Abstract
America's medical schools are gearing up for their biggest expansion in decades. But Jonathan P Weiner argues that more doctors is not the answer to the country's healthcare problems and calls for a more international approach
The American medical education community has reached a consensus that a shortage of doctors is looming. Several years of heated discourse, dominated by current and former medical school deans, culminated in an influential position paper by the American Association of Medical Colleges (AAMC) calling for an urgent and immediate expansion of US medical students by 30%.1
The arguments for expansion have been discussed fully elsewhere,2 3 4 5 They include the belief that patients will soon want and need more services than the current stock of doctors can provide, newly trained doctors will be unwilling or unable to see as many patients each week as in the past, and the US should not be so reliant on doctors trained abroad. But is there really a problem?
US workforce supply
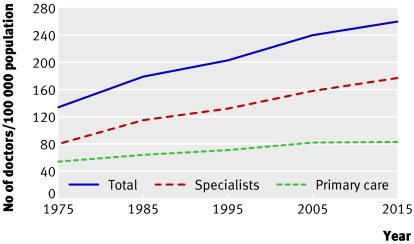
The supply of US doctors has grown faster than the patient population for many decades (fig 1). The proportion of doctors that are generalists has been falling fast. The ever growing importance of specialists in the US, and the plummeting popularity of primary care among new medical graduates has been understandably disquieting to the primary care specialty societies.6 7
Fig 1 Actual and forecasted US non-trainee doctors (MD and DO degrees) per 100 000 population, 1975-2015 (American Medical Association, American Osteopathic Association, 2006).4 Primary care includes family physicians, general internal medicine, and paediatrics
The pipeline for new American medical practitioners is multifaceted (box 1). Although the output of programmes training medical doctors has been level over the past few decades, schools training nurse practitioners, physicians assistants, and doctors of osteopathy (a uniquely American qualification) have grown exponentially.
US clinicians
Medical doctor (MD)—The degree takes four years of medical training after graduating from a four year baccalaureate. About 17 000 MD students entered medical school last year. There are currently about 800 000 trained MDs working in the US
Doctor of osteopathy (DO)—A physician trained equivalently to an MD, although originally based on a more holistic approach involving osteopathic manipulation. The US has around 50 000 trained DOs, and about 3800 entered osteopathy school last year
Nurse practitioner—Requires 1-3 years of training after obtaining registered nurse certification (which requires 3-4 years of training). 85% of nurse practitioners provide primary care. Around 70 000 are currently working in the US and 6500 graduate annually
Physicians assistant—A quasi-independent clinical practitioner who, with minimal supervision (from a doctor), can offer both primary and specialised clinical services including prescriptions. The training is generally four years at the baccalaureate level. Many courses were developed in close alliance with medical schools. About half of physician assistants practise in specialty areas and half in primary care. There are around 50 000 currently working, and 4600 graduate each year
Of the roughly 35 000 new clinical trainees who entered practice in 2006, less than half (43%) had a MD degree from the US; about 8% were osteopathic doctors, 32% were nurse practitioners or physician assistants, and 17% were doctors who trained outside the US. Currently more than 100 000 nurse practitioners and physician assistants are practising in the US. If these non-doctors are added into the mix, the number of clinicians per population increases by around 15% (from 240/100 000 to 277/100 000 in 2005).8
This unabated non-MD growth is, some believe, a major unspoken reason for the AAMC's call for expansion. In its doctor oriented analysis, the association (which represents only schools that grant MD degrees) does not explicitly consider the potential of these clinical trainees to do some of the work of medical doctors or whether expanding their numbers would be more cost effective than training more doctors.
