Abstract
Purpose
To assess changes in retinal nerve fiber layer (NFL) thickness in glaucoma patients after filtration surgery by using optical coherence tomography (OCT).
Design
Retrospective observational case series.
Participants
Thirty-eight eyes of 31 glaucoma patients who underwent trabeculectomy or a combined procedure of cataract extraction and trabeculectomy were evaluated retrospectively.
Methods
Eyes were imaged with OCT before surgery (1 week to 6 months before surgery; mean ± standard deviation [SD], 71.3 ± 61.2 days) and after surgery (6–12 months after surgery; 247.2 ± 63.5 days) to measure peripapillary NFL thickness.
Main Outcome Measures
Changes in mean and segmental NFL thickness with respect to age, postoperative change in intraocular pressure (IOP), preoperative visual field test global indices, and change in visual field global indices.
Results
A significant increase in the overall mean NFL thickness was present after surgery (P < 0.0001). Segmental analysis found a significant increase in NFL thickness in the nasal, superior, and temporal quadrants. IOP decreased after surgery from 22.0 ± 6.4 mmHg to 11.4 ± 4.7 mmHg (mean ± SD). Twenty-eight (73.7%) of 38 eyes had an IOP reduction >30%. The mean NFL thickness increase (0.5-μm/mmHg decrease of IOP) was significantly correlated with the IOP reduction (r = −0.41; P = 0.03). No correlation was found between NFL thickness changes and age, preoperative visual field global indices, or change in visual field global indices.
Conclusions
A significant increase of the mean NFL thickness, which was related to IOP reduction, was detected after glaucoma filtration surgery.
Reversal of glaucomatous damage to the optic nerve head (ONH) and the retinal nerve fiber layer (NFL) after intraocular pressure (IOP)-decreasing treatments has been documented in congenital and infantile glaucoma and in chronic open-angle glaucoma in adults.1–10 Studies investigating reversal of ONH cupping in experimental models and in human subjects after IOP reduction by medical and surgical treatments have been performed by evaluating stereoscopic disc photographs, computer-assisted planimetry, ONH analysis, and confocal scanning laser ophthalmoscopy (CSLO).3–11 Changes have been documented in the optic disc appearance and in stereoscopic parameters, such as neuroretinal rim area and cup volume. However, the effect of IOP reduction on peripapillary NFL is still unclear. Some reports have suggested a nonsignificant change in retinal cross-sectional area with a trend of increase with IOP reduction,6,7 whereas others have shown a significant increase of mean retinal height at the optic disc margin9,11 with CSLO.
In this study, we retrospectively assessed changes in NFL thickness after filtration surgery by using optical coherence tomography (OCT), which is a noninvasive and reproducible technique that permits high-resolution cross-sectional imaging of the retina.12,13 Previous studies assessing the retinal and macular thickness changes as determined by OCT after cataract extraction surgery did not find any significant change.14,15 Assuming that NFL thickness also does not change after cataract surgery, we combined the data obtained from trabeculectomy or combined cataract extraction and trabeculectomy groups for this study.
Materials and Methods
Subjects enrolled in the study were consecutive glaucoma patients who underwent trabeculectomy or combined surgery of phacoemulsification and trabeculectomy at the New England Eye Center, Boston, Massachusetts, from November 1994 to October 1999. Informed consent approved by the New England Medical Center Human Investigation Review Committee was signed by all patients. All patients were scheduled for surgery when IOP exceeded target pressure and/or when visual field (VF) defect and glaucomatous optic nerve damage showed progression despite maximum-tolerated medical therapy. All operations were performed by one surgeon (JSS), who used a standard surgical procedure. Patients were eligible for this study if they had good-quality OCT images within 6 months before surgery and 6 to 12 months after surgery. All patients had a full ophthalmologic examination, including IOP measurement with Goldman applanation tonometry, on the same day of the OCT imaging. Patients who had retinal pathology not attributed to glaucoma or the surgical procedure that they underwent—such as diabetic retinopathy, age-related macular degeneration, or cystoid macular edema—were excluded from the study.
VF Testing
All patients had VF testing with either Humphrey 24-2 full-threshold or Swedish interactive thresholding algorithm standard perimetry. A reliable VF was considered as one with <30% fixation losses, false-positive responses, or false-negative responses. The mean deviation (MD) and pattern standard deviation (PSD) were used for the analysis.
