Abstract
Background
The most common side effect of spinal opioid administration is pruritus, which has been treated with a variety of agents with variable success. Currently, there are few animal models developed to study this side effect. The aim of this study was to establish a nonhuman primate model to pharmacologically characterize the effects of intrathecal administration of morphine.
Methods
Eight adult rhesus monkeys were used. Scratching responses were videotaped and counted by observers who were blinded to experimental conditions. Antinociception was measured by a warm-water (50°C) tail-withdrawal assay. The dose-response of intrathecal morphine (1-320 μg) for both scratching and antinociception in all subjects was established. An opioid antagonist, nalmefene, was administered either intravenously or subcutaneously to assess its efficacy against intrathecal morphine.
Results
Intrathecal morphine (1-32 μg) increased scratching in a dose-dependent manner. Higher doses of intrathecal morphine (10-100 μg) produced thermal antinociception in a dose-dependent manner. On the other hand, nalmefene (10-32 μg/kg intravenously) attenuated maximum scratching responses among subjects. Pretreatment with nalmefene (32μg/kg subcutaneously) produced approximately 10-fold rightward shifts of intrathecal morphine dose-response curves for both behavioral effects.
Conclusions
These data indicate that intrathecal morphine-induced scratching and antinociception are mediated by opioid receptors. The magnitude of nalmefene antagonism of intrathecal morphine is consistent with μ opioid receptor mediation. This experimental itch model is useful for evaluating different agents that may suppress scratching without interfering with antinociception. It may also facilitate the clarification of mechanisms underlying these phenomena.
Keywords: Opioid actions, pruritus, spinal administration
SINCE the first study1 to report that intrathecal morphine produced prolonged pain relief in patients, the intrathecal technique has been widely used for obstetric analgesia and postoperative pain.2-4 It is clear that the application of spinal opioids has become one of the most significant breakthroughs in pain management during the last two decades. However, the most common side effect of spinal opioid administration is pruritus, which sometimes is severe and may lessen the value of spinal opioids for pain relief.4,5 A variety of therapeutic agents have been proposed as antipruritics, but they are effective with variable success.4,5
The development of experimental itch models is valuable for identifying potential antipruritic agents and investigating underlying mechanisms. In rodents, intracisternal administration of morphine has been shown to evoke scratching responses.6,7 However, this centrally administered morphine-induced scratching only lasted for 1 h.6 Currently, there is no report indicating that intrathecal morphine induces scratching behaviors in rodents. Although high doses of intrathecal morphine produced allodynia-like behaviors in rats, these effects were not reversed by opioid antagonists.8 In nonhuman primates, intrathecal morphine has been shown to produce prolonged antinociception.9,10 Nevertheless, characterization of intrathecal morphine-induced scratching responses in terms of dose-response and duration has not been systematically evaluated.
Therefore, the aim of this study was to establish the pharmacologic basis of intrathecal morphine effects in nonhuman primates for scratching responses and antinociception. The time course and dose dependency of both behavioral end points were evaluated in the same subjects over an extensive dose range. Furthermore, a long-acting opioid antagonist, nalmefene,11,12 was used to assess its capacity in attenuating scratching responses and to determine if opioid receptors were involved differently in scratching and antinociception.
Materials and Methods
Subjects
Four adult male and four adult female rhesus monkeys (Macaca mulatta), with body weights ranging from 4.6 to 12.8 kg, were used. They were housed individually with free access to water and were fed approximately 25-30 biscuits (PMI Nutrition International Inc., Brent-wood, MO) and fresh fruit daily. Four monkeys previously trained in the warm-water tail-withdrawal procedure were used for the antinociceptive assay. As noted, one monkey (MK1) had a history of short-term (months) opioid exposure and three monkeys (MK3-MK5) had long-term (years) opioid exposure in which they did not receive systemic opioids more than twice per week. The remaining monkeys did not have prior involvement in opioid studies. No monkey had exposure to opioids for 1 month before the present study. Animals used in this study were maintained in accordance with the University Committee on Use and Care of Animals at the University of Michigan and the Guide for the Care and Use of Laboratory Animals.13
Procedure
Scratching Responses
Scratching responses, inferred as an itch sensation, were recorded on videotapes in home cages for 15 min/h. Recording was conducted for 6 h after intrathecal morphine administration. A scratch was defined as one short-duration (≤ 1 s) episode of scraping contact of the forepaw or hind paw on the skin surface of other body parts. Scratches usually occurred repetitively at the same location. Scratching responses were counted by independent observers who were blinded to experimental conditions. On occasion, different raters separately scored a single tape, and ratings indicated high interrater reliability (coefficient of correlation, r > 0.95).
Thermal Antinociception
The warm-water (50°C) tail-withdrawal assay14 was used to evaluate thermal antinociceptive effects of intrathecal morphine. This procedure has been widely used in nonhuman primates to investigate a variety of analgesics and generally in good agreement with in vitro findings.15-18 Briefly, monkeys were seated in restraint chairs, and the lower part of the shaved tail (approximately 15 cm) was immersed into warm water maintained at temperatures of 40, 50, or 55°C. They were tested one to two times at three temperatures in a random order. Tail-withdrawal latencies were recorded with a computerized timer by an experimenter who was blinded to experimental conditions. A maximum cutoff latency (20 s) was used to prevent tissue damage. Each experimental session began with control determinations at each temperature. Subsequent tail-withdrawal latencies were determined every hour up to 6 h after intrathecal morphine administration.
Intrathecal Injection
Monkeys were anesthetized with ketamine HCl (10 mg/kg administered intramuscularly) and positioned laterally. The lower back of the trunk was shaved and sterilely prepared with betadine. A spinal needle (22-gauge/3.8 cm; Becton Dickinson, Franklin Lakes, NJ) was inserted into the subarachnoid interspace between L4/L5 or L5/L6 lumbar vertebra. Needle position was confirmed by the free flow of clear cerebrospinal fluid. A 1-ml saline solution of morphine (1-320 μg) was slowly infused through the spinal needle within 30 s, and then monkeys were returned to their home cages.
