Abstract
There has been an increase in data suggesting that besides air, hospital water is a potential source of transmission of filamentous fungi, and in particular Aspergillus fumigatus. Molecular characterization of environmental and clinical A. fumigatus isolates, collected prospectively during an 18-month period, was performed to establish if waterborne fungi play a role in the pathogenesis of invasive aspergillosis. Isolates recovered from water (n = 54) and air (n = 21) at various locations inside and outside the hospital and from 15 patients (n = 21) with proven, probable, or possible invasive aspergillosis were genotyped by amplified fragment length polymorphism analysis. Based on genomic fingerprints, the environmental A. fumigatus isolates could be grouped into two major clusters primarily containing isolates recovered from either air or water. The genotypic relatedness between clinical and environmental isolates suggests that patients with invasive aspergillosis can be infected by strains originating from water or from air. In addition, 12 clusters with genetically indistinguishable or highly related strains were differentiated, each containing two to three isolates. In two clusters, clinical isolates recovered from patients matched those recovered from water sources, while in another cluster the clinical isolate was indistinguishable from one cultured from air. This observation might open new perspectives in the development of infection control measures to prevent invasive aspergillosis in high-risk patients. The genetic variability found between airborne and waterborne A. fumigatus strains might prove to be a powerful tool in understanding the transmission of invasive aspergillosis and in outbreak control.
With the continuing increase in the number of severely immunocompromised patients, hospitals are faced with the growing problem of invasive aspergillosis and other opportunistic fungal infections (17). Since treatment of these infections is difficult and the outcome is often fatal, preventive measures are of major importance in the control of invasive filamentous fungal infections. Nosocomial invasive aspergillosis is thought to be primarily airborne; however, despite the use of appropriate hospital air filtration systems, the incidence of this infection continues to increase. Together with the lack of genetic relatedness between airborne strains and those causing invasive disease (10, 12), it is tempting to speculate about the existence of other routes of transmission.
As early as 1985, Aspergillus species and other filamentous fungi were shown to inhabit water distribution systems that deliver water to hospitals in Europe and the United States (13). Recently, there has been an increase in data supporting water as a potential source of filamentous fungi and, in particular, Aspergillus fumigatus (1, 2, 4, 28). However, direct evidence that waterborne A. fumigatus strains are involved in human infection is lacking. To test the hypothesis that a wet route of transmission might exist, we performed molecular typing studies on environmental and clinical isolates of A. fumigatus, prospectively collected during an 18-month period in a single center.
MATERIALS AND METHODS
Environment.
The sampling was performed at the pediatric oncology ward at the Rikshospitalet University Hospital in Oslo, Norway. This ward, containing two bone marrow transplantation (BMT) units, is situated in a relatively new wing of the department of pediatrics built in 1990. The outside air is filtered twice before entering the patient rooms (Camfil HI-FLO F95 air filtration system). After this double air filtration system, the air is cleared for 86, 98, and more than 99% of particles sized 0.35 to 0.45 μm, 0.75 to 1.0 μm, and 2.0 to 3.0 μm, respectively. In the BMT patient room, the air exchange flow is 10 m3/m2/h. The pediatric oncology ward has a yearly admission rate of almost 900 patients, and 10 to 12 allogeneic BMTs are performed annually. From 1992 to 2000, 25 proven invasive filamentous fungal infections were diagnosed, of which 15 (13 in adults, two in children) occurred among BMT patients (incidence, 5.3%).
Environmental sampling.
Water sampling was carried out on 16 different days between December 1998 and June 2000. The sampling was divided in two periods. During the winter season (December through February) sampling was performed on 10 days at a weekly interval; the other 6 sampling days were during the summer (June through August). The samples were taken from two different sink taps (cold water) and showers (warm water) in the BMT unit and from the main pipe bringing the water into the hospital. The samples from the main pipe were obtained via a tap connected with a short tube to this pipe. The tap was opened 10 to 15 min before taking the samples to rinse accumulated dust and dirt from the tube and tap. Water samples of 500 ml each were collected in sterile glass bottles and filtered through Millipore filters (pore size, 0.45 μm). The filters were deposited on Sabouraud glucose agar plates containing penicillin (20,000 IU/liter) and streptomycin (40 mg/liter). The filtration of the water samples was carried out in a safety cabinet (Holten LaminAir, biohazard class 2) to prevent contamination from surrounding air. In total, 168 water samples were taken: 96 from the taps, 36 from the showers, and 36 from the main pipe.
