Abstract
trans-Sialidase is an enzyme present on the surface of Trypanosoma cruzi and is an important antigen recognized by sera from patients with Chagas' disease. In the present study we investigated whether the benznidazole treatment of patients with Chagas' disease induced changes in the reactivity of serum toward a recombinant form of trans-sialidase in order to develop an assay for monitoring of patients after treatment for Chagas' disease, which is needed at Chagas' disease control centers. By using an enzyme-linked immunosorbent assay containing a recombinant protein corresponding to the catalytic domain of trans-sialidase, we found that the antigen had a high specificity for sera from untreated patients with Chagas' disease. Sera from healthy individuals or patients with active visceral leishmaniasis minimally cross-reacted with the antigen. Anti-trans-sialidase immunoglobulin was detected in 98% of 151 untreated patients with Chagas' disease. Of these, 124 patients were treated for 60 days with benznidazole (5 mg/kg of body weight/day), and their sera were assayed for reactivity with the recombinant trans-sialidase. By using this methodology, three groups of patients could be established. The first group (60 patients), which was considered to have been successfully treated, showed no reactivity after treatment. The second group (46 patients) still showed signs of infection, and after treatment their sera recognized trans-sialidase, but with reduced titers. The third group (18 patients) was considered to be resistant to drug treatment, and their sera presented identical reactivities before and after treatment. These results suggest that determination of the absence of antibodies to recombinant trans-sialidase in treated patients by the present assay is indicative of treatment success, while the presence of antibodies may indicate the persistence of infection. Therefore, this method may be useful for the diagnosis and monitoring of patients undergoing benznidazole treatment.
Chagas' disease is a chronic illness that affects 16 million to 18 million people in Latin America. It is a prevalent infection in areas where the disease is highly endemic and where the vectorial transmission of Trypanosoma cruzi has not been eliminated or controlled (20, 31). The natural cycles involving triatomine bugs, wild and domestic reservoirs, as well as humans are still responsible for new cases of the disease; and a large number of patients still require drug treatment (8).
After the acute phase following T. cruzi infection, parasites are rarely found in blood, and the diagnosis is mainly based on serology. Blood centers and clinical laboratories generally use hemagglutination, immunofluorescence, and enzyme-linked immunosorbent assay (ELISA) with serum for the diagnosis of Chagas' disease by using antigens extracted from epimastigotes, the noninfective stage of T. cruzi. However, conventional serology is unable to distinguish whether patients treated with benznidazole are cured. A considerable number of results are inconclusive, even when different serological tests are used (2, 11, 17).
We have developed an ELISA using a recombinant protein corresponding to the N-terminal portion of the T. cruzi trans-sialidase (TS). This enzyme is produced by bloodstream trypomastigotes of T. cruzi, the parasite form responsible for disseminating the infection in mammalian hosts. TS contains two domains. One includes the active site and is located at the N terminus. The other is composed of 12-amino-acid repeats and is located at the C terminus (10, 28). The enzyme's N-terminal domain is responsible for the induction of specific antibodies that inhibit the enzymatic activity of TS during infection (14, 23, 24). Moreover, the N-terminal domain has important roles in the humoral (6, 15, 23) and cellular (26, 27) immune responses that control infection. Therefore, we aimed to investigate whether sera from patients with Chagas' disease specifically recognize this recombinant TS and if this recognition decreases in patients undergoing anti-T. cruzi chemotherapy with benznidazole.
MATERIALS AND METHODS
Patients and diagnosis.
A total of 124 adult patients with chronic Chagas' disease from the Laboratory of Xenodiagnosis, Instituto Dante Pazzanese de Cardiologia, São Paulo, Brazil, were evaluated by clinical and serological methods. Chagas' disease was diagnosed primarily on the basis of clinical examination, electrocardiogram, chest X ray, and conventional serological methods, including an indirect hemagglutination test (Biolab Mérieux Ltda, São Paulo, Brazil) (5), an indirect immunofluorescence test with formaldehyde-fixed epimastigotes as antigen (4), and ELISA (Laboratórios Salk, São Paulo, Brazil). None of the patients included in this study presented with cardiac alterations (indeterminate form), and before treatment all had sera produceding positive reactions by all three tests mentioned above. In addition, the patients were hemoculture positive (22).
