SYNOPSIS
Federally Qualified Health Centers (FQHCs) contribute greatly to reducing health disparities by providing care to underserved communities. Yet these safety-net clinics face chronic manpower shortages and turnover. Practice-Based Research Networks aid in translating medical science from bench to clinical practice. These networks have been used to understand and improve health-care delivery and reduce disparities. Initiatives to strengthen lagging translational research in dentistry have begun, but there is no FQHC research network that addresses oral health.
This article reviews the potential for, and outlines a model of, an Oral Health FQHC Research Network. It characterizes the needs for an FQHC research network, describes a successful FQHC research-oriented program, and outlines an Oral Health FQHC Research Network conceptual model. It argues that strengthening FQHCs through involvement of their dental staff in clinical research may enhance their jobs, draw staff closer to the community, and strengthen their ability to reduce health disparities.
Federally Qualified Health Centers (FQHCs), community health centers (CHCs), and migrant health centers provide much of the care for vulnerable populations1 and contribute substantially to the reduction of inequities in health.2 Nevertheless, oral health disparities, particularly among poverty-stricken or underserved communities, continue to remain great and difficult to address despite recent overall improvements in U.S. oral health.3
These disparities result from a complex interaction of behaviors, socioeconomic conditions, and oral health services access, delivery, and utilization. Some of these factors play more important roles in certain populations, but knowledge to help FQHCs address these specific differences often is not available due to lack of research in these populations. Furthermore, FQHCs are often stymied in providing dental care by chronic dentist shortages and turnover. Many young, inexperienced dentists move through FQHC clinics, which helps them pay back school loans and gain clinical experiences. But beyond that period, FQHCs offer few career advancement incentives to draw long-term commitments.4 At the same time, the safety-net clinics need experienced dentists able to provide high-quality care to our country's most vulnerable residents.
Translation of scientific advances, particularly in preventive medical care, to the network of CHC programs has contributed to improving overall health. This advance, in part, can be attributed to the establishment of primary-care Practice-Based Research Networks (PBRNs) in medicine to better understand, study, and improve health-care delivery.5,6 These partnerships are designed to enhance the interest of the clinicians in science-based inquiry; to increase community participation and promote equitable partnerships among institutions, clinician researchers, and the community; to address issues of primary concern to clinicians and the community; and to assure greater dissemination of findings from research that can be of benefit to clinicians and the community.5,6 This kind of ownership of the research process ties the clinicians to the community in a stronger way than usual and may contribute to a more interesting career and less turnover in FQHCs.
In 2005, the National Institute of Dental and Craniofacial Research (NIDCR) awarded $75 million to fund three regional dental PBRNs that would perform short-term, clinical research and observational studies, primarily in private practice. This NIDCR initiative is important and undoubtedly will result in enhanced, practical, and evidence-based care, but is not sufficient as private practices generally include a very small population of those with the greatest oral health disparities. More frequently, it is the FQHC with its comprehensive health-care programs that serves these populations,7 and work is needed to increase the participation of such populations and clinical settings in oral health research. Such an approach will not only increase the usefulness of research findings, it will also strengthen the clinics themselves.
In 2001, NIDCR and the National Center on Minority Health and Health Disparities sponsored the establishment of Centers for Research to Reduce Oral Health Disparities. These university-based centers have invested major efforts in addressing the needs of communities with poor oral health and have forged partnerships with dental societies, health agencies, FQHCs, and institutions that serve diverse populations.8 However, these relationships are generally specific between the particular disparities center and community or FQHC. For example, the partnership between the center at the University of Washington (UW) and the Yakima Valley Farm Workers Clinic (YVFWC) system has resulted in collaborative research with results that have altered and improved oral health-care delivery.
These community-university collaborations are challenging to cultivate and take time to develop. Moreover, the resulting benefits of the research collaborative may be too narrow to generalize to other communities. Both the community and the university side of the partnership may lack capacity to effectively engage in multi-FQHC research relationships, as evidenced by the absence of such multicenter oral health research in the literature.
