Abstract
Purpose
To compare computer-assisted planimetry using the Discam system (Marcher Enterprises Ltd., Hereford, UK), confocal scanning laser ophthalmoscopy (CSLO), and stereoscopic disc photography with respect to optic nerve head (ONH) measurements and glaucoma status.
Design
Comparative, observational case series and interobserver variability study.
Methods
Three hundred eighty-six eyes of 233 consecutive subjects were imaged with the Discam, and a subset underwent ONH evaluation with CSLO (n = 297), stereoscopic photography (n = 233), or both. Subjects were classified into normal, glaucoma suspect, and glaucoma groups based on clinical findings of slit-lamp disc examination and visual field testing. Agreement of cup-to-disc ratio measurements among the three technologies was assessed by the intraclass correlation coefficient (ICC) and areas under the receiver operator characteristic (AROC) curves.
Main Outcome Measures
Cup-to-disc ratio as measured by Discam, CSLO, and stereography.
Results
Intraclass correlation coefficients calculated using the two-way random effects model for comparing Discam, CSLO, and stereography among cup-to-disc area ratio, vertical cup-to-disc ratio, and horizontal cup-to-disc ratio were 0.46 to 0.53. The ICC was higher for eyes with larger optic discs (0.51) than those with smaller ones (0.32). The ICC calculated using the fixed effects model for the Discam and CSLO comparison was 0.72. Areas under the receiver operator characteristic curves were 0.67 to 0.80 among the three technologies comparing normal with glaucomatous eyes. In general, there was no statistically significant difference between techniques with respect to sensitivity and specificity of glaucoma detection.
Conclusions
There is good agreement between ONH measurements obtained by Discam, CSLO, and stereography; however, the results are not interchangeable. Similar AROC curve values among all three techniques imply that the Discam, CSLO, and stereography perform equally for the determination of glaucoma status.
Identifying structural changes in the optic nerve head (ONH) is essential for detection of glaucoma. Previous studies have demonstrated that neuronal loss precedes any detectable visual field changes.1–3 Cup-to-disc ratio is commonly used in clinical settings to quantify neuronal loss, and it has been found to correlate with global visual field indices.4,5 This parameter relies considerably on observer experience and thus has not proven to be a consistent or reproducible means of ONH evaluation.6,7
Newer technologies, such as computer-assisted planimetry and confocal scanning laser ophthalmoscopy (CSLO), have allowed for more objective measurement of the ONH. These systems have the advantage of high agreement and repeatability among observers, and, theoretically, represent a better means of ONH evaluation.
A new digital stereoscopic optic disc camera, known as the Discam (Marcher Enterprises Ltd, Hereford, UK), is a computer-assisted planimetric system that has been found to have high interobserver and intraobserver agreement.8 The Discam system acquires sequential disc photographs in a semiautomatic fashion, and the operator is required to define the ONH and the cup edges to obtain quantitative parameters of the ONH.
The goals of this study were to compare Discam analysis of the ONH with scanning laser ophthalmoscopy and stereoscopic disc photography (stereography) and to evaluate the ability of these methods to detect glaucomatous changes.
Methods
Subjects
Two hundred thirty-three consecutive subjects were recruited from the glaucoma service at the New England Eye Center, Boston, Massachusetts, between January 2000 and December 2001. Informed consent was received from each subject before participation in our study in accordance with the Investigational Review Board of Tufts-New England Medical Center. Each subject underwent a complete ophthalmic examination, including visual acuity testing, intraocular pressure (IOP) measurement, predilated and postdilated biomicroscopy, indirect ophthalmoscopy, and visual field (VF) testing. All subjects underwent ONH evaluation with the Discam system as well as CSLO and/or stereoscopic ONH photography.
Subjects were classified into the following clinical criteria: normal, glaucoma suspect, and glaucoma. Normal eyes were defined as those with no family history of glaucoma in a first degree relative, no history or evidence of intraocular surgery, and no retinal pathologic features. Normal eyes also had a best corrected visual acuity of 20/40 or better, with refractive error between +3.00 and −6.00 diopters, IOP of 21 mmHg or lower, normal-appearing ONHs, and normal VF tests. Glaucoma suspects had no history or evidence of intraocular surgery, no evidence of retinal pathologic features, and normal VF test results. Glaucoma suspects also had IOPs between 22 and 30 mmHg and/or asymmetric cupping (difference in vertical cupping greater than 0.2 between eyes), large cupping, abnormal-appearing ONHs, or a family history of glaucoma in a first degree relative. Glaucomatous eyes were defined as those with abnormal VF test results with cupping of the ONH corresponding to VF loss, IOP of more than 35 mmHg despite a full VF in the presence of large ONH cupping, a nerve fiber layer defect on stereo biomicroscopy, or a combination thereof.
