Abstract
Objective
Mass-media campaigns have been known to modify the outcome of low back pain (LBP). We assessed the impact on outcome of standardized written information on LBP given to patients with acute LBP.
Methods
Design: A 3-month pragmatic, multicenter controlled trial with geographic stratification. Setting: Primary care practice in France. Participants: 2752 patients with acute LBP. Intervention: An advice book on LBP (the “back book”). Main outcome measures: The main outcome measure was persistence of LBP three months after baseline evaluation.
Results
2337 (85%) patients were assessed at follow-up and 12.4% of participants reported persistent LBP. The absolute risk reduction of reporting persistent back pain in the intervention group was 3.6% lower than in the control group (10.5% vs. 14.1%; 95% confidence interval [−6.3% ; −1.0%]; p value adjusted for cluster effect = 0.01). Patients in the intervention group were more satisfied than those in the control group with the information they received about physical activities, when to consult their physician, and how to prevent a new episode of LBP. However, the number of patients who had taken sick leave was similar, as was the mean sick-leave duration, in both arms, and, among patients with persistent pain at follow-up, the intervention and control groups did not differ in disability or fear-avoidance beliefs.
Conclusions
The level of improvement of an information booklet is modest, but the cost and complexity of the intervention is minimal. Therefore, the implications and generalizability of this intervention are substantial.
Trial Registration
ClinicalTrials.gov NCT00343057
Introduction
About 60% of the population is concerned with low back pain (LBP) in Western industrialized countries [1]. Chronic LBP (cLBP) has become a major medical, social and economic problem [2]. The costs are comparable to those induced by coronary heart disease, diabetes, or depression [3]. Diminishing the cost is a major public health issue. An approach to achieving this goal is to improve the prevention of chronic disease in patients with acute LBP in primary care practice.
Psychosocial factors have been shown to be associated with the development of disability with cLBP [4], and the best individualized factors are anxiety, depression, coping, and fear of and belief about pain [5]. Providing advice to stay active and information about how to cope with pain has been shown to modify patients' fears, avoidance attitudes and beliefs [6], [7]. Because health care providers play a pivotal role in patient information and education in primary care practice, general practitioners (GPs) could greatly influence the outcome in LBP and thus contribute to decreased LBP-related costs.
Several guidelines and reviews on the management of acute LBP and cLBP in primary care practice are available [8]–[25]. They mainly concern prescriptions for X-rays and laboratory tests, treatment options, and information about physical and occupational activities. The consensus among international guidelines seems to be that advice to stay active, reassurance and use of analgesics, if necessary, for pain relief are important for acute episodes of LBP. Specific exercises and occupational activities seem to be useful for persistent but not acute LBP. Exercises, education about back pain, behavioural treatment and multidisciplinary treatment seem effective in preventing persistent/chronic LBP. Concerning information given to patients, evidence suggests that advice about staying active and coping with pain could decrease the rate of patients experiencing chronic pain and the impact of LBP on daily and occupational activities [23]–[25].
Information booklets, the lowest-cost information tools, have been developed to help health care providers inform and educate patients. Among these booklets [7], [23]–[25], the “back book,” developed from evidence-based medicine by a multidisciplinary team and published to accompany the United Kingdom back-pain guidelines [26], has been shown, in a limited sample of English patients with LBP, to significantly affect fears and beliefs about and disability with LPB but not pain level [7]. Other educational booklets or pamphlets have been previously assessed, with relatively modest effects, for acute [27], chronic [28], or occupational [29] back pain. The “back book” has been translated with use of a validated translation/back translation procedure and culturally adapted to French-speaking patients with LBP [30]. It is the only evidence-based information booklet available for such patients (i.e., “le Guide du dos”) but has never been evaluated in this setting.
The aim of this study was to assess the impact of the “back book” on outcome (persistence of pain at 3 months) in acute LBP in a French national sample of patients in a primary care setting.
Methods
The protocol for this trial and supporting CONSORT checklist are available as supporting information; see Checklist S1 and Protocol S1.
Trial design
We conducted a 3-month prospective, controlled study with a quasi-experimental design (i.e., a nonrandomized controlled sample with geographic stratification [30 areas]). Control and intervention areas were selected for their similarities in rural-to-urban distribution of the population and patients' access to GPs and to minimize risk of overlap between areas.
Participants
GPs
A total of 60 GPs per geographic area were selected at random from a national database (Logimed) according to a computerized allocation [31], and 1800 GPs were invited to participate in the study. Those agreeing to participate were assigned to the intervention or control group, depending on their geographic area. Each GP in the intervention group received a personal copy of the “back book” and was asked to read it before including patients and explaining the booklet to patients. GPs in the control group were told that they would get the book at the end of the trial.
Patients
Each GP had to enrol up to 4 consecutive patients with acute LBP. Patients were excluded if they (a) were less than 18 years old; (b) had pain for more than 4 weeks; (c) had pain intensity for the previous 24 hours less than 3 on a 11-point numeric scale (0 = no pain, 10 = maximal pain); (d) had sciatica; (e) had had a previous episode of acute LBP during the last 12 months; (f)did not work; (h) had consulted another practitioner for the same episode of back pain; (i) were pregnant; (j) had back pain related to infection, tumor, or inflammatory disease; or (k) had previously undergone back surgery.