Furthermore, water samples were taken at the intake reservoir. The untreated (raw) water is recovered from large watersheds (surface water) in the forests surrounding Oslo. The untreated water from the lake is clear and without noticeable odor, taste, or color. It undergoes only a simple treatment with aeration (filtered air), microstraining (using Perlon filters with a mesh size of 5 μm), and chlorination (chlorine gas at 0.3 to 0.5 mg/liter). Sampling at the intake reservoir was performed in October 1999 and June 2000. In total, 58 water samples of 500 ml each were taken from both the untreated water (20) and the treated water (20). In June 2000, a total of 14 samples were taken also from surface water in the middle of the lake.
Air sampling was carried out on 15 different days from November 1998 to September 1999. Air in the BMT patient bathrooms, the BMT patient rooms, and the corridor and at the entrance of the ward and outside the hospital was sampled. In addition, 12 paired air samples were taken before and after showering (during 10 min). Air samples (volume, 1,800 liters each) were collected using a surface air sampler (SAS; Pool Bioanalysis Italiana, Milan, Italy). Special plates fitting into the air sampler (RODAC; Becton Dickinson, Cockeysville, Md.) containing Sabouraud glucose agar with penicillin (20,000 IU/liter) and streptomycin (40 mg/liter) were used.
A. fumigatus patient isolates.
During the 18-month period when the environmental sampling was carried out, all A. fumigatus isolates cultured from both pediatric and adult patients suspected of having invasive aspergillosis were collected. Patients were classified as having proven, probable, or possible invasive disease or colonization according to the consensus definition of invasive fungal infections (5). A total number of 28 isolates from 16 patients with either proven or probable invasive aspergillosis, including one patient with chronic granulomatous disease (CGD) colonized with A. fumigatus, were recovered from sputum, bronchoalveolar lavage (BAL) fluid, wound secretions, or tissue obtained after autopsy. Twenty-one (75%) of these isolates were available for molecular fingerprinting.
Culture and identification.
All plates were incubated at 35°C for 7 days and examined for the presence of filamentous fungi every 24 h. Subcultures were made from every CFU to obtain a pure culture. Fungal isolates were identified by macroscopic and microscopic characteristics. Aspergillus isolates were identified to species level, and A. fumigatus isolates were also tested for their ability to grow at 48°C. After cultivation and identification, all clinical isolates and part of the environmental isolates (n = 136; 49%) were stored in a special freeze broth at −80°C until further use. A selection of 75 environmental A. fumigatus isolates (54 were recovered from water and 21 from air) was studied for genetic relatedness in a blinded manner.
DNA isolation.
Chromosomal DNA was isolated from liquid cultures in RPMI 1640 medium (Invitrogen, Breda, The Netherlands) using standard molecular biological procedures (7). Briefly, hyphae were collected by centrifugation and treated with lyticase to produce spheroplasts. Following lysis in 10% sodium dodecyl sulfate, proteins were precipitated upon addition of 5 M potassium acetate and centrifugation in a microcentrifuge. Nucleic acids in the supernatant were precipitated with 0.6 volume of isopropanol, washed with 70% ethanol, dried, and dissolved in an appropriate amount of Tris-EDTA buffer.
Genomic fingerprinting by AFLP analysis.
