Abstract
Objective
To determine the effectiveness of lithium prophylaxis in unipolar major depressive disorder (MDD) and to identify predictors of outcome including comedication.
Methods
In this long-term naturalistic study, clinical data from 55 patients with MDD (DSM-III-R) were collected prospectively in an outpatient clinic specializing in the treatment of affective disorders.
Outcome measures
Change in hospital admission rate (number and duration) during prophylaxis compared with the period before prophylaxis, Morbidity-Index during prophylaxis and time to first recurrence after initiation of lithium treatment.
Results
During an average follow-up period of 6.7 years, a significant decline in the number of days spent in hospital (p < 0.001; 52 d/yr less; 95; CI 31–73 d) and a low Morbidity-Index (mean 0.07) was observed. Only in 6 patients did medication have to be changed because of side-effects (n = 4) or a lack of efficacy (n = 2). None of the independent variables we analyzed proved to be important in predicting the outcome of lithium prophylaxis. Comedication was necessary in 21 patients. The overall outcome of their prophylactic treatment, however, did not differ from the group that did not receive comedication in the symptom-free intervals.
Conclusions
The results of this study, with its long observation period and the inclusion of comedication as a confounding variable, indicate that lithium is a potent prophylactic agent for unipolar MDD in a naturalistic setting. In contrast to the findings of others, age was not associated with the outcome of prophylaxis, and latency did not predict outcome. Contrary to doubts that have been raised in recent years with regard to the effectiveness of lithium in everyday clinical practice, lithium appears to be a safe and potent alternative to antidepressants.
Medical subject headings: depressive disorder; drug therapy, combination; lithium carbonate; treatment outcome
Abstract
Objectif
Déterminer l'efficacité d'un traitement prophylactique faisant appel au lithium dans les cas de trouble dépressif majeur (TDM) unipolaire, et définir les prédicteurs du résultat, y compris l'administration concomitante de médicaments.
Méthodes
Dans cette étude naturaliste à longue échéance, des données cliniques sur 55 patients atteints de TDM (DSM-III-R) ont été recueillies prospectivement dans une clinique externe spécialisée dans le traitement des troubles affectifs.
Mesures de résultat
Variation du taux d'hospitalisation (nombre de cas et durée) au cours du traitement prophylactique par rapport à la période avant la prophylaxie, indice de morbidité au cours du traitement prophylactique et période écoulée avant la première récidive suite au début du traitement au lithium.
Résultats
Au cours d'une période de suivi moyenne de 6,7 ans, on a observé un fléchissement important du nombre de jours d'hospitalisation (p < 0,001; 52 j/an de moins; IC à 95 %, 31–73 j) et un faible indice de morbidité (moyenne 0,07). Il a fallu changer le médicament à cause d'effets secondaires (n = 4) ou d'une efficacité insuffisante (n = 2) chez six patients seulement. Les variables indépendantes que nous avons analysées ne se sont pas révélées importantes comme prédicteurs du résultat du traitement prophylactique au lithium. Il a fallu recourir à l'administration concomitante d'autres médicaments chez 21 patients. Chez ces sujets, le résultat global du traitement prophylactique n'était toutefois pas différent de celui observé dans le groupe des patients pour lesquels on n'a pas recouru à l'administration concomitante d'autres médicaments au cours de l'intervalle sans symptôme.
Conclusions
Les résultats de cette étude, qui repose sur une longue période d'observation et sur l'inclusion de l'administration concomitante d'autres médicaments comme variable confusionnelle, indiquent que le lithium est un médicament prophylactique efficace contre le TDM unipolaire dans un contexte naturaliste. Contrairement aux constatations d'autres instances, on n'a pas établi de lien entre l'âge et le résultat du traitement prophylactique, et la latence n'était pas un prédicteur du résultat. Il semble qu'à l'encontre des doutes qui ont été émis ces dernières années au sujet de l'efficacité du lithium dans la pratique clinique de tous les jours, il s'agisse d'une solution de rechange efficace et sans danger aux antidépresseurs.
