Abstract
Ubiquitin-dependent degradation of the cyclin-dependent kinase inhibitor p27 mediated by SCF-Skp2 ubiquitin ligase is involved in cell cycle regulation. Proliferation of tubular cells is a characteristic feature in obstructed kidneys of unilateral ureteral obstruction. Comparing Skp2+/+ mice with Skp2−/− mice, we investigated the involvement of Skp2, a component of SCF-Skp2 ubiquitin ligase for p27, in the progression of renal lesions in unilateral ureteral obstructed kidneys. mRNA expression of Skp2 was markedly increased in the obstructed kidneys from Skp2+/+ mice and peaked 3 days after unilateral ureteral obstruction. Renal atrophy, tubular dilatation, tubulointerstitial fibrosis, and increases in α-smooth muscle actin expression, the number of tubular cells, and proliferating tubular cells positive for Ki67 were observed in the obstructed kidneys from Skp2+/+ mice; however, these findings were significantly attenuated in Skp2−/− mice. The p27 protein level was increased in the obstructed kidneys but was significantly greater in Skp2−/− mice. The number of Ki67-positive p27-negative cells was lower in obstructed kidneys from Skp2−/− mice than Skp2+/+ mice, whereas that of Ki67-negative p27-positive cells was greater in Skp2−/− mice. These findings suggest that p27 accumulation, which results from SCF-Skp2 ubiquitin ligase deficiency in Skp2−/− mice, is involved in the amelioration of renal damage induced by obstructive nephropathy.
Unilateral ureteral obstruction (UUO) is a representative model of kidney disease with progressive tubulointerstitial injury that reveals many cellular and molecular events during the progression of renal fibrosis associated with cell proliferation and apoptosis.1,2 In the kidney, cell proliferation is believed to be a central response to injury and culminates in the development of fibrosis and renal damage.3 Furthermore, an imbalance between cell proliferation and apoptosis leads to unchecked apoptosis, resulting in progressive cell loss, renal tubular atrophy, and interstitial fibrosis.4
Cell proliferation is a basic biological mechanism that involves transit through the cell cycle. Cell proliferation is controlled by a network of proteins including cyclins, cyclin-dependent kinases (CDKs),5 and cyclin-dependent kinase inhibitors (CKIs).6 The CKI p27Kip1 (p27) negatively regulates the cell cycle and is abundantly expressed in most normal quiescent cells, and its level declines when cells are stimulated to proliferate in response to mitotic stimuli.7,8 In vitro studies have shown that experimentally reducing the level of p27 protein augments the proliferative response to mitogens,9,10 whereas forced overexpression of p27 inhibits cell proliferation.8 The level of p27 protein is controlled not only by transcriptional activation but also by proteolytic degradation of the p27 protein via the ubiquitin-proteasome system. G1-cyclin-CDK is subsequently activated to phosphorylate retinoblastoma protein and progress the cell cycle from G1 to S phase.11,12
The ubiquitin-proteasome pathway of protein degradation plays an important role in the control of the abundance of cell cycle regulatory proteins.13,14 The rapidity and substrate specificity of protein degradation by the ubiquitin-proteasome pathway are consistent with its role in controlling the fluctuations in the intracellular concentration of cyclins, CDKs, and CKIs. Skp2 is the F-box protein component of an SCF-type ubiquitin ligase that interacts specifically with p27, and thereby the SCF-Skp2 complex promotes p27 ubiquitination and degradation.15,16 It has been shown that Skp2-deficient mice exhibit cellular accumulation of p27.17
In the kidney, cell proliferation is believed to be central to the renal response to injury culminating in the development of fibrosis and renal failure. Both mRNA and protein levels of CDK inhibitors such as p27 and p21 are up-regulated at an early stage in obstructed kidneys of UUO mice.18,19,20 It is reported that renal tubular epithelial cell proliferation and apoptosis increase markedly in obstructed kidneys of p27−/− mice.21 Because up-regulation of p27 safeguards against excessive renal epithelial cell proliferation, p27 may be involved in protecting cells and tissue from inflammatory injury. On the other hand, it is reported that proliferation of interstitial cells, especially myofibroblasts, increased, but tubular epithelial cell proliferation and apoptosis were unchanged in obstructed kidneys from p21−/− mice.22 p21, unlike p27, limits the magnitude of early myofibroblast proliferation, but p21 is not essential for the regulation of tubular epithelial cell proliferation and apoptosis following UUO. These studies suggest a differential regulatory role for CKI p27 and p21 in UUO kidneys. However, it has not been elucidated whether post-transcriptional regulation of p27 mediated by ubiquitin-dependent proteasomal degradation is involved in the progression of renal injury. In the present study, we investigated the involvement of SCF-Skp2 ubiquitin ligase for p27 in the development of tubulointerstitial injury in UUO by comparing wild type with Skp2-deficient mice. We found that the increase in p27, which resulted from Skp2 deficiency, inhibited the proliferation of tubular cells and attenuated fibrotic tubulointerstitial lesions in the obstructed kidneys. Our findings suggest that Skp2 is a key molecule involved in progression of renal injury in the UUO model.
Materials and Methods
Experimental Animals
Male C57BL/6J mice, weighing 20 to 25 g, aged 6 weeks at the start of the experiment, were purchased from SLC (Hamamatsu, Shizuoka, Japan) and allowed free access to food and water. The generation of Skp2-null mice (Skp2−/− mice) was designed by Nakayama et al.17 In this line of mice, the targeted construct was designed to delete the region from the translation initiation site to the site corresponding to the C terminus of the F-box domain. Mice were treated according to the protocols approved by the Hamamatsu University School of Medicine Animal Care Committees at the Center Animal Care facility.
Experimental Design of the UUO Model
Ureteral obstruction was achieved by ligating the left ureter with 3-0 silk through a left lateral incision. Sham-operated animals (n = 3) were used as controls. Mice were sacrificed at 1, 3, 5, 7, and 14 days (for each group, n = 3) after operation. Sham-operated mice were sacrificed at day 7 (n = 3). Obstructed kidneys (UUO), nonobstructed contralateral kidneys (CLK), and sham-operated kidneys were harvested at each day and subjected to the studies described below. Skp2+/+ and Skp2−/− mice (for each group, n = 4 to 5) were subjected to ureteral obstruction and sacrificed 7 days after obstruction, and kidneys were harvested. The experimental protocol was approved by the Ethics Review Committee for Animal Experimentation of Hamamatsu University School of Medicine.