Experimental Design
Experimental sessions were conducted no more than three to four times per month in each subject. The experimental interval was 8-10 days to prevent possible tolerance development. The first group of monkeys (MK5-MK8) had not been habituated and trained in the tail-withdrawal procedure. They were used only to study intrathecal morphine-induced scratching responses and to evaluate the efficacy of intravenous nalmefene in attenuating scratching responses. The second group of monkeys (MK1-MK4) was used to study both scratching responses and antinociceptive effects. They were further used to study systemic (subcutaneous) nalmefene antagonism of intrathecal morphine for both behavioral end points. The time course and dose-response curves were replicated two to three times in each subject.
Dose-Response of Intrathecal Morphine
Experiments were conducted to obtain behavioral profiles of scratching responses and thermal antinociception of intrathecal morphine by studying an extensive dose range (1-320 μg). One hour after intrathecal injection, the antinociceptive responses were measured during the first 15 min of each hour. Subsequently, monkeys were returned to their home cages, and scratching responses were recorded for 15 min after the antinociceptive measurement. Monkeys not involved in the antinociceptive procedure were recorded at the same time point for their scratching responses. The effects of intrathecal morphine were studied for 6 h (i.e., six test sessions) by giving different doses randomly in a single dosing procedure.
Antagonism of Intrathecal Morphine
After establishing the dose-response curves of intrathecal morphine in each subject, the opioid antagonist, nalmefene, was chosen to verify the opioid receptor mediation of intrathecal morphine. The dose of intrathecal morphine producing maximum scratching responses in each subject was chosen for the intravenous nalmefene study. The maximum dose of intrathecal morphine for monkey no. MK5 was 320 μg and for other monkeys (MK6-MK8) was 32 μg. After recording in the first test session, subjects were seated in chairs, and one dose of nalmefene was administered intravenously through a saphenous vein from either side of the lower shanks 15 min before the second test session. Monkeys were subsequently returned to their home cages, and recording was continued every 15 min/h for the remaining test sessions. Different doses (1-32 μg/kg) of nalmefene were given in a random order by a single dosing procedure. Effects of intravenous nalmefene were assessed by comparing accumulated total scratches during the second and sixth session after this systemic intervention.
Based on the previously described protocol, 32 μg/kg of nalmefene was chosen for the pKB antagonism study in the second group of monkeys, because this dose significantly reduced scratching. Theoretically, under specific conditions (e.g., competitive and reversible antagonism), the antagonist in vivo pA2 and pKB values for an agonist should be identical. The in vivo pKB analysis can be achieved by use of only one dose of the antagonist and would produce a rightward shift of the agonist dose—response curve.17,19 The magnitude of rightward shift of the dose—response curve would reveal certain receptor populations mediating the observed effects. Nalmefene (32 μg/kg) was administered subcutaneously in the back (i.e., around the scapular region) 3 min before intrathecal morphine injection. The dose-response curves of intrathecal morphine for both scratching responses and thermal antinociception were then determined.
Statistical Analysis
Individual scratching responses were accumulated for all six sessions (15 min per session for six sessions). Individual tail-withdrawal latencies in 50°C water were converted to percent of maximum possible effect (%MPE) by the following formula: %MPE = [(test latency - control latency)/(cutoff latency, 20 s - control latency)] × 100. The area under the curve (%MPE × hours) was used to estimate the magnitude and duration of intrathecal morphine-induced antinociception. The dose-dependent effects of intrathecal morphine and the significant reduction of scratching responses by intravenous nalmefene were analyzed by one-way analysis of variance followed by the Newman-Keuls test. Individual intrathecal morphine ED50 values and 95% confidence limits (CLs) for both scratching responses and antinociception were calculated by least-squares regression using the portion of the dose-response curves spanning the 50% effects in the Manual of Pharmacologic Calculations with Computer Programs.20 The dose ratios were calculated by dividing individual ED50 values in the presence of subcutaneous nalmefene by the baseline ED50 values (i.e., intrathecal morphine alone). Individual apparent pKB values were determined by a modified equation17,19:pKB = -log [B/(dose ratio - 1)], in which B equals the antagonist dose in moles per kilogram. Mean pKB values ± 95% CLs also were calculated from individual pKB values for nalmefene. Apparent pKB values were considered to be significantly different when their 95% CLs did not overlap. The aforementioned statistical analysis is the standard criterion for this type of pharmacologic study.20
Drugs
Morphine sulfate (Mallinckrodt, St. Louis, MO) and nalmefene HCl (National Institute on Drug Abuse, Bethesda, MD) were dissolved in saline. For systemic administration, nalmefene was administered either subcutaneously or intravenously at a volume of 0.1 ml/kg.
Results
Dose-Response of Intrathecal Morphine
Low to medium doses of intrathecal morphine (1-32 μg) dose-dependently induced scratching (fig. 1, top). However, there was no dose dependency with higher doses of intrathecal morphine (100-320 μg; fig. 1, bottom). Peak effects were observed 1-2 h after intrathecal injection, and scratching lasted for at least 6 h. At 24 h after intrathecal injection, the subjects’ scratching responses were similar to those observed in the conditions of the vehicle and 1-μg morphine injection (data not shown).
Fig. 1.
