SYNOPSIS
Objective.
This article estimates the financial impact of a ban on amalgam restorations for selected population groups: the entire population, children, and children and women of childbearing age.
Methods.
Using claim and enrollment data from Delta Dental of Michigan, Ohio, and Indiana and the American Dental Association Survey of Dental Services Rendered, we estimated the per capita use and annual rate of change in amalgam restorations for each age, gender, and socioeconomic subgroup. We used population projections to obtain national estimates of amalgam use, and the dental component of the Consumer Price Index to estimate the annual rate of change in fees. We then calculated the number of dental amalgams affected by the regulation, and the fees for each of the years 2005 to 2020.
Results.
If amalgam restorations are banned for the entire population, the average price of restorations before 2005 and after the ban would increase $52 from $278 to $330, and total expenditures for restorations would increase from $46.2 billion to $49.7 billion. As the price of restorations increases, there would be 15,444,021 fewer restorations inserted per year. The estimated first-year impact of banning dental amalgams in the entire population is an increase in expenditures of $8.2 billion.
Conclusions.
An amalgam ban would have a substantial short- and long-term impact on increasing expenditures for dental care, decreasing utilization, and increasing untreated disease. Based on the available evidence, we believe that state legislatures should seriously consider these effects when contemplating possible restrictions on the use of amalgam restorations.
Caries is the most prevalent oral disease, and the primary treatment for caries is the removal of diseased tissue and replacement with a restorative material. Amalgam—used for more than 150 years and the predominant and clinically preferred material for restoring most posterior teeth (i.e., molars and premolars)—is composed of a mixture of silver, other metals, and mercury (50% by weight).1
There is growing concern about urinary mercury levels in the population, because levels above 50 μg/L for extended periods of time in adults are associated with neurological, renal, and immunological impairments.2 It is known that amalgam restorations release a mercury vapor during mastication, and that children and adults with multiple amalgam restorations have slightly elevated urine mercury levels.3 However, numerous observational studies in adults and two recent randomized control trials in children reported no adverse health effects from the mercury exposure related to amalgams.4–7
Another concern is possible environmental contamination from the residual mercury (amalgam scrap and waste) used in the preparation of amalgams.8 Several studies found no, or minimal, free mercury going into the environment from dentists' offices.9
Although published studies in national refereed journals have not indicated an association between mercury in dental amalgams and the adverse health of dental patients, dental providers,10 or the general population, several countries, including Germany, Sweden, and Denmark, have limited the use of amalgam restorations to adults and nonpregnant women.11 In the United States, bills have been introduced in federal and state legislatures to restrict the use of amalgam restorations.12 To date, these bills have not passed, but efforts to regulate the use of amalgams are likely to continue.
For state legislatures to make informed decisions, it is important for them to understand the impact of an amalgam restoration ban on expenditures and access to dental care. A ban on amalgams will increase the use of two other classes of restorative materials. Tooth-colored resin composites are preferred for anterior teeth, where esthetics are essential. However, they can and are used to restore posterior teeth. Resin composite restorations are more expensive and do not last as long as amalgam restorations.13 Teeth that are more severely impaired by caries or trauma are often restored with cast restorations, such as gold crowns and onlays, which are much more expensive than amalgam or composite restorations.
The purpose of this article is to estimate the financial impact that would result if amalgam restorations are banned in select population subgroups, including children; children and women of childbearing age; or the entire population.
METHODS
Conceptual framework
A partial or total ban on amalgams is equivalent to an increase in the price and a decrease in the number of restorations. The decrease is equivalent to the expected increase in the number of untreated teeth with caries and/or extractions. To determine the decrease in restorations, an estimate of their price elasticity (percent decrease in the number of restorations over the percent increase in their price) is required, but there are no available estimates in the literature, and price elasticity cannot be derived from the available data. There is a national estimate of the price elasticity of all dental services.14
We used this estimate, 0.5, as a reasonable value for the price elasticity of dental restorations because: (1) the estimated elasticity is based on national data and includes people with and without dental insurance; (2) there are no good substitutes for restorations; and (3) expenditures for restorations constitute a large share of total dental expenditures. We performed sensitivity analysis using different price elasticity values (plus/minus 40%) and found that elasticity affected estimates of the number of untreated teeth but not costs. Using this price elasticity estimate, we determined the percent decrease in the quantity of dental restorations, which is the product of the percent increase in price times the elasticity.