Histopathological and Immunohistochemical Analyses
Kidney tissues were fixed in 4% paraformaldehyde in phosphate-buffered saline and embedded in paraffin. Tissue sections (3 μm thick) were rehydrated and stained with periodic acid-Schiff and for histopathological analysis.23 The number of dilated tubules and interstitial cells on these tissue sections were counted. The number of renal tubular epithelial cells in a tubule was counted as the total number of tubular epithelial cells in a field (×300) and was divided by the number of total tubules. Immunoreactivity for α-smooth muscle actin (α-SMA), Ki67, p27 proteins were determined by using Histofine SAB-PO kit (Nichirei, Tokyo, Japan) as a standard biotin-streptavidin-peroxidase method. Endogenous peroxidase activity was blocked by 3% hydrogen peroxide for 10 minutes at −20°C. The primary antibodies were mouse monoclonal anti-human α-SMA (DAKO, Hamburg, Germany), anti-mouse p27 (BD Transduction Laboratories, San Jose, CA), and rabbit polyclonal anti-human Ki67 (Novocastra Laboratories, Newcastle upon Tyne, UK). The secondary antibodies were affinity-purified biotinylated goat anti-mouse or anti-rabbit immunoglobulin (Nichirei). Kidney sections incubated with only the biotinylated secondary antibody without the primary antibody as a negative control. Reaction products were visualized using simple-stain diaminobenzidine solution (Nichirei). Kidney sections were counterstained lightly with hematoxylin. The level of tubulointerstitial fibrosis detected by Masson’s trichrome staining was semiquantitatively graded 0 to 4 at all fields (×300) as follows: 0 (0%); 1, weak (≤20% in interstitial area colored green, which means fibrosis); 2, mild (>20 to ≤50%); 3, moderate (>50 to ≤80%); and 4, strong (>80%). The immunoreactivity for α-SMA was scored at all fields (×300) as follows: 0 (0%); 1, weak (≤20% in interstitial area positive for protein); 2, mild (>20 to ≤50% positive); 3, moderate (>50 to ≤80% positive); and 4, strong (>80% positive). To evaluate the immunoreactivity for Ki67 and p27 in individual kidneys, three randomly selected nonoverlapping fields of renal cortex were examined (×300) and the number of Ki67, p27-positive cells in renal tubular epithelial cells, and interstitial cells were evaluated. The consecutive kidney sections were also used to evaluate the association of Ki67 and p27.
RNA Isolation and Quantitative Analysis of mRNA by Real-Time Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR)
Total RNA was extracted from whole kidney tissue using Isogen (Wako, Osaka, Japan) according to the manufacturer’s instructions. Reverse transcription of the RNA was performed using the SuperScript First-Strand Synthesis System for RT-PCR kit (Invitrogen, Carlsbad, CA) with 2.5 μg of total RNA. The resulting cDNA was subjected to real-time PCR using the Roter-Gene 3000 System (Corbett Research, Mortlake, VIC, Australia) for amplification and online quantification. All PCR experiments were performed using a QuantiTect SYBR Green PCR kit purchased from Qiagen (Valencia, CA). The PCR primer sequences for mouse Skp2 were sense 5′-CAGACCCTGACGCACCTCACG-3′ and antisense 5′-TTCTGACGCCCCGTTGCCTGCT-3′, giving an amplified RT-PCR product of 241 bp. Primers for glyceraldehyde-3-phospate dehydrogenase (GAPDH), used as an internal control, were sense 5′-TGCACCACCAACTGCTTAG-3′ and antisense 5′-GATGCAGGGATGATGTTC-3′, giving an amplified RT-PCR product of 176 bp. Cycling conditions were: 15 minutes’ preincubation at 94°C, 15 seconds’ denaturation at 94°C, 20 seconds’ annealing at 58°C for Skp2, 54°C for GAPDH, and extension at 72°C was performed for 20 seconds for Skp2 and 15 seconds for GAPDH. The fluorescent product was detected for 5 seconds at 79°C. To verify the accuracy of PCR amplification, PCR products were analyzed by ethidium bromide-stained 3% agarose gel electrophoresis and melting curve analysis. Real-time RT-PCR data were analyzed according to the manufacturer’s instructions. Finally, the ratio of Skp2 mRNA was normalized for GAPDH mRNA in each sample.
Evaluation for Apoptosis
Deoxynucleotidyl transferase enzyme for terminal deoxynucleotidyl transferase dUTP nick-end labeling assay was performed to detect apoptotic cell death using the ApopTag plus peroxidase in situ apoptosis detection kit (Chemicon, Temecula, CA). For each kidney, apoptotic cells in 20 nonoverlapping fields of renal cortex were counted under ×600 objective. The number of positive nuclei was averaged for each field.
Western Blot Analysis
Whole kidney tissues were dissolved in RIPA buffer (25 mmol/L Tris-HCl, pH 7.4, 150 mmol/L NaCl, 0.1% sodium dodecyl sulfate, 0.5% Triton X-100, and 0.5% sodium deoxycholate) containing protease inhibitors (150 mg/ml phenylmethylsulfonyl fluoride, 5 mg/ml aprotinin, 5 mg/ml pepstatin, 5 mg/ml leupeptin, and 5 mg/ml E-64) at 4°C. After incubation for 30 minutes, the lysates were centrifuged for 15 minutes at 13,000 × g at 4°C. The protein concentrations of the lysates were measured with a protein assay reagent (Bio-Rad Laboratories, Hercules, CA). Soluble lysates were boiled for 8 minutes with 4× sodium dodecyl sulfate sample buffer (250 mmol/L Tris-HCl, pH 6.8, 12% sodium dodecyl sulfate, 40% glycerol, 20% 2-mercaptoethanol, and 1% bromphenol blue). Equal amounts of proteins were loaded and separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis. Protein was transferred to polyvinylidene difluoride membranes followed by immunoblotting using mouse monoclonal anti-p27 antibody (Transduction Laboratories) and anti-α-tubulin antibody (Sigma). α-Tubulin was used as an internal control. Proteins were visualized using an enhanced chemiluminescence system (Perkin Elmer, Wellesley, MA).
Statistical Analysis
Statistical analysis was performed using computer-assisted software (StatView 5.0; SAS Institute, Inc., Cary, NC). All values are given as means ± SD. Statistical differences were assessed by analysis of variance and followed Fisher’s protected least significant difference post hoc test. The evaluation of Masson’s trichrome and α-SMA was done using the Mann-Whitney U-test. P values <0.05 indicated statistically significant differences.