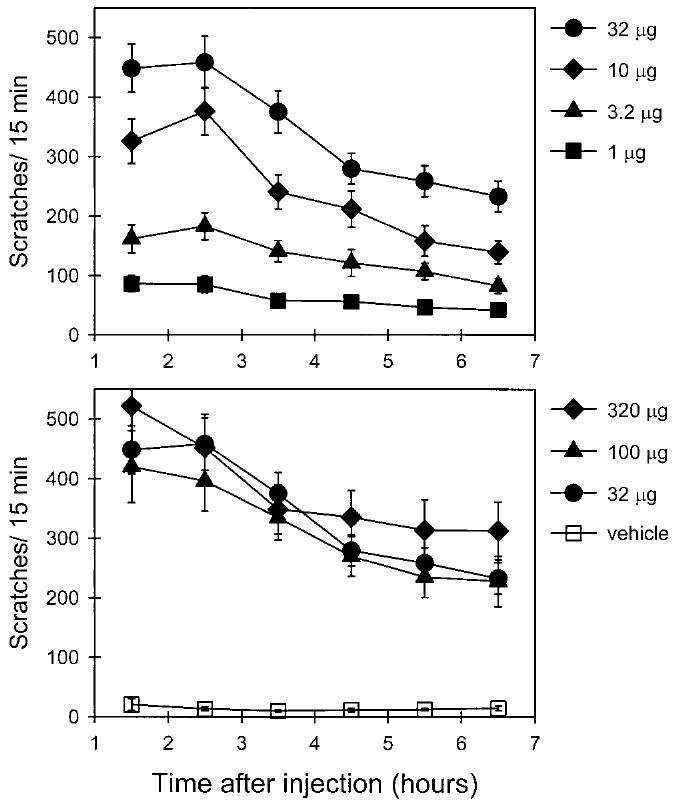
Average time course of intrathecal morphine-induced scratching responses in monkeys (n = 8). Each value represents the mean ± SEM (two to three replications). Abscissae (both panels): time (hours) after intrathecal injection. Ordinates (both panels): scratches per 15 min during each session. Solid symbols represent different doses (micrograms) of intrathecal morphine, and open squares represent the intrathecal vehicle (saline) injection. See figure 2 for individual dose-response curves of intrathecal morphine and Materials and Methods for other details.
Figure 2 illustrates each subject’s dose-response of intrathecal morphine-induced scratching accumulated across six test sessions (i.e., 6-h duration). These data indicate that monkeys have different susceptibilities to intrathecal morphine-induced scratching. For example, 32 μg of intrathecal morphine induced profound scratching responses in monkeys no. MK1 and MK2, but did not evoke similar scratching responses in monkeys no. MK3 and MK4. In addition, monkey no. MK5 had maximum scratching responses at the 320-μg dose, whereas monkeys no. MK6-MK8 had maximum responses at the 32-μg dose. Statistical analysis indicates that intrathecal morphine, from low (1 or 3.2 μg) to high doses (320 μg), significantly evoked scratching responses compared with vehicle (saline) injections (P < 0.05 and 0.01, respectively) and reached a plateau for most monkeys at higher doses (100-320 μg). It is worth noting that both monkeys no. MK4 and MK7 vomited at the 320-μg dose. They were not tested further at this dose.
Fig. 2.
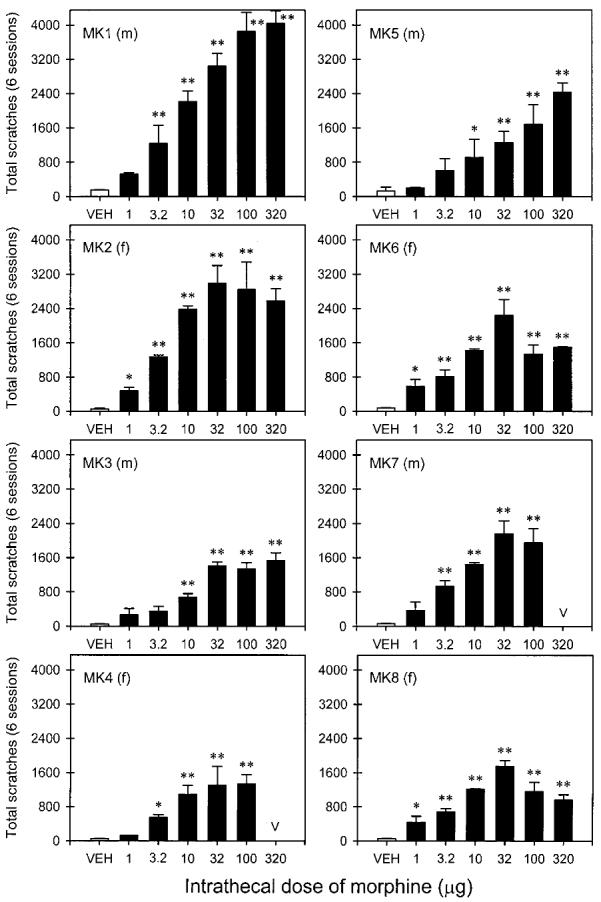
Different doses of intrathecal morphine-induced scratching responses (15 min per session for six sessions) accumulated across the six test sessions in eight monkeys. Each panel represents one monkey and its gender. Abscissae (all panels): different doses (micrograms) of intrathecal morphine. Ordinates (all panels): total scratches accumulated in six test sessions. The character “v” represents vomiting by monkeys at this dose. Asterisks represent a significant difference (*P < 0.05; **P < 0.01) from the vehicle (VEH) condition. Other details are as in figure 1.
The second group of monkeys displayed a consistent profile in warm-water tail-withdrawal responses. They kept their tails in 40°C water for 20 s (cutoff latency) and removed their tails from 50 and 55°C water rapidly (within 1-3 s). Figure 3 illustrates that medium to high doses of intrathecal morphine (10-320 μg) dose-dependently produced thermal antinociception in 50°C water. In particular, both 100 and 320 μg morphine produced maximum antinociception with a long-lasting duration (i.e., approximately 4 h). We did not test higher doses (e.g., 1,000 μg) of morphine alone for safety reasons, as we occasionally observed moderate respiratory depression, slight sedation (i.e., staring into the space), and slight loss of body balance among subjects 1-2 h after 320 μg of intrathecal morphine. Although this study did not use a motor measurement, it should be noted that monkeys did not have overt behavioral changes, such as sedation and motor dysfunction, at the dose range between 1 and 100 μg of intrathecal morphine.
Fig. 3.