The annual economic impact (Ci) of imposing a ban on amalgam restorations is defined as:
| Ci = Q1 × (P1 − P0) + (Q0 − Q1) × (P1 − P0) / 2 |
where Q0 and Q1 stand for the total number of dental restorations before and after the ban, and P0 and P1 stand for the weighted mean price of a dental restoration before and after the ban, respectively. The first right-hand side term measures the added costs of replacing amalgams with nonamalgam restorations, while the second term captures the loss of consumer surplus.
As a first approximation, the annual economic impact of a ban will be equal to the number of restorations used (Q0) times their price increase (P1 − P0). The economic impact will recur annually for as long as amalgam placement would have continued in the absence of regulation. For practical purposes, we assumed that the regulation continued for the period 2005–2020.
Data sources
We used two data sources in the analysis. First, we calculated the current rate of amalgam use based on claims and enrollment data from Delta Dental of Michigan, Ohio, and Indiana. This insurer has a large market share, the claims cover a long time period (1992–2004), and the per capita income of Michigan is close to the national mean.
This approach assumes that those with dental insurance represent those without dental insurance. While only about 50% of the U.S. population has some form of dental insurance, more than 60% of the care consumed is provided to people with insurance.15 Insured individuals visit dentists more often and consume more care at each visit. Further, people who do not have dental insurance, all else equal, consume less dental care per person. Because they are paying full price out of pocket, they are likely to receive the least expensive restorative treatment, which is an amalgam or an extraction. Therefore, while those without insurance go to the dentist less often, when they do go and need a restoration, they are more likely to receive an amalgam than a composite or crown.
Because of possible limitations in claim-based estimates of national amalgam utilization rates, we used a second dataset to assess the validity of the first. In the American Dental Association (ADA) surveys (Survey of Dental Services Rendered), a random group of dentists determined the mix and volume of services provided to all patients, insured and noninsured.16 We determined the concordance between the estimates based on these two independent data sources.
We used the same ADA Survey of Dental Services Rendered to estimate the direct cost of amalgam and nonamalgam restorations.16 The fee differences do not capture the total difference in expenditures, because composites have a higher failure and replacement rate than amalgams.4
ANALYSIS
Using claims and enrollment data from 1992 through 2004, we estimated the annual rate of change in amalgam restorations. We used the number of people insured for all 12 months, in each calendar year from 1992 through 2004, as the denominator and the number of amalgam restorations placed in these individuals each year as the numerator. This was done for each age, gender, socioeconomic, and geographic subgroup. We estimated the per capita use of dental amalgams and then used population projections to get national estimates of annual amalgam use as of January 1, 2005, and beyond.
Similarly, we used the dental component of the Consumer Price Index for the same period (1992–2004) to estimate the annual rate of change in dental fees. These two estimates enabled us to calculate the number of dental amalgams affected by the regulation, and the fees for each of the years 2005 through 2020. We applied the following exponential functional form on the historical data:
| Yt = AeBt or in logarithmic terms: InYt = InA + Bt |
where Yt can represent the number of amalgam restorations used in year t or the dental component of the consumer price index at year t. A is a constant, and B represents the annual rate of change in the number of amalgam restorations used or the annual rate of change in the dental component of the consumer price index.
Based on the estimated rates of annual change in dental fees and dental amalgam use, we calculated the annual direct impact of an amalgam ban for each of the years 2005 through 2020. The present value of these annual estimates for the period 2005–2020 constitutes the direct cost of banning amalgam restorations. The formula to calculate the present value is:
| Present value = ∑t Ct / (1+r)t |
where Mt is the sum of the terms, Ct is the annual direct cost for each of the years 2005 through 2020, and r is the discount rate. We used two different discount rates to arrive at the present value of these costs.
A more detailed report on the study methods and results is available from the ADA or the California Dental Association.17
RESULTS
Current use of amalgams
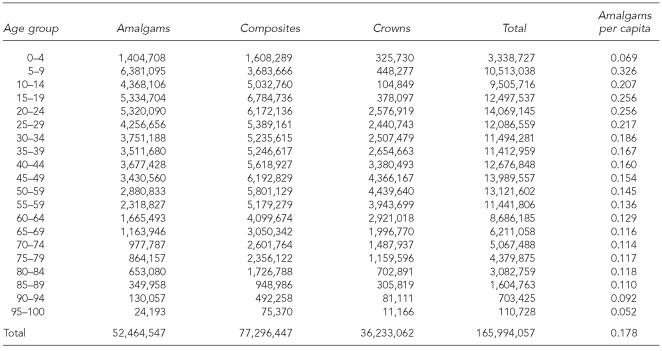
Based on dental insurance claim data, Table 1 presents the estimated total number of amalgams, composites, crowns, and per capita amalgams by age group inserted in 2005. Of the total 166 million restorations, 52.5 million (31.6%) were amalgams, 77.3 million (46.6%) were composites, and 36.2 million (21.8%) were crowns. Per capita, amalgam restorations were highest in children and young adults and lower in older age groups.