Approximately 5 ng of chromosomal DNA was used in the amplified fragment length polymorphism (AFLP) procedure (27). DNA was digested using the restriction enzymes EcoRI and MseI (both from New England Biolabs, Beverly, Mass.). Restriction site-specific adapters were ligated to the chromosomal DNA fragments using T4 DNA ligase (Promega, Leiden, The Netherlands). Both reactions were performed in one combined restriction-ligation procedure. Approximately 10% of the restriction-ligation reaction was used in a PCR using adapter-based EcoRI and MseI primers. For detection purposes, the EcoRI primer was labeled with fluorescein. The MseI primer was extended with three selective residues (TGA) to limit the number of specifically amplified subgenomic PCR fragments that were generated. The unlabeled EcoRI primer did not contain selective extensions. PCR conditions were as follows. After an initial denaturation step for 4 min at 94°C, in the first 20 cycles, a touch down procedure was applied as follows: 15 s of denaturation at 94°C; 15 s of annealing at 66°C, with the temperature for each subsequent cycle lowered by 0.5°C; and 1 min of extension at 72°C. Cycling was then continued for 30 cycles at an annealing temperature of 56°C. After completion of the cycles an additional incubation for 10 min at 72°C was performed before the reaction mixture was cooled down. Amplification products were analyzed on an ABI/PRISM 3100 DNA analysis platform (Applied Biosystems, Nieuwenkerk aan den IJssel, The Netherlands). Obtained data were analyzed using GelCompar II software (Applied Maths, Kortrijk, Belgium) and the unweighted pair group method using arithmetic averages clustering using the Pearson correlation coefficient and expressed as percent similarity. DNA fragments smaller than 40 bp or larger than 550 bp were ignored. Several other fungal species were used as controls. The control isolates were all recovered from water samples and were identified as Aspergillus sp. (non-A. fumigatus), Penicillium sp., Trichoderma sp., and Rhizopus sp.
RESULTS
The results of part of the water sampling were described in detail previously (28). In total, 280 A. fumigatus isolates were recovered from the environmental samples during an 18-month period. One hundred and ninety-two isolates were cultured from water samples, and 88 were cultured from air samples (Table 1). A total of 96 A. fumigatus isolates were included in the analysis; 11 isolates were discarded based on signs of artifacts in the fingerprints, which may be due to impurities in the DNA preparations. Sixty-six environmental A. fumigatus isolates could be evaluated, together with 19 clinical isolates from 13 patients. The underlying disease and age of the patients, classification of the invasive aspergillosis, origin of the samples, and date of positive cultures are summarized in Table 2.
TABLE 1.
A. fumigatus isolates recovered from environmental samples
| Recovery location | Total no. of samples | Total no. of A. fumigatus isolates recovered |
|---|---|---|
| Water | 226 | 192 |
| Lake | 14 | 7 |
| Untreated water | 22 | 34 |
| Treated water | 22 | 28 |
| Main pipe | 36 | 30 |
| Tap | 96 | 91 |
| Shower | 36 | 2 |
| Air | 68 | 88 |
| Inside | 43 | 51 |
| Outside | 13 | 20 |
| Shower effect | 12 | 17 |
| Total | 294 | 280 |
TABLE 2.
Characteristics of patients from whom A. fumigatus isolates were recovereda
| Patient | Age (yr) | Underlying disease and/or condition | Invasive pulmonary aspergillosis status | Sample(s) | Date (day/mo/yr) | Strain |
|---|---|---|---|---|---|---|
| A | 75 | Tx (kidney) | Proven | Sputum | 18/02/1999 | 73a |
| BAL fluid | 22/02/1999 | 71a | ||||
| B | 49 | Bechterews disease; chronic empyema | CNPA | Sputum | 26/01/2000 | 30e |
| C | 48 | ARDS | Proven | Tracheal secretions | 20/12/1999 | 28e |
| D | 38 | Solumedrol therapy | Possible | Tracheal secretions | 28/05/2000 | 57e |
| E | 6 | Relapsed leukemia | Proven | Tracheal secretions | 05/06/2000 | 59e |
| Lung at autopsy | 13/06/2000 | 62e | ||||
| Lung at autopsy | 13/06/2000 | 63e | ||||
| F | 55 | COPD; emphysema | CNPA | Sputum | 02/12/1999 | 30a |
| G | 57 | Wegener's granulomatosis | Proven | Lung at autopsy | 20/12/1999 | 29e |
| I | 18 | CGD | Colonization | BAL fluid | 24/05/2000 | 53e |
| Sputum | 29/05/2000 | 55e | ||||
| Sputum | 31/05/2000 | 54e | ||||
| J | 63 | Tx (kidney) | Probable | BAL fluid | 20/03/1999 | 46b |
| K | 72 | Tx (thumb) | No | Wound | —b/11/1998 | 28 |
| L | 46 | ALL; post-BMT | Proven | Lung at autopsy | 22/03/1999 | 47b |
| M | 25 | Colitis ulcerosa; infliximab therapy | Proven | Sputum | 28/06/2000 | 66e |
| Lung at autopsy | 10/07/2000 | F26 | ||||
| N | 53 | Tumor cerebri | No | BAL fluid | 18/05/1999 | 24c |
Abbreviations: Tx, transplantation; CNPA, chronic necrotizing pulmonary aspergillosis; ARDS, adult respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; ALL, acute lymphatic leukemia.