Subjects were excluded from the study if their fundus was not visible, if their media were opaque, or they were unwilling to participate in the study.
Visual Field Testing
All subjects underwent one of the following Humphrey VF testing protocols: Swedish Interactive Thresholding Algorithm (SITA) standard 24-2 perimetry, Short Wavelength Automated Perimetry (SWAP) full-threshold 24-2, or Frequency Doubling Technology (FDT) full-threshold N-30 perimetry (Carl Zeiss Meditech, Dublin, CA). On our service, subjects with no known VF damage routinely undergo testing by SWAP or FDT perimetry, and subjects with known VF defects are usually followed up with SITA testing. A reliable VF test was defined as one with fewer than 30% fixation losses or false-positive or false-negative responses. A VF defect on SITA or SWAP tests had a characteristic arcuate, Bjerrum, Seidel, paracentral scotoma, or nasal step, or a combination thereof, with clusters of three or more adjacent points depressed more than 5 dB or two adjacent points depressed more than 10 dB. A defect on FDT testing had any defect in the central five locations, two or more mild or moderate defects in the outer 12 regions, or one or more severe defects in the outer 12 regions. The mean deviation and pattern standard deviation were used for the analysis.
Discam
All subjects (n = 386) were photographed with the Discam, a digitized semiautomatic charge-coupled device camera. This device captures 20° × 20° ONH photographs. At least three images were taken for each eye, and the best-quality image of the set was used for analysis. Images were viewed through a stereoviewer, and freehand tracings of both the ONH and optic cup edges were drawn by a trained observer who was blinded to any clinical information. Tracings of the optic cup edge were made based on three-dimensional contours, not pallor, and the course of blood vessels at the cup edges. Blood vessels were included in the tracing of the optic cup if there was no underlying neuroretinal rim tissue. The following parameters, which were automatically calculated by the device, were used for this study: cup-to-disc area ratio (ACDR), vertical cup-to-disc ratio (VCDR), and horizontal cup-to-disc ratio (HCDR).
Confocal Scanning Laser Ophthalmoscopy
Two hundred ninety-seven eyes underwent imaging with the Heidelberg Retina Tomograph (HRT; software version 1.1S, Heidelberg Engineering, Heidelberg, Germany), a CSLO device. This device took a series of 32 consecutive two-dimensional sections of the ONH. Three good-quality 15° × 15° scans were obtained for each eye, and a mean topographic image was used for analysis. A trained technician drew the contour line along the ONH edge and the standard reference was used. Two of the calculated HRT parameters were used for this study: disc area and ACDR.
Stereoscopic Optic Nerve Head Photographs
Two hundred thirty-three eyes had simultaneous stereoscopic ONH photographs taken with the 3Dx Stereo Disc Camera (Nidek Corporation, Ltd., Gamagori, Japan). Two glaucoma specialists, who were masked to any clinical information, estimated both VCDR and HCDR to the nearest first decimal place from the stereoscopic photograph using a stereo slide viewer. The mean of the two observer’s estimations was used for analysis. If a difference of more than 0.2 was found between the two observers, a third observer assessed the photographs, and the mean of the three observer’s estimations was used for analysis.
Statistical Methods
Data were analyzed using SAS statistical software (SAS Institute, Inc., Cary, NC). A analysis of variance was used to compare the mean deviation and the pattern standard deviation across diagnoses for FDT and SITA. The random effect mixed model was used to control for the correlation between eyes within a given subject. The assumptions of normality and equal variance were met for the FDT model, but not for the SITA model. However, because nonparametric tests yielded the same results, the analysis of variance was presented for consistency.