OCT Scanning
Cross-sectional imaging of peripapillary NFL was performed with our prototype OCT system, which has been described previously.12,16–18 OCT is the optical equivalent of ultrasonography for high-resolution measurements and cross-sectional imaging of the human retina and NFL. Because of the different optical properties of the various retinal layers, OCT is able to measure NFL thickness in a noninvasive and noncontact manner. The OCT system used in this study acquired a typical 3-mm-deep, 100-pixel-wide image in <2.5 seconds. The axial resolution of the OCT system was experimentally determined to be 14 μm in air and 10 μm in the eye. After pupil dilation with 1% tropicamide and 2.5% phenylephrine hydrochloride, each eye had circular scans around the optic disc with a diameter of 3.4 mm. Good-quality OCT scans were defined as scans with a signal–noise ratio >40 dB and <15% consecutive and/or <20% additive points with obvious misalignment of the surface or zero values. The average of three qualified circular scans was used to calculate the overall mean and quadrantic NFL thickness.
Statistical Analysis
Paired t tests were used to analyze NFL thickness differences on an individual eye basis and to compare parameters before and after surgery. Pearson’s correlation was used to evaluate the associations between parameters. We used mixed models with patient as a random effect to obtain the P values for correlation and used t tests to adjust for the correlation between eyes of a given patient. All analyses were performed with SAS software (version 8.2; SAS Institute Inc., Cary, NC). P values <0.05 were considered to be statistically significant.
Results
Thirty-eight eyes of 31 patients were qualified for this study; 18 eyes underwent trabeculectomy with intraoperative application of mitomycin C or 5-fluorouracil, and 20 eyes underwent combined phacoemulsification and trabeculectomy with mitomycin C. Patient characteristics are presented in Table 1. Presurgery visual acuity was 20/40 or better in 27 (71.1%) eyes and worse than 20/40 in 11 (28.9%) eyes. Postsurgery visual acuity was 20/40 or better in 36 (94.7%) eyes and worse than 20/40 in 2 (5.3%) eyes. Preoperative OCT images of peripapillary NFL were obtained a mean ± standard deviation (SD) of 71.3 ± 61.2 days (range, 6–179 days) before surgery. Postoperative images were obtained a mean ± SD of 247.2 ± 63.5 days (range, 183–365 days) after surgery. IOP change is presented in Table 2. Twenty-eight (73.7%) of the 38 eyes had an IOP reduction of >30%.
Table 1.
Patient Characteristics
| Age, yrs (mean ± SD) | 60.5 ± 18.4 |
| Race | |
| White | 24 |
| Black | 4 |
| Other | 3 |
| Gender (male/female) | 12/19 |
| Diagnosis | |
| Primary open-angle glaucoma | 16 |
| Juvenile open-angle glaucoma | 5 |
| Normal tension glaucoma | 3 |
| Pseudoexfoliative glaucoma | 3 |
| Others | 4 |
SD = standard deviation.
Table 2.
IOP Measurements before and after Filtration Surgery
| Variable | No. of Eyes | Preoperative IOP, mmHg (mean ± SD) | Postoperative IOP, mmHg (mean ± SD) |
|---|---|---|---|
| Overall | 38 | 22.0 ± 6.4 | 11.4 ± 4.7 |
| Trabeculectomy group | 18 | 23.6 ± 7.5 | 9.6 ± 3.5 |
| Combined surgery group | 20 | 20.5 ± 5.0 | 13.0 ± 5.1 |
IOP = intraocular pressure; SD = standard deviation.
Both preoperative and postoperative reliable VF tests were available for 30 of the 38 eyes participating in the study. To avoid the effect of cataract removal on the VF test, we analyzed the data in patients who had only trabeculectomy (15 eyes). Mean preoperative MD ± SD and PSD ± SD were −11.3 ± 9.2 dB and 8.2 ± 4.2 dB, respectively. Mean postoperative MD and PSD were −10.6 ± 8.1 dB and 7.8 ± 4.5 dB, respectively. These differences were not statistically significant (P = 0.43 and P = 0.34, respectively).