Results
Dilation of Renal Tubules in UUO Kidneys of Skp2+/+ Wild-Type Mice
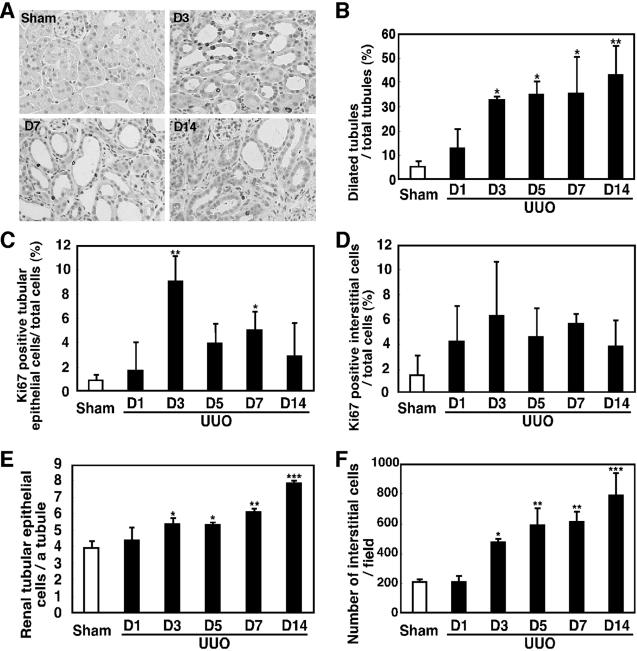
Renal tubules started to dilate in obstructed kidneys on day 1 (13.1%) compared with sham-operated kidneys (5.7%; Figure 1, A and B), and more renal tubules were dilated on day 3 (33.3%). On day 14, the interstitial area was increased while the number of total renal tubules was decreased.
Figure 1.
Representative pictures of UUO kidney sections (A; immunostaining for Ki67; magnification, ×300), percentage of dilated renal tubules (B), the number of Ki67-positive tubular (C) and interstitial cells (D), and the number of tubular epithelial cells (E) and interstitial cells (F) from Skp2+/+ mice at the experimental time points after UUO. Many tubules were dilated in obstructed kidneys from day 3 after UUO (A and B). Numbers of Ki67-positive tubular cells and interstitial cells were increased in obstructed kidneys on day 3 after UUO (C and D). Tubular epithelial cells per tubule (E) and interstitial cells (F) were also increased in obstructed kidneys from day 3. The interstitial area was enlarged widely in obstructed kidneys (A). *P < 0.05 (C); P < 0.005 (B, E, and F); **P < 0.0005, ***P < 0.0001 versus sham-operated kidneys.
Increased Ki67-Positive Cells in UUO Kidneys of Skp2+/+ Wild-Type Mice
Most tubular epithelial cells were not Ki67-positive in sham-operated kidneys (1.0%; Figure 1, A and C), but the number of Ki67-positive cells was increased in obstructed kidneys on day 3 (9.1%) and on day 7 (5.1%). Moreover, the number of renal tubular epithelial cells per tubule increased in obstructed kidneys from day 3 with a significant difference (Figure 1E). Whereas numbers of interstitial cells positive for Ki67 increased in obstructed kidneys compared with sham-operated kidney, this was not significantly different on each day (Figure 1D). The number of total cells that existed in the interstitial area increased gradually in obstructed kidneys (Figure 1F). It increased by approximately 2.2-fold on day 3, reaching 3.7-fold on day 14.
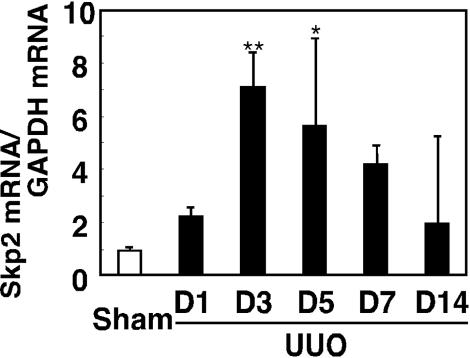
Increased Expression of Skp2 in UUO Kidneys of Skp2+/+ Wild-Type Mice
Skp2 mRNA expression was up-regulated by 2.3-fold in obstructed kidneys of Skp2+/+ wild-type mice on day 1 compared with kidneys from sham-operated mice (Figure 2), reaching a peak (7.1-fold) on day 3 and then gradually decreasing until day 14 in UUO kidneys (2.0-fold).
Figure 2.
Level of Skp2 mRNA measured by quantitative RT-PCR in the obstructed kidneys from Skp2+/+ wild-type mice at the experimental time points after UUO. In the obstructed kidneys from Skp2+/+ mice, mRNA expression of Skp2 markedly increased and peaked 3 days after UUO. *P < 0.05, **P < 0.005 versus sham-operated kidneys.
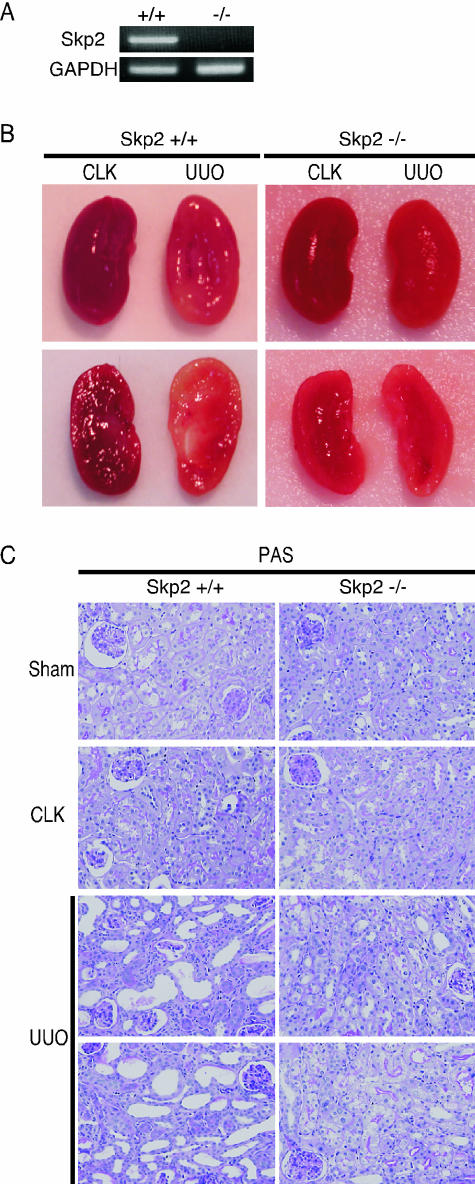
Mitigation of Tubulointerstitial Lesions in UUO Kidney by Skp2 Deficiency
To investigate the role of Skp2 in the progression of tubulointerstitial lesions in UUO kidneys in vivo, Skp2 wild-type (+/+) and Skp2-deficient (−/−) mice on day 7 after UUO were compared histopathologically. We confirmed that Skp2 mRNA was not expressed in obstructed kidneys derived from Skp2−/− mice (Figure 3A). Although remarkable renal atrophy was observed in the obstructed kidneys from Skp2+/+ mice, it was markedly less in Skp2−/− mice (Figure 3B). The weight of obstructed kidneys from Skp2+/+ mice was reduced to 80% compared with nonobstructed contralateral kidneys of UUO mice (CLK), whereas the weight of kidneys from Skp2−/− mice was not significantly different (data not shown). Histologically, tubular dilatation and atrophy and interstitial cell infiltration were observed in obstructed kidneys from Skp2+/+ mice (Figure 3C). However, the severity of these lesions was markedly less in obstructed kidneys from Skp2−/− mice.
