |
| Mom CBCL Internalizing T | 65.40 (8.13) | 59.81 (10.33) | 2.30 | .02 | .56 |
| TRF Internalizing T | 64.11 (7.80) | 58.88 (9.45) | 2.29 | .02 | .57 |
| CDI | 10.0 (8.50) | 8.77 (6.11) | -.78 | .54 | .19 |
| Observed social isolation (proportion) | .02 (.02) | .03 (.03) | -1.01 | .32 | .25 |
| Sociometrics | |||||
| Negative nominations (proportion) | .32 (.23) | .16 (.19) | 3.39 | .00 | .82 |
| Positive nominations (proportion) | .08 (.09) | .10 (.09) | -1.17 | .24 | .28 |
| Cognitive | |||||
| WISC-III VIQ | 97.05 (12.83) | 100.76 (14.34) | -1.06 | .29 | .26 |
| WISC-III PIQ | 93.47 (13.76) | 100.38 (13.74) | -2.03 | .04 | .50 |
| WIAT Reading | 99.90 (14.02) | 102.10 (14.54) | -.629 | .53 | .15 |
| WIAT Math | 93.85 (13.69) | 98.15 (14.32) | -1.25 | .21 | .30 |
Except for income, demographic variables were contrasted by means of X2 tests, as was the percentage ODD variable. The 2-sided Fisher exact test is reported for these tests.
We now compare the two subgroups across the four outcome domains. For externalizing behavior, a MANOVA was conducted with abuse status as the independent variable and all of the externalizing measures (parent CBCL scores and TRF scores, observations of externalizing behavior, and peer ratings of aggression) as the criterion variables. The MANOVA was significant, F(9,89) = 2.4, p < .05, affording the testing of each criterion variable with a univariate t-test (see Table 3). The ADHD and abuse subgroup showed significantly more externalizing problems than their non-abused counterparts on the maternal CBCL Externalizing scale, the TRF Externalizing scale, peer ratings of aggressive behavior, and objective staff observations of noncompliant as well as aggressive behavior. The effect sizes for these comparisons were in the moderate to large range (Cohen, 1988).
For the internalizing domain, the dependent variables in the were the maternal CBCL Internalizing scale, the TRF Internalizing scale, observed social isolation, child reported depression (CDI), and the peer nominations of sadness. This MANOVA was not significant; F(6,91) = 1.79; ns; but we present univariate findings for descriptive purposes in Table 3.
For peer status, with positive and negative peer nominations as the dependent variables, the MANOVA was significant, F(2, 138) = 5.87; p < .005. Individual t-tests revealed that the ADHD and abuse group received significantly more negative nominations than the nonabused subgroup, with a large effect size (d = .82), but positive peer nominations did not distinguish the subgroups.
For cognitive functioning, the dependent measures were WISC PIQ and VIQ as well as WIAT math and reading scores. This MANOVA was not significant F(4, 132) = 1.05, ns, so that individual t-tests were not interpreted (see Table 3).
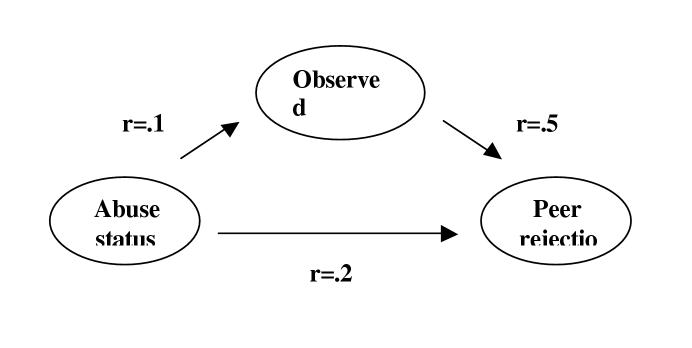
Although a formal test of a mediator process requires that the mediator occur in between the time of the predictor and the criterion variable (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001; for examples in the maltreatment literature, see Whiffen & MacIntosh, 2005), we examined whether measures of aggressive behavior would statistically “mediate” or account for the observed relation between abuse status and peer rejection (see Figure 1). To index aggression, we used the observational category of verbal and physical aggression; for the putative mediator variable of peer rejection, we utilized negative peer nominations. To test for such an effect, three initial conditions must be present (see Baron & Kenny, 1986): (a) an empirical relationship between the predictor and criterion variables (abuse and rejection), (b) an empirical relationship between the predictor and mediator variables (abuse and aggression), and (c) an empirical relationship between the mediator and criterion variables (aggression and rejection). All three were met: Abuse-aggression (r = .18, p < .05) and abuse-rejection (r = .28, p = < .01) linkages were significant, and aggression and rejection were substantially correlated at r = .50, p < .01.