Ethical approval
The study protocol was approved by the Commission Nationale Informatique et Liberté and the French National Medical Council (Conseil National de l'Ordre des Médecins). The study was conducted in compliance with the protocol Good Clinical Practices and Declaration of Helsinki principles. In accordance with the French national law, GPs and patients gave their written consent to participate after being informed about the study protocol.
Intervention
At baseline, all patients received medical care and oral information as usually provided by GPs. In the intervention group, all patients also received the “back book.”
Outcome measures
Main outcome measure
To assess persistence of LBP 3 months after baseline evaluation, patients were asked to answer Yes or No to the question “Has your low back pain persisted since the first visit to your GP 3 months ago?” Patients answering Yes were considered as having persistent back pain.
Physician questionnaire
Parts 1, 2, and 3 of the physician self-administered questionnaire completed at baseline concerned demographic data (age and sex), professional data (years of practice and exclusively private or public/private practice) and personal history of LBP (acute, recurrent, chronic), and self-limitation of physical activities for LBP (never, sometimes, often, always), respectively. Part 4 dealt with GPs' formation of practice and practice for LBP: participation in an educational session on LBP in the last 3 years (yes/no); mean length of sick leave prescription for acute LBP if needed (≤3 days, >3 and ≤8 days, >8 days), advice about physical activities during sick leave for acute LBP (bed rest, rest at home, keep maximum bearable activities). Part 5 assessed GPs' fears, avoidance attitudes and beliefs on the Fear-Avoidance Beliefs Questionnaire (FABQ)[5], which consists of 2 independent subscales: FABQ Phys and FABQ Work. The FABQ Phys assesses fears, avoidance attitudes and beliefs related to general physical activities (4 items, range 0–24), and the FABQ Work assesses fears, avoidance attitudes and beliefs related to occupational activities (7 items, range 0–42). Each item is scored from 0, “do not agree at all,” to 6, “completely agree”. For both subscales, a low score indicates low fears, avoidance attitudes and beliefs. According to the designers of the scale, a score of 14 or more on the FABQ Phys scale indicates strong beliefs [5], [7]. This questionnaire has been validated in English [5], German [32], and, recently, in French [33]. The FABQ was originally developed to assess patients' fears, avoidance attitudes and beliefs. To evaluate GPs' fears, avoidance attitudes and beliefs, we did not modify the phrasing of items but slightly adapted the first sentence of instructions to patients. This sentence was “these are statements that other patients have expressed about their low back pain…”; we just deleted the word “other”.
Patients' questionnaire
Baseline evaluation
Baseline data were collected during the first visit to GPs. Patients were interviewed about pain intensity (11-point numeric scale, from 0, no pain, to 10, maximal pain), physical demand of occupational activities (11-point numeric scale, from 0, no physical demand, to 10, extremely hard physical demand), education level (no full-time education, primary school, high school, post-graduate education), presence of LBP in parents (yes/no), length of back pain (days), work-related back pain (yes/no), sport activities (none, occasional, regular, competition), medication intake for the previous week (analgesics, nonsteroidal anti-inflammatory drugs [NSAIDs], muscle relaxants), pain intensity for the last 48 hours (weak, moderate, severe, extremely severe), and handicap level for activities of daily living (no handicap, weak, moderate, severe, extremely severe). Self-rated disability was assessed on the Quebec questionnaire (20 items scored from 0, no disability, to 5, impossible to do; range 0–100) [34]. LBP beliefs were recorded on the FABQ (see GPs' questionnaire).
3-month follow-up evaluation
At baseline, an appointment for a follow-up visit with the GP was established for the patient. Follow-up data were recorded during this visit to the GP (77% of patients) or by phone interviews (23% of patients), conducted by trained research assistants for patients who did not consult their physician. Patients were asked about persistence of LBP since the baseline evaluation (yes/no); whether radiography, computed tomography (CT), or magnetic resonance imaging had been performed (yes/no); sick leave since baseline evaluation (yes/no); sick leave duration (days); return to work (yes/no); and satisfaction with information received about physical activities, when to see a doctor, how to use medications, and how to prevent new episodes of LBP (very satisfied, rather satisfied, rather not satisfied, unsatisfied). For patients with persistent LBP, pain intensity, level of handicap, perceived disability, anxiety and depression, and LBP beliefs were recorded as during the baseline evaluation.
Sample size
Persistent LBP after an acute episode has previously been reported to occur in 7% of patients in France [35]. We hypothesized (consensus among the authors) that a difference of 3 points between control and intervention groups (7% in the control and 4% in the intervention groups) would have a clinical and public health relevance. With a 2-sided chi-square test at 5%, a sample size of 1212 patients per group would have 90% power for detecting a significant difference between the control and intervention groups. Allowing for 15% of patients lost to follow-up at 3 months, we sought to recruit 2830 patients.
Statistical analysis
The impact of the “back book” intervention was assessed by comparing the proportions of patients with persistent LBP after 3 months who had been exposed to the “back book” and those who had not been exposed. Qualitative outcomes were compared by chi-square test and quantitative outcomes by t-test. To take into account the cluster effect (patients are clustered within physician), the primary outcome (persistent pain) was also analysed in the framework of a generalized estimation equation (GEE) regression model, with the physician considered as a random effect. The same procedure was applied to assess the impact of the “back book” on the secondary outcomes.
The analysis was per protocol. We performed 2 intention-to-treat analyses. In the first analysis, we considered all patients lost to follow-up as having persistent pain at 3 months. In the second, we considered all patients lost to follow-up as having no persistent pain at 3 months.