As we demonstrate in this article, the environment for fundamental and translational research in vulnerable communities and their care facilities is multidimensional and complex. Yet we assert that the U.S. will have little success in dealing with oral health inequities absent a serious effort to further engage these communities and the oral health providers who serve them. To effectively conduct research to address oral health disparities, the active participation of the FQHC and the communities they serve is critically important. Thus, it is essential that research institutions develop the capacity to effectively engage these important community partners.
Furthermore, it is necessary for funders to appreciate the unique research opportunities that FQHCs offer to address oral health disparities and commit sustainable support and resources to promote research at FQHCs. In medical and behavioral health, peer-support networks have been widely used and highly effective in facilitating communication, developing trust, and establishing or maintaining goals among those with similar challenges.9 For these reasons, it is necessary to think about an alternative approach by creating research networks of FQHCs and FQHC-like clinics to study issues relevant to community oral health.
This article explores the development of an Oral Health FQHC Research Network to fill the current gap and develop capacity for FQHCs and the communities they serve to take charge of and direct research that best responds to the clinicians' and community's needs and priorities. Specifically, this article will:
Define the needs for an Oral Health FQHC Research Network;
Describe a case study of an FQHC ready for a research network; and
Define a conceptual model of an Oral Health FQHC Research Network.
THE NEED FOR NETWORKS AND WORKFORCE TO ADDRESS ORAL HEALTH DISPARITIES
In 2005, there were 952 federally funded FQHCs and approximately 100 FQHC Look-Alikes.10 Many of these clinics employed dentists and provided dental care as part of their mandate. Through a research network, these FQHC and FQHC-like centers could provide potential answers to oral health concerns and define best practices for at least 30% of the U.S. population and the majority of underserved populations. Forrest and Whelan2 reported that populations with the greatest health disparities (i.e., ethnic minorities, government-insured and noninsured, and rural dwellers) were more likely to visit FQHCs. Thus, it may be more appropriate for FQHCs to develop their own oral health research networks independent from traditional, practice-based clinics (i.e., private-practice clinics). The needs of their communities and the environments within which the dentists and other oral health providers work may not be comparable, making it difficult to interpret published research and design appropriate treatment or preventive programs.
Oral health disparity is a complex issue that is influenced by many factors, including environment, society, and culture. A recently developed conceptual model for reducing oral health disparities, designed by our colleagues,11 describes levels of influence on oral health and oral health disparities over the life cycle. The model incorporates several levels of influence on health and well-being, such as distal/macro influences (i.e., natural environment, organization and delivery of services, and manpower), intermediate influences (i.e., community—physical, social, and cultural environments), interpersonal influences (i.e., stressors, support, infectious transmission), proximal/individual influences (i.e., biological processes, health behaviors, types and use of services, and individual psychology), and health/well-being influences (i.e., health outcomes and quality of life). This model is useful for guiding FQHCs and the communities they serve to develop research agendas that address one or several of these levels of influence in the causal pathway.
The model also reinforces the need for a stable and experienced health professional workforce. For example, the FQHC may want to focus its research efforts on intermediate or community factors, such as access to oral health care, by evaluating the efficacy and cost/benefit of providing language training for dental clinicians as part of their jobs. This, in turn, could increase adherence to professional advice and help community members make better choices regarding their own oral health. This strategy might be compared to employing professional language interpreters.
YVFWC: CASE STUDY FOR AN FQHC READY FOR AN FQHC RESEARCH NETWORK
The YVFWC is a large community/migrant health center system providing wide-ranging health-care services to eight large communities in Washington State and five communities in Oregon. The YVFWC has 15 medical facilities, nine dental facilities, and six mental health facilities. It has more than 1,400 full- and part-time employees, including 125 medical providers and 25 dentists. The YVFWC also offers other family service programs, including Women, Infants, and Children (WIC) and nutritional services; behavioral health services; human immunodeficiency virus/acquired immunodeficiency syndrome care; drug and alcohol treatment; and community health services.