Table 1.
Number of restorations by type of restoration and per capita number of amalgams placed in the U.S. population, 2005
Regression analysis indicated that the mean percent of decline in the number of amalgams inserted per year for the past 12 years was 3.7% (data not shown). This rate of decline did not vary by age group or year. As the use of amalgams declined, the substitute restorative materials used were 81% composites and 19% crowns. The mean rate of increase in restoration fees over this same time period was 4.5% per year (data not shown).
Impact of ban
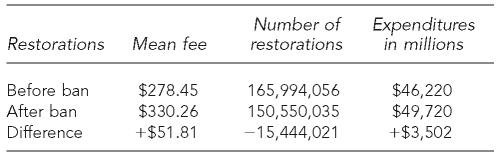
Table 2 shows that the mean price of restorations before 2005 and after a ban on amalgam restorations would increase $52 (18.6%) from $278 to $330, and total expenditures for restorations would increase from $46.2 billion to $49.7 billion. As the price of restorations increases because of the ban, there would be 15,444,021 fewer restorations inserted per year, a 9.3% decline. The direct first-year economic impact of banning dental amalgams in the entire population is estimated to be $8,200,549,077 (change in price per restoration times the number of restorations and the consumer surplus loss of $400,100,250 [value of services to consumers above price paid]).
Table 2.
Estimated annual mean fees, number, and expenditures for restorations before/after a ban on amalgams for the entire population
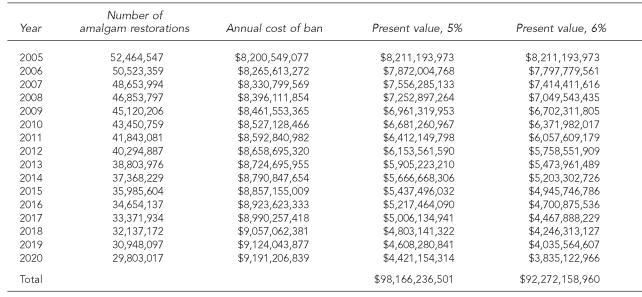
Table 3 gives the estimated financial impact of banning amalgams for the entire population by year from 2005 through 2020. Because the total number of amalgam restorations is expected to decline significantly during this period even with no regulation, and dental fees are expected to rise, the first-year economic impact will stay approximately the same for each of the next 15 years. Using 5% and 6% discount rates, the estimated economic impact of a total ban on amalgam restorations is $98.2 billion and $92.3 billion, respectively.
Table 3.
Projected number of amalgam restorations, annual costs of banning amalgams for the entire population, and their present value, 2005 through 2020
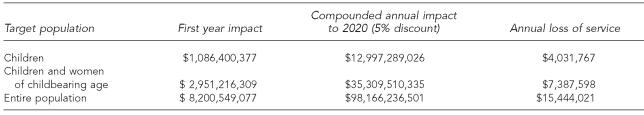
Using the same methodology, Table 4 presents the direct costs of the three regulatory options for banning the use of amalgam restorations. The estimated direct costs of a ban on the use of amalgam restorations varies greatly by the option selected. A ban on just children aged 0 to 19 years will increase dental expenditures about $1.1 billion per year and $13 billion from 2005 through 2020 and would result in more than four million fewer restorations. At the other extreme, banning amalgams in the entire population will increase dental expenditures about $8.2 billion in the first year and $98.1 billion from 2015 through 2020 and would result in 15.4 million fewer needed restorations.
Table 4.
The first year, compounded annual (2005 through 2020), and annual value of service loss impact of banning amalgams by target population
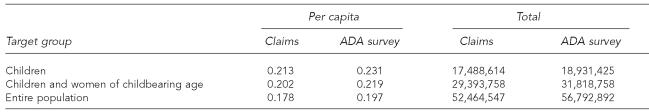
Table 5 compares the estimates of the number of per capita and total amalgam restorations placed in children, children and women of childbearing age, and the entire population, based on dental insurance claims and the 2005 ADA Survey of Dental Services Rendered. For both per capita and total amalgam restorations, the differences between data sources were not significant.
Table 5.
Comparison of per capita and total amalgam restorations inserted in 2005, based on dental insurance claims and the ADA Survey of Dental Services Rendered
ADA = American Dental Association
DISCUSSION
The primary limitation of this study is the lack of a national database on restorative services provided by dentists annually by type of restoration, age, gender, and family income. However, we believe that the Delta Dental insurance claims from Michigan provide a reasonable approximation, and this conclusion is supported by the high concordance of estimates based on claim and ADA survey data.