Introduction
Major depressive disorder (MDD) is a severe mood disorder associated with significant morbidity and mortality that affects individuals of all ages and races. The World Health Organization's recent Global Burden of Disease Study claims that depression is one of the most important public health concerns.1 There is a considerable need for prophylactic treatment in recurrent MDD.2,3,4 However, it has been estimated that up to 50% of patients, including even those who suffer multiple relapses, do not receive prophylactic therapy.5 Angst and Preisig2 reported that less than 10% of their Zurich cohort of 137 patients with unipolar depression received prophylaxis.
A considerable amount of data shows lithium to be an effective agent in the prophylaxis of MDD,6,7,8 although the evidence is less clear than in the case of bipolar disorder. However, some studies have shown lithium to be as effective as antidepressants in the prophylaxis of recurrent depression.6,7,8,9 There is also preliminary evidence that lithium has an antisuicidal effect in the treatment of MDD.10 It is noteworthy from a historical point of view that the Danish physician Carl Lange (1834–1900) reported as early as the nineteenth century on the successful prophylactic use of lithium in recurrent depression.11,12
An international task force from the World Federation of Societies of Biological Psychiatry recently recommended lithium in their treatment guidelines for maintenance therapy of MDD.13 In contrast, the American Psychiatric Association guidelines for the treatment of depressive disorders do not mention lithium as a prophylactic agent.14 Furthermore, the effectiveness of lithium prophylaxis in everyday clinical practice has been questioned in recent years.15
Most studies on the prophylactic use of lithium in the treatment of MDD have had relatively short follow-up periods. To our knowledge, the longest controlled study to date followed up patients for 2.5 years.16 Some studies have shown lithium to have a stabilizing but not necessarily prophylactic effect after depressive episodes, leading several authors to call for longer follow-up periods to determine the long-term effectiveness of lithium in this context.17,18 Unfortunately, controlled or even double-blind studies with such extended follow-up periods, while of great clinical interest, are difficult to conduct in practice.
One way of studying the long-term outcome of prophylaxis in MDD is to conduct well-documented naturalistic investigations. However, there have been few such studies with observation periods of more than 2 or 3 years. Lepkifker and coworkers19 reported on 33 patients with unipolar depression who underwent more than 8 years of lithium prophylaxis on average. They observed a dramatic decline rate and durations of hospital admissions when they compared the time after with the time before the initiation of prophylactic therapy. In addition, they found a positive correlation between the number of episodes before lithium therapy and a worse outcome. Maj and coworkers20 also found more prior episodes to be a predictor of worse outcome. In their study, lithium showed a similarly impressive prophylactic effect in the treatment of recurrent unipolar depression.
Another problem with most studies on the prophylactic use of lithium in recurrent MDD concerns the role of comedication, especially antidepressants. Not taking comedication into account may potentially have blurred the results of these investigations.
The ongoing debate on the efficacy and effectiveness of lithium in unipolar MDD, as well as the lack of long-term studies and data regarding comedication prompted us to conduct the present analysis. Our goals were to assess the prophylactic effectiveness of lithium in a group of patients with unipolar MDD over an extended period of time in a naturalistic setting and to investigate the impact of comedication and several other clinical and demographic predictors on the outcome of prophylactic treatment.