Its patient population is primarily Hispanic (63%) and Caucasian (34%), and 66% of families served have incomes at or below the federal poverty level. In 2005, 123,000 patients were served and 42% of these were seasonal or migrant farm workers.12 Additionally, YVFWC collaborated with UW to develop two dental residency programs (Advanced Education in General Dentistry and Pediatric Dentistry) and also offers short-term clinical experiences for dental as well as medical students. Some of the clinicians and dentists have clinical faculty appointments at UW and have access to UW resources. There is regular contact between the departments at the dental school and the clinics.
The size, strength, and experience of the YVFWC have led to more equitable relationships with the university dental school. For example, the YVFWC offers university undergraduate and graduate dental students a rigorous clinical training site in which to serve populations with diverse racial and income status and gain an appreciation of health disparities in these populations. Furthermore, the expanded academic and research environments at YVFWC have enhanced YVFWC's ability to recruit and retain exceptional clinicians. A growing number of clinicians are engaging in research and remaining in the system well beyond the typical four- to five-year tour.
Research within the YVFWC
Numerous requests by the local universities to collaborate with the YVFWC in research on environmental and occupational health, maternal and child health, and oral health prompted it to gain experience in research skills and methodology, develop capacity to initiate its own research, and evaluate and make informed decisions about the types of research with which it would become involved. It also saw research as a way to understand and address the needs of its clinical staff and the communities it serves.
The YVFWC set in motion the steps it needed to evaluate, make decisions about, and learn from implemented studies. First, it developed policy and procedure to institutionalize the decision making around research involvement. The organizational policy clearly states that the primary purpose of the organization is service delivery, and that the organization is interested in research involvement when it advances and supports that mission. Next, it developed the structure to support the research review process (i.e., Research Review Committee [RRC]/Health Insurance Portability and Accountability Act of 1996 [HIPAA] Privacy Board, Community Advisory Committee) and adopted the UW Principles of Community-based Research for itself and its collaborators.13
The RRC/HIPAA Privacy Board comprises clinical directors and nonclinical members. Its charge is to review and evaluate the proposed research studies for compliance with organizational policies and procedures and for support from within the organization's clinical and management staff. While the review may appear similar to an Institutional Review Board (IRB), it does not replace the need for the researcher's IRB approval. Institutional review is required by the YVFWC RRC prior to final approval of any research. Additionally, YVFWC develops time-limited Community Advisory Committees for specific programs or research. The YVFWC also reviews clinics' needs assessment and community challenges for potential research topics, and it proactively seeks institutional collaborators with similar interests and expertise to jointly develop and conduct research.
The process that YVFWC uses to decide whether to accept outside research has been firmly established. A proposed research project from outside the organization must have a clinic sponsor, who serves as a primary internal contact for the outside researcher. The divisions involved with the proposed research provide input to the RRC, which in turn determines applicability and interest in the research. Once the project is approved, the clinic sponsor takes responsibility for ensuring that the outside researcher complies with YVFWC policies and procedures (e.g., making a final report to YVFWC about the study outcome and allowing for feedback prior to publication) and any conditions put on the project.
Rather than restricting the organization's involvement in research, YVFWC has found that putting the structure and processes described in place has actually increased its research involvement. The number of research projects reviewed and approved by its RRC has steadily grown over the past several years. Not only has the number of projects increased, but they also are more closely aligned with the YVFWC's core mission and priorities. In addition, approved research projects have provided a basis upon which to establish relationships with researchers that have led to the development of more sophisticated projects that will bring more resources to the organization and the community.
