Four weeks ago we described the case of a 46 year old woman who presented with possible miscarriage, severe hypertension, acute renal failure, pulmonary oedema, microangiopathic haemolytic anaemia, and seizures (BMJ 2007;334:1372, doi: 10.1136/bmj.39212.564745.BE). The diagnoses we considered were malignant hypertension, intrinsic renal disease, a primary microangiopathic process—such as haemolytic uraemic syndrome or thrombotic thrombocytopenic purpura, or eclampsia with HELLP syndrome. She was started on intermittent haemodialysis, an angiotensin converting enzyme inhibitor, and plasma exchange (BMJ 2007;335:44, doi: 10.1136/bmj.39239.478495.80). A magnetic resonance imaging scan of the brain showed posterior leucoencephalopathy consistent with hypertensive encephalopathy.
Her platelet count, metabolic abnormalities, and breathlessness improved and she had no further seizures. At one week she was well but remained dependent on dialysis. Bisoprolol and amlodipine were added to control her blood pressure.
Renal Doppler ultrasound showed poor renal perfusion so we performed angiography to exclude renovascular disease. This showed normal renal vessels (fig 1), suggesting a microangiopathic infrarenal process.
Fig 1 The patient's bilateral renal angiography showing normal renal vessels
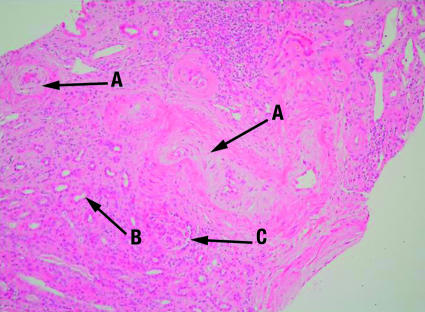
Renal biopsy demonstrated florid myxoid intimal thickening in interlobular arteries (fig 2), widespread acute tubular damage, and glomerular ischaemic changes. There was little thrombotic change to suggest haemolytic uraemic syndrome or thrombotic thrombocytopenic purpura. These appearances are consistent with a diagnosis of malignant hypertension or scleroderma renal crisis.
Fig 2 The patient's renal biopsy showing florid myxoid intimal thickening in interlobular arteries (A), widespread acute tubular damage (B), and glomerular ischaemic changes (C)
The table summarises the other investigations and blood tests. These were negative except for a strongly positive speckled antinuclear antibody at a titre of more than 1/1000. The staining pattern was consistent with anti-RNA polymerase antibodies and this was confirmed with immunoprecipitation.
The patient's immunological profile and results of other investigations
| Investigation | Result (normal range) |
|---|---|
| Antinuclear antibody | Positive, speckled >1/1000; anti-RNA polymerase |
| Anti-neutrophil cytoplasmic antibody | Negative |
| Anti-glomerular basement membrane antibody | Negative |
| Anti-scleroderma-70 antibody | Negative |
| Anti-topoisomerase antibody | Negative |
| Rheumatoid factor | Negative |
| Anti-double stranded DNA antibody | Negative |
| Anti-complement C1q antibodies | Negative |
| Complement C3 | 1.11 g/l (0.7-1.7) |
| Complement C4 | 0.18 g/l (0.16-0.54) |
| Anti-phospholipid/anti-cardiolipin antibody | Negative |
| IgG | 5.9 g/l (5.3-16.5 |
| IgA | 0.96 g/l (0.8-4.0) |
| IgM | 0.53 g/l (0.5-2.0) |
| Renal angiography | Normal |
| Magnetic resonance imaging of adrenals | Normal |
| Spot plasma adrenaline | 0.76 nM (0.00-1.00) |
| Spot plasma noradrenaline | 3.2 nM (0-5.0) |
| Random adrenocorticotrophin | 5.1 ng/l |
| Random cortisol | 222 nM |
| Long dexamethasone suppression test final cortisol | 80 nM |
Anti-RNA polymerase antibodies are strongly associated with scleroderma renal crisis, and we consider this to be the diagnosis. Her hypertension may have precipitated miscarriage on this occasion, but the cause of the earlier miscarriages is less clear.
Scleroderma renal crisis primarily affects young and middle aged women and presents with acute renal failure and hypertension. There may be no prior symptoms of systemic sclerosis, but the history of Raynaud's offered a diagnostic clue in this patient. Other features of malignant hypertension such as encephalopathy, seizures, pulmonary oedema, and microangiopathic haemolytic anaemia may complicate this illness.
Angiotensin converting enzyme inhibitors may facilitate microvascular remodelling and prevent progression of renal impairment; they are used widely in this disease. Intravenous vasodilatory therapy, usually with prostacyclin, is recommended, and dialysis may be required. The benefit of plasma exchange in secondary microangiopathy is controversial and was instituted in this case because initially we could not exclude thrombotic thrombocytopenic purpura as a primary diagnosis.
The prospects for renal recovery are poor in patients who need dialysis at diagnosis. This patient is currently well on haemodialysis three times a week, although she still requires oral antihypertensives. She is currently awaiting renal transplantation.
Contributors: CDP is guarantor.
We welcome contributions of interactive case reports. Cases should raise interesting clinical, investigative, diagnostic, and management issues but not be so rare that they appeal to only a minority of readers. Full details of criteria are available at: bmj.com/cgi/content/full/326/7389/564/DC1