Model Linking Predictor Variable (Abuse Status), Mediator Variable (Observed Aggression), and Criterion Variable (Peer Rejection)
Finally, for aggression to be considered a mediator, the relationship between abuse and rejection must be attenuated or disappear when the effect of aggression is controlled (Baron & Kenny, 1986). Multiple regression analyses revealed that when aggression was entered into the equation, the abuse-peer rejection relationship was significantly reduced in size. The Sobel test was used to indicate whether the relationship between abuse and rejection was significantly reduced by aggression. Tests utilizing the procedures found in Preacher and Leonardelli (2001) indicated that aggression partially mediated the relationship between abuse and rejection—that is, the reduction in the coefficients was significant when aggression was included, Z= 3.57, p < .01.
Discussion
We examined the rates of child abuse in a large and diverse sample of preadolescent girls with and without ADHD. First, we found that the girls with ADHD were at increased risk of having abuse histories. Second, those girls with ADHD and a history of abuse were distinct from their ADHD counterparts in terms of their levels of externalizing behavior and peer rejection. Specifically, the ADHD and abuse subgroup was viewed as significantly more aggressive according to parent, teacher, and peer report as well as objective observations of their behavior; they were also more rejected sociometrically than were the nonabused girls. We did not confirm our hypotheses, however, that the abused subgroup would show higher levels of internalizing behavior or cognitive deficits. We found that the linkage between abuse histories (within the ADHD sample) and peer rejection (indexed by negative peer nominations) was mediated in part by the high rates of aggressive behavior displayed by this subgroup. Finally, although 7 of the 20 girls with ADHD who had abuse histories were also adopted, in all cases the abuse preceded the adoption. Thus, our findings confirm the linkages found (but not reported per se) for boys in Wozniak et al. (1999).
Our findings documented high rates of externalizing behavior in the ADHD and abuse subgroup, across multiple informants and methods of measurement. Unknown, however, are the causal pathways. One possibility is that the combination of abuse and ADHD results in aggressive behavior as an additive function of both risk factors. That is, a combination of parental stress and distress plus difficult child temperament may set the stage for failures in caregiving, leading to abusive parenting, which accentuates aggressive child tendencies. Sequentially, it is conceivable that early trauma may predispose to later aggression, with the risk accentuated if the girl also displays the inattention and impulsivity that are part of the ADHD spectrum. Prospective investigations beginning much earlier in developmental histories are needed to understand such trajectories, as are studies with larger and more representative samples (e.g., Finkelhor & Hashina, 2001; Finkelhor et al., 2005). We note, however, that the majority of the abuse documented in this sample was sexual, rather than physical in nature; there are less clearly established pathways from sexual abuse to externalizing behavior than from physical abuse to such behavior (Margolin & Gordis, 2000). Clearly, our findings are in need of replication.
The second noteworthy subgroup effect was found for the domain of peer rejection: The abused subgroup showed a strong tendency to receive negative peer nominations from their classmates at the summer programs. ADHD and abuse status are each associated with risk for peer rejection; here, the combination of the two risk factors led to extremely high disapproval from classmates. Given that abuse histories in the sample tended to occur early in development (of the 24 girls, 16 had been exposed to trauma at or before the age of 5), it is plausible to assume that peer rejection is a consequence of abuse. Still, however, causal developmental pathways are not fully known. Overall, a possible synergistic effect regarding negative peer status appears to arise when ADHD status and a history of abuse are combined.