Chemotherapy and evaluation.
Patients were treated for 60 days with 5 mg of benznidazole per kg of body weight per day (9). After treatment, they were evaluated for several years by clinical examination and parasitological and serological tests at 1-year intervals. Treatment and clinical evaluation were performed by one of us (Abilio Augusto Fragata-Filho). This protocol for the treatment of patients with Chagas' disease is traditionally used at the Instituto Dante Pazzanese de Cardiologia, São Paulo, which focuses mainly on the cardiac involvement and evolution of Chagas' disease (9).
Serum samples.
The sensitivity and specificity of TS were determined by assaying 201 serum samples from 151 patients with chronic Chagas' disease before the specific treatment, 40 healthy individuals who had never lived in an area where T. cruzi is endemic and who were negative for Chagas' disease by conventional serological methods, and 10 patients with active visceral leishmaniasis (which was diagnosed serologically by the Laboratory of Parasitology, Instituto Aldofo Lutz). The evolution of treatment was analyzed by assaying 372 samples, 124 samples before treatment and 248 samples 1 and 2 years after treatment. All sera used in this study were stored at −20°C without additives and were colleted from individuals who had given informed consent to participate in this protocol, which was approved by the Ethics Committees of the Instituto Dante Pazzanese de Cardiologia and Instituto Adolfo Lutz.
Recombinant TS production and purification.
Recombinant TS was generated and purified from Escherichia coli cells transformed with plasmid pTS-cat7, as described previously (25). The purity of each TS batch was checked by sodium dodecyl sulfate-10% polyacrylamide gel electrophoresis (SDS-PAGE) (12), and the protein concentration was estimated by the Bradford procedure (12).
TS ELISA.
The TS ELISA was performed with microtiter polystyrene plates (flat bottom; Corning) coated with the recombinant TS. Each well was incubated overnight at 4°C with 200 ng of recombinant TS dissolved in 0.1 ml of 0.1 M NaHCO3 (pH 8.5). Unbound antigen was removed by washing the plates with phosphate-buffered saline (PBS; pH 7.2) containing 0.05% Tween 20. The free binding sites were blocked by treating the wells with 5% skim milk-PBS. After 2 h, 50 μl of each serum sample diluted 1:50 in 5% skim milk-PBS was incubated for 60 min at 37°C. After five washes with PBS-Tween 20, the wells were incubated for 30 min at 37°C with a horseradish peroxidase-conjugated goat anti-human immunoglobulin G (IgG; Life Technologies) diluted 1:10,000 in 5% skim milk-PBS. After a new wash cycle with PBS-Tween 20, substrate solution (0.1 M citric acid, 0.2 M Na2HPO4, 0.05% o-phenylenediamine, 0.1% H2O2) was added to each well, and the plates were left to stand at room temperature in the dark for 15 min. Color development was stopped by adding 50 μl of 4 N H2SO4, and the absorbance was measured with an ELISA reader (Multiscan) with a 492-nm filter. To standardize the ELISA reaction, 20 serum samples from healthy individuals and 20 serum samples from patients with Chagas' disease with different concentrations of T. cruzi antibodies, as determined by conventional serology, were used. Different concentrations of purified recombinant TS (0.1 to 5 μg/ml) on the microtiter plates, different conjugate dilutions (1/100 to 1/100,000), and different serum dilutions (1/5 to 1/500) were tested (data not shown). The optimal TS concentration was 2 μg/ml, and the optimal conjugate dilution was 1:10,000. Each serum sample was assayed in duplicate. The absorbance values were subtracted from the background, and the arithmetic mean was calculated. The cutoff for each reaction was three times the mean and standard deviation for 20 serum samples from healthy individuals. The values shown in the figures represent the absorbance at 492 nm relative to the cutoff absorbances.
Immunoblotting.