Figure 3.
Levels of Skp2 and GAPDH mRNA expression (A) and the representative macroscopic (B) and microscopic (C; periodic acid-Schiff, magnification, ×300) findings of the obstructed (UUO) and nonobstructed contralateral (CLK) kidneys of Skp2+/+ (left) and Skp2−/− mice (right) 7 days after UUO. No detectable expression of Skp2 mRNA was observed in Skp2−/− mice (A). Although remarkable renal atrophy was noted in the obstructed kidneys from Skp2+/+ mice, it was markedly less in Skp2−/− mice (B). Tubular dilatation and atrophy and interstitial cell infiltration were observed in obstructed kidneys from Skp2+/+ mice. However, the severity of these lesions was markedly less in obstructed kidneys from Skp2−/− mice (C).
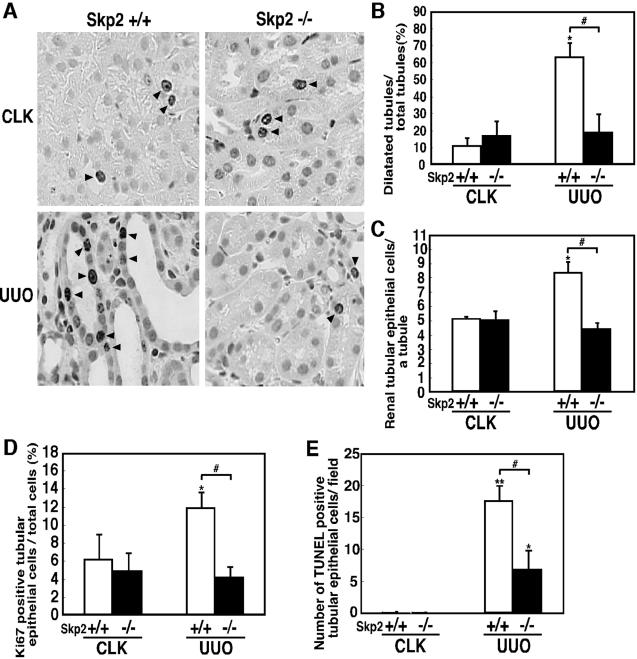
Amelioration of Renal Tubular Dilatation, Tubular Epithelial Cell Proliferation, and Apoptosis in UUO Kidneys from Skp2−/− Mice
As shown in Figure 4B, 64% of renal tubules were dilated in obstructed kidneys from Skp2+/+ mice (Figure 4A), whereas only 12% of renal tubules were dilated in CLK from Skp2+/+ mice. In obstructed kidneys from Skp2−/− mice, dilatation of renal tubules was significantly decreased to 17% (Figure 4, A and B). The number of tubular epithelial cells per tubule was significantly increased in obstructed kidneys from Skp2+/+ mice compared with CLK from Skp2+/+ mice (Figure 4, A and C). Surprisingly, the number of tubular epithelial cells was significantly decreased in obstructed kidneys from Skp2−/− mice compared with Skp2+/+ mice. On the other hand, there was no difference in the basal level between obstructed kidneys and CLK from Skp2−/− mice. We next evaluated the renal tubular epithelial cell proliferation by immunostaining for Ki67, a marker of cell proliferation. In CLK from Skp2+/+ mice, 6% of renal tubular epithelial cells were Ki67-positive (Figure 4D). Increases in Ki67-positive cells were observed in the dilated tubular cells in obstructed kidneys from Skp2+/+ mice (12%, Figure 4, A and D). However, no significant increases in Ki67-positive tubular cells were observed in the obstructed kidneys from Skp2−/− mice (Figure 4, A and D). These results indicated that Skp2 deficiency suppressed proliferation of renal tubular epithelial cells in obstructed kidneys. We then evaluated apoptosis in tubular epithelial cells. There were few tubular epithelial apoptotic cells in CLK from both Skp2+/+ mice (0.7) and Skp2−/− mice (0.4) on day 7 after obstruction. The number of apoptotic cells increased in obstructed kidneys from Skp2+/+ mice (Figure 4E), but it was significantly less in the obstructed kidneys from Skp2−/− mice.
Figure 4.
Representative pictures of immunostaining for Ki67 (A; magnification, ×600), percentage of dilated renal tubules (B), number of tubular epithelial cells per tubule (C), Ki67-positive tubular cells (D), and apoptosis (E) in the obstructed (UUO) and nonobstructed contralateral (CLK) kidneys of Skp2+/+ and Skp2−/− mice 7 days after UUO. Many tubules were dilated (A and B), with increased numbers of tubular epithelial cells (C), and their tubules had Ki67-positive tubular epithelial cells (A and D) in obstructed kidney from Skp2+/+ mice. However, tubular dilatation, increases of tubular cells, Ki67-positive cells, and apoptosis were markedly less in obstructed kidneys from Skp2−/− mice. *P < 0.0001; Skp2+/+ CLK versus Skp2+/+ UUO, #P < 0.0001; Skp2+/+ UUO versus Skp2−/− UUO in B, C, and D. *P = 0.0001; Skp2−/− CLK versus Skp2−/− UUO, **P < 0.0001; Skp2+/+ CLK versus Skp2+/+ UUO, #P < 0.0001; Skp2+/+ UUO versus Skp2−/− UUO in E.