The mediator analyses support the notion that the aggression displayed by these girls during our summer programs helped to explain their high rates of peer rejection. However, because the measurements of aggression and rejection occurred at nearly the same times during our summer research camps, we cannot be sure as to what mediates what: Does aggressive behavior mediate the relationship between abuse status and peer rejection, as we found, or does peer rejection mediate the relationship between abuse status and aggression? We conducted a parallel mediator analysis with rejection as the mediator and aggressive behavior as the criterion, which yielded a significant attenuation in the abuse-aggression link. Causal sequencing is not certain from our cross-sectional examination.
We did not find support for our hypotheses that abuse status within the ADHD sample would predict higher internalizing features or cognitive/achievement deficits. The lack of a significant multivariate finding led us not to interpret the moderate-to-large univariate subgroup effects for parent and teacher reports of internalizing behavior or the moderate effect for Performance IQ (see Table 3). The safest interpretation is that our clearest findings lie in the realms of externalizing behavior and peer rejection.
When thinking about the results, one must keep in mind the already high levels of impairment of children with ADHD in general and the marked impairment in the present female sample (see Hinshaw, 2002). For a subgroup of children (in this case, with abuse histories) to have even higher levels of rejection and aggression than the rest of an ADHD sample provides clear evidence for the level of dysfunction in that subgroup. Whereas the hypothesized mechanisms for the increased rates of abuse in an ADHD sample were that abuse would either be an etiologic or exacerbating agent, those mechanisms become more complex when one becomes aware the histories of these children. Because of limitations of sample size we could not formally assess the group differences between abuse that occurred at different developmental stages. In some cases very early abuse clearly preceded a diagnosis of ADHD. For example, several girls in the sample were repeatedly sexually abused at a young age; for them, it is conceivable that a longstanding post-traumatic stress disorder may have been a more accurate diagnosis---or at least a clear-cut comorbidity. For others, however, the behavioral patterns associated with ADHD (and its diagnosis) preceded any documented abuse; it is possible that early externalizing problems combined with ineffective discipline that escalated into out-of-control physical punishment. In other cases, it was not possible to ascertain the timing of abuse occurrence and onset of ADHD status.
These developmental patterns have important implications for diagnosis and the treatment of both abused children and those with ADHD. Certainly there are children with ADHD for whom abuse appears to be overlooked diagnostically, either as an etiologic factor or an exacerbating variable. If such trauma is not addressed, symptoms associated with it may go unchecked and may even become worse as the child develops. The usual interventions for ADHD (behavioral modification procedures, stimulant medications) may not be the appropriate treatments for traumatized children (Weinstein, Stafflebach, & Biaggio, 2000). On the other hand, there is no research in the field on the optimal treatment strategies for children who present with the troubling combination of abuse histories and ADHD. More attention to trauma histories in the diagnosis of ADHD is in order as well as examination of optimal treatment strategies for children with both ADHD and abuse histories.
Limitations of this study include the all-female nature of the sample, the small size of the abused subgroup, and the retrospective nature of information regarding child abuse. In fact, it is quite possible that the “late” ascertainment of sample (after the age of 5 in all cases) resulted in underreporting of abuse that may have occurred. Also, abuse-specific consequences may have been obscured by the combining of all abuse types. To understand the possible etiologic or exacerbating role of trauma in disruptive behavior disorders and in ADHD, priorities for the future include larger sample sizes, the use of both clinical and non-clinical samples, and prospective longitudinal studies of young children at risk for both abuse and ADHD. Finally, the clinical recruitment strategy may have led to children with more problems (and therefore a stronger likelihood of abuse history) than would have been found in a representative sample.
Overall, the provocative findings here regarding linkages between ADHD status and abuse histories calls for more intensive research on this overlapping subgroup.
Acknowledgements
We thank the girls and families who participated in our summer research programs and the research coders who diligently aided in the preparation of the data. We give special thanks to Elizabeth Owens for help with data analyses.
Footnotes
Work on this article was supported by National Institute of Mental Health Grant 45064, awarded to Stephen Hinshaw, and an Underrepresented Minority Supplement to this grant, awarded to Allison Briscoe-Smith.