SDS-PAGE and immunoblotting with purified recombinant TS were performed as described previously (30). One microgram of TS was loaded, fractionated by SDS-10% PAGE, and transferred to nitrocellulose membranes. The membranes were cut into 3- to 4-mm-wide strips, blocked for 2 h with 5% skim milk-PBS, and incubated with serum diluted 1:50 at 37°C. After 1 h, the strips were washed with PBS and incubated for 30 min at 37°C with goat horseradish peroxidase-conjugated anti-human IgG diluted in 1% skim milk-PBS. Bound antibodies were visualized after incubation with 0.017% diaminobenzidine and 0.1% H2O2 in PBS.
RESULTS
Sensitivity and specificity of TS as antigen in ELISA.
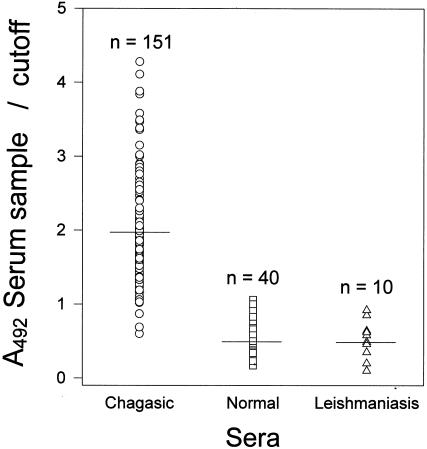
Specificity and sensitivity were assessed by testing 40 serum samples from apparently healthy individuals, 10 serum samples from patients with active visceral leishmaniasis, and 151 serum samples from untreated patients with chronic Chagas' disease. The absorbance at 492 nm of each serum sample was read and expressed as the ratio of the absorbance relative to that for the control sera. The values obtained are shown in Fig. 1; and a summary of the results, including the specificity and sensitivity for each group, is presented in Table 1. The mean value for sera from patients with Chagas' disease was 1.93. In this group, three serum samples presented values below 1.0, giving a sensitivity of 0.98 for the assay. In contrast, the serum samples from healthy individuals presented a mean value of 0.51. Three serum samples presented values greater than 1.0, resulting in a specificity of 0.925. All serum samples from patients with visceral leishmaniasis presented values below the cutoff, with mean values of 0.52. The specificity obtained when the results for all serum samples from individuals without Chagas' disease are considered was estimated to be 0.94.
FIG. 1.
Reactivities of sera from healthy individuals (squares), patients with Chagas' disease (circles), and patients with leishmaniasis (triangles) against recombinant TS by the TS ELISA. The results were calculated as the ratio of the absorbance of each serum sample at an optical density of 492 nm (A492) to the cutoff value. Values greater than 1.0 were considered reactive. The horizontal lines represent the arithmetic means.
TABLE 1.
Sensitivity, specificity, and 95% confidence intervals of recombinant TS in the ELISA
| Serum source | No. of patients
|
Avg ELISA value (95% confidence interval) | ||
|---|---|---|---|---|
| Total | Anti-TS negative | Anti-TS positive | ||
| Healthy individuals | 40 | 37 (0.925)a | 3 | 0.51 (0.43-0.59) |
| Leishmaniasis patients | 10 | 10 (1.0)a | 0 | 0.52 (0.33-0.71) |
| Non-Chagas' disease patientsb | 50 | 47 (0.94)a | 3 | 0.51 (0.44-0.58) |
| Chagas' disease patients | 151 | 3 | 148 (0.98)c | 1.93 (1.82-2.04) |
The values in parentheses are percent specificity.
Healthy individuals and patients with leishmaniasis.
The value in parentheses is percent sensitivity.
Evaluation of Chagas' disease treatment.
To investigate whether the sera from benznidazole-treated patients with Chagas' disease displayed significant changes in reactivity to TS, we tested sera from 124 patients with chronic Chagas' disease before and after treatment. Two samples were collected after treatment at intervals of at least 1 year.
