SYNOPSIS
Objective.
We assessed fetal death certificates (FDCs) as a source of surveillance for stillbirths with birth defects by linkage with data from the Metropolitan Atlanta Congenital Defects Program (MACDP), a population-based birth defects surveillance system.
Methods.
Stillbirths with defects in MACDP were identified from 1994 through 2002 and linked to FDCs. Sensitivity of FDCs for capturing stillbirths with defects was estimated, and predictors for a case being reported were assessed. Concordance for selected variables from each data source was evaluated.
Results.
Two hundred twenty-four of 257 stillbirths with birth defects in MACDP were linked to an FDC (linkage rate = 87.2%; 95% confidence interval [CI] 82.4, 91.0). Stillbirths of non-Hispanic black and Hispanic/other mothers were more likely to be issued an FDC (odds ratio [OR] = 5.6 [95% CI 1.9, 17.0] and 14.0 [95% CI 1.7, 114.0], respectively). Cases undergoing autopsy were more likely to be issued an FDC (OR=3.2; 95% CI 1.1, 8.7). Performance of an amniocentesis was poorly recorded on FDCs. The sensitivity and positive predictive value of FDCs for selected classes of defects ranged from 10% to 70% and 25% to 93%, respectively.
Conclusions.
Compared to FDCs, MACDP's active case identification improves the ascertainment of stillbirths with birth defects and the quality of certain recorded data.
Stillbirth (intrauterine fetal death at 20 or more weeks of gestation or 350 or more grams, if age is unknown) is one of the most common adverse outcomes of pregnancy. In the United States, an estimated seven stillbirths occur for every 1,000 live births, accounting for about half of all perinatal deaths.1–4 Nonetheless, the literature on population-based surveillance of stillbirths is limited compared with that of other adverse pregnancy outcomes, such as preterm delivery, low birth weight, and birth defects.5
Although vital records might be a logical source of such surveillance data, use of vital records for surveillance purposes has been problematic.6–11 Fetal deaths are by law a reportable event in most states. However, fetal deaths, and in particular early fetal deaths, are underreported for a variety of reasons.12–15 In addition, uncertainties about the quality of the data recorded raise questions about the adequacy of these registries for monitoring and conducting etiologic studies.15,16
The most comprehensive, population-based stillbirth surveillance and evaluation program to date in the U.S. is the Wisconsin Stillbirth Service Project (WiSSP), an independent stillbirth assessment program. Established in 1983, WiSSP provides a unique method for collecting and analyzing information about primarily fetal causes of stillbirth.12 WiSSP has demonstrated that passive fetal death reporting through vital records underestimates the occurrence of this event and also yields inaccurate information concerning fetal-related causes of death.15 It has also provided ongoing education and training in both the need for and use of specific evaluation protocols to health-care facilities throughout Wisconsin.
WiSSP has long served as a model stillbirth evaluation program, yet most states do not have the resources to support such a program. Existing population-based birth defect surveillance programs employing active case ascertainment, however, might be able to provide an infrastructure for collecting, analyzing, and reporting surveillance data on stillbirths. As a preliminary step, it would be useful to determine whether the data collected by a surveillance program on stillbirths with birth defects enhance the data collected by FDCs.
In this study, we used data from the Metropolitan Atlanta Congenital Defects Program (MACDP), a birth defects surveillance system in operation since 1967 and administered by the Centers for Disease Control and Prevention (CDC) to evaluate the completeness of ascertainment of stillbirths with birth defects in FDCs and the quality of the information they provide.17
METHODS
Study population
MACDP actively monitors birth defects occurring among residents of five counties in metropolitan Atlanta with more than 50,000 births annually. Infants, fetuses, and children with birth defects are identified on an ongoing, regular basis by trained abstractors who visit birth hospitals, pediatric hospitals, specialty clinics, and perinatal offices to actively review multiple data sources. Cases with potential birth defects are also identified via regular and systematic review of vital records. Cases are therefore ascertained from multiple sources and include malformations in stillborn infants, defined as a fetal death occurring at 20 or more completed weeks of gestation, or 350 or more grams if the gestational age is unknown.18
For this study, we focused on cases among stillborn infants born from 1994 through 2002. We selected this time period because 1994 was the first year for which we were able to obtain electronic fetal death records, and when this analysis began, 2002 was the most recent year for which ascertainment of birth defects was considered complete. All records of stillbirths with birth defects during the years 1994 through 2002 and recorded in MACDP were identified and treated as the reference group (n=257).