Data analyses involved use of SAS (SAS institute Inc, Cary, NC).
Results
Flow of participants through trial
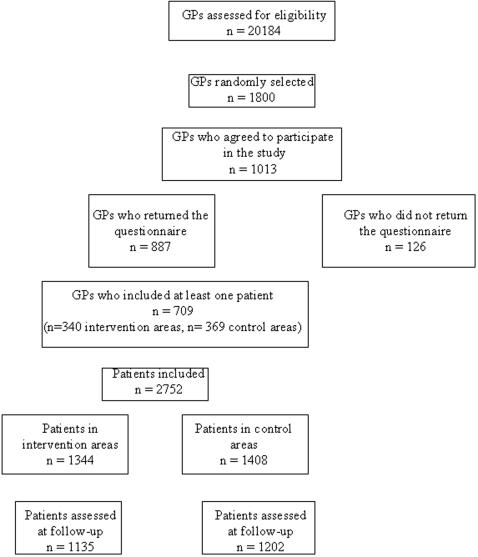
The Logimed database contains information on 20 184 GPs. A total of 60 GPs per geographic area were selected at random from the database and asked to participate, with 1013 GPs agreeing to participate. Of these, 88% returned their questionnaires, and 709 (70%) included at least 1 patient (Figure 1). Among the GPs who agreed to participate, 488 were in intervention areas and 525 in control areas, and 69.7% of GPs in the intervention and 70.3% in the control areas returned their questionnaires and included at least one patient.
Figure 1. Flow of general practitioners and patients through the trial.
A total of 2752 patients met the inclusion criteria, and 2337 (82.6%) (1135 and 1202 in the intervention and control groups, respectively) were assessed at follow-up. At baseline, patients lost to follow-up did not differ from those assessed at 3 months in terms of age, gender, pain and handicap levels, sport activities, education level, disability, and beliefs (table 1). The number of patients lost to follow-up did not differ between the intervention and control groups (209 [15.5%] and 206 [14.6%] respectively).
Table 1. Baseline demographic and clinical characteristics of patients.
| Patients assessed at follow-up N = 2337 | Intervention group N = 1135 | Control Group N = 1202 | Lost to follow-up N = 412 | |
| Age (m±SD), years | 45±12 | 45±12 | 44±12 | 43±12 |
| Sex (M) | 1321 (57%) | 628 (56%) | 693 (58%) | 237 (57%) |
| Back pain duration (median (interquartile range), days | 3 (5) | 3 (4) | 4 (5) | 3 (6) |
| Physical demand of work (0–10) (m±SD) | 5.7±2.5 | 5.7±2.5 | 5.7±2.5 | 5.5±2.6 |
| Education level | ||||
| No full-time education | 51 (2%) | 27 (2%) | 24 (2%) | 7 (2%) |
| Primary school | 656 (28%) | 294 (26%) | 362 (30%) | 114 (28%) |
| High school | 1075 (46%) | 528 (47%) | 547 (46%) | 207 (50%) |
| Post graduate | 552 (24%) | 284 (25%) | 268 (22%) | 86 (20%) |
| Back pain in parents | 1242 (54%) | 593 (53%) | 649 (55%) | 198 (49%) |
| Work-related back pain | 193 (8%) | 95 (8%) | 98 (8%) | 37 (9%) |
| Sports activities | ||||
| None | 1061 (45%) | 502 (45%) | 559 (47%) | 199 (48%) |
| Occasional | 830 (36%) | 411 (36%) | 419 (35%) | 133 (32%) |
| Usual | 414 (18%) | 207 (18%) | 207 (17%) | 76 (18%) |
| Competition | 21 (1%) | 10 (1%) | 11 (1%) | 4 (2%) |
| Medications * | ||||
| Analgesics (yes) | 1903 (81%) | 929 (82%) | 974 (81%) | 322 (78%) |
| NSAIDs (yes) | 611 (26%) | 286 (25%) | 325 (27%) | 102 (25%) |
| Muscle-relaxants (yes) | 434 (19%) | 196 (17%) | 238 (20%) | 87 (21%) |
| Pain level (m±SD) | 6.8±1.5 | 6.7±1.5 | 6.8±1.5 | 6.7±1.5 |
| Pain intensity | ||||
| None/weak | 49 (2%) | 24 (2%) | 25 (2%) | 11 (5%) |
| Moderate | 485 (21%) | 229 (20%) | 256 (21%) | 85 (21%) |
| Severe | 1598 (69%) | 777 (70%) | 821 (69%) | 276 (68%) |
| Extremely severe | 181 (8%) | 90 (8%) | 91 (8%) | 24 (6%) |
| Handicap level ** | ||||
| None/weak | 78 (3%) | 35 (3%) | 43 (4%) | 14 (3%) |
| Moderate | 704 (30%) | 328 (28%) | 376 (31%) | 131 (32%) |
| Severe | 1352 (59%) | 671 (60%) | 681 (57%) | 236 (59%) |
| Extremely severe | 178 (8%) | 85 (8%) | 93 (8%) | 23 (6%) |
| LBP beliefs | ||||
| FABQ Phys (0–24) (m±SD) | 16.9±5.0 | 16.7±5.0 | 17.1±4.9 | 16.2±5.0 |
| FABQ Work (0–42) (m±SD) | 19.7±10.9 | 19.7±11.1 | 19.7±10.6 | 18.8±10.8 |
| Disability | ||||
| Quebec (0–100) (m±SD) | 55.0±17.2 | 55.3±16.9 | 54.7±17.6 | 54.6±17.6 |
Values are number of patients (percentages)
for the last week
for activities of daily living
NSAID = nonsteroidal anti-inflammatory drug; FABQ = Fear-Avoidance Beliefs Questionnaire
Baseline characteristics
Patients (Table 1) and GPs (Table 2) in the intervention and control groups did not differ in baseline characteristics. The patients' mean (±SD) age was 45±12 years, and 57% were male. The median pain duration at baseline was 3 (median interquartile range 5) days and pain level 6.8±1.5 (range 0–10). Before seeing their GP, 81% of patients had taken analgesics, 26% NSAIDs, and 19% muscle relaxants. The Quebec disability scale mean score was 55.0±17.2 (range 0–100). Fears and beliefs were high, with FABQ Phys and Work mean scores of 16.9±5.0 and 19.7±10.9, respectively. A total of 72% of patients had strong fears and beliefs about back pain [5], [7]. The GPs' mean age was 48±7 years; 79% in both groups were male, 69% worked in an urban environment, and 87% had more than 10 years of practice.