References
- Achenbach TM. Manual for the Child Behavior Checklist 4/18 and 1991 Profile. University Associates in Psychiatry; Burlington, VT: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4rd ed., text revision Author; Washington, DC: 2000. [Google Scholar]
- Anastopoulos AD, Guevremont DC, Shelton TL, DuPaul GJ. Parenting stress among families of children with attention decit hyperactivity disorder. Journal of Abnormal Child Psychology. 1992;20:503–520. doi: 10.1007/BF00916812. [DOI] [PubMed] [Google Scholar]
- Anderson CA, Hinshaw SP, Simmel C. Mother-child interactions in ADHD and comparison boys: Relationships with overt and covert externalizing behavior. Journal of Abnormal Child Psychology. 1994;22:247–265. doi: 10.1007/BF02167903. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello E, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Arnold LE. Sex differences in ADHD: Conference summary. Journal of Abnormal Child Psychology. 1996;24:555–569. doi: 10.1007/BF01670100. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Blachman DR, Hinshaw SP. Patterns of friendship in girls with and without attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2002;30:625–640. doi: 10.1023/a:1020815814973. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch F, Lynch M, Holt K. Resilience in maltreated children: Processes leading to adaptive outcome. Development and Psychopathology. 1993;5:629–647. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Erlbaum; Mahwah, NJ: 1988. [Google Scholar]
- Deater-Deckard K, Dodge K. Externalizing behavior problems revisited: Nonlinear effects and variation by culture, context and gender. Psychological Inquiry. 1997;8:161–175. [Google Scholar]
- Erhardt D, Hinshaw SP. Initial sociometric impressions of ADHD and comparison boys: Predictions from social behaviors and from nonbehavioral variables. Journal of Consulting and Clinical Psychology. 1994;62:833–842. doi: 10.1037/0022-006X.62.4.833. [DOI] [PubMed] [Google Scholar]
- Ethier LS, Lemelin J-P, Lachorite C. A longitudinal study of the effects of chronic maltreatment on children’s behavioral and emotional problems. Child Abuse & Neglect. 2004;28:1265–1278. doi: 10.1016/j.chiabu.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Hashina P. The victimization of children and youth: A comprehensive overview. In: White SO, editor. Handbook of youth and violence. Kluwer Academic/Plenum; New York: 2001. pp. 49–78. [Google Scholar]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: A comprehensive, national survey. Child Maltreatment. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19:337–346. [Google Scholar]
- Ford JD, Racussin R, Ellis C, Daviss W, Reiser J, Fleischer A, Thomas J. Child maltreatment, other trauma exposure, and posttraumatic symptomatology among young children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment. 2000;5:205–217. doi: 10.1177/1077559500005003001. [DOI] [PubMed] [Google Scholar]
- Gaub M, Carlson CL. Gender differences in ADHD: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1036–1045. doi: 10.1097/00004583-199708000-00011. [DOI] [PubMed] [Google Scholar]
- Gil E, Johnson T. Sexualized children. Launch Press; Rockville, MD: 1993. [Google Scholar]
- Hinshaw SP. On the distinction between attentional deficits/hyperactivity and conduct problems/aggression in child psychopathology. Psychological Bulletin. 1987;101:443–463. [PubMed] [Google Scholar]
- Hinshaw SP. Externalizing behavior problems and academic underachievement in childhood and adolescence: Causal relationships and underlying mechanisms. Psychological Bulletin. 1992;111:127–155. doi: 10.1037/0033-2909.111.1.127. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Psychosocial intervention for childhood ADHD: etiologic and developmental themes, comorbidity, and integration with pharmacotherapy. In: Cicchetti D, Toth SL, editors. Rochester Symposium on Developmental Psychopathology (Vol 9): Developmental approaches to prevention and intervention. University of Rochester Press; Rochester, NY: 1999. pp. 221–270. [Google Scholar]
- Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology. 2002;70:1086–1098. doi: 10.1037//0022-006x.70.5.1086. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Blachman DR. Attention-deficit/hyperactivity disorder. In: Bell-Dolan D, Foster S, Mash EJ, editors. Handbook of behavioral and emotional problems in girls. Kluwer Academic/Plenum; New York: 2005. pp. 117–147. [Google Scholar]