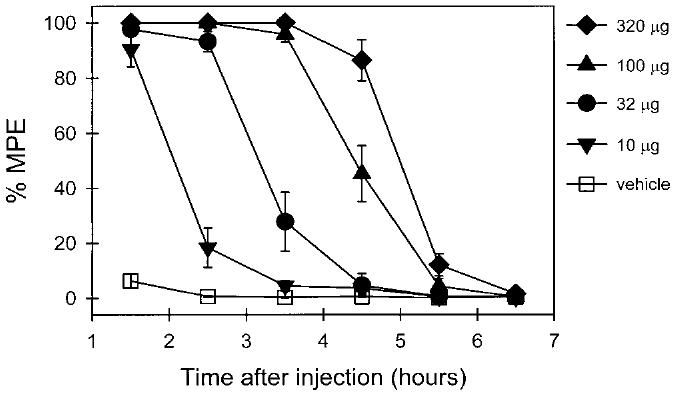
Average time course of intrathecal morphine-induced antinociception against 50°C water in monkeys (n = 4). Each value represents the mean ± SEM (two to three replications). Abscissa: time (hours) after intrathecal injection. Ordinate: percent of maximum possible effect. Solid symbols represent different doses (micrograms) of intrathecal morphine, and open squares represent the intrathecal vehicle (saline) injection. See figure 4 for individual dose-response curves of intrathecal morphine and Materials and Methods for other details.
Figure 4 illustrates each subject’s dose-response of intrathecal morphine-induced antinociception across six test sessions (i.e., 6 h). Low doses (1-3.2 μg) of intrathecal morphine did not produce significant antinociception in this procedure. Medium to high doses (10-320 μg) of intrathecal morphine significantly produced antinociception against 50°C water in a dose-dependent manner (P < 0.05 and 0.01, respectively). It should be noted that ketamine, administered before intrathecal injection, may have influenced the behavioral measurement. Monkeys normally recovered from ketamine anesthesia (e.g., body balance and motor coordination) within 25-40 min in this procedure. However, considering the possible residual effects of ketamine, behavioral measurements were not started until 1 h after intrathecal injection. Nevertheless, to what extent ketamine may interfere with behavioral observations in the present study is unknown.
Fig. 4.
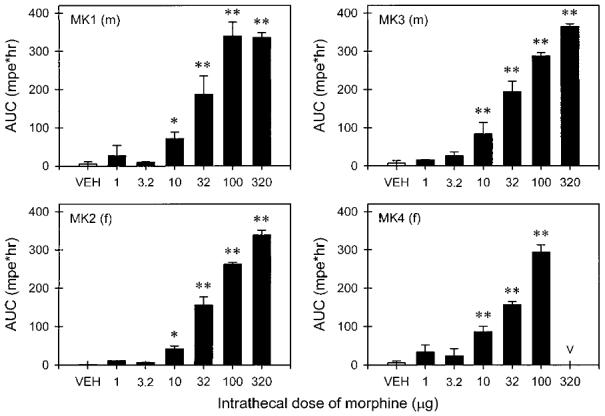
Different doses of intrathecal morphine-induced antinociception against 50°C water during the six test sessions in four monkeys. Abscissae (all panels): different doses (micrograms) of intrathecal morphine. Ordinates (all panels): area under curve (percent maximum possible effect × hours). Asterisks represent a significant difference (*P < 0.05; **P < 0.01) from the vehicle (VEH) condition. Other details are as in figures 2 and 3.
Antagonism of Intrathecal Morphine
Figure 5 shows the efficacy of intravenous nalmefene in suppressing intrathecal morphine-induced scratching responses. The dose of intrathecal morphine chosen was based on each monkey’s previously determined dose that produced maximum scratching responses (320 μg for monkey no. MK5 and 32 μg for monkeys no. MK6-MK8). Intervention with intravenous nalmefene dose-dependently attenuated subsequent scratching responses in each monkey between the second and sixth session. In particular, both 10 and 32 μg/kg significantly attenuated scratching responses in these four monkeys.
Fig. 5.
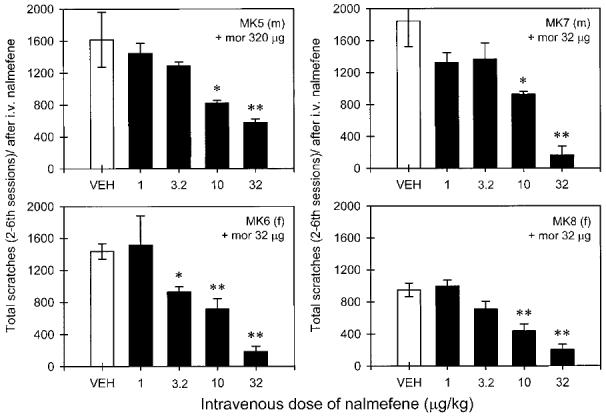
Effect of intravenous nalmefene in attenuating intrathecal morphine-induced scratching responses in four monkeys. Each value represents the mean ± SEM (two to three replications). Abscissae (all panels): different doses (micrograms per kilogram) of intravenous nalmefene. Ordinates (all panels): total scratches accumulated from the second to sixth session after intravenous injection. Asterisks represent a significant difference (*P < 0.05; **P < 0.01) from the vehicle (VEH) injection. Other details are as in figures 1 and 2.
Pretreatment with subcutaneous nalmefene (32 μg/kg) produced a rightward shift of the intrathecal morphine dose—response curve for scratching in all monkeys in the second group (fig. 6). Similar rightward shifts of intrathecal morphine dose-response curves for antinociception were also observed (fig. 7). Subcutaneous nalmefene, 32 μg/kg administered alone, did not produce any effects in this procedure (data not shown). The ED50 calculations from the linear ascending portion of each subject’s dose-response curve are summarized in table 1. As shown, a single dose of subcutaneous nalmefene produced approximately a 10-fold rightward shift for both scratching responses and antinociception in monkeys (figs. 6 and 7). The pKB analysis did not reveal any difference for nalmefene antagonism between scratching and antinociception (i.e., both mean pKB values were within similar 95% CLs, table 1).
Fig. 6.