Table 3 summarizes the mean peripapillary NFL thickness as measured by the OCT for the entire study group. A significant increase in the NFL thickness was found for the overall measurement and in all quadrants except the inferior quadrant. The NFL thickness change (mean ± SD) was 8.9 ± 10.3 μm for overall NFL (range, −12.7 to 36.5 μm; median, 9.9 μm; P = < 0.0001). We observed a mean overall NFL thickness increase in 31 (81.6%) of 38 eyes (mean increase, 12.6 ± 7.1 μm). In segmental analysis, there was an increase of NFL thickness in the superior quadrant of 25 (65.8%) eyes (mean, 16.7 ± 11.8 μm), in the nasal quadrant of 30 (78.9%) eyes (mean, 24.5 ± 17.2 μm), in the inferior quadrant of 21 (55.3%) eyes (mean, 20.3 ± 14.4 μm), and in the temporal quadrant of 27 (71.1%) eyes (mean, 12.7 ± 10.8 μm).
Table 3.
Mean Peripapillary NFL Thickness as Measured by OCT
| Variable | Preoperative NFL, μm (mean ± SD) | Postoperative NFL, μm (mean ± SD) | Mean Difference, μm (mean ± SD) | P Value |
|---|---|---|---|---|
| Overall | 72.8 ± 20.5 | 81.7 ± 21.1 | 8.9 ± 10.3 | <0.0001 |
| Superior | 87.9 ± 26.7 | 95.8 ± 25.4 | 7.9 ± 18.2 | 0.02 |
| Nasal | 55.3 ± 25.3 | 72.0 ± 28.7 | 16.7 ± 22.0 | <0.0001 |
| Inferior | 85.9 ± 33.5 | 92.0 ± 36.5 | 6.1 ± 20.2 | 0.07 |
| Temporal | 61.0 ± 23.0 | 66.6 ± 18.5 | 5.5 ± 15.4 | 0.03 |
NFL = nerve fiber layer; OCT = optical coherence tomography; SD = standard deviation.
To evaluate the relationship between preoperative glaucomatous damage and postoperative thickness change, we arbitrarily divided the eyes into three equal groups on the basis of the preoperative NFL thickness and compared the 1/3 group with the lowest thickness values with the 2/3 group with higher values for overall circumpapillary and segmental NFL thickness changes. There was no significant difference of postoperative NFL thickness changes between these groups except for the temporal quadrant. In that quadrant, the NFL thickness increase was significantly higher in the first group (with the lowest preoperative thickness values; P = 0.02).
Tables 4 and 5 summarize the mean NFL thickness measurements after dividing the patients into two groups on the basis of surgical procedure.
Table 4.
Mean Peripapillary NFL Thickness OCT Measurements in the Combined Surgery Group
| Variable | Preoperative NFL, μm (mean ± SD) | Postoperative NFL, μm (mean ± SD) | Mean Difference, μm (mean ± SD) | P Value |
|---|---|---|---|---|
| Overall | 72.0 ± 24.1 | 79.1 ± 22.4 | 7.1 ± 7.2 | <0.0004 |
| Superior | 85.6 ± 26.4 | 95.9 ± 25.5 | 10.3 ± 12.8 | 0.003 |
| Nasal | 54.1 ± 27.4 | 65.1 ± 29.3 | 11.0 ± 15.0 | 0.01 |
| Inferior | 84.7 ± 37.6 | 90.3 ± 37.7 | 5.6 ± 21.2 | 0.26 |
| Temporal | 62.3 ± 25.8 | 64.5 ± 19.0 | 2.1 ± 12.8 | 0.33 |
NFL = nerve fiber layer; OCT = optical coherence tomography; SD = standard deviation.
Table 5.
Mean Peripapillary NFL Thickness OCT Measurements in the Trabeculectomy Group
| Variable | Preoperative NFL, μm (mean ± SD) | Postoperative NFL, μm (mean ± SD) | Mean Difference, μm (mean ± SD) | P Value |
|---|---|---|---|---|
| Overall | 73.7 ± 16.3 | 84.6 ± 19.7 | 10.9 ± 12.8 | 0.004 |
| Superior | 90.4 ± 27.5 | 95.7 ± 26.0 | 5.3 ± 22.9 | 0.47 |
| Nasal | 56.6 ± 23.3 | 79.7 ± 26.7 | 23.1 ± 26.9 | 0.01 |
| Inferior | 87.3 ± 29.3 | 93.9 ± 36.2 | 6.6 ± 19.6 | 0.18 |
| Temporal | 59.6 ± 20.0 | 68.9 ± 18.3 | 9.3 ± 17.4 | 0.04 |
NFL = nerve fiber layer; OCT = optical coherence tomography; SD = standard deviation.