Table 2. Demographic and professional characteristics, and personal history of back pain of GPs, GPs' formation of and self-reported attitude about acute low back pain, and GPs' self-reported recommendations for chronic low back pain.
| Whole sample of GPs N = 709 | Intervention practices N = 340 | Control practices N = 369 | p-value (t-test or Chi2) | |
| Age mean (SD) | 48.0 (7.0) | 48.2 (6.6) | 47.9 (7.4) | p = 0.71 |
| Gender (M) | 563 (79.5%) | 269 (79.1%) | 294 (79.9%) | p = 0.80 |
| Years of practice | ||||
| <10 | 93 (13.2%) | 39 (11.6%) | 54 (14.7%) | p = 0.16 |
| 10–20 | 296 (42.0%) | 155 (46.0%) | 141 (38.4%) | |
| 21–30 | 279 (39.6%) | 129 (38.3%) | 150 (40.9%) | |
| >30 | 36 (5.2%) | 14 (4.1%) | 22 (6.0%) | |
| Environment of practice | ||||
| Rural | 216 (30.5%) | 116 (34.1%) | 100 (27.1%) | p = 0.10 |
| Urban | 390 (69.1%) | 222 (65.3%) | 268 (72.6%) | |
| Rural and urban | 3 (0.4%) | 2 (0.6%) | 1 (0.3%) | |
| Personal history of back pain | ||||
| Acute | 353 (49.9%) | 171 (50.4%) | 182 (49.3%) | p = 0.77 |
| Recurrent | 234 (33.0%) | 108 (31.9%) | 126 (34.2%) | p = 0.52 |
| Chronic | 102 (14.4%) | 52 (15.3%) | 50 (13.6%) | p = 0.49 |
| Self-limitation of physical activity for back pain | ||||
| Never | 215 (49.9%) | 96 (47.5%) | 119 (52.0%) | p = 0.61 |
| Rarely | 185178 (42.9%) | 90 (44.6%) | 95 (41.5%) | |
| Frequently | 23 (5.3%) | 13 (6.4%) | 10 (4.4%) | |
| Always | 8 (1.9%) | 3 (1.5%) | 5 (2.1%) | |
| GPs' education about back pain | ||||
| Education session on back pain in the last 3 years (yes) | 316 (46.4%) | 154 (47.2%) | 162 (45.6%) | p = 0.67 |
| GPs' attitude about back pain | ||||
| Specific information delivered (yes) | 586 (85.8%) | 281 (85.9%) | 305 (85.7%) | p = 0.92 |
| Recommended sick leave duration for acute back pain | ||||
| ≤3 days | 59 (8.4%) | 30 (9.0%) | 29 (7.9%) | p = 0.54 |
| 3–8 days | 570 (81.3%) | 266 (79.6%) | 304 (82.8%) | |
| >8 days | 72 (10.3%) | 38 (11.4%) | 34 (9.3%) | |
| Physical activities recommended during sick leave for acute back pain | ||||
| Bed rest | 37 (5.4%) | 17 (5.2%) | 20 (5.5%) | P = 0.13 |
| Rest | 454 (65.7%) | 204 (62.2%) | 250 (68.9%) | |
| Maximum bearable activity | 200 (28.9%) | 107 (32.6%) | 93 (25.6%) | |
| GPs' FABQ Phys score (range 0–24) | 9.6 (4.8) | 9.2 (4.5) | 10.0 (5.0) | P = 0.10 |
| GPs' FABQ Work score (range 0–42) | 17.5 (6.7) | 17.6 (6.7) | 17.4 (6.6) | P = 0.69 |
Values are numbers (percentages) or m±SD
Impact of the intervention at 3-month follow-up
At 3-month follow-up, 12.4% of participants reported persistent LBP. In the intervention group, the proportion of patients experiencing persistent back pain was lower than in the control group (10.5% vs. 14.1%; difference −3.6%; 95% CI [−6.3% ; −1.0%]) (Table 3). The outcome was different depending on the method used to collect data for the primary outcome. In the intervention group, among patients reporting persistent pain, only 7.6% were assessed by phone interviews as compared with 25.6% of those free of pain. A similar proportion was observed in the control group, with 13.6% and 24.2% for those reporting pain and those free of pain, respectively. In the intervention group, persistent pain was reported by 3.5% of patients assessed by phone and 12.7% by face-to-face interview. In the control group, persistent pain was reported by 8.4% of those assessed by phone and 15.7% by face-to-face interview. Finally, the method of collecting data did not differ between groups (23.7% and 22.7% in the intervention and control groups were assessed by phone interview, respectively). For the current LBP episode, patients in the intervention group were not less often referred to a spine specialist and had a similar rate of spine imaging exams as patients in the control group. The number of patients who had taken sick leave was similar, as was the mean sick-leave duration in both arms. Fewer patients had taken NSAIDs and muscle relaxants in the intervention group than the control group. Patients in the intervention group were more satisfied than those in the control group about the information and advice they received about physical activities, when to consult their physician, and how to prevent a new episode of LBP but not more satisfied about advice on medication intake. Adjusting for the cluster effect did not change the crude results, except for referring to a spine specialist.