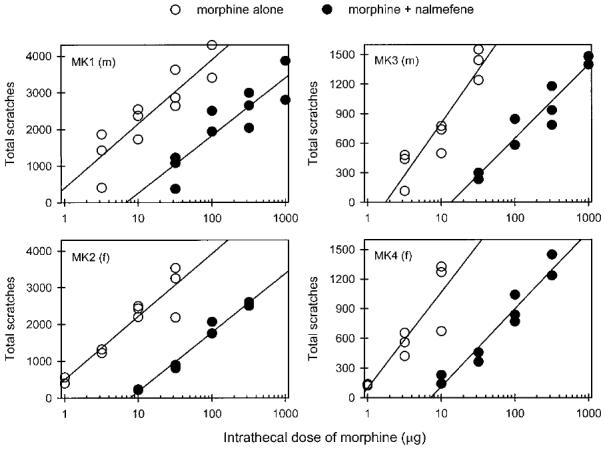
Rightward shifts of intrathecal morphine dose-response curves in scratching by a single dose (32 μg/kg, administered subcutaneously) of nalmefene pretreatment. Abscissae (all panels): intrathecal doses (micrograms) of morphine. Ordinates (all panels): total scratches accumulated in six test sessions. Open circles represent total scratching responses after intrathecal morphine. Solid circles represent total scratching responses after intrathecal morphine in the presence of nalmefene pretreatment. See figure 2, table 1, and Materials and Methods for other details.
Fig. 7.
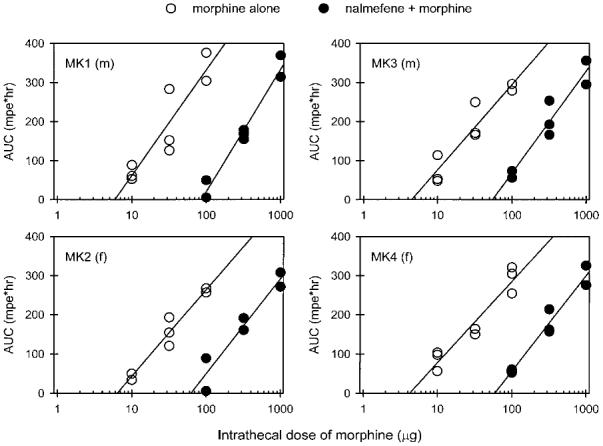
Rightward shifts of intrathecal morphine dose-response curves in thermal antinociception by a single dose (32 μg/kg, administered subcutaneously) of nalmefene pretreatment. Abscissae (all panels): intrathecal doses (micrograms) of morphine. Ordinates (all panels): area under curve (percent maximum possible effect × hours). Open circles represent antinociceptive effects after intrathecal morphine. Solid circles represent antinociceptive effects after intrathecal morphine in the presence of nalmefene pretreatment. See figure 4, table 1, and Materials and Methods for other details.
Table 1.
Nalmefene (32 μg/kg) Antagonism of Intrathecal Morphine-induced Scratching Responses and Thermal Antinociception
| Scratching Responses |
Thermal Antinociception |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morphine Alone |
Morphine + Nalmefene |
Morphine Alone |
Morphine + Nalmefene |
|||||||||
| Subjects | ED50 (μg) | 95% CL | ED50 (μg) | 95% CL | Dose Ratio | pKB* | ED50 (μg) | 95% CL | ED50 (μg) | 95% CL | Dose Ratio | pKB† |
| MK1 | 7.2 | 3.6-14.3 | 113.9 | 55.0-235.5 | 15.8 | 8.20 | 35.0 | 12.1-101.0 | 410.8 | 335.3-503.4 | 11.7 | 8.06 |
| MK2 | 4.4 | 0.9-23.1 | 64.4 | 43.7-94.6 | 14.5 | 8.16 | 39.2 | 23.7-64.9 | 304.7 | 198.0-468.9 | 7.8 | 7.86 |
| MK3 | 15.3 | 2.6-92.0 | 137.1 | 66.6-282.5 | 9.0 | 7.93 | 32.9 | 19.4-55.9 | 302.7 | 69.8-1312.8 | 9.2 | 7.94 |
| MK4 | 5.2 | 0.5-58.7 | 50.6 | 21.7-118.2 | 9.7 | 7.97 | 35.1 | 24.9-49.4 | 310.0 | 122.1-787.0 | 8.8 | 7.92 |
Mean pKB 58.06; 95% CL, 7.85-8.28.
† Mean pKB 57.94; 95% CL, 7.81-8.08.
Discussion
The present study illustrates that both scratching responses and thermal antinociception can be studied in the same monkey after intrathecal morphine administration. Both behavioral effects were long-lasting and dose-dependent. The antagonist study confirmed that μ opioid receptors mediated intrathecal morphine-induced scratching and antinociception under these experimental conditions.
Dose-Response of Intrathecal Morphine
This study clearly shows the long duration and dose dependency of intrathecal morphine-induced scratching in monkeys (figs. 1 and 2). For most monkeys, 10 and 32 μg of intrathecal morphine evoked maximum scratching activity across the test sessions for 6 h. The dose dependency can be observed at the lower dose range (e.g., 1-32 μg). However, scratching responses seemed to reach a plateau at higher doses such as 100 and 320 μg. This dose-response profile is similar to the finding in a recent clinical study,21 which showed that patients given intrathecal morphine (0.2-0.5 mg) reported similarly high pruritus scores, but lower doses (0.025-0.075 mg) of intrathecal morphine produced lower pruritus scores. Another study also showed that both 1 and 2 mg intrathecal morphine had 92-100% of parturients reporting an itching sensation.2 Taken together, these studies indicate that the dose-response of pruritus may depend partly on the dose range studied.
Itch is a skin sensation leading to a desire to scratch. This sensation is distinct from pain or touch in its nature.22 The intensity of itching sensation in monkeys in this study was quantified as number of scratches. Monkeys showed different susceptibilities to intrathecal morphine-induced scratching. This observation is consistent with clinical studies indicating that the incidence of pruritus varies widely from 0 to 100% in patients receiving spinal opioids.4,5 These large individual differences should be considered when treating patients with opioid medication. It would be interesting to investigate if there is a correlation of itching sensitivity in the same individual who responds to different sources of itch stimulation (i.e., spinal opioids vs. local/peripheral itch mediators, such as substance P, interleukin-2, and histamine).