The issue of international medical graduates is controversial. The US has long been a magnet for all types of well educated immigrants, including doctors. Today about 25% of all practising doctors in the US were trained abroad, and international graduates fill about the same proportion of postgraduate (residency) training slots. Calls are also growing for reassessment of the role of international graduates, not (overtly at least) because of protectionism or quality concerns but because of the ethical considerations of a global “brain drain.”9 10
Many parties believe that allowing the US to become more self sufficient is a valid reason to support the expansion of home grown doctors.9 However, without a comprehensive overhaul of medical and general immigration policy, more US trainees would not necessarily decrease the brain drain from developing nations. Moreover, if the larger number of US medical school graduates is to translate into more practising clinicians down the road, the number of postgraduate residency positions must increase concomitantly. Otherwise the expanded pool of US graduates will displace the large cohort of international graduates now in these positions and there would be no net gain of doctors.
Assessing the need
Not everyone agrees that the AAMC's plan for 30% growth is supported by evidence.11 12 13 In the resource rich, fee for service US healthcare system, doctors can easily keep their offices busy with well insured patients who have come to equate intensive care with better care. However, population based research suggests that above a certain threshold, more is not better. As use of services increases, quality and health related outcomes (at least to the degree we can currently measure it) do not improve.
For example, two recent studies (one at the US county level, the other at state level) show that as the supply of specialists per population increases, indicators of quality of care decrease, costs increase, and population mortality does not change. However, the same studies show that as the generalist supply increases, quality increases and both cost and mortality decrease.14 15
Another argument against the need for expansion is that high quality, efficient care can be delivered with far fewer doctors than the AAMC calls for. This is shown by comparisons between areas with low and high doctor supply in the US, doctor supply ratios in other countries, and US organised practice settings such as health maintenance organisations.16 17
Although more doctors could increase access to care for those who need it, past expansions have only modestly benefited regions with shortages; far more doctors have been added to areas with high supply. Programmes that offer targeted incentives (such as paying off loans) to young doctors who practise in areas of special need, are a more efficient way to ensure even distribution than blanket subsidies to all training programmes.13 17
For several reasons—including the lack of central control and population focus—there has been almost no public discourse on issues surrounding medical workforce. Specifically, is the annual public sector investment of $3bn-$5bn (£1.5bn-£2.5bn; €2bn-€4bn) necessary to expand medical training the best use of resources to improve population health? In a nation that already has one well trained clinician for every 320 patients, and at the same time has over 45 million residents with no health insurance and tens of millions receiving third world levels of care, could these added health care dollars be used more effectively in other ways? This is not the type of question American health policymakers are used to asking; but it should be.
Global context
How does the supply of doctors in the US compare with that in the UK and other countries? The current medical education expansion plans in the US have direct parallels in the UK. The UK's medical education capacity has grown by about 50% over the past decade, and from 2008, training slots are likely to be increased even further.18
Most people assume that the UK has far fewer doctors per person and a far higher percentage of generalists than the US. But this historical notion is no longer accurate. Britain is fast approaching the US in terms of its overall level of total doctors per person and, surprisingly, the percentage of practising doctors trained as generalists in England will soon be lower than in America. As recently as 1995, the US had 83% more practising (non-trainee) doctors than England per person. In that year, 52% of all English practising doctors were generalists19 20; far higher than the comparable rate in the US (35%). By 2005, the gap narrowed slightly. The US had 70% more doctors per capita than England and the proportion of English doctors that were general practitioners decreased to 45% (table).
Numbers of doctors per 100 000 population in England and US, 1995 and 2005
| England19 | US* | ||||||
|---|---|---|---|---|---|---|---|
| Primary care | Specialist | Total | Primary care† | Specialist | Total | ||
| 1995 | |||||||
| Trained only | 58 | 53 | 111 | 71 | 132 | 203 | |
| Including trainees‡ | 64 | 106 | 170 | 86 | 153 | 239 | |
| 2005 | |||||||
| Trained only | 64 | 78 | 142 | 82 | 158 | 240 | |
| Including trainees‡ | 78 | 157 | 235 | 95 | 179 | 274 | |
*Data from US Department of Health and Human Services, 2005; American Medical Association, 2006; and American Osteopathy Association, 2006.
†Includes family physicians and specialists in general internal medicine and paediatrics.
‡House officers and registrars or foundation years 1 and 2 in England and house staff in training in US.