Linkage of MACDP and fetal death records
Fetal deaths occurring at any gestational age are by law a reportable event in Georgia; they are reported using the revised U.S. Standard Report of Fetal Death. MACDP obtains an electronic copy of the fetal death records for the state of Georgia on a monthly basis. The records of stillbirths identified in MACDP were linked to fetal death vital records for the same birth cohort (1994–2002) by means of a deterministic matching process with multiple iterations using the following variables: mother's name and race, father's name, fetal gender, date of event, hospital, county of residence, and address at the time of birth.
Sensitivity of FDCs
Using MACDP stillbirth cases as the gold standard, we first estimated the sensitivity of vital records for capturing stillbirths with birth defects as the percent (with 95% confidence intervals [CIs]) of MACDP stillbirth cases captured by the FDCs. This is termed the linkage rate and was calculated for early (≤28 weeks of gestation) and late/term (>28 weeks of gestation) fetal deaths. For those MACDP stillbirth cases that could not be linked to vital records, we repeated the same process using live birth records to identify stillbirths potentially misclassified as live births. MACDP abstraction data record forms were retrieved and reviewed for those cases that linked to a live birth certificate to confirm that they were stillbirths, indicated by a one-minute Apgar score of zero.
Predictors of FDCs
Multivariate logistic regression was used to assess predictors for whether or not a stillbirth with a defect was issued an FDC. Stillbirths linked to a birth certificate were excluded. Variables evaluated were maternal age and race/ethnicity, gestational age, birth weight, county of residence, autopsy status, and selected classes of birth defects. Adjusted odds ratios (AORs) and 95% CIs were reported for the final model containing race/ethnicity and autopsy status, with and without gestational age included, as gestational age has been shown to be a predictor for whether a fetal death is reported to vital records.15
Concordance of information reported on MACDP and FDC
For cases with records in both MACDP and FDC, the concordance of certain information from each data source was calculated. For categorical variables, a simple kappa statistic (κ) was calculated, as this statistic accounts for percent agreement due to chance.19 The concordance of autopsy status could not be assessed because the U.S. Standard Report of Fetal Death in use for this time period did not record this information. For the continuous variables, maternal age, gestational age, and fetal birth weight, a correlation coefficient was calculated for agreement between each data source. Jittered scatter plots were also constructed to visually assess the extent of correlation between data sources. Finally, the sensitivity and positive predictive value (PPV) of FDCs for reporting any birth defect were evaluated.
Selected birth defect categories were also evaluated separately and included anencephaly, spina bifida, cleft lip and/or palate, Down's syndrome, heart defect, omphalocele, and renal agenesis. These defects were chosen because they are specifically listed on the FDC, and providers are to indicate if the defect was present or absent. All analyses were conducted using SAS.20
RESULTS
There were 407,155 live births and 4,050 stillbirths recorded among residents of the five-county MACDP catchment area for the years 1994–2002. For this time period, MACDP recorded 257 (1.9%) stillbirths with defects in a cohort of 13,275 (96.2%) live births and 266 (1.9%) elective terminations with defects. Two hundred twenty-four of the stillbirths in MACDP linked to an FDC, giving an overall linkage rate of 87.2% (95% CI 82.4, 91.0). The linkage rate for early fetal deaths was 84.7% (95% CI 77.4, 90.4) compared with 92.0% (95% CI 85.0, 95.9) for fetal deaths occurring at more than 28 completed weeks of gestation. Three of the unreported cases linked to a live birth certificate.
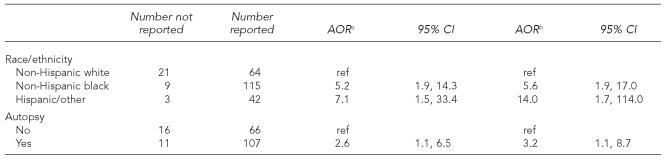
The mean gestational age and weight for cases that were not reported were 27.9 weeks and 1,046 grams, compared with 28.7 weeks and 1,203 grams for those that were reported. These differences were not statistically significant; however, there were significant differences in race/ethnicity and autopsy status for those reported vs. those not reported (p=0.0004 and 0.0381, respectively). Compared with stillbirths of non-Hispanic white mothers, stillbirths of non-Hispanic black and Hispanic/other mothers were more likely to be reported to fetal death vital records after adjusting for autopsy status and gestational age (AOR55.6 [95% CI 1.9, 17.0] and 14.0 [95% CI 1.7, 114.0]). Cases that underwent an autopsy also were more likely to be reported after adjusting for race/ethnicity and gestational age (AOR=3.2 [95% CI 1.1, 8.7]) (Table 1). County of residence and class of birth defect (anencephaly, spina bifida, heart defect, cleft lip/palate, renal agenesis, Down's syndrome, omphalocele) did not predict whether or not a case was issued an FDC (data not shown).