The correlation between the NFL thickness changes and the following factors are summarized in Table 6: age, IOP change (mmHg), percentage of change in IOP (in overall group), preoperative VF indices, and change in VF indices before and after surgery (only in eyes after trabeculectomy). The only significant correlations were found with the IOP change (r = −0.41; P = 0.03; Fig 1) and the percentage of IOP change (r = −0.49; P = 0.02; Fig 2). In the quadrant analysis of overall group, the only significant correlation between NFL thickness change and IOP change occurred in the inferior quadrant (r = −0.38; P = 0.001). Using linear regression, we found that for each IOP decrease of 1 mmHg after surgery, the overall mean NFL was thicker by 0.5 μm.
Table 6.
Pearson’s Correlation between Change in Mean NFL Thickness and Age, IOP, and Visual Field Parameters
| Factor | r | P Value |
|---|---|---|
| Age* | −0.01 | 0.94 |
| IOP change (mmHg)* | −0.41 | 0.03 |
| IOP change (%)* | −0.49 | 0.02 |
| Preoperative VF-MD† | 0.35 | 0.39 |
| Preoperative VF-PSD† | −0.25 | 0.36 |
| Change in VF-MD‡ | −0.35 | 0.31 |
| Change in VF-PSD‡ | −0.17 | 0.60 |
Based on 38 eyes of the overall group.
Based on 16 eyes of the trabeculectomy group.
Based on 15 eyes of the trabeculectomy group.
IOP = intraocular pressure; NFL = nerve fiber layer; VF-MD = visual field test mean deviation; VF-PSD = visual field test pattern standard deviation.
Figure 1.
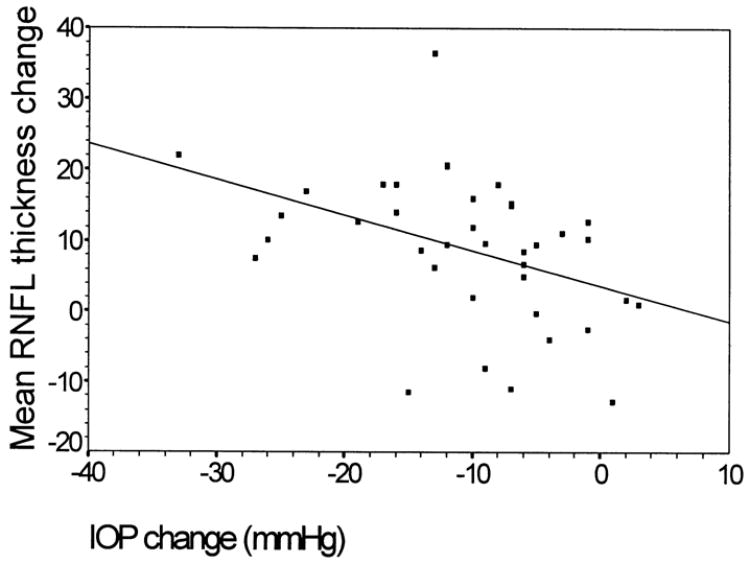
Scatterplot of mean retinal nerve fiber layer (RNFL) thickness change from before to after filtration surgery and intraocular pressure (IOP) change (mmHg).
Figure 2.
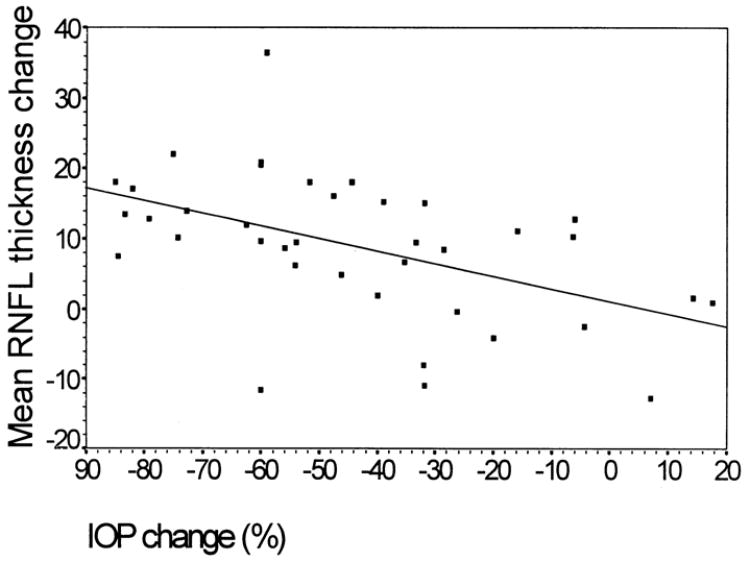
Scatterplot of mean retinal nerve fiber layer (RNFL) thickness change from before to after filtration surgery and the percentage of intraocular pressure (IOP) change.