Intraclass correlation coefficients (ICCs), as described by Shrout and Fleiss9 using the two-way random effects model were used to measure agreement. The measurement methods (i.e., Discam, HRT, and stereography) were considered to be a random subset of all possible measurement methods. The ICC for the Discam and HRT comparison was also calculated using the fixed effects model to compare our results with the method used for the analysis in previous studies. Scatter plots of the differences of two measurements against their average were also created to assess agreement among technologies, as described by Bland and Altman.10
Tertile groups based on absolute disc area were created for ACDR measurements between Discam and HRT to determine if optic disc size influenced agreement. Area under the receiver operator characteristic (AROC) curve analysis was performed to assess the ability of each method to detect glaucomatous changes with respect to the glaucoma status as determined by clinical diagnosis and VF defects.
Results
The mean VF global indices of the study population are presented in Table 1. The analysis of variance tests for overall difference among the three subject groups are also reported for each strategy with the exception of SWAP, in which only a limited number of normal subjects were available (n = 2).
Table 1.
Mean Values (±Standard Deviation) of Visual Field Indices for Normal, Glaucoma Suspect, and Glaucomatous Eyes
| Normal (n = 30) | Suspect (n = 165) | Glaucoma (n = 125) | Analysis of Variance Test | |
|---|---|---|---|---|
| SITA | ||||
| (n = 10) | (n = 81) | (n = 78) | ||
| MD | −0.39 (1.00) | −0.98 (1.74) | −4.80 (5.62) | < 0.0001 |
| PSD | 1.98 (0.81) | 2.06 (1.62) | 4.64 (3.72) | < 0.0001 |
| SWAP | ||||
| (n = 2) | (n = 25) | (n = 18) | ||
| MD | 0.21 (0.74) | −3.48 (4.09) | −1.35 (2.63) | * |
| PSD | 4.42 (1.87) | 3.08 (0.86) | 3.75 (1.23) | * |
| FDT | ||||
| (n = 18) | (n = 59) | (n = 29) | ||
| MD | −1.99 (2.34) | −1.76 (2.70) | −3.40 (3.69) | 0.26 |
| PSD | 4.27 (1.08) | 4.48 (1.60) | 5.67 (2.39) | 0.02 |
FDT = frequency doubling technology; MD = mean deviation; PSD = pattern standard deviation; SITA = Swedish interactive thresholding algorithm; SWAP = short wavelength automated perimetry.
Analysis of variance test not calculated because of limited number of normal subjects.
The ICCs between the two observers’ evaluations of stereoscopic ONH photographs for VCDR and HCDR were 0.66 and 0.67, respectively.
The mean ONH results obtained by the three technologies are reported in Table 2. Moderate agreement was found between the Discam and other technologies among all cup-to-disc ratio comparisons with a range of 0.46 to 0.53 (Table 3). In addition, the ICC for the Discam and HRT comparison using the fixed effects model was 0.72. Plots of the differences of the two cup-to-disc ratio measurements against the average of the two measurements on the Discam and HRT or stereography are shown in Figures 1, 2, and 3.
Table 2.
Mean Value, Standard Deviation, and Range of Cup-to-Disc Ratio Determined by Discam, Heidelberg Retina Tomograph, and Stereoscopic Disc Photography
| Mean (±Standard Deviation) | Range | |
|---|---|---|
| Discam (n = 386) | ||
| ACDR | 0.29 (0.09) | 0.10–0.67 |
| VCDR | 0.53 (0.09) | 0.33–0.84 |
| HCDR | 0.54 (0.10) | 0.32–0.82 |
| HRT (n = 297) | ||
| ACDR | 0.41 (0.15) | 0.04–0.86 |
| Stereo photos (n = 233) | ||
| VCDR | 0.64 (0.17) | 0.10–0.98 |
| HCDR | 0.63 (0.18) | 0.10–0.98 |
ACDR = cup-to-disc area ratio; HCDR = horizontal cup-to-disc ratio; HRT = Heidelberg Retina Tomograph; VCDR = vertical cup-to-disc ratio.
Table 3.
Mean Differences (Standard Deviation), 95% Confidence Intervals, 95% Limits of Agreement, and Intraclass Correlation Coefficients in Estimating Cup-to-Disc Ratio among Discam, Heidelberg Retina Tomograph, and Stereoscopic Disc Photography
| Mean Difference (±Standard Deviation) | 95% Confidence Interval | 95% Limits of Agreement | Intraclass Correlation Coefficient | |
|---|---|---|---|---|
| HRT, ACDR and Discam ACDR | 0.11 (0.11) | 0.10–0.12 | −0.11–0.33 | 0.49 |
| Stereo photo VCDR and Discam VCDR | 0.11 (0.13) | 0.09–0.13 | −0.15–0.37 | 0.46 |
| Stereo photo HCDR and Discam HCDR | 0.09 (0.13) | 0.07–0.11 | −0.17–0.35 | 0.53 |
ACDR = cup-to-disc area ratio; HCDR = horizontal cup-to-disc ratio; HRT = Heidelberg Retina Tomograph; VCDR = vertical cup-to-disc ratio.