Day of isolation not specified.
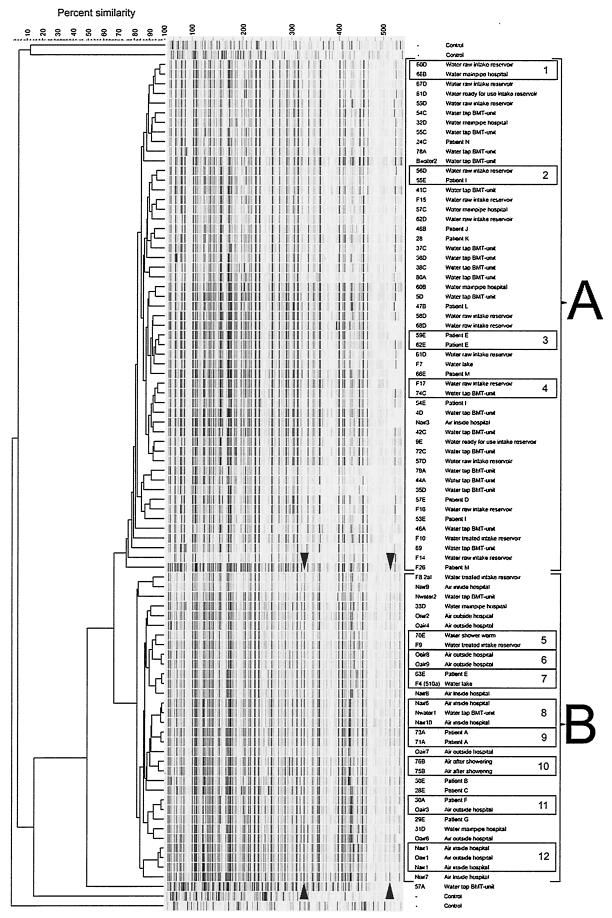
The dendrogram in Fig. 1 shows the results of the AFLP analysis. We defined strains to be genetically indistinguishable when the level of similarity was 96% or greater, based on the fact that repeated typing of the same strains showed this level of relatedness. Close genetic relatedness between strains was defined when they were at the 94 to 95% correlation level. Twelve clusters were found, of which seven included genetically indistinguishable strains. Two clusters each contained a clinical isolate and an isolate recovered from water. Close genetic relatedness was shown for an A. fumigatus strain recovered from sputum (patient I) and a strain recovered from water at the intake reservoir (cluster 2). Identical patterns were observed for an A. fumigatus strain recovered from autopsy cultures of the lungs of patient E and a strain recovered from water taken from the lake (cluster 7). In cluster 11, indistinguishable genotypes were found for a clinical strain (from patient F) and a strain recovered from outside air. Three clusters (clusters 1, 4, and 5) each contained two isolates from water at various locations. In one of these three the A. fumigatus strains were genetically indistinguishable, while in the other two clusters the strains were closely related. For two patients multiple A. fumigatus isolates obtained from different specimens on different days were genetically related (patient E) or indistinguishable (patient A). Furthermore, three clusters contained each two A. fumigatus strains isolated from both inside and outside air. One cluster containing two A. fumigatus isolates recovered from air in the BMT unit and one isolate recovered from tap water in a BMT patient bathroom showed identical AFLP patterns (cluster 8).
FIG.1.
Clustering of AFLP banding patterns of A. fumigatus isolates recovered from patients and the environment. Two main clusters of water-derived (A) and air-derived (B) isolates can be distinguished. Furthermore, 12 subclusters containing two or three isolates with identical or closely related genotypes are present.
Patient E, who had proven invasive pulmonary aspergillosis, was infected with two different A. fumigatus strains. One isolate recovered from the lung during autopsy and one from tracheal secretions while he was on a respirator were closely related to each other (see cluster 3); a second strain cultured from a postmortem lung sample (different tissue samples were obtained during autopsy) was genetically different from the first two strains. Patient M, who had proven invasive pulmonary aspergillosis, was also infected with two genetically different strains. Consecutive sputum and BAL fluid samples obtained during one week from patient I, who was suffering from CGD, showed that he was colonized with at least three different A. fumigatus strains.