Discussion
This study evaluated the NFL thickness changes, as measured by OCT, after trabeculectomy or combined cataract extraction and trabeculectomy. The OCT scans in this study were all performed with a prototype device. Our group previously found a strong correlation between NFL measurements obtained by a prototype and commercial OCT (Invest Ophthalmol Vis Sci 39[suppl]:S932, 1998). Thus, although the study has been performed with prototype OCT data, these findings are also likely to reflect changes as determined by the commercial OCT device.
We found a significant increase in the peripapillary NFL thickness, as determined by OCT, after glaucoma filtration surgery (Table 3). The NFL thickening was significant for the overall measurement and in all quadrants except the inferior quadrant. Segmental analysis should be performed cautiously because the reproducibility decreased for quadrant measurements in glaucoma subjects, especially in the temporal and nasal quadrants.13 More subjects may be needed for segmental analysis. The NFL thickness changes were found to be highly correlated with IOP changes as determined either by the mean IOP change or the percentage of change.
To assess the association between preoperative glaucomatous NFL damage and postoperative thickness change, we divided the eyes into three equal groups on the basis of the preoperative NFL thickness; we compared the first group (with the lowest thickness values) with the second group (with higher values for overall circumpapillary and segmental NFL thickness changes). Between these two groups, there was no statistically significant difference of postoperative NFL thickness changes except in the temporal quadrant. In that quadrant, there was a significantly higher NFL thickness increase in the first group (with the lowest preoperative thickness values; P = 0.02).
The reason for the differences in the NFL thickness changes between the two surgical approaches is unclear (Tables 4 and 5) and might be due to the small sample size. On the basis of our findings, after filtration surgery, we would expect a 0.5-μm thickening of the mean NFL for each 1-mmHg decrease of the IOP, indicating the relationship between IOP reduction and mean NFL thickness.
These findings were consistent with other studies in which different methods were used to evaluate ONH changes after filtration surgery. These methods detected the changes in the ONH and the NFL thickness along the ONH margin. Sogano et al6 imaged 12 eyes with the Rodenstock optic nerve analyzer 2 to 6 months after glaucoma surgery and found a significant decrease in cup volume and an increase in rim area. No statistically significant change was observed in that study in relative NFL height; however, the authors reported that relative NFL height increased in 7 of 12 eyes in which IOP was markedly reduced, and the changes in NFL height were shown by linear regression analysis to be pressure dependent.
Irak et al7 used a CSLO device to evaluate 49 eyes of 49 glaucoma patients 3 months after filtration surgery and found a significant decrease in mean cup area, cup volume, and cup-to-disc area ratio, as well as a significant increase in mean rim area and rim volume. No significant change was found in NFL cross-sectional area, but the change was significantly associated (P < 0.01) with the change in IOP. Lesk et al8 reported similar results with the CSLO device in 17 glaucoma patients 6 months after surgery; however, the correlation with the IOP change did not reach significance.
Kotecha et al10 evaluated longitudinal optic disc changes after trabeculectomy in 95 patients with CSLO. They found a significant increase in rim area and rim volume at 2 years after surgery. Segmental analysis showed a significant change in rim volume in the nasal, inferonasal, superonasal, and superotemporal sectors. A significant correlation was reported between changes in the optic disc parameters and reduction of IOP. Kotecha et al have suggested that the improvement is confined to the nasal hemidisc and the adjacent NFL because this area tends to be least affected by the disease, so nerve fiber bundle compression is not as long-standing as that within the temporal hemidisc. Thus, with the reduction of IOP and anterior movement of the lamina cribrosa, the retinal nerve fibers within the nasal region may regain their original shape and thickness, whereas those within the temporal region may be too damaged.