It is worth noting that scratching in this primate model is generalized; monkeys scratch the whole body, including trunk, limbs, tail, and face. The majority of scratching on trunk and limbs may reflect the distribution of the 1-ml injection volume of intrathecal morphine within the cerebrospinal fluid surrounding the spinal cord. To what extent intrathecal morphine has cephalad migration in the cerebrospinal fluid requires further study, as intrathecal or epidural morphine injected in different volumes in primates migrated rostrally in varying quantities.23-26 It will be interesting to investigate if monkeys change the scratching locations after intracisternal injection of morphine in this procedure. In contrast, clinical studies suggest that the most common location of intrathecal morphine-induced pruritus in parturients is the facial area.4,5 The medullary dorsal horn has been demonstrated to be one central site in which μ opioid agonists act to produce facial scratching in monkeys.27 It has been speculated that cerebrospinal fluid flow may radically increase under strain conditions such as childbirth, which may increase the possibility of spinal opioids reaching the brain stem.27
In the warm-water tail-withdrawal assay, intrathecal morphine also dose-dependently produced long-lasting antinociception in monkeys (figs. 3 and 4). The dose dependency of intrathecal or epidural morphine-induced prolonged antinociception in primates has been well documented in the literature.9,10,21,28 In this study, 320 μg of intrathecal morphine produced antinociception for 4 h. However, in the shock titration threshold procedure,9,10 1,000-1,200 μg intrathecal morphine produced longer antinociception for approximately 18-20 h in monkeys. Comparing each monkey’s ED50 values for both behavioral end points indicates that intrathecal morphine is more potent to induce scratching than antinociception in the tail-withdrawal procedure (table 1). Nevertheless, it needs to be noted that analgesic ED50 values in experimental pain models can be changed by using different sources or intensities of nociceptive stimuli.15,16 For example, μ opioid agonists are more potent to produce antinociception against capsaicin- or prostaglandin E2-induced thermal hyperalgesia than the noxious 50°C water used in this study.29,30 Therefore, one must interpret the present results with caution, remembering that intrathecal morphine ED50 values for both pain relief and pruritus in patients may be similar or not, depending on different forms and intensities of pain.
The long-lasting scratching responses and thermal antinociception of intrathecal morphine was centrally mediated because a centrally effective dose (320 μg) of morphine administered subcutaneously in the back did not produce any effects in monkeys (data not shown). Several studies have demonstrated that spinal opioids produce effects centrally across different species and assays.23,31 In the warm-water tail-withdrawal procedure, subcutaneous morphine also produced antinociception against 50°C water in rhesus monkeys.16,29 However, the dose of intrathecal morphine (10-320 μg) was much less than systemic morphine (3.2-10 mg/kg, administered subcutaneously) in rhesus monkeys under this condition. In a pilot experiment, we found that a single dose of subcutaneous morphine (10 mg/kg) produced antinociception for approximately 4 h, but monkeys did not have as much scratching activity when compared with 320 μg of intrathecal morphine (unpublished observation). It seems that intrathecal morphine evokes a unique profile of scratching responses in which systemic morphine may have general inhibition. This notion can be supported by an observation that intervention with intramuscular morphine (1 mg/kg) reduced ongoing facial scratching behavior in monkeys.32 The hydrophilic property of morphine and the associated difficulty crossing the blood-brain barrier may be part of the reason for this phenomenon.33 It will be important to investigate further the relative potency in evoking scratching between intrathecal and subcutaneous administration of μ opioid agonists with different lipophilicities.
Antagonism of Intrathecal Morphine
After intrathecal morphine-induced scratching, intravenous nalmefene dose-dependently attenuated this activity for the remaining test sessions (fig. 5). Nalmefene is a very long-lasting opioid antagonist. Its onset is within a few minutes, and its antagonist effects last for more than 8 h in humans after systemic administration.11 It has a similar duration of antagonist action in rhesus monkeys, approximately 6 h, in a behavioral assay.12 In addition, nalmefene has been used to ameliorate the pruritus of cholestasis, indicating the involvement of increased endogenous opioid neurotransmission.34 Nevertheless, it is not clear which opioid receptor subtype mediated intrathecal morphine actions.
In vivo pKB analysis can be used to verify functional receptor populations of intrathecal morphine for both scratching and antinociception. If both behavioral effects are mediated by the same receptor population, the same magnitude of rightward shifts of dose-response curves are expected.17,19 Pretreatment with a single dose of nalmefene (32 μg/kg) produced approximately 10-fold rightward shifts of each monkey’s dose-response curves of intrathecal morphine for scratching and antinociception (figs. 6 and 7). The mean nalmefene pKB values (95% CL, 7.81-8.28) were similar for both behavioral end points (table 1), indicating that intrathecal morphine-induced scratching and antinociception are mediated by the same receptor population. These values are not different from the nalmefene pA2 values (8.16-8.45) for systemic μ opioid agonists, including alfentanil and morphine, in antinociception in rhesus monkeys.12 This indicates that intrathecal morphine produces scratching and antinociception through μ opioid receptors that are functionally similar to that acted on by systemic μ agonists.9 The μ opioid receptor-mediation in intrathecal morphine-induced scratching is also supported by the evidence that central administration of κ and δ opioid agonists does not induce scratching in rodents and monkeys.6,35
Although morphine can release histamine from mast cells, this does not seem to be the mechanism underlying intrathecal morphine-induced pruritus. Several studies have shown that antihistamines are not effective in relieving opioid-mediated pruritus.27,36 Antihistamines may be effective antipruritics secondary to their sedative effects.4,22 Although opioid antagonists are effective in attenuating opioid-mediated pruritus, they are not ideal therapeutic agents for parturients. Several studies have shown that spinal opioid-maintained analgesia was reversed when the opioid antagonist was systemically applied to treat pruritus.37-39 Careful titration of doses of intravenous opioid antagonists to partially antagonize opioid receptors may occasionally be achieved in the clinical setting. However, variation of dose-response among patients may complicate this treatment strategy. The data presented in this study do not support pure opioid antagonists for treatment, because nalmefene produced parallel reduction of both scratching and antinociception. Perhaps some mixed opioids, such as nalbuphine and butorphanol, with low to medium efficacy at both μ and κ receptors, are useful antipruritics, as they may partially antagonize μ actions with intact κ actions to maintain analgesic function.36,37,39 Recently, several agents, such as ondansetron and tenoxicam, have been proposed to treat spinal morphine-induced pruritus.40,41 It will be interesting to investigate these agents in this nonhuman primate model and further verify the role of 5-HT3, prostaglandins, and other neurotransmitters in pruritus.