Figure 1.
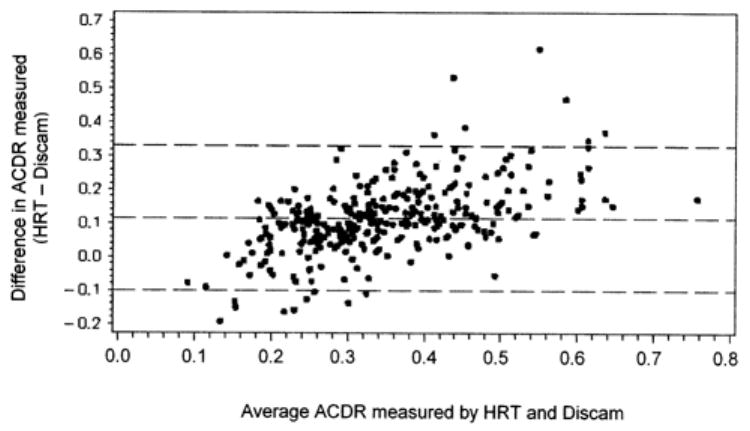
Scatter plot showing difference in cup-to-disc area ratio (ACDR) measured by the Heidelberg Retina Tomograph (HRT) and Discam against the average ACDR of the two measurements. Dashed lines represent mean difference and 95% limits of agreement.
Figure 2.
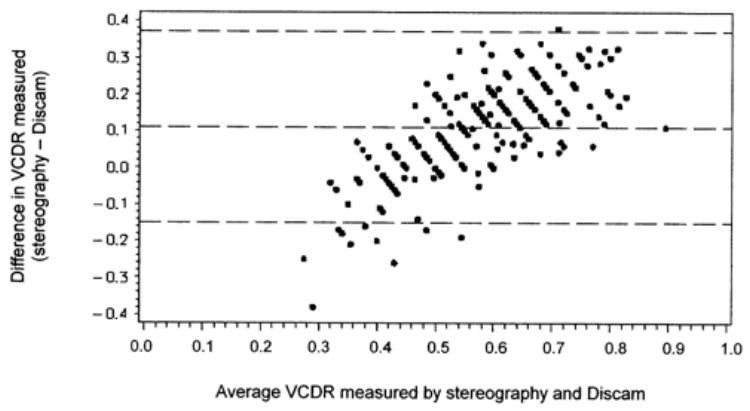
Scatter plot showing difference in vertical cup-to-disc ratio (VCDR) measured by stereoscopic disc photography and Discam against the average VCDR of the two measurements. Dashed lines represent mean difference and 95% limits of agreement.
Figure 3.
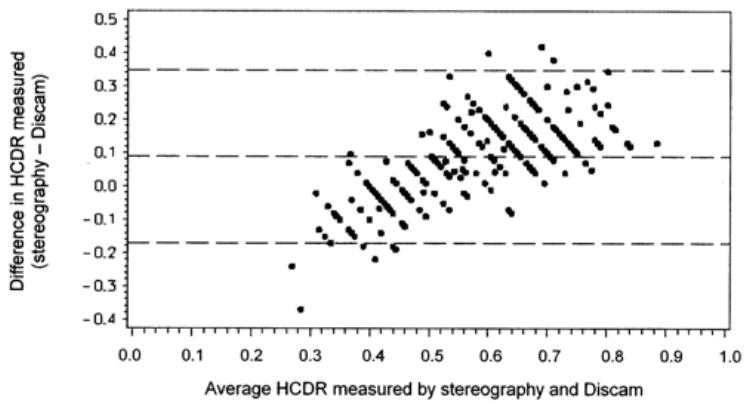
Scatter plot showing difference in horizontal cup-to-disc ratio (HCDR) measured by stereoscopic disc photography and Discam against the average HCDR of the two measurements. Dashed lines represent mean difference and 95% limits of agreement.