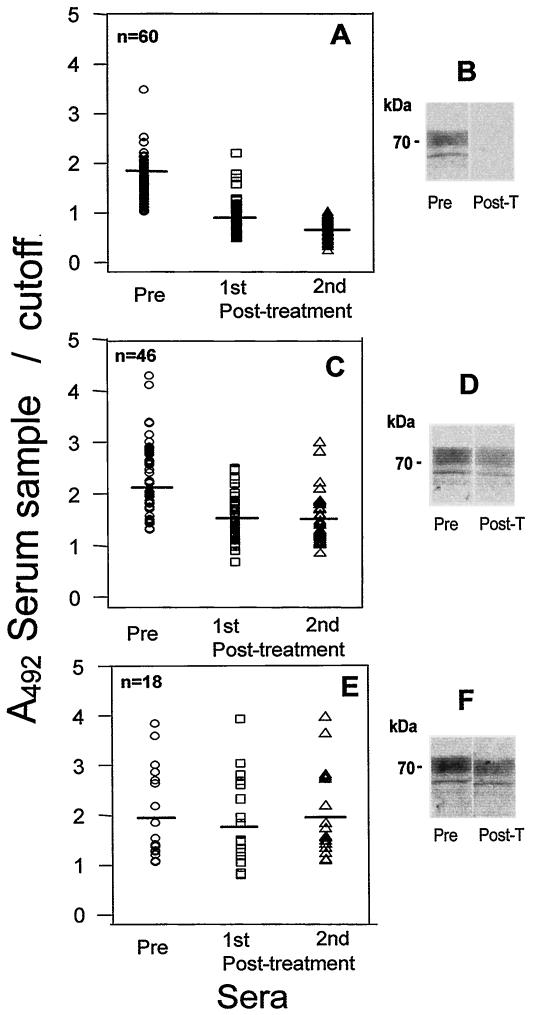
Three groups of individuals were identified on the basis of the ELISA results. The first group, consisting of 60 patients, had values greater than 1 (mean value, 1.71) before treatment, and the first posttreatment samples showed a mean value of 0.91. The second sample (collected at least 1 year later) showed a mean value of 0.72. In both cases, the posttreatment samples presented values below the cutoff (Fig. 2A). These results were confirmed by immunoblotting with each serum sample. As shown in Fig. 2B, a serum sample collected before treatment reacted well with TS, while a serum sample collected from the same individual after treatment failed to do so. Similar results were obtained when we tested sera from several other patients, and no reaction was detected with sera from leishmaniasis patients (data not shown). Most relevant was the fact that this group of individuals had negative blood culture test results and no clinical signs of infection.
FIG. 2.
Treatment follow-up. The reactivities of sera from chronic Chagas' disease patients with successful therapy (A), a decrease in titers after treatment (C), and resistance to treatment (E) determined before benznidazole treatment (○) and 1 year (□) and 2 years (▵) after benznidazole treatment are shown. The values are the ratio of the absorbance of each serum sample at 492 nm to the reaction cutoff. Values greater than 1.0 were considered reactive. The horizontal lines represent the arithmetic means. Immunoblots for serum samples from the three groups of patients before treatment (Pre) and after treatment (Post-T) are shown in panels B, D, and F, respectively.
The reactivities of the sera from the second group of patients (n = 46) are shown in Fig. 2C. The mean value for the serum samples collected before treatment was 2.24, and the mean values for samples collected 1 and 2 years after treatment decreased to 1.49 and 1.39, respectively. Because these values were above the mean for noninfected individuals, they were considered positive. As expected, serum samples collected after treatment were still reactive with TS by immunoblotting, but at lower intensities compared to those for the corresponding samples collected before treatment (Fig. 2D). Four of the 46 individuals had positive blood culture test results.
Patients from the third group (n = 18) were considered resistant to treatment and presented clear signs of infection, including positive blood cultures. The sera from these individuals showed the same reactivities before and after treatment. The mean values for samples collected before treatment and 1 and 2 years after treatment were 1.97, 1.86, and 1.97, respectively (Fig. 2E). This result was confirmed by immunoblotting, as shown in Fig. 2F.