MODEL OF AN ORAL HEALTH FQHC RESEARCH NETWORK: HOW IT CAN IMPROVE ORAL HEALTH
Conceptual model of FQHC Research Networks to conduct translational research to reduce oral health disparities
A conceptual model of an FQHC Research Network proposed framework is illustrated in Figure 1. The FQHCs are the principal drivers of the research agendas, with the communities and academic institutions/researchers/grantors functioning in advisory and collaborative roles. The dashed lines indicate the collaborative/advisory nature of the different entities' impact on the process. Both the communities and academic institutions/researchers/grantors may provide expertise and assist the FQHCs in exploring and setting the research agendas, but the FQHCs principally determine the final agenda.
Figure 1.
Conceptual model of an FQHC research network
FQHC = Federally Qualified Health Center
For example, the FQHCs may want to focus their research efforts on preventive strategies for childhood caries but are unsure of who the target audience should be, how best to approach the research question and recruit the specific population, and which strategies may work best for their clinics. FQHCs may enlist the help of institutions/researchers to assist them in developing specific, researchable questions, and help them identify individuals with expertise about specific strategies. FQHCs may also gain the advice and insight of community leaders on approaches to recruitment and retention. Researchers would help refine the questions, protocols, and strategies, but would not be the principal developers of the research questions.
As shown in Figure 1, after the research agenda has been set and the research has been completed, the FQHCs as principal investigators interpret the research outcomes. Again, institutions, researchers, and the communities may serve in a collaborative and advisory capacity to provide data analysis expertise, help interpret and present the findings, or provide alternative perspectives. For example, the FQHCs might go back to the community with the data and ask community members for their perspectives on the interpretation as well as how the information should be used and disseminated. This step helps avoids stigmatizing the community. After research outcomes are interpreted, the FQHC can use that information to do one or all of the following: change clinical practice, develop and implement a health program, and disseminate the information or program. One or all of these events may lead to improved community health and reduction of disparity.
An illustration of the model using a fabricated example follows. A study was done on having medical providers apply topical fluoride varnish during well-child visits. A previous assessment found that the majority (80%) of children seen at the FQHC clinics experience tooth decay by age 3, and the clinics posited that having the medical providers—who see almost every child—deliver this service would increase its availability and reduce disease. The FQHC studied short- and long-term variables (i.e., impact on clinicians and clinical visits and tooth decay outcomes) and found that the medical providers did not feel overly burdened by adding fluoride varnish applications to their well-child exams. The study also showed that dental decay was reduced in children who received the varnish compared to those who did not. From this information, the FQHC could decide to change its clinical practice and incorporate fluoride varnish applications into their well-child visits.
Concurrently, an educational program could be developed to educate the community about fluoride varnish, its benefits, availability, and integration into well-child visits. This change in clinical practice and community education could significantly reduce the number of children with dental disease and its severity, thus minimizing a significant community health disparity, as well as saving money and clinical resources in the long term.
Key components of successful research networks
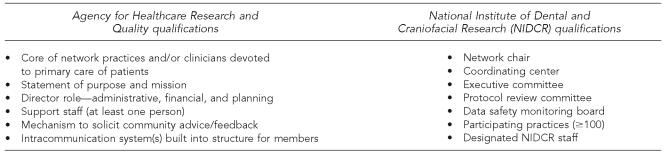
There has been no definitive study of what components are necessary for a successful PBRN.14 In 2004, the Agency for Healthcare Research and Quality (AHRQ) put forth a request for a PBRN (RFA-HS-05-011).15 In the request, AHRQ listed six minimum qualifications that each proposed network needed to meet (Figure 2). In addition, the NIDCR announcement (RFA-DE-05-006) for general dental PBRNs also outlined a basic structure for the network's organizational structure and described the role of each group member in detail.16
Figure 2.