Comparisons of only doctors who have finished their training is misleading in the case of the UK. About 40% of all British medical school graduates are still in the education pipeline; more than three times the US rate of 13%. When all active doctors (including trainees) are compared, the total number of active and trainee doctors combined is only 16% higher in the US than in England (table). Moreover, the proportion (33%) of English doctors trained or training as general practitioners is now a bit lower than the comparable rate of generalist doctors in the US (35%).
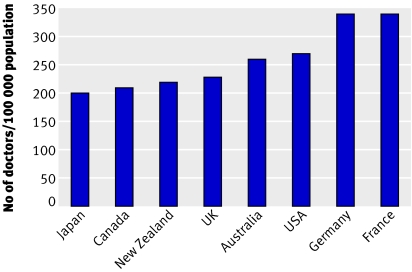
Comparison with several other developed countries in 2004, the most recent year for which statistics are available from the Organisation for Economic Cooperation and Development,21 shows that the numbers of doctors (including trainees) in the US and UK fall towards the middle of the range (fig 2).
Fig 2 Doctors per 100 000 population for selected countries in the Organisation for Economic Cooperation and Development, 2004.21 Some countries have higher and lower ratios, ranging from 140/100 000 in Turkey to 490/100 000 in Greece
What can we learn from this natural experiment in doctor staffing? Just as the US data do not show a clear positive relation between more providers and better outcomes, it is hard to see linkages between more doctors and improved health in these countries. However, as patient populations age and societies get wealthier, patients have come to expect more and better services. Countries with a higher number of doctors seem to do a better job of meeting those expectations.22
Conclusions
The US healthcare system is consumer focused but often inequitable and non-rational. In contrast, the NHS has a long history of equity and rationality, if not always bottom-up consumerism. It is interesting that the approaches to medical workforce staffing within the two nations are in many ways converging.
The next few years will be crucial for planners, policymakers, educators, managers, and researchers concerned with ensuring a well trained cadre of medical practitioners. Many shared issues are likely to be confronted. One example, is how to get the right medical workforce, in terms of both overall number and relative mix. The answer will be coloured by context. Just as many in the US are concerned with impending shortages, the UK may be facing an overabundance of doctors. Will all the young doctors find posts to their liking? Will the concerns of US primary care advocates regarding an inappropriate dominance of specialists be a harbinger of things to come for the UK? International research into these and other related issues will be essential.
Medical workforce policy challenges are becoming ever more global. Leaders of health policy and medical education have much to gain from a shared international research and policy analysis framework. Box 2 suggests some priorities.
Box 2 Priorities for international research on medical workforce
Forecasting and measuring supply, demand, and need
Evolving roles of primary and specialty care
Best way to structure and staff health care organisations to maximise population benefit
Roles of alternative professionals
Ways to encourage doctors to practise in less desirable settings
Approaches for assessing and assuring provider efficiency and productivity
Ways to predict and ethically manage patterns of international medical migration
The objective of all this is to find creative and financially feasible ways to produce a medical workforce that balances clinical need, consumer preference, professional aspirations, and population equity. Although accomplishing this will hardly be easy, it will be essential.
Summary points
Above a certain threshold, there is little evidence that more doctors add to health of population
Many countries, US regions, and health maintenance organisations provide superior care with fewer doctors per person than the current US national ratio
Forecasts of a future US doctor shortage do not adequately consider the availability of other clinical providers
Information technology and preventive healthcare may increase productivity and decrease patient demand
The billions to be spent on expanding US medical training would be better spent on meeting the needs of citizens without access to basic care
I thank Barbara Starfield, Atul Grover, and Azeem Majeed for reviewing earlier versions of this article and Tanaz Petigara and Samantha Flanzer for help with research.
Contributors and sources: JPW is a health care policy researcher and analyst who has worked in the health care workforce area for over 25 years. In the US he is well known as an advocate for population based assessments of workforce that emphasise needs based planning and a strengthened role for primary care. He has done extensive health policy and health services research in the UK over the past two decades, most recently as an Atlantic fellow based in London during 1999-2000.