The dendrogram (Fig. 1) shows that the environmental strains are divided into two clusters. The upper half of the dendrogram (strain numbers 60d to F26) consists of 84% of A. fumigatus strains isolated from water (cluster A), with only one strain recovered from air. In the lower part of the dendrogram (strain numbers F8 2aI to 57a), 94% of strains isolated from air are clustered (cluster B), with only nine recovered from water. The strains recovered from air have a banding pattern that contains several distinct bands (two of which are indicated in Fig. 1) not present in the cluster of strains recovered from water. The separation of the environmental strains into two clusters (water and air) was statistically significant (Fisher test; P < 0.0001).
During the 18-month study period, no episodes of contamination with A. fumigatus and other filamentous fungi were encountered in the microbiology laboratories where the samples were handled, thereby reducing the possibility of confounding due to cross-contamination. The filtration of the water samples was performed at a different location than where the environmental samples were cultured. Clinical isolates were processed in the clinical microbiology laboratory, a different location than where the environmental samples were handled.
DISCUSSION
To our knowledge, this is the first study to demonstrate (i) that A. fumigatus isolates recovered from air and water are clustered in different genetic groups, (ii) that A. fumigatus isolates from patients were grouped in either the water or the air cluster or both, (iii) that A. fumigatus isolates recovered from water showed genetic relatedness with isolates recovered from patients, and (iv) that the intake reservoir is the source of A. fumigatus strains found in tap water inside the hospital.
At present the “gold standard” for fingerprinting of A. fumigatus is restriction fragment length polymorphism analysis (6). Although yielding high-quality fingerprints with excellent discriminatory power, restriction fragment length polymorphism analysis requires large amounts of high quality DNA and is very laborious to perform. For obvious practical reasons, PCR-based fingerprinting methods are gaining more interest. We used AFLP fingerprinting for determining the epidemiologic relatedness between the collected isolates. To date several other PCR fingerprinting methods have been described for A. fumigatus, but they either lack the necessary reproducibility between experiments (like Random Amplified Polymorphic DNA analysis [RAPD]) or require previous genomic information (like microsatellite analysis) (14). AFLP fingerprinting, however, has proven to be a generic fingerprinting method with intrinsic superior reproducibility and a high degree of discriminatory power compared to other random amplification methods like RAPD (19). AFLP fingerprinting has already successfully been used with a large variety of other microorganisms with relatively large genomes including fungi (9, 15, 19, 23).
Our results suggest that the environmental A. fumigatus strains may consist of two distinct subgroups. By using the AFLP technique, we were able to distinguish A. fumigatus strains recovered from water and air. The number of cluster-specific DNA bands is on the order of 5 to 10% of the total number of DNA fragments in the fingerprints. Since with the AFLP technique DNA fragments are obtained from random locations within the fungal genome, this implies that roughly the same percentage of the organism's genome would be responsible for, or involved in, the difference between the two groups. It might be hypothesized that one group is best adapted to growth and transmission via the air and the other group is best adapted to an aqueous environment. It implies that the two subgroups are physically separated from each other and that the incidental recovery of an air-adapted isolate from the water, and vice versa, may be due to sampling errors or intermediate states of transmission. It may very well be that conidia from the air may have fallen into water supplies without being able to continuously manifest themselves in such an environment. Although this notion is highly speculative at this point, the genes involved may be responsible for the well recognized extreme hydrophobic nature of the organism which seems to be at odds with an aquatic habitat. We do know that filamentous fungi spend most of their lives in a humid environment such as soil, wood, leaf litter, and organic debris. Fungi proliferate by producing extensively hyphal networks that spread in all directions. To spread to new territory, however, most filamentous fungi need to produce conidia. Hydrophobins, small proteins secreted by filamentous fungi, release these fungal structures from their damp surroundings and enable them to grow up into the air to sporulate (30). Targeted disruption of the gene coding the hydrophobin protein led to less hydrophobic conidia, but furthermore, these mutants where not able to form aerial hyphae (20, 24). A further analysis of these cluster specific bands might provide additional information to explain our findings. The finding that environmental A. fumigatus can be genomic divided in two subgroups, water and air, might implicate that molecular fingerprinting of clinical A. fumigatus isolates leads us directly to the environmental source.