Methods
This open prophylaxis study was performed in an outpatient clinic specializing in the long-term treatment of affective disorders (Berlin Lithium Clinic). The clinic is part of the Department of Psychiatry at the Freie Universität Berlin (tertiary care hospital). Patients visited the clinic every 1–12 weeks, depending on their clinical status. Visits consisted of a psychiatric clinical interview and an assessment of lithium serum levels (target levels 0.6–0.9 mmol/L), in addition to other routine laboratory tests. Psychopathological status was assessed using the Bech–Rafaelsen Melancholia Scale.21 Depressive episodes were treated according to the standards of antidepressant pharmacotherapy. All clinical data were collected prospectively. Upon admission to the clinic, patients were fully informed about the scientific purpose of the study before giving their written informed consent. (For details of the clinical setting, see Berghöfer et al.22)
Inclusion criteria
Patients who fulfilled the following criteria were included in the analysis:
· age 18 years or above
· a confirmed diagnosis of recurrent unipolar major depressive disorder (DSM-III-R). Diagnoses were verified using a checklist of DSM-III-R criteria for recurrent depressive disorder. Consensus diagnoses were made by the attending psychiatrist and other research psychiatrists during a meeting held for this purpose. The psychiatrists had at their disposal additional information about the patient from a semistructured diagnostic interview, including demographic characteristics and psychiatric history. For some patients, the diagnoses had to be confirmed retrospectively on the basis of a thorough chart review
· prophylactic treatment with lithium for at least 3 months
· no previous trial or concomitant use of any one mood stabilizer (carbamazepine or valproate) for more than 3 months
Maintenance treatment with lithium was initiated when the patient was admitted to the clinic. At this point, the patients were in remission. Data on earlier periods of illness were collected retrospectively using clinical interviews and chart analyses. In our opinion, the number of days spent in hospital is the most reliable parameter for assessing illness severity before admission to our clinic (i.e., the start of lithium). This same parameter is also the most dependable means of comparing the course of illness before and during lithium prophylaxis (i.e., response). However, to improve validity in our search for potential predictor variables, we decided to apply another approach using collected data prospectively. As a result, the dependent variables in the predictor search (as opposed to the calculation of response) are Morbidity-Index23 (MI) and time to first recurrence.
Outcome analyses in predictor search
1. The MI allows the course of illness to be documented in a more realistic and accurate manner than other measures of disease (e.g., hospital admissions or episodes). During episodes, the severity of psychopathology was assessed on a weekly basis and characterized by degrees of 1 (i.e., mild symptoms without need for additional treatment), 2 (i.e., additional psychotropic treatment) or 3 (i.e., need for inpatient care). The duration of symptoms was recorded in weeks. The MI could only be determined for the time of lithium prophylaxis and was calculated according to the following formula:
(wks of degree 1) х 1 + (wks of degree 2) х 2 + (wks of degree 3) х 3
Total observation time in weeks
2. The time elapsed until the first recurrence of an illness episode (according to DSM-III-R criteria) during prophylactic treatment was also recorded as a parameter of outcome.
Due to the fact that long-term treatment is probably influenced by several independent variables, we chose a multivariate approach for the analysis. The choice of predictor variables was based on established demographic and clinical measures for affective disorders.2 The independent variables were:
· antidepressant comedication of at least 50 mg imipramine equivalent per day for at least 3 months (the use of antidepressant medication during relapses — acute treatment medication — was not included)
· latency, or the time elapsed between onset of illness (definition below) and the first prophylactic treatment with lithium
· illness severity, determined by the number of days per year spent in hospital before prophylactic treatment
· age at onset of illness, defined as age at the time of the first medical contact due to the disorder as stated by the patient
· number of psychiatric admissions before the start of prophylaxis
· family history of affective disorders in first-degree relatives (yes/no)
· sex
Statistical analysis
Multivariate statistics were used to analyze the data. Statistical evaluation was conducted according to descriptive statistical methods for the calculation of average values and rates. For the identification of predictors (see above for independent variables), a multiple linear regression analysis with the MI as the dependent variable was applied. Survival analyses of the time to the first recurrence were performed using Cox regression with the same independent variables used in the regression analysis. A level of significance of 5% was established, with a 2-tailed test for all analyses.
Results
Fifty-five patients with a median age of 36.5 years at illness onset fulfilled the inclusion criteria. (For demographic and clinical characteristics, see Table 1 and Table 2). On average, 11.4 years of illness and 2.4 hospital admissions had passed before lithium prophylaxis was initiated. Patients were followed up for an average of 6.7 years (standard deviation [SD] 7.4 yr) during lithium prophylaxis. Beginning treatment earlier was correlated with greater illness severity before prophylaxis (as measured by days spent in hospital per year). This indicates that the more severe cases started earlier with lithium prophylaxis than the less severe cases (Spearman's rho –0.79, p < 0.01).