Table 3. Follow-up assessment at 3 months.
| Whole sample N = 2337 | Intervention group N = 1135 | Control group N = 1202 | Percentage or mean difference (95% CI) | P value* (Chi-square or t-test) | P value** (adjusted for cluster effect) | |
| Persistent back pain | 289 (12.4%) | 119 (10.5%) | 170 (14.1%) | −3.6 (−6.3; −1.0) | 0.0072 | 0.0131 |
| Visit to spine specialist | 680 (29.4%) | 305 (27.2%) | 375 (31.5%) | −4.3 (−8.0 ; −0.5) | 0.0253 | 0.0566 |
| Spine imaging | ||||||
| Plain radiography | 676 (29.2%) | 327 (29.1%) | 349 (29.2%) | −0.1 (−3.8 ; 3.6) | 0.9428 | 0.8099 |
| Computed tomography | 194 (8.4%) | 89 (7.9%) | 105 (8.8%) | −0.9 (−3.1 ; 1.4) | 0.4469 | 0.4379 |
| Magnetic resonance imaging | 45 (1.9%) | 24 (2.1%) | 21 (1.8%) | 0.3 (−0.7 ; 1.5) | 0.5114 | 0.6886 |
| Sick leave | ||||||
| Yes | 1037 (44.9%) | 503 (45.0%) | 534 (44.8%) | 0.2 (−4.9 ; 4.3) | 0.9250 | 0.9132 |
| Sick leave duration (m±SD) | 6.5±14.4 | 6.0±12.9 | 6.9±15.7 | −0.9 (−2.0 ; 0.4) | 0.1592 | 0.2847 |
| Analgesic intake | 1964 (84.0%) | 936 (82.5%) | 1028 (85.5%) | −3.0 (−6.0 ; −0.1) | 0.0437 | |
| NSAID intake | 1008 (43.1%) | 447 (39.4%) | 561 (46.7%) | −7.3 (−11.3 ; −3.3) | 0.0004 | 0.0103 |
| Muscle-relaxant intake | 864 (37.0%) | 374 (32.9%) | 490 (40.8%) | −7.9 (−11.7 ; −3.9) | <0.0001 | 0.0176 |
| Information about Physical activities | 0.0003 | 0.0020 | ||||
| Very satisfied | 1699 (73.7%) | 868 (77.4%) | 831 (70.3%) | 7.1 (3.5 ; 10.7) | ||
| Rather satisfied | 437 (19.0%) | 194 (17.3%) | 243 (20.5%) | −3.6 (−6.4 ; −0.1) | ||
| Rather unsatisfied | 152 (6.6%) | 55 (4.9%) | 97 (8.2%) | −3.2 (−5.3 ; −1.3) | ||
| Unsatisfied | 17 (0.7%) | 5 (0.4%) | 12 (1.0%) | −0.6 (−1.3 ; 0.1) | ||
| When to consult a physician | 0.0010 | 0.0052 | ||||
| Very satisfied | 1428 (62.0%) | 739 (66.0%) | 689 (58.2%) | 7.8 (3.8 ; 11.8) | ||
| Rather satisfied | 632 (27.5%) | 281 (25.1%) | 351 (29.7%) | −4.6 (−8.2 ; −1.0) | ||
| Rather unsatisfied | 215 (9.3%) | 86 (7.7%) | 129 (10.9%) | −3.2 (−5.6 ; −0.8) | ||
| Unsatisfied | 27 (1.2%) | 13 (1.3%) | 14 (1.2%) | 0.1 (−0.9 ; 0.9 ) | ||
| How to prevent a new episode of back pain | 0.0033 | 0.0243 | ||||
| Very satisfied | 1290 (56.0%) | 660 (58.8%) | 630 (53.3%) | 5.5 (1.5 ; 9.6) | ||
| Rather satisfied | 750 (32.6%) | 359 (32.0%) | 391 (33.1%) | −1.1 (−4.9 ; 2.7) | ||
| Rather unsatisfied | 245 (10.6%) | 97 (8.7%) | 148 (12.5%) | −3.8 (−6.4 ; −1.4) | ||
| Unsatisfied | 19 (0.8%) | 6 (0.5%) | 13 (1.1%) | −0.6 (−1.3 ; 0.2) | ||
| Medication intake | 0.7090 | 0.9901 | ||||
| Very satisfied | 1531 (66.4%) | 743 (66.3%) | 788 (66.6%) | −0.3 (−4.2 ; 3.5) | ||
| Rather satisfied | 622 (27.0%) | 309 (27.5%) | 313 (26.5%) | 1.0 (−2.5 ; 4.7) | ||
| Rather unsatisfied | 142 (6.2%) | 66 (5.9%) | 76 (6.4%) | −0.5 (−2.5 ; 1.4) | ||
| Unsatisfied | 9 (0.4%) | 3 (0.3%) | 6 (0.5%) | −0.2 (−0.8 ; 0.3) | ||
Values are numbers (%); NSAID = nonsteroidal anti-inflammatory drug
P value when computing absolute difference
P value when taking into account the cluster effect
For intention-to-treat analysis on the main outcome measure, we used sensitivity analysis on the primary outcome by considering two extreme scenarios (worst and best-case imputation, respectively). In the first scenario, we considered that all patients lost to follow-up had persistent back pain at 3 months. The proportion of patients reporting persistent back pain at 3 months was lower in the intervention than in the control group, but the difference was not significant (24.4% versus 26.7%; difference −2.3%; 95% CI [−1.0 ; 5.6]). However, for this scenario, the power of the test to detect a statistically significant difference was only 25%. In the second scenario, we considered that all patients lost to follow-up had no persistent back pain at 3 months. The proportion of patients reporting persistent back pain was lower in the intervention than in the control group, but the difference was significant (8.9% versus 12.1%; difference −3.2%; 95% CI [−5.5 ; −1.0]). For this scenario, the power of the test was 70%.