A. fumigatus strains originating from both water and air were shown to be able to infect patients, resulting in invasive aspergillosis. Eight patients were infected with A. fumigatus strains grouped into the predominantly water cluster. In addition, clinical isolates from two different patients, a leukemia patient suffering from invasive pulmonary aspergillosis and a CGD patient colonized with A. fumigatus in his lungs, were genotypically indistinguishable from and closely related to, respectively, strains recovered from water sources. Taken together, our data provide good circumstantial evidence of invasive aspergillosis and a link to water. Earlier suggestions that a wet route of transmission might exist can be found in anecdotal reports linking invasive aspergillosis with aspiration of contaminated surface water in near-drowning patients (22, 26). Furthermore, molecular characterization (RAPD) of a clinical A. fumigatus isolate with an isolate recovered from the shower wall showed genotypically indistinguishable A. fumigatus isolates (2). However, this retrospective study did not determine if the A. fumigatus isolate from the shower wall originated from water as opposed to air. At present, no other reports have been published using molecular tools to support or prove the existence of a wet route of transmission for A. fumigatus.
Two patients suffering from a proven invasive aspergillosis were probably infected with two different A. fumigatus strains. For patient E, a child with a relapse of acute leukemia, the two A. fumigatus strains recovered from two different lung tissue samples obtained at autopsy show that it is likely that he was indeed infected by two strains. Several previous studies have demonstrated that patients with invasive aspergillosis might be infected by more than one strain (7, 8, 18). Colonization with multiple A. fumigatus genotypes in the CGD patient has also been shown in patients with cystic fibrosis (11, 25).
The low level of genetic diversity of the A. fumigatus isolates in the two large clusters in our study is remarkable. Several reports have documented a huge diversity among environmental and clinical isolates, clouding any clear conclusions about sources of infecting strains and their transmission (12, 21). An explanation for the difference might be the small and relatively isolated geographic area in which the present study was performed.
Our findings might open new perspectives in preventing invasive aspergillosis in high-risk patients. Up until now, the standard infection control measures for the prevention of nosocomial invasive aspergillosis relied on strict air filtration methods such as laminar airflow and HEPA filtration to prevent exposure of high-risk patients to airborne fungal spores. The results presented in our study suggest that additional measures directed to water quality and activities leading to aerosolization of water might be required. It is clear that the level of contamination of hospital water varies between hospitals and countries, depending on the source of the water. Water originating from ground water was free of A. fumigatus as opposed to water derived from surface water (29). Although fungal conidia or elements were not eliminated during the purification process in this study, elimination of fungi during purification appears to be the logical strategy to reduce exposure of high-risk patients and requires further research. As yet it is unknown how patients become infected with waterborne A. fumigatus strains, although aerosolization appears to be the most logical route of infection since all our patients infected with a waterborne strain had a pulmonary infection. Restriction of exposure of high-risk patients to contaminated aerosolized water, such as that resulting from showers, has been suggested (3). Additional studies are required to further characterize the relative importance of each route of transmission ultimately to allow implementation and evaluation of preventive measures.
Acknowledgments
A. Warris and C. H. W. Klaassen contributed equally to the work presented in this paper.
This project has been supported by a European Community Grant (TMR Programme, EUROFUNG, contract FMRX-CT97-0145).
We thank Barto Veldhuis for his help with the graphics.