Table 1

Table 2
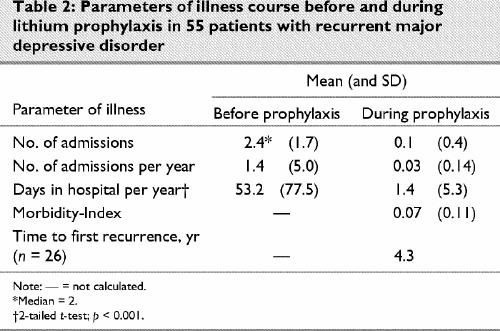
Twenty-six patients (47%) experienced at least 1 recurrence during lithium prophylaxis. Among those who relapsed, the first recurrence occurred after an average of 4.3 years. Fig. 1 shows the estimated survival curve of the entire sample as calculated by the Kaplan-Meier method. The number of days spent in hospital fell dramatically from an average of 53 per year before lithium prophylaxis to 1.4 days per year during prophylactic treatment (p < 0.001; 95% confidence interval 31–73 d). There was also a remarkable decrease in the number of psychiatric admissions (Table 2).
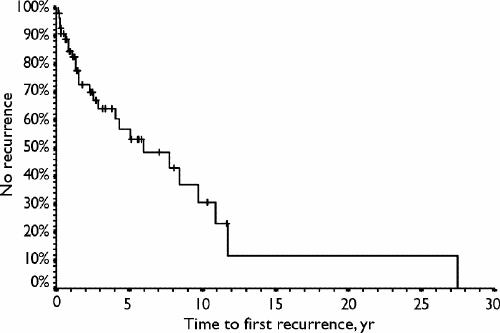
Fig. 1: Survival analysis of time to first recurrence using the Kaplan-Meier method (n = 55).
Twenty-one patients (38%) received antidepressant medication for more than 3 months (i.e., they were prescribed antidepressants for maintenance therapy). During an average of 8.5 years of lithium prophylaxis, this group of patients received antidepressant comedication for an average of 2.9 years. The subgroup of patients receiving comedication (n = 21) did not differ significantly from the subgroup that did not (n = 34) on any of the clinical or demographical variables assessed in this study (data not shown).
At the end of the observation period, 14 patients were still being treated with lithium and 6 had discontinued therapy in accordance with the treating physician after an extended symptom-free interval. Nine patients had moved or died (for reasons not related to lithium), and 9 patients were not compliant. It is noteworthy that only 4 patients (7%) discontinued lithium treatment because of side-effects, and only 2 patients had to switch drug regimens because of a lack of efficacy.
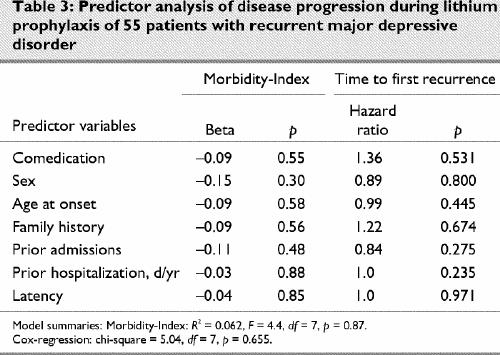
None of the independent variables were associated with treatment outcome. This applies to the prediction of the MI, to the time to first recurrence (Table 3) and also to the change in hospital admission rate when compared with the time before prophylaxis (data not shown).
Table 3
Discussion
Two important findings emerged from our study of lithium in the long-term prophylactic treatment of recurrent unipolar MDD: (1) the course of the illness was significantly improved during lithium treatment, and (2) none of the clinical and demographic variables predicted prophylaxis outcome.