Among patients with persistent pain at follow-up, the intervention and control groups did not differ in disability (Quebec mean score 31.0±14.7 and 31.3±15.5, respectively) or fear-avoidance beliefs (FABQ Phys and Work mean scores 12.0±5.3 and 13.3±5.6, and 19.1±10.3 and 19.8±11.6, respectively).
Discussion
Interpretation
Our results suggest that providing the “back book” to patients consulting their GPs for acute LBP can reduce the proportion of patients reporting persistent pain at 3 months by 3.6% as compared with patients who did not receive the book. Previous studies have demonstrated a positive impact of such books for patients [7] or physicians [36] in terms of beliefs about LBP, patients' satisfaction with information [23], [24], patients' knowledge about LBP [25], and number of visits to GPs [37]. However, we failed to demonstrate any effect of the book on disability and pain level in patients reporting persistent pain and, as others, on work absenteeism [29]. Our study is the first to report the impact of this simple educational intervention on the outcome of patients with acute LBP in a large national sample. The “back book” has also been used as a part of an information intervention including radio and TV spots and newspaper advertising in a large mass-media campaign about LBP in Australia, which had a short- [6] and long-term positive impact [38] on claims and costs related to LBP. These multimedia interventions are difficult to perform and very expensive, but booklets or pamphlets are simple to use and inexpensive.
The “back book” may have several other positive effects. We observed a decrease of NSAID and myo-relaxant but not analgesic intake in the intervention group. This observation is not surprising, since advice about pain medications in this booklet recommends grade I analgesics, especially paracetamol. The other positive effect was patients' satisfaction with information. Most of patients' complaints and claims about medical procedures relate to lack of information [39].
However, overall the “back book” had no effect on the other main back-pain outcomes: the number of sick leaves taken or sick-leave duration and perceived disability in patients reporting persistent pain. This observation had already been observed after occupational low back injury [29]. More complex and expensive interventions involving several participants may be required to reach this objective. As compared with actual experience and behavioural experiments, education seems to be a weak intervention for changing attitudes and beliefs with cLBP [40]. Despite the existence of guidelines [8], the mean sick-leave duration reported in this study may seem quite long. This finding may be explained, at least in part, by the French sick-leave policy: GPs are free to order sick leave and, until recently, sick leaves of less than one month received almost no monitoring. Furthermore, during the first 3 months of sick leave, most employees receive their entire salary.
The “back book” also had no effect on the rate of prescriptions to undergo spine imaging. Almost 29% of patients underwent plain radiography and 8% CT. Thus, GPs are not following guidelines [8], [9], which emphasizes the need for large-scale education programs on this topic.
Finally, the effects of the “back book” may be underestimated in this study, since GPs in the control group knew that the trial assessed the impact of information on patients with LBP and may have followed the guidelines more closely than under real-life conditions.
Another important result is the high proportion of patients reporting persistent pain after 3 months in the control group. This proportion probably differs among countries [41], and the only information available for France at the beginning of our study was 6.2% of patients consulting their GP for an acute episode of LBP having persistent LBP 7 weeks later [35]. The difference between our results and those from the previous French study may seem paradoxical, since some of the patients in the previous study had severe symptoms (sciatica). The principal explanation for the difference probably lies in the definition of persistent back pain between the 2 studies: no pain in our study (a stricter definition, as patients undoubtedly define it), and no decrease in pain in the previous study. Finally, in the first French study, only 64% of patients were totally free from LBP.
Limitations
Randomized controlled trials are widely accepted as the criterion standard in assessing the effectiveness of specific therapies [42]. However, nonrandomized evaluation design is now widely accepted as quasi-experimental design that can contribute important data on the efficacy or effectiveness of interventions [43], [44], especially to evaluate public health interventions [31]. Moreover, quasi-experimental study designs that use control groups and pretests are considered to be the soundest of nonrandomized evaluations in terms of establishing causality [45]. In our study, the individual randomization of patients was not appropriate, since the GP was considered part of the intervention, which mainly consisting of information and education. GPs in the intervention arm were given the “back book” and those in the control group were not. Furthermore, during the course of our study, no LBP-centred intervention (press release or Heath Care Services intervention) that could have affected the evaluation of the impact of the “back book” was implemented in any of the included geographic areas. Finally, we did not perform a cluster randomized study by randomizing GPs practices to intervention or control because we assumed that the risk of contact between GPs in control and intervention practices during the trial would have been higher than with a quasi-experimental design with geographic stratification.