The Discam and HRT comparison was divided into tertiles based on ONH size, as determined by the HRT, to assess the influence of ONH size (Table 4). The best agreement of 0.51 was found in the medium-sized ONH, whereas for the larger ONH, the agreement was slightly lower (0.43).
Table 4.
Intraclass Correlation Coefficient in Estimating the Cup-to-Disc Area Ratio among Discam and The Heidelberg Retinal Tomograph Subdivided into Three Groups Based on Optic Disc Area as Determined by the The Heidelberg Retinal Tomograph
| Disc Area (mm2) | Intraclass Correlation Coefficient |
|---|---|
| 0.69–1.81 | 0.32 |
| 1.81–2.17 | 0.51 |
| 2.18–4.15 | 0.43 |
An AROC curve analysis was performed to evaluate the ability of each technology to detect glaucomatous ONH changes, based on the clinical classification (Table 5) or the presence of VF defects (Table 6). There was no statistically significant difference among Discam, HRT, and stereography with respect to sensitivity and specificity of glaucoma detection. A sample AROC curve of ACDR between normal and glaucomatous eyes for both Discam and HRT is shown in Figure 4.
Table 5.
Area under Receiver Operating Characteristic Curve Values with 95% Confidence Intervals among Normal, Glaucoma Suspect, and Glaucomatous Eyes
| Normal versus Glaucoma | Normal versus Suspect | Suspect versus Glaucoma | |
|---|---|---|---|
| Discam | |||
| ACDR | 0.70 (0.61–0.80) | 0.64 (0.53–0.75) | 0.59 (0.53–0.66) |
| VCDR | 0.73 (0.64–0.82) | 0.65 (0.54–0.75) | 0.62 (0.56–0.68) |
| HCDR | 0.68 (0.58–0.77) | 0.64 (0.53–0.75) | 0.55 (0.49–0.62) |
| HRT | |||
| ACDR | 0.67 (0.54–0.79) | 0.60 (0.47–0.73) | 0.60 (0.52–0.67) |
| Stereo photos | |||
| VCDR | 0.80 (0.70–0.90) | 0.71 (0.60–0.81) | 0.61 (0.53–0.69) |
| HCDR | 0.76 (0.66–0.87) | 0.70 (0.59–0.80) | 0.57 (0.49–0.65) |
| Visual field | |||
| MD (SITA) | 0.83 (0.73–0.93) | 0.60 (0.44–0.77) | 0.75 (0.67–0.83) |
| PSD (SITA) | 0.78 (0.64–0.92) | 0.42 (0.24–0.60) | 0.79 (0.73–0.86) |
| MD (SWAP) | * | * | 0.64 (0.48–0.81) |
| PSD (SWAP) | * | * | 0.67 (0.50–0.83) |
| MD (FDT) | 0.62 (0.46–0.80) | 0.49 (0.34–0.65) | 0.62 (0.49–0.75) |
| PSD (FDT) | 0.69 (0.53–0.84) | 0.49 (0.34–0.65) | 0.67 (0.54–0.79) |
ACDR = cup-to-disc area ratio; FDT = frequency doubling technology; HCDR = horizontal cup-to-disc ratio; HRT = Heidelberg Retina Tomograph; MD = mean deviation; PSD = pattern standard deviation; SITA = Swedish interactive thresholding algorithm; SWAP = short wavelength automated perimetry; VCDR = vertical cup-to-disc ratio.
The area under receiver operating characteristic curve not calculated because of a limited number of normal subjects.
Table 6.