The significant decline in hospitalization during prophylactic treatment is in line with observations made by other researchers. For example, Lepkifker and coworkers19 observed a similarly impressive decline in both rate and duration of hospital admissions in their study of 33 unipolar patients. In our study, not only did the hospitalization rate decline dramatically during prophylaxis, but the rather low MI indicates that even outpatient care (in addition to lithium) was rarely necessary. Moreover, only in a few patients did lithium have to be discontinued. It is of note that no suicides occurred during the prophylaxis, which is compatible with observations of a possible antisuicidal effect of lithium in unipolar disorder.10
The 21 patients who did require treatment with antidepressants in addition to lithium received antidepressants for a comparably short period of time. On average, the duration of comedication (2.9 yr) amounted to one-third of the follow-up period (8.4 yr in the group of 21 who received comedication). It is worth noting that the course of illness among these 21 patients neither worsened nor improved during prophylaxis as compared with the group of patients that did not require additional antidepressants. Because there were no group differences, we cannot comment on which patients would most likely benefit from treatment with additional antidepressant medication. However, one should bear in mind that our groups were small and that real differences might have been detected with larger groups.
In summary, the results of our study confirm findings reported both in controlled trials and in naturalistic observations on the efficacy and effectiveness of lithium in the treatment of recurrent unipolar MDD. However, this study is unique in that it shows the outcome under routine clinical conditions in a lithium clinic after a very long follow-up period, while at the same time considering the role played by comedication.
None of our variables were predictors of prophylaxis outcome. It is of note that we could not replicate the important role of the number of preceding episodes as a predictor of worse outcome. This is in contrast to observations made by several other researchers.19,20 Apart from other methodological and sample differences, it is conceivable that this is related to differences in statistical analyses. Lepkifker and coworkers19 dichotomized their sample (good v. bad response), whereas we applied a multiple linear regression analysis.
To our knowledge, this study is the first to investigate the significance of latency (the time between illness onset and start of prophylaxis) for prophylaxis outcome in recurrent unipolar MDD. The role of latency in disease progression has received a great deal of attention in association with the kindling hypothesis of affective disorders24,25 and also because of observations indicating that patients treated early in the course of their illness have a more favourable outcome.26 In previous studies, we showed, too, that latency is not an important predictor in the success or failure of prophylactic treatment in bipolar or in schizoaffective disorder.27,28,29 In our sample of unipolar patients, latency was also not predictive of the outcome of prophylactic therapy. However, starting prophylaxis earlier was correlated with higher illness severity, as measured in days in hospital before prophylaxis, indicating that the most severe cases were treated earlier. Although our findings indicate that latency does not play a decisive role in the success or failure of prophylactic treatment, this does not mean that we encourage patients to begin prophylaxis later in the course of their illness. There are many reasons to start prophylaxis of affective disorders early, but the hypothesis that lithium becomes less effective in the later stages of the illness is probably not one of them.
Of course, the naturalistic approach taken in this study limits the conclusions that can be drawn from our findings. By its very nature, the non-randomized, open and uncontrolled design of this study does not allow us to determine the efficacy of lithium prophylaxis with any great precision. On the other hand, conducting a controlled follow-up study with an observation period as long as ours would hardly be feasible. In contrast to controlled trials, which include highly selected patient populations, naturalistic studies have the advantage of offering important insights into everyday clinical practice.30
There is currently no doubt that antidepressants are the most important compounds in the long-term treatment of recurrent depression.13,14 However, it is not clear from this study which patients should be treated preferably with antidepressants and which patients with lithium. Administration of lithium for prophylactic purposes in recurrent unipolar depression might be considered in cases in which the risk of suicide is particularly high or if patients have a family history of bipolar disorder and are, therefore, at a higher risk to develop manic episodes.
Future research should focus on a comparison of mood stabilizers and antidepressants, while at the same time considering additional predictors such as comorbidity or the characteristics of the course of illness (e.g., full remission v. chronic course).
In summary, lithium appears to be a potent and safe alternative to antidepressants in the prophylaxis of recurrent major depressive disorder.