Increased p27 Protein Level, Decreased in Proliferative but Increased in Quiescent Tubular Cells in the UUO Kidneys from Skp2−/− Mice
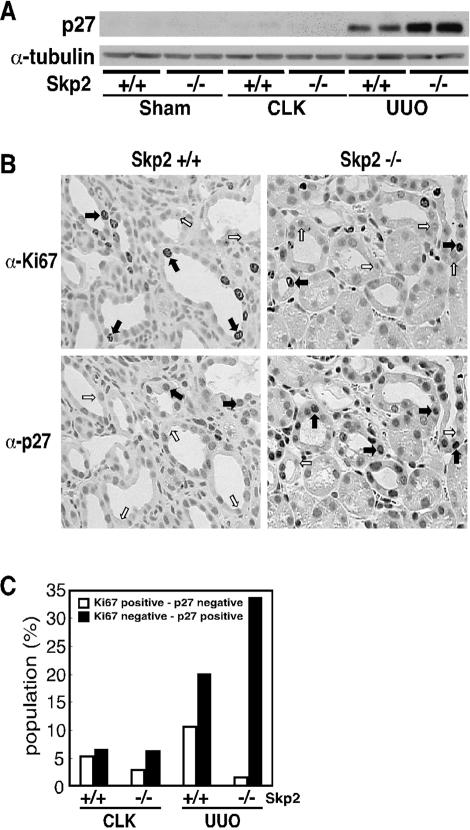
Because the proliferation of renal tubular epithelial cells was suppressed in obstructed kidneys from Skp2−/− mice (Figure 4D), we examined whether p27 protein expression in obstructed kidneys from Skp2−/− mice differed from that from Skp2+/+ mice on day 7 after obstruction. Using Western blot analysis with the anti-p27 antibody, an increase in p27 protein was observed in obstructed kidneys from Skp2+/+ mice, and further up-regulation of p27 protein level was detected in obstructed kidneys from Skp2−/− mice (Figure 5A). To examine the association between Ki67 and p27 in obstructed kidneys, serial sections of the kidney were subjected to immunostaining with anti-Ki67 and -p27 antibodies (Figure 5B). Proliferating tubular cells, positive for Ki67 and negative for p27, were 11% in obstructed kidneys from Skp2+/+ mice (Figure 5C, white bar), but decreased to 2% in obstructed kidneys from Skp2−/− mice. On the other hand, quiescent tubular cells, negative for Ki67 and positive for p27, were 20% in obstructed kidneys from Skp2+/+ mice (Figure 5C, black bar) and 34% in obstructed kidneys from Skp2−/− mice. These results suggest that the enhanced accumulation of p27 protein by Skp2 deficiency is involved in the inhibition of cell proliferation, resulting in decreases in the population of proliferative tubular cells and increases in that of quiescent tubular cells in the obstructed kidneys from Skp2−/− mice.
Figure 5.
Levels of p27 protein detected by Western blot analysis (A) and the representative pictures of immunostaining for Ki67 and p27 in consecutive renal sections (B; magnification, ×300) from the obstructed (UUO) kidneys of Skp2+/+ (left) and Skp2−/− mice (right) 7 days after UUO and the population of proliferating and quiescent tubular epithelial cells (C). p27 protein accumulated in obstructed kidneys from Skp2−/− mice (A and B). Black arrows show each Ki67-positive cell in top panels or p27-positive cell in bottom panels. White arrows show each Ki67-negative cell in top panels or p27 negative cell in bottom panels. Proliferating cells, Ki67-positive/p27-negative (C, white bar), decreased and quiescent cells, Ki67-negative/p27-positive (C, black bar), increased in obstructed kidneys from Skp2−/− mice.
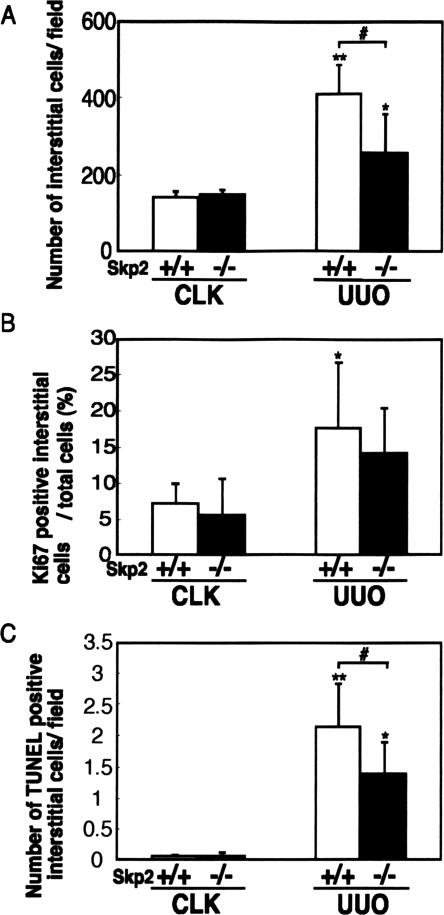
Suppression of Renal Interstitial Cell Proliferation and Apoptosis in UUO Kidney from Skp2−/− Mice
The number of interstitial cells also increased by 2.9-fold in the obstructed kidneys from Skp2+/+ mice compared with CLK from Skp2+/+ mice (Figure 6A). In obstructed kidneys from Skp2−/− mice, interstitial cells increased by 1.7-fold compared with CLK from Skp2−/− mice, but there was a significant difference between obstructed kidneys from Skp2+/+ mice and kidneys from Skp2−/− mice. To evaluate cell proliferation, 7% of interstitial cells were Ki67-positive in CLK from Skp2+/+ mice on day 7 (Figure 6B), and 18% were Ki67-positive in obstructed kidneys from Skp2+/+ mice. Similarly, the number of Ki67-positive interstitial cells increased, but it was mitigated slightly in obstructed kidneys from Skp2−/− mice (14%), but this was not significantly different to obstructed kidneys from Skp2+/+ mice. On the other hand, to evaluate apoptosis, there were also few terminal deoxynucleotidyl transferase dUTP nick-end labeling-positive interstitial apoptotic cells in CLK from both Skp2+/+ mice (0.1) and Skp2−/− mice (0.1) on day 7 after obstruction. Interstitial apoptotic cells increased to 2.1 in obstructed kidneys from Skp2+/+ mice (Figure 6C). Obstructed kidneys from Skp2−/− mice showed significantly less interstitial apoptosis than that from Skp2+/+ mice.
Figure 6.
The number of interstitial cells (A), Ki67-positive (B), and apoptotic interstitial cells (C) in the obstructed (UUO) and nonobstructed contralateral (CLK) kidneys of Skp2+/+ and Skp2−/− mice 7 days after UUO. The number of interstitial cells and apoptosis decreased in obstructed kidneys from Skp2−/− mice. *P < 0.05; Skp2−/− CLK versus Skp2−/− UUO, **P < 0.0001; Skp2+/+ CLK versus Skp2+/+ UUO, #P < 0.005; Skp2+/+ UUO versus Skp2−/− UUO in A. *P < 0.05; Skp2+/+ CLK versus Skp2+/+ UUO in B. *P < 0.001; Skp2−/− CLK versus Skp2−/− UUO, **P < 0.0001; Skp2+/+ CLK versus Skp2+/+ UUO, #P < 0.05; Skp2+/+ UUO versus Skp2−/− UUO in C.