In summary, this study demonstrates that intrathecal morphine-induced scratching and antinociception in monkeys are mainly mediated by μ opioid receptors. It also illustrates individual differences in dose-response of both behavioral effects. This experimental itch model provides a valuable pharmacologic basis for identifying potential therapeutic agents that may attenuate scratching behavior without reversing antinociception. It can be further used to explore the mechanisms underlying these phenomena.
Acknowledgments
The authors thank Drs. James H. Woods and Kevin K. Tremper for critical advice and generous support for this study and express their gratitude to Kurt Willmont, Mark Johnson, Michael Song, Kevin Choo, Tom Larmee, Jim Ferguson, John Busenbark, Beck McLaughlin, and Zana Logovsky for excellent technical assistance.
Supported by grant no. DA00254 from the United States Public Health Service, Rockville, Maryland; and the Clinical Research Partnership Fund from the University of Michigan Medical School, Ann Arbor, Michigan. Preliminary results presented at the 9th World Congress on Pain, Vienna, Austria, August 22-27, 1999, and the 31st Annual Meeting of the Society for Obstetric Anesthesia and Perinatology, Denver, Colorado, May 19-22, 1999.
References
- 1.Wang JK, Nauss LA, Thomas JE. Pain relief by intrathecally applied morphine in man. ANESTHESIOLOGY. 1979;50:149–51. doi: 10.1097/00000542-197902000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Baraka A, Noueihid R, Hajj S. Intrathecal injection of morphine for obstetric analgesia. ANESTHESIOLOGY. 1981;54:136–40. doi: 10.1097/00000542-198102000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Cousins MJ, Mather LE. Intrathecal and epidural administration of opioids. ANESTHESIOLOGY. 1984;61:276–310. [PubMed] [Google Scholar]
- 4.Chaney MA. Side effects of intrathecal and epidural opioids. Can J Anaesth. 1995;42:891–903. doi: 10.1007/BF03011037. [DOI] [PubMed] [Google Scholar]
- 5.Kam PCA, Tan KH. Pruritus: Itching for a cause and relief? Anaesthesia. 1996;51:1133–8. doi: 10.1111/j.1365-2044.1996.tb15050.x. [DOI] [PubMed] [Google Scholar]
- 6.Tohda C, Yamaguchi T, Kuraishi Y. Intracisternal injection of opioids induces itch-associated response through mu-opioid receptors in mice. Jpn J Pharmacol. 1997;74:77–82. doi: 10.1254/jjp.74.77. [DOI] [PubMed] [Google Scholar]
- 7.Ko MC, Johnson MD, Choo KS, Song MS, Chang D, Naughton NN, Woods JH. An experimental itch model in rats: Characterization of intracisternal morphine-induced scratching and antinociception (abstract) FASEB J. 1999;13:A802. [Google Scholar]
- 8.Yaksh TL, Harty GJ. Pharmacology of the allodynia in rats evoked by high-dose intrathecal morphine. J Pharmacol Exp Ther. 1988;244:501–7. [PubMed] [Google Scholar]
- 9.Yaksh TL, Reddy SV. Studies in the primate on the analgetic effects associated with intrathecal actions of opiates, alpha-adrenergic agonists and baclofen. ANESTHESIOLOGY. 1981;54:451–67. doi: 10.1097/00000542-198106000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Yaksh TL. In vivo studies on spinal opiate receptor systems mediating antinociception: I. Mu and delta receptor profiles in the primate. J Pharmacol Exp Ther. 1983;226:303–16. [PubMed] [Google Scholar]
- 11.Gal TJ, DiFazio CA. Prolonged antagonism of opioid action with intravenous nalmefene in man. ANESTHESIOLOGY. 1986;64:175–80. doi: 10.1097/00000542-198602000-00008. [DOI] [PubMed] [Google Scholar]
- 12.France CP, Gerak LR. Behavioral effects of 6-methylene naltrexone (nalmefene) in rhesus monkeys. J Pharmacol Exp Ther. 1994;270:992–9. [PubMed] [Google Scholar]
- 13.Institute of Laboratory Animal Resources Guide for the Care and Use of Laboratory Animals revised 1996National Academy Press; Washington, DC: 7th Edition [Google Scholar]
- 14.Dykstra LA, Woods JH. A tail withdrawal procedure for assessing analgesic activity in rhesus monkeys. J Pharmacol Methods. 1986;15:263–9. doi: 10.1016/0160-5402(86)90056-2. [DOI] [PubMed] [Google Scholar]
- 15.Walker EA, Butelman ER, DeCosta BR, Woods JH. Opioid thermal antinociception in rhesus monkeys: Receptor mechanisms and temperature dependency. J Pharmacol Exp Ther. 1993;267:280–6. [PubMed] [Google Scholar]
- 16.Zernig G, Butelman ER, Lewis JW, Walker EA, Woods JH. In vivo determination of mu opioid receptor turnover in rhesus monkeys after irreversible blockade with clocinnamox. J Pharmacol Exp Ther. 1994;269:57–65. [PubMed] [Google Scholar]
- 17.Ko MC, Butelman ER, Traynor JR, Woods JH. Differentiation of kappa opioid agonist-induced antinociception by naltrexone apparent pA2 analysis in rhesus monkeys. J Pharmacol Exp Ther. 1998;285:518–26. [PMC free article] [PubMed] [Google Scholar]
- 18.Butelman ER, Ko MC, Sobczyk-kojiko K, Mosberg HI, Van Bemmel B, Zernig G, Woods JH. Kappa-opioid receptor binding populations in rhesus monkey brain: Relationship to an assay of thermal antinociception. J Pharmacol Exp Ther. 1998;285:595–601. [PubMed] [Google Scholar]
- 19.Negus SS, Burke TF, Medzihradsky F, Woods JH. Effects of opioid agonists selective for mu, kappa and delta opioid receptors on schedule-controlled responding in rhesus monkeys: Antagonism by quadazocine. J Pharmacol Exp Ther. 1993;267:896–903. [PubMed] [Google Scholar]