Another limitation is the lack of a price elasticity estimate for different dental restorations. This limitation impacts primarily the estimate of the number of untreated teeth. The sensitivity analysis showed that different price elasticities had little effect on the estimates of expenses, suggesting that the price elasticity figure used is adequate.
This research indicates that a ban on amalgams will have a substantial short- and long-term financial impact on expenditures for dental care. Even if limited to children, we estimate that expenditures will increase $1.1 billion the first year of the ban and $13 billion over a 15-year period. Considering that in 2005 national expenditures for dental care were about $85 billion, this is a 1.3% increase.18 Further, with higher expenditures for dental care, utilization will decrease, resulting in more untreated disease.
There are two reasons for the increase in aggregate expenditures. First, the materials that substitute for amalgams—composite resins and cast restorations—are more expensive per restoration (e.g., mean fees for composite restorations are 46% higher than amalgam restorations). Second, composites do not last as long as amalgams and require more frequent replacement. Also, studies indicate that replacement restorations are often more complex and expensive.19 In addition to direct expenditures, there will be a significant increase in indirect expenditures associated with patient time and travel costs for more dental visits.
Predictably, lower-income families will have the most difficulty adjusting to the increased cost of dental care and will experience reductions in access to dental care. This is unfortunate because lower-income families have the higher prevalence of dental disease and lower utilization rates. Thus, the ban on amalgams will widen access and oral health disparities.20
Another likely impact of a ban on amalgam restorations is known as the “announcement effect.” That is, a ban on amalgams is certain to affect the treatment decisions of some patients and dentists who are not subject to the ban. Thus, more patients are likely to refuse amalgam restorations, and some will even have amalgam restorations replaced. Likewise, more dentists are likely to encourage patients to have resin composite and crown restorations on their molar teeth instead of amalgams. The magnitude of the announcement impact is unknown but could be substantial.
A ban on amalgams will increase the incomes of general dentists, as they generate more net revenues per unit time, providing more expensive and profitable restorations. Also, if there is a large announcement effect, the demand for dental care may increase for some period of time, and this may lead to greater inflation in dental fees.
Finally, it is important to stress that even without a ban on amalgams, the continuing discussion on the need for a ban is likely to accelerate the current 3.7% annual decline in the use of amalgam restorations.
CONCLUSION
State legislators need to balance the evidence of any adverse effects of amalgams on patients and the environment and the impact of the ban on access to dental care and oral health. Based on several well-done studies, there is no evidence that the use of amalgam restorations leads to any adverse neurological impairments for children or that dentists and dental assistants who handle amalgams every day and have done so for more than 150 years have any adverse health outcomes as a result of their continuous exposure to this material.10 Likewise, the disposal of residual mercury used in the preparation of amalgams is not a significant source of environmental mercury.
In contrast, a ban on amalgams will lead to a significant increase in dental care expenditures and a reduction in utilization that will mainly impact children and adults from lower-income families. The more people included in the ban, the greater the adverse impact on access to dental care and oral health. Indeed, if amalgams are banned for the entire population, the first-year direct costs will be more than $8 billion, which is almost 10% of the current national dental expenditures.
Based on the available evidence, we believe that state legislatures should seriously consider these effects when contemplating possible restrictions on the use of amalgam restorations. There is no evidence that this restorative material is having an adverse impact on health, and there is substantial evidence that a ban will increase access and oral health disparities. Finally, the use of amalgam restorations is slowly declining, so that in 25 years relatively few carious teeth will be restored with this material, even in the absence of a ban.
Acknowledgments
The authors give special thanks to Delta Dental of Michigan, Ohio, and Indiana for providing valuable claims data, without which this project would not have been possible. The authors would also like to thank a number of individuals who reviewed earlier drafts of this article and provided valuable comments.
Footnotes
This research project was funded by the American Dental Association (ADA) and the California Dental Association (CDA). Any opinions and conclusions contained in this report are those of the author(s) and not necessarily those of, nor endorsed by, the ADA or the CDA.