Table 1.
Adjusted odds ratios for an MACDP case of stillbirth with defects being reported on a fetal death certificate, 1994–2002
Adjusted for race/ethnicity and autopsy
Adjusted for race/ethnicity, autopsy, and gestational age
MACDP = Metropolitan Atlanta Congenital Defects Program
AOR = adjusted odds ratio
CI = confidence interval
Ref = reference group
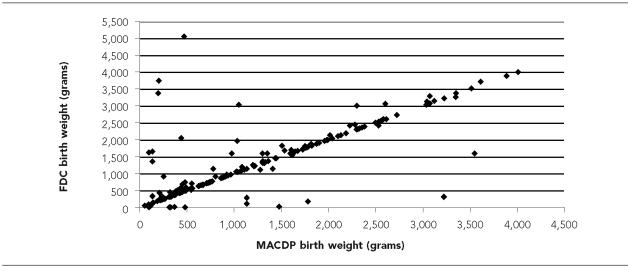
Evaluation of the concordance in the information from the two data sources revealed poor agreement relative to whether an amniocentesis was performed (κ=0.08 [95% CI 0.06, 0.22]). Maternal age and gestational age were evaluated as continuous variables and had very good agreement with correlation coefficients of 0.98 (Pearson) and 0.96 (Spearman), respectively. Fetal weight had slightly less but good agreement as well, with an overall Spearman correlation coefficient of 0.80 (Figure 1).
Figure 1.
Birth weight of stillbirths with defects as recorded in MACDP vs. FDCs, 1994–2002
MACDP = Metropolitan Atlanta Congenital Defects Program
FDC = fetal death certificate
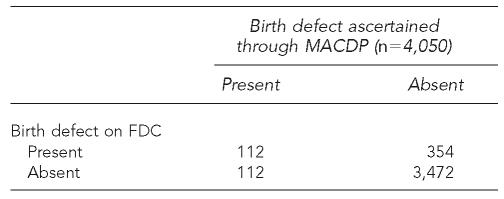
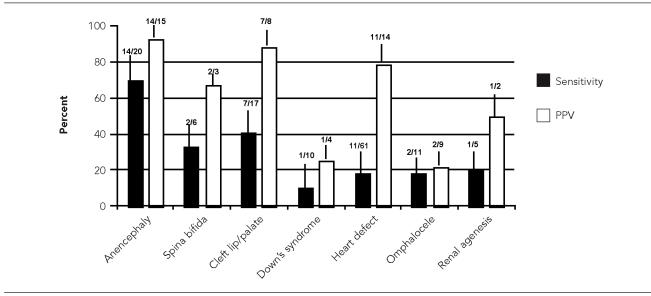
For the 224 stillbirths with defects in MACDP, the sensitivity of FDCs for indicating that any defect was present was only 50%. FDCs also had a high percentage of false positives, yielding a PPV of 24% (Table 2). For the selected birth defects examined, the sensitivity ranged from 10% for Down's syndrome to 70% for anencephaly, and the PPV ranged from 25% for Down's syndrome to 93% for anencephaly (Figure 2).
Table 2.
Comparison of the reporting of birth defects by FDCa and MACDP, Atlanta, 1994–2002
Sensitivity = 0.50, specificity = 0.91, positive predictive value = 0.24
FDC = fetal death certificate
MACDP = Metropolitan Atlanta Congenital Defects Program
Figure 2.
Sensitivity and positive predictive value of FDCs for selected birth defects compared with MACDP, 1994–2002
FDC = fetal death certificate
MACDP = Metropolitan Atlanta Congenital Defects Program
PPV = positive predictive value
DISCUSSION
This study illustrated some of the limitations associated with using FDCs to monitor the occurrence of stillbirths with birth defects. In this study, FDCs captured about 13% fewer stillbirths with defects than did MACDP. Underreporting did not appear to be random: stillbirths of mothers who were of a race/ethnicity other than non-Hispanic white, or who had an autopsy, were much more likely to be issued an FDC. The accuracy of information recorded on FDCs for stillbirths with defects varied, with maternal age, gestational age, and fetal weight having reasonably good agreement with MACDP data. On the other hand, performance of an amniocentesis was less accurately recorded on the FDC. The overall sensitivity of FDCs for identifying any defect was only 50%.