Area under Receiver Operating Characteristic Curve Values with 95% Confidence Intervals among Visual Field Defect Comparison Groups
| Visual Field Defect (Swedish Interactive Thresholding Algorithm) | Visual Field Defect (Short Wavelength Automated Perimetry) | Visual Field Defect (Frequency Doubling Technology) | |
|---|---|---|---|
| Discam | |||
| ACDR | 0.70 (0.61–0.79) | 0.71 (0.49–0.93) | 0.53 (0.35–0.70) |
| VCDR | 0.73 (0.64–0.81) | 0.73 (0.57–0.90) | 0.51 (0.34–0.69) |
| HCDR | 0.65 (0.56–0.74) | 0.66 (0.41–0.91) | 0.56 (0.39–0.73) |
| HRT | |||
| ACDR | 0.72 (0.62–0.83) | 0.63 (0.12–1.00) | 0.66 (0.52–0.79) |
| Stereo photos | |||
| VCDR | 0.71 (0.61–0.81) | 0.64 (0.38–0.90) | 0.67 (0.42–0.91) |
| HCDR | 0.65 (0.54–0.76) | 0.64 (0.38–0.90) | 0.61 (0.31–0.90) |
| Visual field | |||
| MD (SITA) | 0.84 (0.76–0.91) | — | — |
| PSD (SITA) | 0.90 (0.85–0.95) | — | — |
| MD (SWAP) | — | 0.49 (0.28–0.70) | — |
| PSD (SWAP) | — | 0.83 (0.70–0.96) | — |
| MD (FDT) | — | — | 0.76 (0.64–0.89) |
| PSD (FDT) | — | — | 0.82 (0.70–0.94) |
ACDR = cup-to-disc area ratio; FDT = frequency doubling technology; HCDR = horizontal cup-to-disc ratio; HRT = Heidelberg Retina Tomograph; MD = mean deviation; PSD = pattern standard deviation; SITA = Swedish interactive thresholding algorithm; SWAP = short wavelength automated perimetry; VCDR = vertical cup-to-disc ratio.
Figure 4.
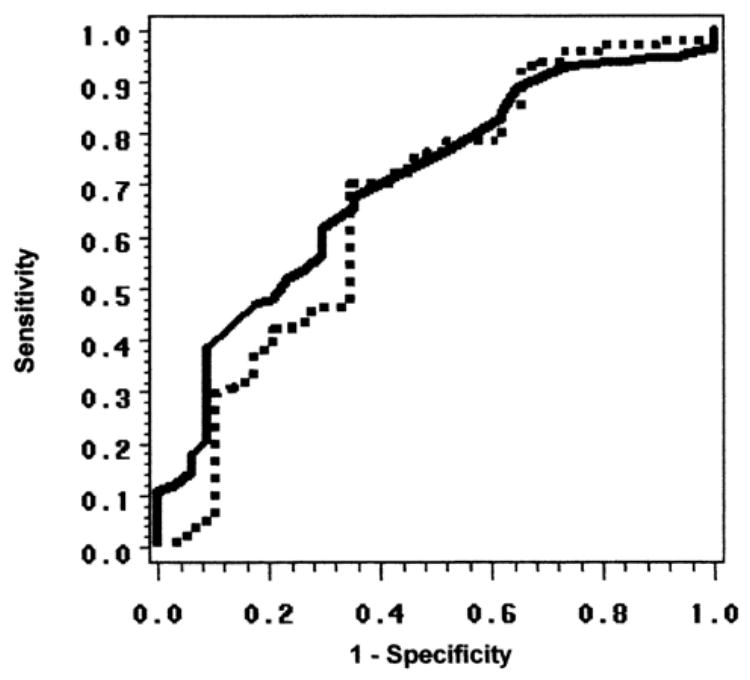
Receiver operator characteristic (ROC) curve for cup-to-disc area ratio (ACDR) measured by Discam (continuous line) and the Heidelberg Retina Tomograph (HRT) for distinguishing between glaucoma and normal subjects; areas under the ROC curves (AROCs) are 0.70 and 0.67, respectively. These curves are shown as examples of ROC curves summarized by AROCs in Tables 5 and 6.
Discussion
Identifying ONH changes is crucial for the detection and follow-up of glaucoma patients. Few methods are currently available to assess ONH changes. Three of the most common methods have been examined in this study: stereoscopic ONH photography, CSLO, and computer-assisted planimetry using a digital camera. The incorporation of a digital camera into an imaging system provides a significant advantage over conventional photography because of the possibility of obtaining real-time planimetry.
The study group included normal subjects and subjects with early-stage VF abnormalities (Table 1). The heterogeneity of the glaucoma suspect group is reflected in the VF indices that are comparable with those of the normal group, with the exception of subjects who underwent SWAP testing. Also of note is the SWAP and FDT bias toward subjects with normal VFs, which can be attributed to our service’s protocol for ordering VF tests.
The ONH measurements obtained by the Discam were found to be smaller than those obtained with the other methods (Table 2). The large difference in the ACDR between Discam and HRT reflects the detrimental difference in the location of the optic cup edge. The optic cup edge is defined by the HRT at the height of 50 μm posterior to the mean retinal surface along a 6° sector in the temporal inferior contour line. The Discam uses definitions of the optic cup rim that are closer to those used in the clinical assessment of stereoscopic ONH photographs.