REFERENCES
- 1.Mackert JR, Jr., Berglund A. Mercury exposure from dental amalgam fillings: absorbed dose and the potential for adverse health effects. Crit Rev Oral Biol Med. 1997;8:410–36. doi: 10.1177/10454411970080040401. [DOI] [PubMed] [Google Scholar]
- 2.Risher JF. Concise international chemical assessment document 50: elemental mercury and inorganic mercury compounds: human health aspects. Geneva: World Health Organization; 2003. [Google Scholar]
- 3.Dye BA, Schober SE, Dillon CF, Jones RL, Fryar C, McDowell M, et al. Urinary mercury concentrations associated with dental restorations in adult women aged 16-49 years: United States, 1999–2000. Occup Environ Med. 2005;62:368–75. doi: 10.1136/oem.2004.016832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Public Health Service (US) Dental amalgam: a scientific review and recommended public health service strategy for research, education and regulation. 1993. Jan, [cited 2005 May 10]. Available from: URL: http://www.health.gov/environment/amalgam1/ct.htm.
- 5.Food and Drug Administration Center for Devices and Radiological Health (US) CDRH consumer information. 2002 consumer update: dental amalgams. [cited 2006 Apr 19]. Available from: URL: http://www.fda.gov/cdrh/consumer/amalgams.html.
- 6.Bellinger DC, Trachtenberg F, Barregard L, Tavares M, Cernichiari E, Daniel D, et al. Neuropsychological and renal effects of dental amalgam in children. JAMA. 2006;295:1775–83. doi: 10.1001/jama.295.15.1775. [DOI] [PubMed] [Google Scholar]
- 7.DeRouen TA, Martin MD, Leroux BG, Townes BD, Woods JS, Leitao J, et al. Neurobehavioral effects of dental amalgam in children. JAMA. 2006;295:1784–92. doi: 10.1001/jama.295.15.1784. [DOI] [PubMed] [Google Scholar]
- 8.McGroddy S, Chapman P. Is mercury from dental amalgam an environmental problem? Env Toxicol Chem. 1997;16:2213–4. [Google Scholar]
- 9.McManus KR, Fan PL. Purchasing, installing and operating dental amalgam separators: practical issues. J Am Dent Assoc. 2003;134:1054–65. doi: 10.14219/jada.archive.2003.0319. [DOI] [PubMed] [Google Scholar]
- 10.Ritchie KA, Burke FJ, Gilmour WH, MacDonald EB, Dale IM, Hamilton RM, et al. Mercury vapour levels in dental practices and body mercury levels of dentists and controls. Br Dent J. 2004;197:625–32. doi: 10.1038/sj.bdj.4811831. [DOI] [PubMed] [Google Scholar]
- 11.Department of Health and Human Services (US) Bethesda (MD): Life Sciences Research Office; 2004. Review and analysis of the literature on the potential adverse health effects of dental amalgam; pp. 1–59. [Google Scholar]
- 12.Diogo SJ. Amalgam on trial. [cited 2007 May 10];AGD Impact. 2003 31:1. Also available from: URL: http://www.agd.org/library/2003/jan/200301_diogo.asp. [Google Scholar]
- 13.Bogacki RE, Hunt RJ, del Aguila M, Smith WR. Survival analysis of posterior restorations using an insurance claims database. Oper Dent. 2002;27:488–92. [PubMed] [Google Scholar]
- 14.Beazoglou T, Brown LJ, Heffley D. Dental care utilization over time. Soc Sci Med. 1993;37:1461–72. doi: 10.1016/0277-9536(93)90180-c. [DOI] [PubMed] [Google Scholar]
- 15.Manski RJ, Macek MD, Moeller JF. Private dental coverage: who has it and how does it influence dental visits and expenditures? J Am Dent Assoc. 2002;133:1551–9. doi: 10.14219/jada.archive.2002.0087. [DOI] [PubMed] [Google Scholar]
- 16.American Dental Association. Survey of dental fees and dental services rendered, 2005. Chicago: American Dental Association; 2005. [Google Scholar]
- 17.Beazoglou T, Bailit HL, Eklund S, Heffley D, Meiers J, Brown LJ. Economic impact of various dental amalgam regulatory options. Chicago: American Dental Association; 2006. [Google Scholar]
- 18.Heffler S, Smith S, Keehan S, Clemens MK, Zezza M, Truffer C. Health spending projections through 2013. Health Aff (Millwood) 2004;(Suppl) doi: 10.1377/hlthaff.w4.79. Web exclusives:W4-79-93. [DOI] [PubMed] [Google Scholar]
- 19.Mjor IA, Reep RL, Kubilis PS, Mondragon BE. The change in size of replaced amalgam restorations: a methodology study. Oper Dent. 1998;23:272–7. [PubMed] [Google Scholar]
- 20.Vargas CM, Crall JJ, Schneider DA. Sociodemographic distribution of pediatric dental caries: NHANES III, 1988-1994. J Am Dent Assoc. 1998;129:1229–38. doi: 10.14219/jada.archive.1998.0420. [DOI] [PubMed] [Google Scholar]