Our data support previous findings described in the literature. Goldhaber and Greb et al. have both demonstrated that nonreporting of fetal deaths to vital registries is not random.14,15 Goldhaber demonstrated that fetal death ratios (per live births) can be significantly affected by the underreporting of early fetal deaths.14 Furthermore, Greb et al. showed that the mean gestational age and birth weight for fetal deaths not reported vs. those that were reported were 24.3 vs. 33.4 weeks for gestational age and 646 vs. 1,906 grams for birth weight, respectively.15 In our data, gestational age and birth weight were not significantly associated with the likelihood of a fetal death with a birth defect being issued an FDC, suggesting that the presence of a birth defect may minimize such reporting biases. Maternal race and autopsy status, on the other hand, were both associated with a stillbirth being issued an FDC.
The association of race/ethnicity and issuance of an FDC is interesting. In the same MACDP population, Siffel et al., in a study looking at the impact of prenatal diagnosis on the live birth prevalence of Down's syndrome, demonstrated that among Down's syndrome pregnancies in women 35+ years of age, black women had a lower proportion of elective terminations compared with white women.21 Because autopsies are less likely to be performed on stillbirths than on deaths after birth,22,23 a race/ethnicity differential for other prenatally diagnosed birth defects might explain in part the observed associations of race/ethnicity and autopsy with issuance of FDCs. The extent to which elective terminations varied by race/ethnicity for other birth defects in our data is not clear at this time. However, we are planning a study to examine these differentials by race/ethnicity and autopsy further among all stillbirths and with a larger sample size.
The main strength of this study involved the use of MACDP stillbirth cases with defects as a gold standard reference for evaluating FDCs. MACDP is population-based and uses trained abstractors for active case ascertainment and data abstraction. Cases are identified using multiple sources, including FDCs, to enhance completeness. Our study was limited, however, in that we were only able to evaluate stillbirths with identified major structural malformations. An evaluation of FDCs for all stillbirths in this population was not possible, as MACDP ascertains and records data for stillbirths with birth defects only. Therefore, our results could not be generalized to all stillbirths.
This study was further limited by the relatively small number of stillbirths identified. Therefore, the results should be interpreted accordingly, especially when considering the factors predicting whether or not an FDC was issued. The factors that fully explain whether an FDC was issued are likely multifaceted and require further evaluation. Additionally, it is unknown how these factors interrelate in different geographical populations; the degree of underascertainment may not be uniform across populations. The factors influencing this systematic underestimation of birth weight need to be further evaluated, but may represent miscoding of units in some cases. Concordance of information should be evaluated for all stillbirths to better examine systematic errors.
CONCLUSION
More accurate estimates of stillbirth occurrence and improvements in the quality and reliability of data recorded are needed if meaningful population-based etiologic studies are to be conducted. The expansion of existing active, population-based birth defects surveillance programs to include information on stillbirths—with or without defects—could potentially enhance the completeness and quality of the data derived from fetal death vital registries. FDCs are generally considered complete after one year; MACDP tracks birth defects and is considered complete after two years. However, because clinical follow-up is not done in the case of stillbirth, information on this outcome would be considered complete much sooner.
Pilot studies to assess the feasibility, cost, and effectiveness of expanding MACDP or similar programs to incorporate data on all stillbirths are needed. Reliability and quality of recorded fetal death data could also presumably be improved through the development and implementation of strategies to raise awareness of stillbirths as a public health issue, to emphasize the importance of documenting key variables, and to educate health-care providers in the use of postmortem evaluation protocols.