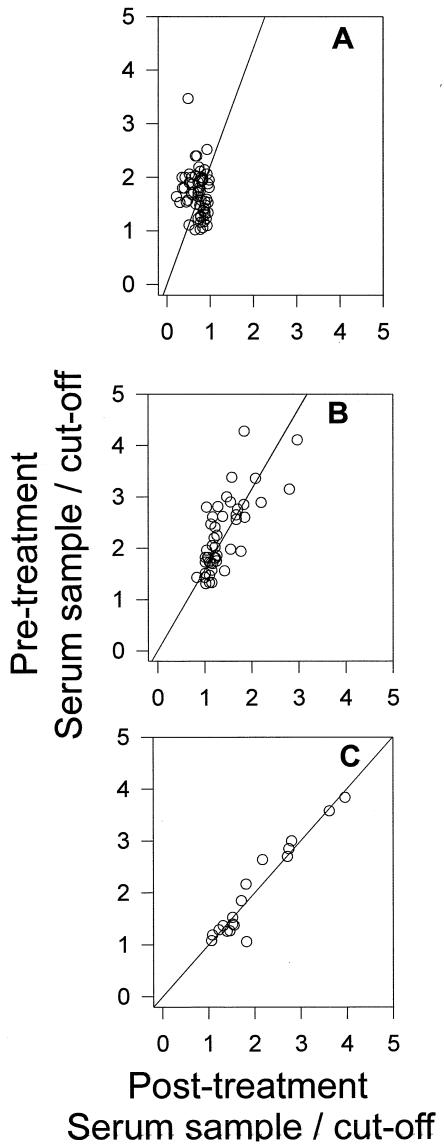
Figure 3 shows the data plotted as the distribution of the values for serum samples obtained from each group before and after treatment. The linear regression clearly indicates that the sera from the patients in the third group remained reactive to TS.
FIG. 3.
Distribution of reactivities of sera from each group of patients. Each point represents the reactivity of each serum sample before and after benznidazole treatment (second serum sample). (A) Chronic Chagas' disease patients with successful therapy; (B) chronic Chagas' disease patients with decreases in titers after treatment; (C) chronic Chagas' disease patients with resistance to treatment.
DISCUSSION
The aim of the present study was to assess the possibility of using recombinant TS for the diagnosis of Chagas' disease and the evaluation of treatment of Chagas' disease patients. We standardized a new ELISA to detect IgG antibodies against the catalytic domain of TS by using a purified recombinant protein. The population studied included adult patients with chronic Chagas' disease who had been infected more than three decades earlier and who were hemoculture positive. As controls we used apparently healthy individuals and patients with active visceral leishmaniasis. The diagnostic value was high compared to that of conventional serology for Chagas' disease, with a sensitivity of 0.98 and a specificity of 0.94. Individuals infected with any Leishmania sp. always show low, albeit detectable, titers for antibodies against T. cruzi antigens (18). In the present assay, no cross-reaction was observed with sera from patients with leishmaniasis. This observation is compatible with the knowledge that members of the genus Leishmania do no synthesize TS and confirms previous suggestions that anti-TS antibodies can be used to distinguish T. cruzi-infected individuals with other diseases, such as leishmaniasis (3).
More important, we have provided clear evidence that-anti-TS antibody levels decrease upon benznidazole treatment, as detected by ELISA with recombinant TS. We found a group of patients who showed reactivities below the cutoff levels 2 years after treatment and for whom no clinical symptoms or parasites were detectable by blood culture. This group was considered to have a distinct serological behavior after treatment. In contrast, two groups of patients presented reactivities above the cutoff after drug treatment. Posttherapy sera from one group, formed by 37% of the patients, exhibited positive results, but the values were lower than those obtained before treatment. This finding led us to assume that if treatment was unable to abolish all the parasites, it at least reduced the number of parasites in the circulation. Some of these patients still showed evidence of active infection. A second group of individuals corresponded to 14% of the patients and was considered to be resistant to treatment. Ten patients in this group had positive blood culture test results and no clinical improvement. They presented the same levels of anti-TS recognition before and after treatment.