Infrastructure qualifications for Practice-Based Research Networks, as outlined by funding agencies
Research infrastructure at clinics involved in research
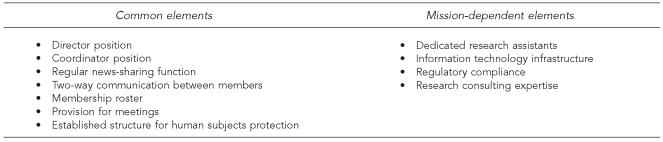
The previous examples of PBRN infrastructure are from granting agencies that required specific elements for funding consideration. Green et al.14 provide an excellent summary of infrastructure requirements for PBRNs based on a systematic review of published research network articles, the PBRN Resource Center 2003 survey, and their colleagues' PBRN experiences. They describe both elements of a basic infrastructure and of a mission-dependent infrastructure (Figure 3) and suggest the elements “should be designed to support its research mission and should be designed after that research mission has been determined.”
Figure 3.
Practice-Based Research Network infrastructure elements, based on Green et al.
a Green LA, White LL, Barry HC, Nease Jr. DE, Hudson BL. Infrastructure requirements for practice-based research networks. Ann Fam Med 2005;3:S5-11.
The approach of Green et al. is unique in that the research mission drives the infrastructure requirements beyond the basic, common elements. This approach, however, has implications for funding, as it requires a more flexible infrastructure—one suited to the research itself. Granting agencies wishing to fund this type of research network would need to be less rigid in their requirements.
Key players involved in facilitating research networks
There are essentially three key groups to take into account when considering initiating a research network: clinics/centers, communities, and institutions. Research networks can be initiated by any of these groups, but to truly be an FQHC research network that utilizes a community-based participatory research approach, the clinics/centers and/or communities should initiate the development of the network.
Under the clinics/centers group, their board of directors, executive directors, executive committees, administrators, clinicians, and staff may be included. Under the communities group, leaders of the community, outreach workers, clinic employees, community organizations or groups, patients, and the general public may be key subgroups. Also, under the institutions group, universities, researchers, funding agencies, and grantors may be included. If the FQHC research network is truly using a bottom-up approach, the institutions group will act mainly in an advisory/expert capacity, with the research topics/questions being proposed by the clinics/centers and the communities.
Gatekeepers for bringing and implementing clinical research projects
The FQHC research network will need to identify any known or implied gatekeepers for entry into the FQHC clinics. Gatekeepers are individuals who have initial contact with research questions or opportunities and decide whether to pursue them. Gatekeepers often serve in a translational role, with understanding of both research and the community. Frequently, initial research ideas are filtered through clinicians or the director of the clinic organization. These individuals then decide whether or not to bring the research idea or proposal to the appropriate board or committee and to the rest of the staff who might be involved in the research. It is important to identify these gatekeepers, as they will set the tone of the clinic's research ideas and implementation. Once identified, a standard approach can be developed for working with them. Additionally, they are often the individuals who can engage their coworkers or employees to participate in the research.
Developing an Oral Health FQHC Research Network
Overcoming challenges.
There are three general challenges to initiating an FQHC research network: (1) buy-in by the FQHC's executive director, clinical directors, clinicians, gatekeepers, and community; (2) manpower, time, resources, and grantor's funding assurance; and (3) commitment and responsibility to the network.
First, for a network to get off the ground, it is essential that initial buy-in from the FQHC's executive director, dental director, and dentists has been established. This is usually accomplished by initiating a relationship-building exercise with executive and dental directors and by engaging the dentists' interest and experience in practical issues or challenges of relevance to their clinical practice. Research institutions, particularly dental schools, need to lay the groundwork for such interest by promoting and encouraging careers within public service among students and reaching out to clinicians working in these settings by providing affiliated faculty appointments, access to library and journal resources, and in-service training. The dental schools themselves need to see the safety-net clinics as something other than a laboratory where their students can practice on low-income patients who have few alternatives.
Once the collaborative relationships among institutions, researchers, and FQHCs and their clinicians have been established, and input and contributions from all members are equally represented and respected, the collaborative will be better able to identify oral health topics that all members feel are important. FQHC clinicians, now with greater investment and prospect in their careers, would make research recommendations to the health center's board of directors, executive committee, and research committee. Community support would also be necessary, and a community advisory board would be needed to help refine the research network mission and goals.