In contrast to these studies, Topouzis et al19 did not find any significant changes in ONH parameters 8 months after surgery. This result might be due to the high degree of preexisting glaucomatous damage (mean MD, −13.2 dB), because experimental studies9,20,21 have shown that reversal of damage is more likely to occur in earlier stages of glaucoma.
The physiologic basis of the improvement in ONH appearance and NFL thickness with IOP reduction is not clear. It has been suggested that IOP reduction results in less posterior bowing of the lamina cribrosa.1,22 This theory may explain changes in ONH parameters, such as the decrease in cup volume and cup area and the increase in rim volume and rim area. However, it is difficult to directly explain, with this mechanical theory, the increase in the NFL thickness, which is detected with the peripapillary OCT scan in a 3.4-mm-diameter circle. Another explanation for this improvement could be ONH and peripapillary swelling due to the sudden postoperative IOP reduction. However, the inclusion criteria in our study were OCT scans obtained 6 to 12 months after surgery, to minimize the likelihood of this effect. Therefore, it is unlikely that postoperative edema accounts for our results. Finally, the increase of NFL thickness may reflect the recovery of the compressed NFL, which regains its original shape because of the IOP reduction. This relates to our initial point regarding the change in configuration of the lamina cribrosa. As compression on the axons is relieved with IOP reduction, the axons may recover their normal shape and size, with resultant increase in NFL thickness and changes in ONH parameters.
The clinical implications of the ONH topography and NFL thickness improvement are unclear, although previous studies have shown that there may be an associated improvement of visual function that corresponds to this improvement.5,23–25 However, in our study, we did not find a significant change in the mean MD and PSD after surgery (P = 0.43 and P = 0.34, respectively), and similar findings have been reported by Lesk et al.8 In terms of practical implications, an increase in NFL thickness can be expected after IOP-decreasing procedures, and we recommend obtaining new OCT images after these procedures as a baseline for follow-up of glaucoma patients.
In conclusion, we showed an increase in NFL thickness after glaucoma filtration surgery that correlated with IOP reduction. The physiologic basis for this improvement is unknown, and it has yet to be evaluated whether these changes have any clinical significance in long-term follow-up.
Acknowledgments
The authors thank Liselotte Pieroth, MD, for providing essential support in study design.
Footnotes
Presented in part at the annual meeting of the American Academy of Ophthalmology, Orlando, Florida, October 2002.
Supported in part by the National Institutes of Health (grant nos.: 1-RO1 EY 13178-02 [JSS] and 2-RO1 EY 11289-15 [J. G.J. G. Fujimoto, PhD]), Bethesda, MD, and by Carl Zeiss Meditech research grant support (JSS), Dublin, CA.
References
- 1.Quigley HA. The pathogenesis of reversible cupping in congenital glaucoma. Am J Ophthalmol. 1977;84:358–70. doi: 10.1016/0002-9394(77)90680-8. [DOI] [PubMed] [Google Scholar]
- 2.Robin AL, Quigley HA. Transient reversible cupping in juvenile-onset glaucoma. Am J Ophthalmol. 1979;88:580– 4. doi: 10.1016/0002-9394(79)90518-x. [DOI] [PubMed] [Google Scholar]
- 3.Quigley HA. Childhood glaucoma: results with trabeculectomy and study of reversible cupping. Ophthalmology. 1982;89:219–26. doi: 10.1016/s0161-6420(82)34803-4. [DOI] [PubMed] [Google Scholar]
- 4.Greenidge KC, Spaeth GL, Traverso CE. Change in appearance of the optic disc associated with lowering of intraocular pressure. Ophthalmology. 1985;92:897–903. doi: 10.1016/s0161-6420(85)33937-4. [DOI] [PubMed] [Google Scholar]
- 5.Katz LJ, Spaeth GL, Cantor LB, et al. Reversible optic disk cupping and visual field improvement in adults with glaucoma. Am J Ophthalmol. 1989;107:485–92. doi: 10.1016/0002-9394(89)90492-3. [DOI] [PubMed] [Google Scholar]