- Hinshaw SP, Carte ET, Sami N, Treuting JJ, Zupan BA. Preadolescent girls with attention-deficit/hyperactivity disorder: II. Neuropsychological performance in relation to subtypes and individual classification. Journal of Consulting and Clinical Psychology. 2002;70:1099–1111. doi: 10.1037//0022-006x.70.5.1099. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Melnick S. Peer relationships in boys with attention-deficit hyperactivity disorder with and without aggression. Development and Psychopathology. 1995;7:627–647. [Google Scholar]
- Hinshaw SP, Zupan B, Simmel C, Nigg J, Melnick S. Peer status in boys with and without attention-deficit hyperactivity disorder: Predictions from overt and covert antisocial behavior, social isolation, and authoritative parenting beliefs. Child Development. 1997;68:880–896. doi: 10.1111/j.1467-8624.1997.tb01968.x. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice, and DSM-V. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:437–446. doi: 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kazdin A. Depressive symptoms among physically abused and psychiatrically disturbed children. Journal of Abnormal Psychology. 1985;94:298–307. doi: 10.1037//0021-843x.94.3.298. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K, Williams L, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;113:164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Manual: Children’s Depression Inventory. MultiHealth Systems, Inc; Toronto, Canada: 1992. [Google Scholar]
- Kraemer HC, Stice E, Kazdin AE, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein R. Adolescent and adult outcomes in attention-deficit/hyperactivity disorder. In: Quay HC, Hogan AE, editors. Handbook of disruptive behavior disorders. Kluwer Academic/Plenum Plenum Press; New York: 1999. pp. 279–294. [Google Scholar]
- Margolin G, Gordis E. The effects of family and community violence on children. Annual Review of Psychology. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Hinshaw SP. Parent personality traits and psychopathology associated with antisocial behavior patterns in childhood attention-deficit hyperactivity disorder. Journal of Child Psychology and Psychiatry. 1998;39:145–159. [PubMed] [Google Scholar]
- Osofsky J. Prevalence of children’s exposure to domestic violence and child maltreatment: Implications for prevention and intervention. Clinical Child and Family Psychology Review. 2003;6:161–170. doi: 10.1023/a:1024958332093. [DOI] [PubMed] [Google Scholar]
- Parker JG, Asher SR. Peer relations and later personal adjustment: are low-accepted children at risk? Psychological Bulletin. 1987;102:357–389. doi: 10.1037//0033-2909.102.3.357. [DOI] [PubMed] [Google Scholar]
- Preacher K, Leonardelli G. Calculation for the Sobel test; an interactive calculation tool for mediation tests. 2001 http://quantrm2/psy.ohio-state.edu/kris/sobel/sobel.htm.
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from pervious versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Tannock R. Attention deficit hyperactivity disorder: Advances in cognitive, neurobiological, and genetic research. Journal of Child Psychology and Psychiatry. 1998;39:65–99. [PubMed] [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children. 3rd ed. Psychological Corporation/Harcourt Brace; New York: 1991. [Google Scholar]
- Wechsler D. Manual for the Wechsler Individual Achievement Test. Psychological Corporation/Harcourt Brace; New York: 1992. [Google Scholar]
- Weinstein A, Stafflebach D, Biaggio M. ADHD and posttraumatic stress disorder. ADHD Report. 2000;8:1–7. [Google Scholar]
- Whiffen VE, MacIntosh HB. Mediators of the link between child sexual abuse and emotional disorders: A critical review. Trauma, Violence, and Abuse. 2005;6:24–39. doi: 10.1177/1524838004272543. [DOI] [PubMed] [Google Scholar]
- Widom CS. Child abuse, neglect and witnessing violence. In: Stoff D, Breiling J, Maser J, editors. Handbook of antisocial behavior. Wiley; New York: 1997. pp. 159–170. [Google Scholar]
- Wozniak J, Crawford M, Biederman J, Faraone S, Spencer T, Taylor A, Blier H. Antecedents and complications of trauma in boys with ADHD: Findings from a longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:48–55. doi: 10.1097/00004583-199901000-00019. [DOI] [PubMed] [Google Scholar]