Acknowledgments
The authors gratefully acknowledge the support of Don Gambrell and many others from the Metropolitan Atlanta Congenital Defects Program and the Georgia Department of Human Resources.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Fretts RC. Etiology and prevention of stillbirth. Am J Obstet Gynecol. 2005;193:1923–35. doi: 10.1016/j.ajog.2005.03.074. [DOI] [PubMed] [Google Scholar]
- 2.Goldenberg RL, Kirby R, Culhane JF. Stillbirth: a review. J Matern Fetal Neonatal Med. 2004;16:79–94. doi: 10.1080/14767050400003801. [DOI] [PubMed] [Google Scholar]
- 3.Pauli RM, Reiser CA, Lebovitz RM, Kirkpatrick SJ. Wisconsin Stillbirth Service Program: I. Establishment and assessment of a community-based program for etiologic investigation of intrauterine deaths. Am J Med Genet. 1994;50:116–34. doi: 10.1002/ajmg.1320500204. [DOI] [PubMed] [Google Scholar]
- 4.Yuan H, Platt RW, Morin L, Joseph KS, Kramer MS. Fetal deaths in the United States, 1997 vs. 1991. Am J Obstet Gynecol. 2005;193:489–95. doi: 10.1016/j.ajog.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Pauli RM, Reiser CA. Wisconsin Stillbirth Service Program: II. Analysis of diagnoses and diagnostic categories in the first 1,000 referrals. Am J Med Genet. 1994;50:135–53. doi: 10.1002/ajmg.1320500205. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez SR, Mallonee S, Archer P, Gofton J. Evaluation of death certificate-based surveillance for traumatic brain injury—Oklahoma 2002. Public Health Rep. 2006;121:282–9. doi: 10.1177/003335490612100310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watkins ML, Edmonds L, McClearn A, Mullins L, Mulinare J, Khoury M. The surveillance of birth defects: the usefulness of the revised U.S. standard birth certificate. Am J Public Health. 1996;86:731–4. doi: 10.2105/ajph.86.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Northam S, Knapp TR. The reliability and validity of birth certificates. J Obstet Gynecol Neonatal Nurs. 2006;35:3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 9.Hoyert DL, Martin JA. Vital statistics as a data source. Semin Perinatol. 2002;26:12–6. doi: 10.1053/sper.2002.29835. [DOI] [PubMed] [Google Scholar]
- 10.Honein MA, Paulozzi LJ. Birth defects surveillance: assessing the “gold standard.”. Am J Public Health. 1999;89:1238–40. doi: 10.2105/ajph.89.8.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin JA, Hoyert DL. The national fetal death file. Semin Perinatol. 2002;26:3–11. doi: 10.1053/sper:2002.29834. [DOI] [PubMed] [Google Scholar]
- 12.Pauli RM, Reiser CA. The Wisconsin Stillbirth Service Project: the ”Wisconsin idea” in practice. Wisconsin Acad Rev. 1984;31:62–4. [Google Scholar]
- 13.Buck GM, Johnson CD. Methodologic considerations for population-based research on fetal deaths: overcoming data gaps. Semin Perinatol. 2002;26:31–5. doi: 10.1053/sper.2002.29837. [DOI] [PubMed] [Google Scholar]
- 14.Goldhaber MK. Fetal death ratios in a prospective study compared to state fetal death certificate reporting. Am J Public Health. 1989;79:1268–70. doi: 10.2105/ajph.79.9.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greb AE, Pauli RM, Kirby RS. Accuracy of fetal death reports: comparison with data from an independent stillbirth assessment program. Am J Public Health. 1987;77:1202–6. doi: 10.2105/ajph.77.9.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lydon-Rochelle MT, Cardenas V, Nelson JL, Tomashek KM, Mueller BA, Easterling TR. Validity of maternal and perinatal risk factors reported on fetal death certificates. Am J Public Health. 2005;95:1948–51. doi: 10.2105/AJPH.2004.044305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Correa-Villasenor A, Cragan J, Kucik J, O'Leary L, Siffel C, Williams L. The Metropolitan Atlanta Congenital Defects Program: 35 years of birth defects surveillance at the Centers for Disease Control and Prevention. Birth Defects Res A Clin Mol Teratol. 2003;67:617–24. doi: 10.1002/bdra.10111. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics (US) Model State Vital Statistics Act and Regulations, 1992 Revision. 1995. DHHS Publication No. (PHS) 94-1115.
- 19.Fleiss JL. 2nd ed. New York: John Wiley and Sons; 1981. Statistical methods for rates and proportions. [Google Scholar]
- 20.SAS Institute. SAS: Version 9.1. Cary (NC): John Wiley and Sons; 2004. [Google Scholar]
- 21.Siffel C, Correa-Villasenor A, Cragan J, Alverson CJ. Prenatal diagnosis, pregnancy terminations and prevalence of Down's syndrome in Atlanta. Birth Defects Res A Clin Mol Teratol. 2004;70:565–71. doi: 10.1002/bdra.20064. [DOI] [PubMed] [Google Scholar]
- 22.Magee JF. Investigation of stillbirth. Pediatr Dev Pathol. 2001;4:1–22. doi: 10.1007/s100240010121. [DOI] [PubMed] [Google Scholar]
- 23.Michalski ST, Porter J, Pauli RM. Costs and consequences of comprehensive stillbirth assessment. Am J Obstet Gynecol. 2002;186:1027–34. doi: 10.1067/mob.2002.122450. [DOI] [PubMed] [Google Scholar]