Second, the biggest challenge for FQHC practitioners or any practitioners in a research network is the inherent tension in resource allocation among the primary mission of the organization, service provision, and research. FQHCs are often understaffed and some clinics are not large enough to support extensive research activities. From the perspective of FQHC clinicians, some burn out just trying to address immediate clinical care needs and often they do not have the time, resources, or organizational support to address research. Nevertheless, involvement in research and academia per se may have the potential to improve their career outlooks, job satisfaction, and professional respect, thereby leading to greater dissemination of new clinical knowledge and better outcomes for patients. Additionally, it may attract a new type of clinician to public health service.
To overcome this second challenge, it is imperative that a mechanism for equitable and appropriate funding is established to address manpower and resources such that the research incentives, monetary or otherwise, must be at least comparable to the clinical productivity incentives inherent in most FQHCs. More importantly, if the research network is to be sustainable beyond the life of a particular research program, the funding for infrastructure and continuing growth needs to be consistently available to the organization. As Green et al. noted, although research networks have some basic elements, they do have some flexibility in their infrastructure, depending on the research mission.14 This flexibility often coincides with funding availability.
Thus, it is essential for funders, such as foundations and government, to step up commitment and assurance for consistent, long-term funding and infrastructure support for both development of research and sustainability if Oral Health FQHC Research Networks are to be accepted by FQHCs and the community and have any lasting benefit. This implies providing funds to hire additional staff to assist with the research network activities/projects and to have enough resources to employ these staff long term. In many ways, this problem is no different than the problem of long-term maintenance of research laboratories at the university. But in the FQHCs and community, the stakes are higher.
Finally, the third considerable challenge is how FQHCs maintain their commitment and responsibility to the research network. The FQHC research network can establish a steering committee and a well-defined organizational structure. It is necessary to negotiate clear guidelines for responsibility and involvement for each of the key groups within the infrastructure. Furthermore, it is imperative to emphasize that participation in specific research projects is voluntary and may be based on the clinic's or clinicians' interest in the research topic.
Basic steps for developing a research network.
Now that some basic elements of a research network have been described, it is useful to think about how one would go about developing an FQHC research network. There are some basic steps that FQHCs can take to develop a network (Figure 4).
Figure 4.
Steps for developing an FQHC research network
FQHC = Federally Qualified Health Center
CHC = community health center
The first step in identifying clinic research interest is often to identify clinicians, gatekeepers, or clinics/ CHCs with some interest in research that would have direct benefit to their patient population. In most existing PBRNs, this is most often a top-down approach. However, in the case of an FQHC research network, it may be more useful to think of developing the research network as an exercise in building capacity in and among the various FQHCs, capacity for research, and capacity to engage in equitable research partnerships with university researchers.
In this case, then, it will be most effective if an FQHC that already has some interest, capacity, and experience for such research partnerships recruits other centers through director-to-director and clinician-to-clinician contact. Once interest is established, it may be useful to hold a conference or workshop to further engage clinicians and clinics, to discuss the applicability of research networks for improving the health of the FQHC's communities, and to begin to share structure and systems that have previously worked to support centers as they engage in research partnerships. Research institutions and researchers may be helpful at this point for providing research methodology overview and instruction.
After interest has been generated by the clinicians/gatekeepers/clinics/board of directors, a steering committee should be formed to guide the development of the FQHC research network. The members will consist of an equitable representation of FQHC and researchers. At this point, the steering committee will define the research network's mission (purposes/goals), develop its basic infrastructure (see Green et al. for infrastructure elements14), and identify additional capacity building that needs to occur in the FQHCs. The committee will also assess strengths and weaknesses in terms of community capacities and disease burden, and the similarities and uniqueness among the different FQHCs. The committee will also be charged with prioritizing the agenda for exploration, research, and program development, including strategizing for developing and designing studies aimed at answering specific questions of interest to the FQHCs. Researchers will be helpful in framing the research questions, appropriate methodology, and data analysis. And finally, the steering committee will identify funders/grantors and other potential university/agency collaborators.