Competing interests: JPW has received private and government grants and contracts to do research on this topic but currently has no income from this area.
References
- 1.Association of American Medical Colleges. AAMC statement on the physician workforce 2006. www.aamc.org/workforce/workforceposition.pdf
- 2.Cooper RA, Getzen TE, McKee HJ, Laud P. Economic and demographic trends signal an impending physician shortage. Health Aff (Milwood) 2002;21:140-54. [DOI] [PubMed] [Google Scholar]
- 3.Cooper RA. Weighing the evidence for expanding physician supply. Ann Intern Med 2004;141:705-14. [DOI] [PubMed] [Google Scholar]
- 4.Council on Graduate Medical Education. Physician workforce policy guidelines for the United States, 2000-2020 Washington, DC: US Department of Health and Human Services, 2005. www.cogme.gov/16.pdf
- 5.Blumenthal D. New steam from an old cauldron—the physician supply debate. N Engl J Med 2004;350:1780-7. [DOI] [PubMed] [Google Scholar]
- 6.Green LA, Dodoo MS, Ruddy G, Fryer GE, Phillips RL, McCann JL, et al. The physician workforce of the United States. A family medicine perspective Washington, DC: Robert Graham Center, 2004. www.graham-center.org/PreBuilt/physician_workforce.pdf
- 7.Sandy LG, Schroeder SA. Primary care in a new era: disillusion and dissolution? Ann Intern Med 2003;138:262-7. [DOI] [PubMed] [Google Scholar]
- 8.Hooker RS. Physician assistants and nurse practitioners: the United States experience. Med J Aust 2006;185:4-7. [DOI] [PubMed] [Google Scholar]
- 9.Mullan F. The metrics of the physician brain drain. N Engl J Med 2005;358:1810-8. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad OB. Managing medical migration from poor countries. BMJ 2005;331:43-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiner J. A shortage of physicians or a surplus of assumptions? Health Aff (Milwood) 2002;21:160-2. [DOI] [PubMed] [Google Scholar]
- 12.Grumbach K. Fighting hand to hand over physician workforce policy. Health Aff (Milwood) 2002;21:13-27. [DOI] [PubMed] [Google Scholar]
- 13.Goodman DC. The physician workforce crisis: where is the evidence? Health Aff (Milwood) 2005;web exclusives:W5-108-W5-110. [DOI] [PubMed]
- 14.Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations' health: assessing the evidence. Health Aff 2005;web exclusives:W5-97-W5-107. [DOI] [PubMed]
- 15.Baicker K, Chandra A. Medicare spending, the physician workforce, and beneficiaries quality of care. Health Affairs (Milwood)2004;web exclusives:W4-184-97. [DOI] [PubMed]
- 16.Weiner JP. Prepaid group practice staffing and US physician supply: lessons for workforce policy. Health Aff (Milwood) 2005;web exclusives:W4-43-59. [DOI] [PubMed]
- 17.Goodman DC. Twenty-year trends in regional variations in the US physician workforce. Health Aff (Milwood) 2004;web exclusives:VAR90-7. [DOI] [PubMed]
- 18.Bloor K, Hendry V, Maynard A. Do we need more doctors? J R Soc Med 2006;99:281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Information Centre. General and personal medical services in England: 1996-2005 www.ic.nhs.uk/statistics-and-data-collections/workforce/nhs-numbers/general-and-personal-medical-services-2005-detailed-results
- 20.NHS hospital and community health workforce. Information Centre. www.ic.nhs.uk/statistics-and-data-collections/workforce/nhs-hospital-and-community-workforce
- 21.Organisation for Economic Cooperation and Development. Statistics for 2004. Paris: OECD, 2006. www.oecd.org/statisticsdata/0,3381,en_2649_37407_1_119656_1_1_37407,00.html
- 22.Simoens S, Hurst J. The supply of physician services in OECD countries OECD Health Working Papers, 2006. www.oecd.org/dataoecd/27/22/35987490.pdf