Previous studies have shown that anti-TS antibodies are present in patients with active infection and that some of these antibodies inhibit the activity of the enzyme (14, 24). On the basis of this specific inhibition, the use of TS inhibition assays has been proposed for the monitoring of treatment (3, 16). In these studies the inhibitory antibodies seem to persist even when infection disappears, as evaluated by clinical and other immunological tests (15). In our case, the absence of a significant amount of antibodies distinguished the patients without clinical symptoms of infection. One explanation for this apparent contradiction is the fact that our method detected a different population of antibodies against TS, which may represent the majority of antibodies against the enzyme. These antibodies could possibly bind to the enzyme portions not involved in substrate binding. In addition, we used a solid-phase assay in which most of the accessible epitopes could be distinct from the substrate binding site. It would be interesting to compare the epitopes recognized by the different types of antibodies.
It has been accepted that the titers of protective IgG antibodies against trypomastigote antigens decrease following chemotherapy, when most of the parasites are eliminated (1, 7, 13). These antibodies were shown to react to parasite surface components (19), inducing complement-mediated lysis of trypomastigotes (11). Some are directed at proteins that induce complement resistance to the parasites (21); but some other trypomastigote antigens, such as mucins (2), proteins (7), and excreted antigens (29), have also been shown to detect a decrease in the levels of protective antibodies. In contrast, the levels of antibodies to epimastigote antigens are not dramatically changed after treatment. Such dissociation has been used as a criterion of cure in successfully treated patients (11).
In summary, the present data show that the catalytic domain of TS can also be used for the diagnosis and monitoring of Chagas' disease treatment, providing a simple methodology for monitoring the results of chemotherapy for Chagas' disease patients. After drug treatment the sera of some patients showed reduced reactivities, while the sera of other patients had more discrete changes in reactivity. Compared to other methods that use TS, the present one is simpler and does not depend on the measurement of TS activity, especially when several serum samples with serial dilutions should be used. The effective cure of the infection, however, requires negative results by clinical, serological, and parasitological tests after a long period of monitoring. Long-term clinical monitoring of the same patients is being conducted by one of us, and preliminary data suggest that benznidazole treatment is effective for most patients in the chronic phase of Chagas' disease.
Acknowledgments
We thank Rosangela Borges Reina, Laboratório de Parasitologia, Instituto Adolfo Lutz, for providing serum samples from patients with active visceral leishmaniasis.
REFERENCES
- 1.Almeida, I. C., D. T. Covas, L. M. Soussumi, and L. R. Travassos. 1993. A highly sensitive and specific chemiluminescent enzyme-linked immunosorbent assay for diagnosis of active Trypanosoma cruzi infection. Transfusion 37:850-857. [DOI] [PubMed] [Google Scholar]
- 2.Almeida, I. C., G. M. Krautz, A. U. Krettli, and L. R. Travassos. 1993. Glycoconjugates of Trypanosoma cruzi: a 74 kD antigen of trypomastigotes specifically reacts with lytic anti-α-galactosyl antibodies from patients with chronic Chagas disease. J. Clin. Lab. Anal. 7:307-316. [DOI] [PubMed] [Google Scholar]
- 3.Buchovsky, A. S., O. Campetella, G. Russomando, L. Franco, R. Oddone, N. Candia, A. Luquetti, S. M. Gonzalez Cappa, and M. S. Leguizamon. 2001. trans-Sialidase inhibition assay, a highly sensitive and specific diagnostic test for Chagas' disease. Clin. Diagn. Lab. Immunol. 8:187-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Camargo, M. E. 1966. Fluorescent antibody test for the serodiagnosis of American trypanosomiasis. Technical modification employing preserved culture forms of Trypanosoma cruzi in a slide test. Rev. Inst. Med. Trop. Sao Paulo 8:227-235. [PubMed] [Google Scholar]
- 5.Camargo, M. E., S. Hoshino, and G. R. Siqueira. 1973. Hemagglutination with preserved, sensitized cells, a practical test for routine serologic diagnosis of American trypanosomiasis. Rev. Inst. Med. Trop. Sao Paulo 15:81-85. [PubMed] [Google Scholar]
- 6.Costa, F., M. Ribeirão, V. L. Pereira-Chioccola, S. Schenkman, and M. M. Rodrigues. 1999. trans-Sialidase delivered as a naked DNA vaccine elicits an immunological response similar to a Trypanosoma cruzi infection. Braz. J. Med. Biol. Res. 32:235-239. [DOI] [PubMed] [Google Scholar]
- 7.Da Silveira, J. F., E. S. Umezawa, and A. O. Luquetti. 2001. Chagas disease: recombinant Trypanosoma cruzi antigens for serological diagnosis. Trends Parasitol. 17:286-291. [DOI] [PubMed] [Google Scholar]
- 8.Dias, J. C. P. 1992. Epidemiology of Chagas' disease, p. 49-80. In S. Wendel, Z. Brener, M. E. Camargo, and A. Rassi (ed.), Chagas’ disease (American trypanosomiase): its impact on transfusion and clinical medicine—1992. ISPT, São Paulo, Brazil.