In conjunction with the steering committee and its agenda, the FQHCs may choose to develop their own RRC, either for each CHC or for the entire network. HIPAA regulations provide a mechanism for a privacy board, which may serve this function. Institutional partners/researchers may be able to assist with the development of this committee. As mentioned, the RRC may be an IRB-like group that comprises clinicians, nonclinicians, and community members. It will review and approve all research studies on behalf of the FQHC and community, but does not replace the academic IRB review.
Preparing FQHCs for research and a research network.
Before FQHCs feel comfortable engaging in oral health research, let alone driving a practice-based research mission, it may be necessary to introduce FQHCs to the general research process as well as the practice-based research approach. Universities and/or granting agencies could promote dialog and interest in research and evaluation useful to FQHCs. This could be accomplished by partnering with the FQHCs to hold workshops on general research methodology, specific methodology such as the community-based participatory research approach, research ethics, basic evaluation, and needs assessment methodologies.
Institutions and granting agencies can also play an advisory role to the FQHCs as they develop their research networks. They can assist the FQHCs with more research-oriented needs assessments of the communities for potential research topics. They can also help the FQHCs seek collaborations with other colleagues/institutions with similar interests or needs to conduct research addressing community concerns. This may be especially useful for smaller FQHCs with limited resources. In conjunction with this, they can help identify funds for pilot studies to learn more about the characteristics of the FQHC itself.
CONCLUSIONS
Disparities in oral health remain a tremendous challenge to address. Populations of racial and lower-income levels in communities suffer a significantly higher rate of oral diseases than their more affluent peers. Furthermore, they also suffer from a higher rate of untreated diseases. These populations more often receive general and oral health care from FQHCs (and FQHC Look-Alikes) than from private practices. As such, the PBRN model and research agenda currently in place in dentistry is likely to have minimal impact on the population with the greatest suffering and greatest need. Moreover, it will do little to strengthen the infrastructure needed to recruit and maintain an adequate workforce, which is essential to reducing oral health disparities.
To date, there is no true FQHC research network that is dedicated to addressing oral health disparities. For these reasons, it is imperative to think about an alternative approach to PBRNs by creating similar networks involving FQHCs to effectively address this health disparity. There is a need to establish Oral Health FQHC Research Networks that will lead, identify, design, and conduct studies that are of interest to these communities. This research network would utilize the principles of community-based participatory research. Through these principles, the network would focus the research topics on the needs and strengths of the community, invest in the community, and build capacity in the community to recognize its own health strengths and challenges, study them, and disseminate and translate the findings into useful programs for improving its oral health.
Finally, for an Oral Health FQHC Research Network to become established, it is necessary that funders, including foundations and government agencies, appreciate the relationship between a strong infrastructure in the safety-net sector and the reduction of disparities, and commit support and resources to develop and sustain such clinics and their research networks. Funding should be prioritized to promote network development through conferences and planning grants and by providing supplementary funds through existing granting mechanisms. This may require cross-agency agreements within government to facilitate funding; for example, Health Resources and Services Administration grants from the Bureau of Primary Health Care.
Additionally, granting agencies and/or FQHCs should partner with foundations to support basic, sustainable infrastructure. Groups comprising racially diverse health professionals, such as the Hispanic Dental Association,17 as well as FQHC health providers should advocate and lobby for funding to support Oral Health FQHC Research Network development. Such a research network will substantially enhance our understanding of oral health disparities and will help elucidate more appropriate approaches to improving oral health.
Footnotes
This research was supported by the National Institute of Dental and Craniofacial Research Grant # U54DE14254.