REFERENCES
- 1.Anaissie, E. J., R. T. Kuchar, J. H. Rex, A. Francesconi, M. Kasai, F.-M. C. Müller, M. Lozano-Chiu, R. C. Summerbell, M. C. Dignani, S. J. Chanock, and T. J. Walsh. 2001. Fusariosis associated with pathogenic Fusarium species colonization of a hospital water system: a new paradigm for the epidemiology of opportunistic mold infections. Clin. Infect. Dis. 33:1871-1878. [DOI] [PubMed] [Google Scholar]
- 2.Anaissie, E. J., S. L. Stratton, M. C. Dignani, R. C. Summerbell, J. H. Rex, T. P. Monson, T. Spencer, M. Kasai, A. Francesconi, and T. J. Walsh. 2002. Pathogenic Aspergillus species recovered from a hospital water system: a 3-year prospective study. Clin. Infect. Dis. 34:780-789. [DOI] [PubMed] [Google Scholar]
- 3.Anaissie, E. J., S. L. Stratton, M. C. Dignani, C.-K. Lee, T. H. Mahfouz, J. H. Rex, R. C. Summerbell, and T. J. Walsh. 2002. Cleaning patient shower facilities: a novel approach to reducing patient exposure to aerosolized Aspergillus species and other opportunistic molds. Clin. Infect. Dis. 35:86-88. [DOI] [PubMed] [Google Scholar]
- 4.Arvanitidou, M., S. Spaia, A. Velegraki, M. Pazarloglou, D. Kanetidis, P. Pangidis, N. Askepidis, Ch. Katsinas, G. Vayonas, and V. Katsouyannopoulos. 2000. High level of recovery of fungi from water and dialysate in haemodialysis units. J. Hosp. Infect. 45:225-230. [DOI] [PubMed] [Google Scholar]
- 5.Ascioglu, S., J. H. Rex, B. de Pauw, J. E. Bennet, J. Bille, F. Crokaert, D. W. Denning, J. P. Donnelly, J. E. Edwards, Z. Erjavec, D. Fiere, O. Lortholary, J. Maertens, J. F. Meis, T. F. Patterson, J. Ritter, D. Selleslag, P. M. Shah, D. A. Stevens, and T. J. Walsh. 2002. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin. Infect. Dis. 34:7-14. [DOI] [PubMed] [Google Scholar]
- 6.Bart-Delabesse, E., J. Sarfati, J. P. Debeaupuis, W. van Leeuwen, A. van Belkum, S. Bretagne, and J.-P. Latgé. 2001. Comparison of restriction fragment length polymorphism, microsatellite length polymorphism, and random amplification of polymorphic DNA analyses for fingerprinting Aspergillus fumigatus isolates. J. Clin. Microbiol. 39:2683-2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bart-Delabesse, E., C. Cordonnier, and S. Bretagne. 1999. Usefulness of genotyping with microsatellite markers to investigate hospital-acquired invasive aspergillosis. J. Hosp. Infect. 42:321-327. [DOI] [PubMed] [Google Scholar]
- 8.Bertout, S., F. Renaud, R. Barton, F. Symoens, J. Burnod, M.-A. Piens, B. Lebeau, M.-A. Viviani, F. Chapuis, J.-M. Bastide, R. Grillot, M. Mallié, et al. 2001. Genetic polymorphism of Aspergillus fumigatus in clinical samples from patients with invasive aspergillosis: investigation using multiple typing methods. J. Clin. Microbiol. 39:1731-1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boekhout, T., B. Theelen, M. Diaz, J. W. Fell, W. C. J. Hop, E. C. A. Abeln, F. Dromer, and W. Meyer. 2001. Hybrid genotypes in the pathogenic yeast Cryptococcus neoformans. Microbiology 147:891-907. [DOI] [PubMed] [Google Scholar]
- 10.Chazalet, V., J.-P. Debeaupuis, J. Sarfati, J. Lortholary, P. Ribaud, P. Shah, M. Cornet, H. V. Thien, E. Gluckman, G. Brücker, and J.-P. Latgé. 1998. Molecular typing of environmental and patient isolates of Aspergillus fumigatus from various hospital settings. J. Clin. Microbiol. 36:1494-1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cimon, B., F. Symoens, R. Zouhair, D. Chabasse, N. Nolard, A. Defontaine, and J-. P. Bouchara. 2001. Molecular epidemiology of airway colonisation by Aspergillus fumigatus in cystic fibrosis patients. J. Med. Microbiol. 50:367-374. [DOI] [PubMed] [Google Scholar]
- 12.Debeaupuis, J.-P., J. Sarfati, V. Chazalet, and J.-P. Latgé. 1997. Genetic diversity among clinical and environmental isolates of Aspergillus fumigatus. Infect. Immun. 65:3080-3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geldreich, E. E. 1996. Microbial quality of water supply in distribution systems, p. 103-158. CRC Lewis, Boca Raton, Fla.