- 9.Fragata Filho, A. A., M. A. da Silva, and E. Boainain. 1995. Etiologic treatment of acute and chronic Chagas' disease. Rev. Paul Med. 113:867-872. [DOI] [PubMed] [Google Scholar]
- 10.Frasch, A. C. 2000. Functional diversity in the trans-sialidase and mucin families in Trypanosoma cruzi. Parasitol. Today 16:282-286. [DOI] [PubMed] [Google Scholar]
- 11.Galvão, L. M., R. M. Nunes, J. R. Cançado, Z. Brener, and A. U. Krettli. 1993. Lytic antibody titre as a means of assessing cure after treatment of Chagas disease: a 10 years follow-up study. Trans. R. Soc. Trop. Med. Hyg. 87:220-223. [DOI] [PubMed] [Google Scholar]
- 12.Harlow, E., and D. Lane. 1988. Antibodies: a laboratory manual. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 13.Krettli, A. U., and L. Pontes de Carvalho. 1986. Binding of C3 fragments to the Trypanosoma cruzi surface in the absence of specific antibodies and without activation of the complement cascade. Clin. Exp. Immunol. 62:270-277. [PMC free article] [PubMed] [Google Scholar]
- 14.Leguizamon, M. S., O. Campetella, G. Russomando, M. Almiron, I. Guillen, S. M. Ganzalez Cappa, and A. C. Frasch. 1994. Antibodies inhibiting Trypanosoma cruzi trans-sialidase activity in sera from human infections. J. Infect. Dis. 170:1570-1574. [DOI] [PubMed] [Google Scholar]
- 15.Leguizamon, M. S., G. Russomando, A. Luquetti, A. Rassi, M. Almiron, S. M. Gonzalez-Cappa, A. C. Frasch, and O. Campetella. 1997. Long-lasting antibodies detected by a trans-sialidase inhibition assay of sera from parasite-free, serologically cured Chagasic patients. J. Infect. Dis. 175:1272-1275. [DOI] [PubMed] [Google Scholar]
- 16.Leguizamon, M. S., G. Russomando, D. A. Rojas, M. Samudio, M. Cabral, S. M. Gonzalez-Cappa, A. C. Frasch, and O. Campetella. 1998. Use of trans-sialidase inhibition assay in a population serologically negative for Trypanosoma cruzi but at a high risk of infection. Clin. Diagn. Lab. Immunol. 5:254-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levy, A. M., E. Bainain, and J. K. Kloetzel. 1996. In situ indirect fluorescent antibody: a new specific test to detect ongoing Chagasic infections. J. Clin. Lab. Anal. 10:98-103. [DOI] [PubMed] [Google Scholar]
- 18.Malchiodi, E. L., M. G. Chiaramonte, N. J. Taranto, N. W. Zwirner, and R. A. Margni. 1994. Cross-reactivity studies and differential serodiagnosis of human infections caused by Trypanosoma cruzi and Leishmania spp; use of immunoblotting and ELISA with a purified antigen (Ag163B6). Clin. Exp. Immunol. 97:417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martins, O. A., M. E. S. Pereira, J. F. Carvalho, J. R. Cancado, and Z. Brener. 1995. Flow cytometry, a new approach to detect anti-live trypomastigote antibodies and monitor the efficacy of specific treatment in human Chagas' disease. Clin. Diagn. Lab. Immunol. 2:569-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moncayo, A. 1992. Chagas' disease: epidemiology and prospects for interruption of transmission in the Americas. World Health Stat. Q. 45:276-279. [PubMed] [Google Scholar]