- 20.Tallarida RJ, Murray RB. Manual of Pharmacologic Calculations with Computer Programs. 2nd Edition Springer-Verlag; New York: 1987. [Google Scholar]
- 21.Palmer CM, Emerson S, Volgoropolous D, Alves D. Dose-response relationship of intrathecal morphine for postcesarean analgesia. ANESTHESIOLOGY. 1999;90:437–44. doi: 10.1097/00000542-199902000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Greaves MW, Wall PD. Pathophysiology of itching. Lancet. 1996;348:938–40. doi: 10.1016/s0140-6736(96)04328-0. [DOI] [PubMed] [Google Scholar]
- 23.Bromage PR, Camporesi EM, Durant PA, Nielsen CH. Rostral spread of epidural morphine. ANESTHESIOLOGY. 1982;56:431–6. doi: 10.1097/00000542-198206000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Max MB, Inturrisi CE, Kaiko RF, Grabinski PY, Li CH, Foley KM. Epidural and intrathecal opiates: Cerebrospinal fluid and plasma profiles in patients with chronic cancer pain. Clin Pharmacol Ther. 1985;38:631–41. doi: 10.1038/clpt.1985.237. [DOI] [PubMed] [Google Scholar]
- 25.Hampton WA, Lavies NG, Downing JW, Brock-Utne JG, Salisbury RT, Elson KI. Cisternal cerebrospinal fluid concentrations of morphine following intrathecal and epidural administration in the baboon. Anaesth Intensive Care. 1987;15:445–50. doi: 10.1177/0310057X8701500416. [DOI] [PubMed] [Google Scholar]
- 26.Gustafsson LL, Hartvig P, Bergstrom K, Lundqvist H, Lindberg BS, Langstrom B, Svard H, Rane H, Tamsen A. Distribution of 11C-labelled morphine and pethidine after spinal administration to rhesus monkey. Acta Anaesthesiol Scand. 1989;33:105–11. doi: 10.1111/j.1399-6576.1989.tb02870.x. [DOI] [PubMed] [Google Scholar]
- 27.Thomas DA, Williams GM, Iwata K, Kenshalo DR, Jr, Dubner R. The medullary dorsal horn: A site of action of morphine in producing facial scratching in monkeys. ANESTHESIOLOGY. 1993;79:548–54. [PubMed] [Google Scholar]
- 28.Bailey PL, Rhondeau S, Schafer PG, Lu JK, Timmins BS, Foster W, Pace NL, Stanley TH. Dose-response pharmacology of intrathecal morphine in human volunteers. ANESTHESIOLOGY. 1993;79:49–59. doi: 10.1097/00000542-199307000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Negus SS, Butelman ER, Ai Y, Woods JH. Prostaglandin E2-induced thermal hyperalgesia and its reversal by morphine in the warm-water tail-withdrawal procedure in rhesus monkeys. J Pharmacol Exp Ther. 1993;266:1355–63. [PubMed] [Google Scholar]
- 30.Ko MC, Butelman ER, Woods JH. The role of peripheral mu opioid receptors in the modulation of capsaicin-induced thermal nociception in rhesus monkeys. J Pharmacol Exp Ther. 1998;286:150–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Yaksh TL. In: The spinal actions of opioids, Opioid II. Herz A, editor. Springer-Verlag; Berlin: 1993. pp. 53–90. [Google Scholar]
- 32.Thomas DA, Williams GM, Iwata K, Kenshalo DR, Jr, Dubner R. Multiple effects of morphine on facial scratching in monkeys. Anesth Analg. 1993;77:933–5. doi: 10.1213/00000539-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Herz A, Teschemacher HJ. In: Activities and sites of antinociceptive action of morphine-like analgesics and kinetics of distribution following intravenous, intracerebral and intraventricular application, Advances in Drug Research. Harper NJ, Simmonds AB, editors. Academic Press; New York: 1971. pp. 79–119. [Google Scholar]
- 34.Jones EA, Bergasa NV. The pruritus of cholestasis and the opioid system. JAMA. 1992;268:3359–62. [PubMed] [Google Scholar]
- 35.Thomas DA, Williams GM, Iwata K, Kenshalo DR, Jr, Dubner R. Effects of central administration of opioids on facial scratching in monkeys. Brain Res. 1992;585:315–7. doi: 10.1016/0006-8993(92)91227-6. [DOI] [PubMed] [Google Scholar]
- 36.Dunteman E, Karanikolas M, Filos KS. Transnasal butorphanol for the treatment of opioid-induced pruritus unresponsive to antihistamines. J Pain Symptom Manage. 1996;12:255–60. doi: 10.1016/0885-3924(96)00154-6. [DOI] [PubMed] [Google Scholar]
- 37.Cohen SE, Ratner EF, Kreitzman TR, Archer JH, Mignano LR. Nalbuphine is better than naloxone for treatment of side effects after epidural morphine. Anesth Analg. 1992;75:747–52. [PubMed] [Google Scholar]
- 38.Saiah M, Borgeat A, Wilder-Smith OH, Rifat K, Suter PM. Epidural-morphine-induced pruritus: Propofol versus naloxone. Anesth Analg. 1994;78:1110–3. doi: 10.1213/00000539-199406000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Wang JJ, Ho ST, Tzeng JI. Comparison of intravenous nalbuphine infusion versus naloxone in the prevention of epidural morphine-related side effects. Reg Anesth Pain Med. 1998;23:479–84. doi: 10.1016/s1098-7339(98)90031-1. [DOI] [PubMed] [Google Scholar]
- 40.Borgeat A, Stirnemann H-R. Ondansetron is effective to treat spinal or epidural morphine-induced pruritus. ANESTHESIOLOGY. 1999;90:432–6. doi: 10.1097/00000542-199902000-00017. [DOI] [PubMed] [Google Scholar]
- 41.Colbert S, O’Hanlon DM, Chambers F, Moriarty DC. The effect of intravenous tenoxicam on pruritus in patients receiving epidural fentanyl. Anaesthesia. 1999;54:76–80. doi: 10.1046/j.1365-2044.1999.00610.x. [DOI] [PubMed] [Google Scholar]