The main analysis was conducted on a per protocol population. However, the proportion of patients lost to follow-up (15%) is acceptable and was similar in both arms. Moreover, patients lost to follow-up did not differ from those evaluated at 3 months in terms of baseline characteristics. Finally, to provide data on an intention-to-treat basis, we conducted a sensitivity analysis using two scenarios (worst and best-case imputation), which were highly unrealistic.
Another possible limitation is that 2 procedures were used to record data at follow-up: visits to GPs and phone interviews. Phone interviews were used to decrease the number of patients lost to follow-up and were conducted by a trained research assistant. Outcome measures were easy to record by phone and the proportion of patients for whom data were collected by phone did not differ between the control and intervention groups. The difference in proportion of patients with persistent pain between phone and face-to-face interviews is probably a result of patient improvement. The patients without persistent pain were less likely to visit their doctors at 3 months than patients with persistent pain.
Only patients reporting persistent pain were reassessed at 3-month follow-up, which limits the ability of this study to detect effects of the intervention on outcome measures that may influence back-pain recurrence such as disability and fear-avoidance beliefs.
Finally, the sample size calculation did not take into account the cluster effect, which resulted in a lower power of our study, but which has no impact since the study results were positive.
Overall evidence
Low-tech and easy-to-disseminate interventions have enormous promise in LBP interventions. The level of improvement described in this study is modest, but the cost and complexity of the intervention is minimal. Therefore, the implications and generalizability of this intervention are substantial.
Supporting Information
CONSORT Checklist
(0.04 MB DOC)
Trial protocol
(2.15 MB PDF)
Translation of the abstract into French by Serge Poiraudeau
(0.02 MB DOC)
Acknowledgments
We are grateful to Laura Heraty for English reviewing of the manuscript. A translation of the abstract into French is available as Alternate Language Abstract S1.
Footnotes
Competing Interests: Honoria from Sanofi-Aventis
Funding: This study was funded by Sanofi-Aventis. The funding sponsor took part in the design and conduct of the study and collection, management, and analysis of the data. It was not involved in the writing and final approval of the manuscript. Independent data analysis was conducted by one of the authors (FT) who did not receive compensation or funding for conducting the analyses.
References
- 1.Anderson GB. Epidemiological features of chronic low back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 2.Waddell G. Edinburgh: Churchill Livingstone; 1998. The back pain revolution. p. 266. [Google Scholar]
- 3.Druss BG, Rosenheck RA, Sledge WH. Health and disability costs of depressive illness in a major US Corporation. Am J Psychiatry. 2000;157:1274–78. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- 4.Feurstein M, Beatie P. Behavioral factors affecting pain and disability in low back pain: mechanisms and assessment. Phys Ther. 1995;4:267–80. doi: 10.1093/ptj/75.4.267. [DOI] [PubMed] [Google Scholar]
- 5.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 6.Buchbinder R, Jolley D, Wyatt M. Population based intervention to change back pain beliefs and disability: three part evaluation. BMJ. 2001;322:1516–1520. doi: 10.1136/bmj.322.7301.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burton AK, Waddell G, Tillotson KM, Summerton N. Information and advise to patients with low back pain can have a positive effect: a randomized controlled trial of a novel educational booklet in primary care. Spine. 1999;24:2484–91. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 8.Recommendations of the Agence Nationale d'Accreditation et d'Evaluation en Sante. Diagnostic and therapeutic management of common lumbago and sciatica of less than 3 months of duration. J Radiol. 2000. 2000;81:1665–6. [PubMed] [Google Scholar]
- 9.Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, et al. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. 2000;25:1–33. doi: 10.1097/00007632-200002151-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Linton SJ, Morley SJ, et al. Behavioural treatment for chronic low-back pain. The Cochrane Database of Systematic Reviews Issue 2. 2005 doi: 10.1002/14651858.CD002014.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Hagen KB, Hilde G, Jamtvedt G, Winnem M. Bed rest for acute low-back pain and sciatica. The Cochrane Database of Systematic Reviews Issue 2. 2005 doi: 10.1002/14651858.CD001254. [DOI] [PubMed] [Google Scholar]
- 12.Hagen KB, Hilde G, Jamvedt G, Winnem MF. The Cochrane review of advice to stay active as a single treatment for low back pain and sciatica. Spine. 2002;27:1736–41. doi: 10.1097/00007632-200208150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332:1430–4. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malmivaara A, Koes BW, Bouter LM, van Tulder MW. Applicability and clinical relevance of results in randomized controlled trials: the Cochrane review on exercise therapy for low back pain as an example. Spine. 2006;31:1405–9. doi: 10.1097/01.brs.0000219868.30427.66. [DOI] [PubMed] [Google Scholar]
- 15.Wessels T, van Tulder M, Sigl T, Ewert T, Limm H, et al. What predicts outcome in non-operative treatments of chronic low back pain? A systematic review. Eur Spine J. 2006;15:1633–44. doi: 10.1007/s00586-006-0073-4. [DOI] [PubMed] [Google Scholar]