- 21.Norris, K. A. 1998. Stable transfection of Trypanosoma cruzi epimastigotes with the trypomastigote-specific complement regulatory protein cDNA confers complement resistance. Infect. Immun. 66:2460-2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pereira, V. L., A. M. Levy, and E. Boainain. 1989. Xenodiagnosis, hemoculture and the complement mediated lysis test, as criteria in selecting chronic chagasic patients for chemotherapy. Rev. Inst. Med. Trop. Sao Paulo 31:301-307. (In Portuguese.) [DOI] [PubMed] [Google Scholar]
- 23.Pereira-Chioccola, V. L., F. Costa, M. Ribeirão, I. S. Soares, F. Arena, S. Schenkman, and M. M. Rodrigues. 1999. Comparison of antibody and protective immune responses against Trypanosoma cruzi infection elicited by immunization with a parasite gene delivered as naked DNA or recombinant protein. Parasite Immunol. 21:103-110. [DOI] [PubMed] [Google Scholar]
- 24.Pereira-Chioccola, V. L., S. Schenkman, and J. Kloetzel. 1994. Sera from chronic Chagasic patients and animals infected with Trypanosoma cruzi inhibit trans-sialidase by recognizing its catalytic domain. Infect. Immun. 62:2973-2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ribeirão, M., V. L. Pereira-Chioccola, D. Eichinger, M. M. Rodrigues, and S. Schenkman. 1997. Temperature differences for trans-glycosylation and hydrolysis reaction reveal an acceptor binding site in the catalytic mechanism of Trypanosoma cruzi trans-sialidase. Glycobiology 7:1237-1246. [DOI] [PubMed] [Google Scholar]
- 26.Ribeirão, M., V. L. Pereira-Chioccola, L. Renia, A. A. Fragata-Filho, S. Schenkman, and M. M. Rodrigues. 2000. Chagasic patients develop a type 1 immune response to Trypanosoma cruzi trans-sialidase. Parasite Immunol. 22:49-53. [DOI] [PubMed] [Google Scholar]
- 27.Rodrigues, M. M., M. Ribeirão, V. L. Pereira-Chioccola, L. Renia, and F. Costa. 1999. Predominance of CD4 Th1 and CD8 TC1 cells revealed by characterization of the cellular immune response generated by immunization with a DNA vaccine containing a Trypanosoma cruzi gene. Infect. Immun. 67:3855-3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schenkman, S., D. Eichinger, M. E. A. Pereira, and V. Nussenzweig. 1994. Structural and functional properties of Trypanosoma cruzi trans-sialidase. Annu. Rev. Microbiol. 48:499-523. [DOI] [PubMed] [Google Scholar]
- 29.Umezawa, E. S., M. S. Nascimento, N. Kesper, Jr., J. R. Coura, J. Borges-Pereira, A. C. Junqueira, and M. E. Camargo. 1996. Immunoblot assay using excreted-secreted antigens of Trypanosoma cruzi in serodiagnosis of congenital, acute, and chronic Chagas' disease. J. Clin. Microbiol. 34:2143-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Umezawa, E. S., M. A. Shikanai-Yasuda, A. Gruber, V. L. Pereira-Chioccola, and B. Zingales. 1996. Trypanosoma cruzi defined antigens in the serological evaluation of an outbreak of acute Chagas' disease in Brazil (Catole do Rocha, Paraiba). Mem. Inst. Oswaldo Cruz 91:87-93. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. 1995. Chagas' disease: important advances in elimination of transmission in four countries in Latin America. WHO Feature 183:1-3. [Google Scholar]