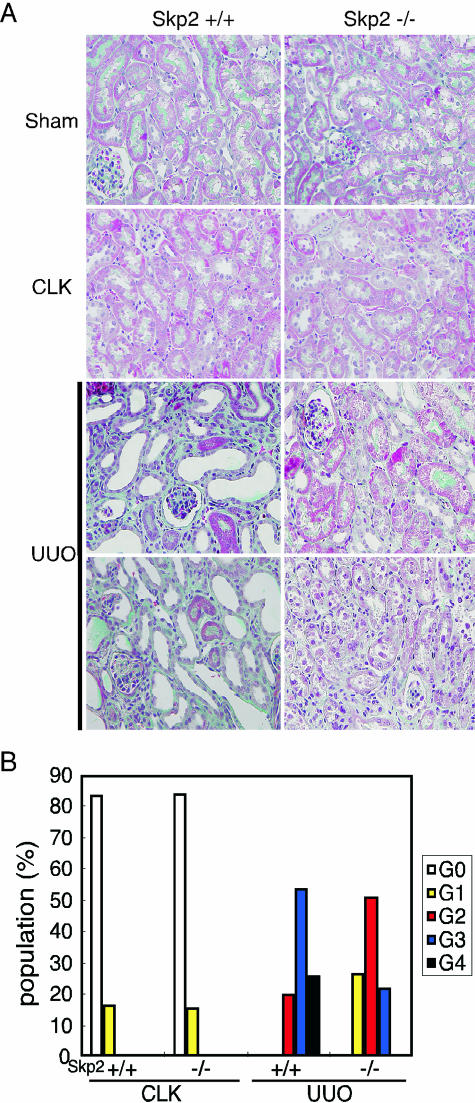
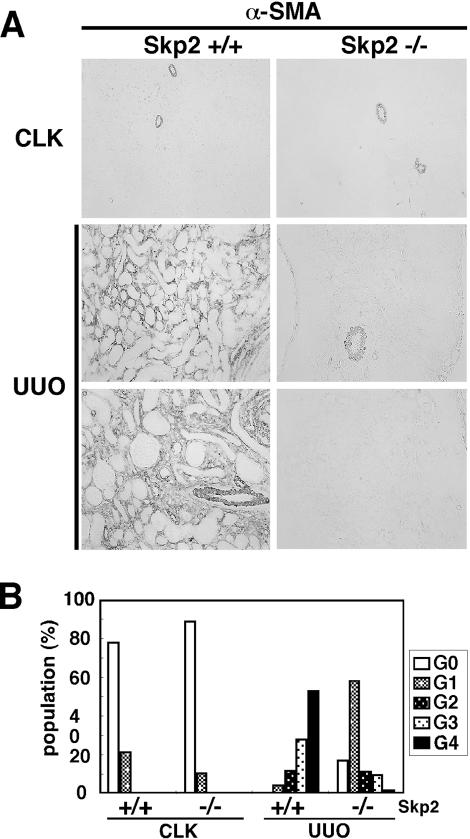
Amelioration of Fibrosis in UUO Kidneys from Skp2−/− Mice
The interstitial area and the number of tubulointerstitial cells increased, and interstitial fibrosis progressed in obstructed kidneys from Skp2+/+ mice (Figure 7A). In contrast, the development of interstitial fibrosis was ameliorated in obstructed kidneys from Skp2−/− mice. A significant increase in interstitial myofibroblastic cells positive for α-SMA was observed in obstructed kidneys from Skp2+/+ mice on day 7, but the levels were markedly attenuated in obstructed kidneys from Skp2−/− mice (Figure 8A). There were significant differences between obstructed kidneys from Skp2+/+ mice and those from Skp2−/− mice (Figures 7B and 8B).
Figure 7.
Representative pictures of the CLK and UUO kidney sections from Skp2+/+ mice (A, left) and Skp2−/− mice (A, right) and the semiquantification of staining intensity (B) for Masson’s trichrome 7 days after obstruction. The interstitial area was increased, and fibrosis progressed in obstructed kidneys from Skp2+/+ mice. However, it was moderated in obstructed kidneys from Skp2−/− mice. The grading of intensities shown in B was as follows: G0 (grade 0, 0%, white bars): G1 (grade 1, ≤20% in interstitial area colored green, yellow bars); G2 (grade 2, 21 ≈ 50%, red bars); G3 (grade 3, 51 ≈ 80%, blue bars); and G4 (grade 4, ≥81%, black bars). P < 0.0001; Skp2+/+ UUO versus Skp2−/− UUO.
Figure 8.
Representative pictures of the CLK and UUO kidney sections from Skp2+/+ mice (A, left) and Skp2−/− mice (A, right) and the semiquantification of immunostaining intensity (B) for α-SMA 7 days after obstruction. Significant increases of interstitial myofibroblastic cells positive for α-SMA were observed in obstructed kidneys from Skp2+/+ mice on day 7, but the levels were markedly attenuated in obstructed kidneys from Skp2−/− mice (A, magnification, ×300). The grading of immunostaining intensities for α-SMA shown in B was as follows: G0 (grade 0, positive area 0%); G1 (grade 1, ≤20% in interstitial area were positive); G2 (grade 2, 21 ≈ 50% positive); G3 (grade 3, 51 ≈ 80% positive); and G4 (grade 4, ≥81% positive). P < 0.0001; Skp2+/+ UUO versus Skp2−/− UUO.
Discussion
There is much evidence from molecular and cellular studies suggesting that SCF-Skp2 ubiquitin ligase plays a role as a powerful positive regulator on cell growth through the degradation of negative regulators of the cell-cycle such as p27, a CDK inhibitory protein.15,24 In human cancers, decreases in p27 as a result of Skp2 overexpression have been demonstrated, supporting the role of Skp2 in the accelerated growth and malignant potential.25 However, it is unclear whether regulation of p27, resulting from ubiquitin-dependent regulation mediated by SCF-Skp2 ubiquitin ligase, is involved in the progression of renal diseases. In the present study, we investigated whether Skp2 is involved in the progression of tubulointerstitial injury induced by UUO by comparing Skp2+/+ wild-type mice with Skp2−/− mice. We found remarkable attenuation of tubular cell proliferation, apoptosis, and tubulointerstitial fibrosis in the obstructed kidneys from Skp2−/− mice. These results suggest that Skp2 plays an important role in the development of tubulointerstitial lesions induced by UUO.
It was recently reported that p27 plays a protective role in the development of obstructive nephropathy.21 In the obstructed kidneys, we demonstrated that the increase in mRNA expression of Skp2 components of SCF-Skp2 ubiquitin ligase for p27 peaked on day 3 but decreased gradually thereafter. On day 3, the number of proliferating tubular cells positive for Ki67 and tubular epithelial cells was increased, and many tubules were dilated in the obstructed kidneys. These data suggest that the decease in p27 mediated by its ubiquitin-dependent degradation involving SCF-Skp2 ubiquitin ligase plays an important role in the regulation of tubular cell proliferation in progressive tubulointerstitial lesions in UUO kidneys.