The agreement between the two observers’ evaluations of stereoscopic ONH photographs was found to be good (ICC, 0.66 vertical, 0.67 horizontal). Our interobserver agreement is similar to those reported in previous studies.7,11,12
In our study, agreement between the Discam and HRT measurements of ACDR was good. The ICC was found to be 0.49, and the mean difference was 0.11 (±0.11), indicating that the Discam systematically underestimates ACDR when compared with the HRT. When the ICC was calculated for tertiles based on disc area, agreement was significantly lower for eyes with smaller optic discs. Our fixed effect ICC calculation (0.72) agreed favorably with that of Sung et al,13 who found similar ICCs (0.53 and 0.67) when comparing the two systems. Previous studies that have evaluated agreement between HRT and other semiautomated planimetric devices have reported similar ICCs ranging from 0.57 to 0.65 and mean differences of −0.07 to 0.11, despite these technologies using slightly different techniques for observer identification of the optic disc and cup rims.12,14,15
Past studies comparing planimetry with the HRT have noted several reasons for differences among these technologies. Jonas et al16 initially attributed this difference to the algorithm by which the HRT evaluates the optic cup rim, in which retinal vessels can be included falsely as neuroretinal rim tissue because of the system’s definition of the standard reference plane. By planimetric definition, retinal vessels are only included in the neuroretinal rim when there is underlying tissue. This discrepancy becomes more apparent as the amount of neuroretinal rim tissue decreases throughout the progression of glaucoma, and thus will lead to progressive overestimations of ACDR by the HRT.
The Discam and subjective assessment of disc photographs showed an agreement of 0.46 and 0.53 for VCDR and HCDR, respectively, and underestimated stereography by 0.11 and 0.09, respectively. Previous studies that have compared semiautomated planimetry with stereography have found ICCs ranging from 0.45 to 0.63 and mean differences ranging from 0.10 to 0.14.11,15 Varma et al11 gave an explanation that clinicians often use nontopographic clues, such as pallor, to estimate cup-to-disc ratio by stereography, where as the semiautomated device will adhere only to topographic data. Furthermore, semiautomated systems may have problems identifying features on ONHs with insufficient contrasting.
Surprisingly, the Discam did not correlate with stereoscopic assessment as well as expected. The Discam software was designed to provide estimations of VCDR and HCDR by measuring the longest vertical and horizontal lines from observer tracings of the optic disc and optic cup as they appear on the screen. In theory, a clinician would follow the same algorithm when evaluating stereoscopic ONH photographs. We attributed differences between the Discam and stereography to two reasons. Delineation of the optic disc rim and the peripapillary region, as well as the optic cup rim and the neuroretinal rim tissue (especially on images with marked temporal slope flattening), was sometimes difficult on the Discam’s images. Variability in stereo angle among eyes may have also contributed to differences as each fundus was imaged by the different systems.
The highest AROC for discriminating between glaucoma and the other clinically defined groups was VF global indices (Table 5). These results are biased toward VF indices because our clinical classification of participants included the VF findings. The definition of both the normal and glaucoma suspects required the presence of normal VF test results, and therefore the discrimination between these groups based on VF indices is limited, as reflected by lower AROC.
Among the three methods for evaluating the ONH, stereoscopic disc photography was found to have the highest AROC, although the differences among all three methods were not statistically significant. We attributed higher values obtained by stereography to the bias of clinical examination in the definition of disease, as well as to the ability of the observer to take into account several physical findings (i.e., nerve fiber layer defect, minute disc hemorrhage) that could not be fully appreciated with the other methods. The AROC for the ACDR was found to be similar for Discam and HRT. One should remember, however, that the HRT provided numerous stereometric ONH parameters, and the combination of these parameters has been shown to improve sensitivity and specificity of detecting glaucomatous changes.17,18
In conclusion, we found good agreement between the ONH measurements obtained by the Discam, HRT, and stereoscopic ONH photography. However, the results of the three methods were not interchangeable. Similar AROCs were found for distinguishing between glaucoma and non-glaucoma subjects among the three methods. These results imply the usefulness of the Discam system as a simple method for ONH analysis. Future prospective studies are needed to evaluate the ability of the Discam to assess longitudinal glaucomatous change.
Acknowledgments
Supported in part by the National Eye Institute, Bethesda, Maryland (grant nos.: R01-EY13178, R01-EY11289, and P30-EY13078).