- 6.Sogano S, Tomita G, Kitazawa Y. Changes in retinal nerve fiber layer thickness after reduction of intraocular pressure in chronic open-angle glaucoma. Ophthalmology. 1993;100:1253– 8. doi: 10.1016/s0161-6420(93)31497-1. [DOI] [PubMed] [Google Scholar]
- 7.Irak I, Zangwill L, Garden V, et al. Change in optic disk topography after trabeculectomy. Am J Ophthalmol. 1996;122:690–5. doi: 10.1016/s0002-9394(14)70488-x. [DOI] [PubMed] [Google Scholar]
- 8.Lesk MR, Spaeth GL, Azuara-Blanco A, et al. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology. 1999;106:1013– 8. doi: 10.1016/S0161-6420(99)00526-6. [DOI] [PubMed] [Google Scholar]
- 9.Shirakashi M, Nanba K, Iwata K. Reversal of cupping in experimental glaucoma. Ophthalmologica. 1991;202:194–201. doi: 10.1159/000310198. [DOI] [PubMed] [Google Scholar]
- 10.Kotecha A, Siriwardena D, Fitzke FW, et al. Optic disc changes following trabeculectomy: longitudinal and localisation of change. Br J Ophthalmol. 2001;85:956– 61. doi: 10.1136/bjo.85.8.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raitta C, Tomita G, Vesti E, et al. Optic disc topography before and after trabeculectomy in advanced glaucoma. Ophthalmic Surg Lasers. 1996;27:349–54. [PubMed] [Google Scholar]
- 12.Schuman JS, Hee MR, Puliafito CA, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113:586–96. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- 13.Schuman JS, Pedut-Kloizman T, Hertzmark E, et al. Reproducibility of nerve fiber layer thickness measurements using optical coherence tomography. Ophthalmology. 1996;103:1889–98. doi: 10.1016/s0161-6420(96)30410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grewing R, Becker H. Retinal thickness immediately after cataract surgery measured by optical coherence tomography. Ophthalmic Surg Lasers. 2000;3:215–7. [PubMed] [Google Scholar]
- 15.Sourdille P, Santiago PY. Optical coherence tomography of macular thickness after cataract surgery. J Cataract Refract Surg. 1999;25:256– 61. doi: 10.1016/s0886-3350(99)80136-9. [DOI] [PubMed] [Google Scholar]
- 16.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178– 81. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schuman JS, Hee MR, Arya AV, et al. Optical coherence tomography: a new tool for glaucoma diagnosis [review] Curr Opin Ophthalmol. 1995;6:89–95. doi: 10.1097/00055735-199504000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Izatt JA, Hee MR, Swanson EA, et al. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch Ophthalmol. 1994;112:1584–9. doi: 10.1001/archopht.1994.01090240090031. [DOI] [PubMed] [Google Scholar]
- 19.Topouzis F, Peng F, Kotas-Neuman R, et al. Longitudinal changes in optic disc topography of adult patients after trabeculectomy. Ophthalmology. 1999;106:1147–51. doi: 10.1016/S0161-6420(99)90248-8. [DOI] [PubMed] [Google Scholar]
- 20.Shirakashi M, Nanba K, Iwata K. Changes of reversal of cupping in experimental glaucoma. Longitudinal study Ophthalmology. 1992;99:1104–10. doi: 10.1016/s0161-6420(92)31844-5. [DOI] [PubMed] [Google Scholar]
- 21.Coleman AL, Quigley HA, Vitale S, et al. Displacement of the optic nerve head by acute changes in intraocular pressure in monkey eyes. Ophthalmology. 1991;98:35– 40. doi: 10.1016/s0161-6420(91)32345-5. [DOI] [PubMed] [Google Scholar]
- 22.Albon J, Purslow PP, Karwatowski WS, et al. Age related compliance of the lamina cribrosa in human eyes. Br J Ophthalmol. 2000;84:318–23. doi: 10.1136/bjo.84.3.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsai CS, Shin DH, Wan JY, et al. Visual field global indices in patients with reversal of glaucomatous cupping after intraocular pressure reduction. Ophthalmology. 1991;98:1412–9. doi: 10.1016/s0161-6420(91)32118-3. [DOI] [PubMed] [Google Scholar]
- 24.Spaeth GL. The effect of change in intraocular pressure on the natural history of glaucoma: lowering intraocular pressure in glaucoma can result in improvement of visual fields. Trans Ophthalmol Soc U K. 1985;104:256– 64. [PubMed] [Google Scholar]
- 25.Yildirim E, Bilge AH, Ilker S. Improvement of visual field following trabeculectomy for open angle glaucoma. Eye. 1990;4:103– 6. doi: 10.1038/eye.1990.12. [DOI] [PubMed] [Google Scholar]