- 16.van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, et al. On behalf of the COST B13 Working Group on Guidelines for the Management of Acute Low Back Pain in Primary Care. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15:S169–91. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15:S64–81. doi: 10.1007/s00586-005-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2005;30:2153–63. doi: 10.1097/01.brs.0000182227.33627.15. [DOI] [PubMed] [Google Scholar]
- 19.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. The Cochrane Database of Systematic Reviews Issue 3. 2005 doi: 10.1002/14651858.CD000335.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breen AC, van Tulder MW, Koes BW, Jensen I, Reardon R, et al. Mono-disciplinary or multidisciplinary back pain guidelines? How can we achieve a common message in primary care? Eur Spine J. 2006;15:641–7. doi: 10.1007/s00586-005-0883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–85. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 22.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–75. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 23.Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W. Pitfalls of patient education. Limited success of a program for back pain in primary care. Spine. 1996;21:345–55. doi: 10.1097/00007632-199602010-00019. [DOI] [PubMed] [Google Scholar]
- 24.Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339:1021–9. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 25.Roberts L, Little P, Chapman J, Cantrell T, Pickering R, et al. The back home trial: general practitioner-supported leaflets may change back pain behavior. Spine. 2002;27:1821–8. doi: 10.1097/00007632-200209010-00002. [DOI] [PubMed] [Google Scholar]
- 26.Royal College of General Practitioners. London: RCGP; 1996. Clinical Guidelines for the Management of Acute Low Back Pain. [Google Scholar]
- 27.Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339:1021–9. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 28.Udermann BE, Spratt KF, Donelson RG, Mayer J, Graves JE, et al. Can a patient educational book change behavior and reduce pain in chronic low back pain patients? Spine J. 2004;4:425–35. doi: 10.1016/j.spinee.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Hazard RG, Reid S, Haugh LD, McFarlane G. A controlled trial of an educational pamphlet to prevent disability after occupational low back injury. Spine. 2000;25:1419–23. doi: 10.1097/00007632-200006010-00015. [DOI] [PubMed] [Google Scholar]
- 30.Coudeyre E, Givron P, Gremeaux V, Lavit P, Herisson C, et al. French translation and cultural adaptation of the “Back Book”. Ann Readapt Med Phys. 2003;46:553–7. doi: 10.1016/j.annrmp.2003.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Breart G, Bouyer J. Epidemiological methods in evaluation. Rev Epidemiol Sante Publique. 1991;39:S5–14. [PubMed] [Google Scholar]
- 32.Pfingsten M, Kroner-Herwig B, Leibing E, Kronshage U, Hildebrandt J. Validation of the German version of the Fear-Avoidance Beliefs Questionnaire (FABQ). Eur J Pain. 2000;4:259–66. doi: 10.1053/eujp.2000.0178. [DOI] [PubMed] [Google Scholar]
- 33.Chaory K, Fayad F, Rannou F, Fermanian J, Revel M, et al. Validation of the French version of the Fear Avoidance Beliefs Questionnaire (FABQ). Spine 14. 2004;29:908–13. doi: 10.1097/00007632-200404150-00018. [DOI] [PubMed] [Google Scholar]
- 34.Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, et al. The Quebec Back Pain Disability Scale. Measurement properties. Spine. 1995;20:341–52. doi: 10.1097/00007632-199502000-00016. [DOI] [PubMed] [Google Scholar]
- 35.Valat JP, Goupille P, Rozenberg S, Urbinelli R, Allaert F. Acute low back pain: predictive index of chronicity from a cohort of 2487 subjects. Spine Group of the Societe Francaise de Rhumatologie. Joint Bone Spine. 2000;67:456–61. [PubMed] [Google Scholar]
- 36.Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12:223–32. doi: 10.1023/a:1020218422974. [DOI] [PubMed] [Google Scholar]
- 37.Roland M, Dixon M. Randomized controlled trial of an educational booklet for patients presenting with back pain in general practice. J R Coll Gen Pract. 1989;39:244–6. [PMC free article] [PubMed] [Google Scholar]
- 38.Buchbinder R, Jolley D. Population based intervention to change back pain beliefs: three year follow up population survey. BMJ. 2004;328:321. doi: 10.1136/bmj.328.7435.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Orr CJ. How to minimize litigation. Br J Hosp Med. 1989;42:439. [PubMed] [Google Scholar]
- 40.De Jong JR, Vlaeyen JW, Onghena P, Goossens MF, Geilen M, et al. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction. Clin J Pain. 2005;21:9–17. doi: 10.1097/00002508-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Raspe H, Matthis C, Croft P, O'Neill T. Variation in back pain between countries. Spine. 2004;29:1017–21. doi: 10.1097/00007632-200405010-00013. [DOI] [PubMed] [Google Scholar]
- 42.Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, et al. Factors that limit the quality, number and progress of randomised controlled trials. Health Technol Assess. 1999;3:1–143. [PubMed] [Google Scholar]
- 43.Godwin M, Ruhland L, Casson I, MacDonald S, Delva D, et al. Pragmatic controlled clinical trials in primary care: the struggle between external and internal validity. BMC Med Res Methodol. 2003;3:28. doi: 10.1186/1471-2288-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94:361–6. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harris AD, Bradham DD, Baumgarten M, Zuckerman IH, Fink JC, et al. The use and interpretation of quasi-experimental studies in infectious diseases. CID. 2004;38:1586–1591. doi: 10.1086/420936. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT Checklist
(0.04 MB DOC)
Trial protocol
(2.15 MB PDF)
Translation of the abstract into French by Serge Poiraudeau
(0.02 MB DOC)