The finding in this study was that proliferation of tubular epithelial cells was limited by the absence of Skp2. Although a significant increase in the number of renal tubular cells, which was associated with marked tubular dilatation, was observed in obstructed kidneys of Skp2+/+ mice, these changes were significantly less in obstructed kidneys of Skp2−/− mice. Moreover, proliferative tubular cells, which were positive for Ki67 and negative for p27, were decreased to a greater extent in obstructed kidneys of Skp2−/− mice than that of Skp2+/+ mice. We also confirmed that the p27 protein level was up-regulated more in obstructed kidneys of Skp2−/− mice than in Skp2+/+ mice. As shown in Figure 1, we found tubular dilatation in UUO kidney from Skp2+/+ (wild-type) mice that may be associated with the increment of renal epithelial cell number following cell proliferation. This is because the number of epithelial cells with tubular dilation significantly increased in Skp2+/+ mice (Figure 4A). In Skp2−/− mice, the increment of renal epithelial cell number following cell proliferation was inhibited by the accumulation of p27, and thereby tubular dilatation may be suppressed in UUO kidney. As well, architectural changes of the intracellular cytoskeleton should occur simultaneously and may also be involved in tubular dilatation. These results suggest that the increased p27, which resulted from Skp2 deficiency, limited cellular proliferation, and dilatation of renal tubules were suppressed in Skp2-deficient mice.
It is reported that the effects of CKI p27 and p21 on cell cycle regulation vary according to cell type in obstructed kidney. p27 is thought to play a role in limiting tubular epithelial cell proliferation21 and p21 to regulate interstitial cell proliferation.22 In our study, immunohistochemistry showed that there was no significant difference in the rate of increased p27-positive interstitial cells in obstructed kidney between Skp2−/− and Skp2+/+ mice (data not shown). Our results suggest that in this model p27 regulates proliferation of tubular epithelial cells rather than interstitial cells. Furthermore, we analyzed p21 protein level by Western blot assay. As shown in Supplemental Figure 1 at http://ajp.amjpathol.org, p21 levels were slightly increased in UUO kidney compared with CLK kidney in Skp2+/+ mice. Although p21 is reported to be another target for SCF-Skp2 ubiquitin ligase,26 p21 was only slightly accumulated in CLK kidney in Skp2−/− mice compared with CLK kidney in Skp2+/+ mice. Moreover, the increment of p21 was only slight in UUO kidney from Skp2−/− mice compared with that from Skp2+/+ mice (see Supplemental Figure 1 at http://ajp.amjpathol.org), whereas p27 was significantly increased in UUO kidney from Skp2−/− mice (Figure 5A). As described above, p21 has been suggested to regulate interstitial cell proliferation.22 Therefore, the absence of Skp2 may mainly contribute to an increment of p27 rather than p21, and thereby renal epithelial cell proliferation is suppressed and the renal damage ameliorated. The terminal deoxynucleotidyl transferase dUTP nick-end labeling assay showed reduced apoptosis of the tubular cells in obstructed kidneys from Skp2−/− mice. Renal tubular apoptosis after obstruction was thought to contribute to the progressive loss of renal function and accumulation of the extracellular matrix surrounding the lost cells.2 The weight of UUO kidney in Skp2+/+ mice was reduced. We presumed that tubular atrophy following apoptosis resulted in a significant loss of renal tissue. Augmentation of tubular cell proliferation and apoptosis has been demonstrated in p27 knockout mice.21 These data suggest that Skp2 was involved in renal tubular apoptosis following renal damage.
Moreover, we detected a change in tubulointerstitial fibrosis. In our study, a large area showed severe fibrosis in obstructed kidneys of Skp2+/+ mice, whereas it was milder in Skp2−/− mice. We suggest that the reduced tubular cell proliferation in UUO kidneys of Skp2−/− mice may be related to epithelial-mesenchymal transdifferentiation27,28,29 inhibition. We believe that the progression of renal damage, which was stopped in the early stage after obstruction by absence of Skp2 and renal fibrosis, was moderated in obstructed kidneys of Skp2−/− mice. Accordingly, Tashiro et al30 reported that proteasome inhibitors attenuated renal fibrosis in rat obstructive nephropathy. Consistent with our results, they suggest that proteasome inhibitors at least partially target Skp2-dependent proteolysis in obstructed kidneys. Skp2-siRNA drugs or small molecular Skp2 inhibitors may be useful as a specific therapy for renal diseases.
Taking all our findings into account, we suggest that Skp2 expression is induced by renal damage, and the subsequent proliferation of renal tubular epithelial cells is facilitated and tubulointerstitial fibrosis is enhanced in obstructive nephropathy. Therefore, Skp2 plays an important role in the progression of tubulointerstitial renal injury. However, the present data do not exclude the possibility that Skp2 could also target other molecules in addition to p27 in renal diseases; further studies are required to examine this.
Supplementary Material
Acknowledgments
We thank Dr. Chihaya Kakinuma and our laboratory members for helpful discussions.
Footnotes
Address reprint requests to Masatoshi Kitagawa, Department of Biochemistry 1, Hamamatsu University School of Medicine, 1-20-1 Handayama, Hamamatsu 431-3192, Japan. E-mail: kitamasa@hama-med.ac.jp.
Supported by grants-in-aid for Science Research from the Ministry of Education, Science, Sports, Culture, and Technology of Japan (to M.K. and K.K.) and COE (Center of Excellence) Program of Hamamatsu University School of Medicine funded by the Ministry of Education, Science, Sports, Culture, and Technology (to M.K.).
Supplemental material for this article can be found on http://ajp.amjpathol.org.