- 14.Lasker, B. A. 2002. Evaluation of performance of four genotypic methods for studying the genetic epidemiology of Aspergillus fumigatus isolates. J. Clin. Microbiol. 40:2886-2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leissner, C. E. W., M. L. Niessen, and R. F. Vogel. 1997. Use of AFLP technique for the identification and discrimination of Fusarium graminearum. Cereal Res. Commun. 25:555-556. [Google Scholar]
- 16.Loeffler, J., H. Herbart, U. Schumacher, H. Reitze, and H. Einsele. 1997. Comparison of different methods for extraction of DNA of fungal pathogens from cultures and blood. J. Clin. Microbiol. 35:3311-3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marr, K. A., R. A. Carter, F. Crippa, A. Wald, and L. Corey. 2002. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin. Infect. Dis. 34:909-917. [DOI] [PubMed] [Google Scholar]
- 18.Radford, S. A., E. M. Johnson, J. P. Leeming, M. R. Millar, J. M. Cornish, A. B. M. Foot, and D. W. Warnock. 1998. Molecular epidemiological study of Aspergillus fumigatus in a bone marrow transplantation unit by PCR amplification of ribosomal intergenic spacer sequences. J. Clin. Microbiol. 36:1294-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Savelkoul, P. H. M., H. J. M. Aarts, J. de Haas, L. Dijkshoorn, B. Duim, M. Otsen, J. L. W. Rademaker, L. Schouls, and J. A. Lenstra. 1999. Amplified-fragment length polymorphism analysis: the state of an art. J. Clin. Microbiol. 37:3083-3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stringer, M. A., and W. E. Timberlake. 1995. dewA encodes a fungal hydrophobin component of the Aspergillus spore wall. Mol. Microbiol. 16:33-44. [DOI] [PubMed] [Google Scholar]
- 21.Symoens, F., J. Burnod, B. Lebeau, M. A. Viviani, M. A. Piens, A. M. Tortorano, N. Nolard, F. Chapuis, and R. J. Grillot. 2002. Hospital-acquired Aspergillus fumigatus infection: can molecular typing methods identify an environmental source? Hosp. Infect. 52:60-67. [DOI] [PubMed] [Google Scholar]
- 22.ter Maaten, J. C., R. P. Golding, R. J. M. Strack van Schijndel, and L. G. Thijs. 1995. Disseminated aspergillosis after near-drowning. Neth. J. Med. 47:21-24. [DOI] [PubMed] [Google Scholar]
- 23.van der Lee, T., I. de Witte, A. Drenth, C. Alfonso, and F. Govers. 1997. AFLP linkage map of the oomycete Phytophthora infestans. Fungal Genet. Biol. 21:278-291. [DOI] [PubMed] [Google Scholar]
- 24.van Wetter, M. A., F. H. J. Schuren, and J. G. H. Wessels. 1996. Targeted mutation of the Sc3 hydrophobin gene of Schizophyllum commune affects formation of aerial hyphae. FEMS Microbiol. Lett. 140:265-270. [Google Scholar]
- 25.Verweij, P. E., J. F. G. M. Meis, J. Sarfati, J. A. A. Hoogkamp-Korstanje, J. P. Latgé, and W. J. G. Melchers. 1996. Genotypic characterization of sequential Aspergillus fumigatus isolates from patients with cystic fibrosis. J. Clin. Microbiol. 34:2595-2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vieira, D. F., H. K. F. Van Saene, and D. R. Miranda. 1984. Invasive pulmonary aspergillosis after near-drowning. Int. Care Med. 10:203-204. [DOI] [PubMed] [Google Scholar]
- 27.Vos, P., R. Hogers, M. Bleeker, M. Reijans, T. van de Lee, M. Hornes, A. Frijters, J. Pot, J. Peleman, M. Kuiper, and M. Zabeau. 1995. AFLP: a new technique for DNA fingerprinting. Nucleic Acids Res. 23:4407-4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Warris, A., P. Gaustad, J. F. G. M. Meis, A. Voss, P. E. Verweij, and T. G. Abrahamsen. 2001. Recovery of filamentous fungi from water in a paediatric bone marrow transplantation unit. J. Hosp. Infect. 47:143-148. [DOI] [PubMed] [Google Scholar]
- 29.Warris, A., A. Voss, T. G. Abrahamsen, and P. E. Verweij. 2002. Contamination of hospital water with Aspergillus fumigatus and other molds. Clin. Infect. Dis. 34:1159-1160. [DOI] [PubMed] [Google Scholar]
- 30.Wösten, H. A. B., M. A. van Wetter, L. G. Lugones, H. C. van der Mei, H. J. Busscher, and J. G. Wessels. 1999. How a fungus escapes the water and grow into the air. Curr. Biol. 9:85-88. [DOI] [PubMed] [Google Scholar]