REFERENCES
- 1.Forrest CB, Whelan EM. Primary care safety-net delivery sites in the United States: a comparison of community health centers, hospital outpatient departments, and physician offices. JAMA. 2000;284:2077–83. doi: 10.1001/jama.284.16.2077. [DOI] [PubMed] [Google Scholar]
- 2.Politzer RM, Yoon J, Shi L, Hughes RG, Regan J, Gaston MH. Inequality in America: the contribution of health centers in reducing and eliminating disparities in access to care. Med Care Res Rev. 2001;58:234–48. doi: 10.1177/107755870105800205. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health and Human Services (US) Oral health in America: a report of the Surgeon General. 2000. [cited 2005 Jun 7]. Available from: URL: http://www.surgeongeneral.gov/library/oralhealth.
- 4.Rosenblatt RA, Andrilla CH, Curtin T, Hart LG. Shortages of medical personnel at community health centers: implications for planned expansion. JAMA. 2006;295:1042–9. doi: 10.1001/jama.295.9.1042. [DOI] [PubMed] [Google Scholar]
- 5.Nutting PA, Beasley JW, Werner JJ. Practice-based research networks answer primary care questions. JAMA. 1999;281:686–8. doi: 10.1001/jama.281.8.686. [DOI] [PubMed] [Google Scholar]
- 6.Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med. 2005;3(Suppl 1):S12–20. doi: 10.1370/afm.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Byck GR, Cooksey RA, Russinof H. Safety-net dental clinics. J Am Dent Assoc. 2005;136:1013–21. doi: 10.14219/jada.archive.2005.0296. [DOI] [PubMed] [Google Scholar]
- 8.Milgrom P, Garcia RI, Ismail A, Katz RV, Weintraub JA. Improving America's access to care: the National Institute of Dental and Craniofacial Research addresses oral health disparities. J Am Dent Assoc. 2004;135:1389–96. doi: 10.14219/jada.archive.2004.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green LA, Dovey SM. Practice based primary care research networks: they work and are ready for full development and support. BMJ. 2001;322:567–8. doi: 10.1136/bmj.322.7286.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Association of Community Health Centers, Inc. Based on Bureau of Primary Health Care, HRSA, DHHS. 2005 Uniform Data System. 2006. [cited 2007 May 10]. Available from: URL: http://www.nachc.com/research/Files/USfactsheet.pdf.
- 11.Patrick DL, Lee RSY, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;(6 Suppl 1):S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.YVFWC Report to Our Communities. [cited 2007 Feb 20]. Available from: URL: http://www.yvfwc.com/images_YV/RTC.06.pdf.
- 13.University of Washington School of Public Health and Community Medicine. Community-based research principles. [cited 2006 Jul 17]. Available from: URL: http://sphcm.washington.edu/research/community.asp.
- 14.Green LA, White LL, Barry HC, Nease DE, Jr., Hudson BL. Infrastructure requirements for practice-based research networks. Ann Fam Med. 2005;(3 Suppl 1):S5–11. doi: 10.1370/afm.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Department of Health and Human Services (US); Agency for Healthcare Research and Quality. RFA-HS-05-011, Small research grants for primary care Practice-Based Research Networks (PBRNs) [cited 2006 Jan 10]. Available from: URL: http://grants.nih.gov/grants/guide/rfa-files/RFA-HS-05-011.html.
- 16.Department of Health and Human Services (US); National Institute of Health/National Institute of Dental and Craniofacial Research. RFA-DE-05-006, General Dental Practice-Based Research Network. [cited 2005 Dec 21]. Available from: URL: http://grants.nih.gov/grants/guide/rfa-files/RFA-DE-05-006.html.
- 17.Ramos-Gomez F, Cruz GD, Watson MR, Canto MT, Boneta AE. Latino oral health: a research agenda toward eliminating oral health disparities. J Am Dent Assoc. 2005;136:1231–40. doi: 10.14219/jada.archive.2005.0339. [DOI] [PubMed] [Google Scholar]