References
- Walton G, Buttyan R, Garcia ME, Olsson CA, Hensle TW, Sawczuk IS. Renal growth factor expression during the early phase of experimental hydronephrosis. J Urol. 1992;148:510–514. doi: 10.1016/s0022-5347(17)36641-7. [DOI] [PubMed] [Google Scholar]
- Klahr S, Morrissey J. Obstructive nephropathy and renal fibrosis. Am J Physiol. 2002;283:F861–F875. doi: 10.1152/ajprenal.00362.2001. [DOI] [PubMed] [Google Scholar]
- Couser WG, Johnson RJ. Mechanisms of progressive renal disease in glomerulonephritis. Am J Kidney Dis. 1994;23:193–198. doi: 10.1016/s0272-6386(12)80971-1. [DOI] [PubMed] [Google Scholar]
- Gobe GC, Axelsen RA. Genesis of renal tubular atrophy in experimental hydronephrosis in the rat: role of apoptosis. Lab Invest. 1987;56:273–281. [PubMed] [Google Scholar]
- Morgan DO. Principles of CDK regulation. Nature. 1995;374:131–134. doi: 10.1038/374131a0. [DOI] [PubMed] [Google Scholar]
- Sherr CJ, Roberts JM. Inhibitors of mammalian G1 cyclin-dependent kinases. Genes Dev. 1995;9:1149–1163. doi: 10.1101/gad.9.10.1149. [DOI] [PubMed] [Google Scholar]
- Nourse J, Firpo E, Flanagan WM, Coats S, Polyak K, Lee MH, Massague J, Crabtree GR, Roberts JM. Interlukin-2-mediated elimination of the p27kip1 cyclin-dependent kinases inhibitor prevented by rapamycin. Nature. 1994;372:570–573. doi: 10.1038/372570a0. [DOI] [PubMed] [Google Scholar]
- Polyak K, Lee MH, Erdjument-Bromage H, Koff A, Roberts JM, Tempst P, Massague J. Cloning of p27kip1, a cyclin-dependent kinases inhibitor and potential mediator of extracellular antimitogenic signals. Cell. 1994;78:59–66. doi: 10.1016/0092-8674(94)90572-x. [DOI] [PubMed] [Google Scholar]
- Coats S, Flanagan WM, Nourse J, Roberts JM. Requirement of p27kip1 for restriction point control of the fibroblast cell cycle. Science. 1996;272:877–880. doi: 10.1126/science.272.5263.877. [DOI] [PubMed] [Google Scholar]
- Shankland SJ, Pippin J, Flanagan M, Coats SR, Nangaku M, Gordon KL, Roberts JM, Couser WG, Johnson RJ. Mesangial cell proliferation mediated by PDGF and bFGF is determined by levels of the cyclin kinase inhibitor p27kip1. Kidney Int. 1997;51:1088–1099. doi: 10.1038/ki.1997.151. [DOI] [PubMed] [Google Scholar]
- Kamb A. Cell-cycle regulators and cancer. Trends Genet. 1995;11:136–140. doi: 10.1016/s0168-9525(00)89027-7. [DOI] [PubMed] [Google Scholar]
- Weinberg RA. The retinoblastoma protein and cell cycle control. Cell. 1995;81:323–330. doi: 10.1016/0092-8674(95)90385-2. [DOI] [PubMed] [Google Scholar]
- Weissman AM. Regulating protein degradation by ubiquitination. Immunol Today. 1997;18:189–198. doi: 10.1016/s0167-5699(97)84666-x. [DOI] [PubMed] [Google Scholar]
- Hershko A, Ciechanover A. The ubiquitin system. Annu Rev Biochem. 1998;67:425–479. doi: 10.1146/annurev.biochem.67.1.425. [DOI] [PubMed] [Google Scholar]
- Carrano AC, Eytan E, Hershko A, Pagano M. SKP2 is required for ubiquitin-mediated degradation of the CDK inhibitor p27. Nat Cell Biol. 1999;1:193–199. doi: 10.1038/12013. [DOI] [PubMed] [Google Scholar]
- Tsvetkov LM, Yeh KH, Lee SJ, Sun H, Zhang H. p27(Kip1) ubiquitination and degradation is regulated by the SCF(Skp2) complex through phosphorylated Thr187 in p27. Curr Biol. 1999;9:661–664. doi: 10.1016/s0960-9822(99)80290-5. [DOI] [PubMed] [Google Scholar]
- Nakayama K, Nagahama H, Minamishima YA, Matsumato M, Nakamichi I, Kitagawa K, Shirane M, Tsunematsu R, Tsukiyama T, Ishida N, Kitagawa M, Nakayama KI, Hatakeyama S. Targeted disruption of Skp2 results in accumulation of cyclin E and p27kip1, polyploidy and centrosome overduplication. EMBO J. 2000;19:2069–2081. doi: 10.1093/emboj/19.9.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrissey JJ, Ishidoya S, McCrachen R, Klahr S. Control of p53 and p21 (WAF1) expression during unilateral ureteral obstruction. Kidney Int. 1996;50(Suppl 57):S84–S92. [PubMed] [Google Scholar]
- Gerth JH, Kriegsmann J, Trinh TT, Stahl RA, Wendt T, Sommer M, Stein G, Wolf G. Induction of p27KIP1 after unilateral ureteral obstruction is independent of angiotensin II. Kidney Int. 2002;61:68–79. doi: 10.1046/j.1523-1755.2002.00111.x. [DOI] [PubMed] [Google Scholar]
- Schaefer L, Macakova K, Raslik I, Micegova M, Gröne HJ, Schönerr E, Robenek H, Echtermeyer FG, Grässel S, Bruckner P, Schaefer RM, Iozzo RV, Kresse H. Absence of decorin adversely influences tubulointerstitial fibrosis of the obstructed kidney by enhanced apoptosis and increased inflammatory reaction. Am J Pathol. 2002;160:1181–1191. doi: 10.1016/S0002-9440(10)64937-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ophascharoensuk V, Fero ML, Hughes J, Roberts JM, Shankland SJ. The cyclin-dependent kinases inhibitor p27kip1 safeguards against inflammatory injury. Nat Med. 1998;4:575–58. doi: 10.1038/nm0598-575. [DOI] [PubMed] [Google Scholar]
- Hughes J, Brown P, Shankland SJ. Cyclin kinase inhibitor p21CIP1/WAF1 limits interstitial cell proliferation following ureteric obstruction. Am J Physiol. 1999;277:F948–F956. doi: 10.1152/ajprenal.1999.277.6.F948. [DOI] [PubMed] [Google Scholar]
- Sheehan DC, Hrapchak B. Columbus: Battelle Press,; Theory and Practice of Histotechnology. 1980:pp 188–194. [Google Scholar]
- Sutterlüty H, Chatelain E, Marti A, Wirbelauer C, Senften M, Müller U, Krek W. p45SKP2 promotes p27Kip1 degradation and induces S phase in quiescent cells. Nature Cell Biol. 1999;1:207–214. doi: 10.1038/12027. [DOI] [PubMed] [Google Scholar]
- Gstaiger M, Jordan R, Lim M, Catzavelos C, Mestan J, Slingerland J, Krek W. Skp2 is oncogenic and overexpressed in human cancers. Proc Natl Acad Sci USA. 2001;98:5043–5048. doi: 10.1073/pnas.081474898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein G, Bloom J, Sitry-Shevah D, Nakayama K, Pagano M, Hershko A. Role of the SCFSkp2 ubiquitin ligase in the degradation of p21Cip1 in S phase. J Biol Chem. 2003;278:25752–25757. doi: 10.1074/jbc.M301774200. [DOI] [PubMed] [Google Scholar]
- Zeisberg M, Kalluri R. The role epithelial-to mesenchymal transition in renal fibrosis. J Mol Med. 2004;82:175–181. doi: 10.1007/s00109-003-0517-9. [DOI] [PubMed] [Google Scholar]
- Hay ED, Zuk A. Transformations between epithelium and mesenchyme: normal, pathological, and experimentally induced. Am J Kidney Dis. 1995;26:678–690. doi: 10.1016/0272-6386(95)90610-x. [DOI] [PubMed] [Google Scholar]
- Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;112:1776–1784. doi: 10.1172/JCI20530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashiro K, Tamada S, Kuwabara N, Komiya T, Takekida K, Asai T, Iwao H, Sugimura K, Matsumura Y, Takaoka M, Nakatani T, Miura K. Attenuation of renal fibrosis by proteasome inhibition in rat obstructive nephropathy: possible role of nuclear factor kappaB. Int J Mol Med. 2003;12:587–592. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.