Footnotes
Presented in part at the American Academy of Ophthalmology annual meeting, Orlando, Florida, October 2002.
References
- 1.Quigley HA, Dunkelberger GR, Green WR. Chronic human glaucoma causing selectively greater loss of large optic nerve fibers. Ophthalmology. 1988;95:357–63. doi: 10.1016/s0161-6420(88)33176-3. [DOI] [PubMed] [Google Scholar]
- 2.Sommer A, Katz J, Quigley HA, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991;109:77–83. doi: 10.1001/archopht.1991.01080010079037. [DOI] [PubMed] [Google Scholar]
- 3.Zeyen TG, Caprioli J. Progression of disc and field damage in early glaucoma. Arch Ophthalmol. 1993;111:62–5. doi: 10.1001/archopht.1993.01090010066028. [DOI] [PubMed] [Google Scholar]
- 4.Airaksinen PJ, Drance SM, Douglas GR, et al. Neuroretinal rim areas and visual field indices in glaucoma. Am J Ophthalmol. 1985;99:107–10. doi: 10.1016/0002-9394(85)90216-8. [DOI] [PubMed] [Google Scholar]
- 5.Caprioli J, Miller JM. Correlation of structure and function in glaucoma. Quantitative measurements of disc and field. Ophthalmology. 1988;95:723–7. doi: 10.1016/s0161-6420(88)33116-7. [DOI] [PubMed] [Google Scholar]
- 6.Lichter PR. Variability of expert observers in evaluating the optic disc. Trans Am Ophthalmol Soc. 1976;74:532–72. [PMC free article] [PubMed] [Google Scholar]
- 7.Tielsch JM, Katz J, Quigley HA, et al. Intraobserver and interobserver agreement in measurements of optic disc characteristics. Ophthalmology. 1988;95:350–6. doi: 10.1016/s0161-6420(88)33177-5. [DOI] [PubMed] [Google Scholar]
- 8.Shuttleworth GN, Khong CH, Diamond JP. A new digital optic disc stereo camera: intraobserver and interobserver repeatability of optic disc measurements. Br J Ophthalmol. 2000;84:403–7. doi: 10.1136/bjo.84.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 10.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 11.Varma R, Spaeth GL, Steinmann WC, et al. Agreement between clinicians and an image analyzer in estimating cup-to-disc ratios. Arch Ophthalmol. 1989;107:526–9. doi: 10.1001/archopht.1989.01070010540027. [DOI] [PubMed] [Google Scholar]
- 12.Hatch WV, Trope GE, Buys YM, et al. Agreement in assessing glaucomatous discs in a clinical teaching setting with stereoscopic disc photographs, planimetry, and laser scanning tomography. J Glaucoma. 1999;8:99–104. [PubMed] [Google Scholar]
- 13.Sung VC, Bhan A, Vernon SA. Agreement in assessing optic discs with a digital stereoscopic optic disc camera (Discam) and Heidelberg retina tomograph. Br J Ophthalmol. 2002;86:196–202. doi: 10.1136/bjo.86.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azuara-Blanco A, Spaeth GL, Nicholl J, et al. Comparison between laser scanning tomography and computerised image analysis of the optic disc. Br J Ophthalmol. 1999;83:295–8. doi: 10.1136/bjo.83.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ikram MK, Borger PH, Assink JJM, et al. Comparing ophthalmoscopy, slide viewing, and semiautomated systems in optic disc morphometry. Ophthalmology. 2002;109:486–93. doi: 10.1016/s0161-6420(01)00983-6. [DOI] [PubMed] [Google Scholar]
- 16.Jonas JB, Mardin CY, Grundler AE. Comparison of measurements of neuroretinal rim area between confocal laser scanning tomography and planimetry of photographs. Br J Ophthalmol. 1998;82:362–6. doi: 10.1136/bjo.82.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mikelberg FS, Parfitt CM, Swindale NV, et al. Ability of the Heidelberg Retina Tomograph to detect early glaucomatous visual field loss. J Glaucoma. 1995;4:242–7. [PubMed] [Google Scholar]
- 18.Wollstein G, Garway-Heath DF, Hitchings RA. Identification of early glaucoma cases with the scanning laser ophthalmoscope. Ophthalmology. 1998;105:1557–63. doi: 10.1016/S0161-6420(98)98047-2. [DOI] [PubMed] [Google Scholar]