Footnotes
Competing interests: None declared.
Correspondence to: Dr. Christopher Baethge, Mailman Research Center, McLean Division of Massachusetts General Hospital, 115 Mill St., Belmont, MA 02478-9106; fax 617 855-3479; cbaethge@mclean.harvard.edu
Submitted July 17, 2002 Revised Dec. 11, 2002 Accepted Feb. 11, 2003
References
- 1.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 1997;349:1436-42. [DOI] [PubMed]
- 2.Angst J, Preisig M. Outcome of a clinical cohort of unipolar, bipolar and schizoaffective patients. Results of a prospective study from 1959 to 1985. Schweiz Arch Neurol Psychiatr 1995; 146: 17-23. [PubMed]
- 3.Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry 1999;156:1000-6. [DOI] [PubMed]
- 4.Bauer M, Whybrow PC, Angst J, Versiani M, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for biological treatment of unipolar depressive disorders, Part 1: Acute and continuation treatment of major depressive disorder. World J Biol Psychiatr 2002;3:5-43. [DOI] [PubMed]
- 5.Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea T, et al. Multiple recurrences of major depressive disorder. Am J Psychiatry 2000;157:229-33. [DOI] [PubMed]
- 6.Kane J, Quitkin F, Rifkin A, Ramos-Lorenzi JR, Nayak DD, Howard A. Lithium carbonate and imipramine in the prophylaxis of unipolar and bipolar II illness. Arch Gen Psychiatry 1982; 38:1065-9. [DOI] [PubMed]
- 7.Glen A, Johnson A, Shepherd M. Continuation therapy with lithium and amitriptyline in unipolar depressive illness: a randomized, double-blind, controlled trial. Psychol Med 1981; 14: 37-50. [DOI] [PubMed]
- 8.Davis JM, Janicak PG, Hogan DM. Mood stabilizers in the prevention of recurrent affective disorders: a meta-analysis. Acta Psychiatr Scand 1999;100:406-17. [DOI] [PubMed]
- 9.Franchini L, Zanardi R, Gasperini M, Perez J, Smeraldi E. Fluvoxamine and lithium in long-term treatment of unipolar subjects with high recurrence rate. J Affect Disord 1996;26:67-9. [DOI] [PubMed]
- 10.Müller-Oerlinghausen B, Wolf T, Ahrens B, Schou M, Grof E, Grof P, et al. Mortality during initial and during later lithium treatment: a collaborative study by the International Group for the Study of Lithium-treated Patients (IGSLi). Acta Psychiatr Scand 1994;90:295-7. [DOI] [PubMed]
- 11.Lange C. Om periodiske Depressionstilstande og deres Patogenese. Copenhagen: Jacob Funds Forlag; 1886.
- 12.Felber W. Lithium prevention of depression 100 years ago — an ingenious misconception [in German]. Fortschr Neurol Psychiatr 1987 ; 55: 141-4. [DOI] [PubMed]
- 13.Bauer M, Whybrow PC, Angst J, Versiani M, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for biological treatment of unipolar depressive disorders, Part 2: Maintenance treatment of major depressive disorder and treatment of chronic depressive disorders and subthreshold depressions. World J Biol Psychiatr 2002;3:67-84. [DOI] [PubMed]
- 14.Practice guideline for the treatment of patients with major depressive disorder (revision). American Psychiatric Association. Am J Psychiatry 2000;157(4 Suppl);1-45. [PubMed]
- 15.Moncrieff J. Lithium: evidence reconsidered. Br J Psychiatry 1997; 171: 113-9. [DOI] [PubMed]
- 16.Greil W, Ludwig-Mayerhofer W, Erazo N, Engel RR, Czernik A, Giedke H, et al. Comparative efficacy of lithium and amitriptyline in the maintenance treatment of recurrent unipolar depression: a randomised study. J Affect Disord 1996;40:179-90. [DOI] [PubMed]
- 17.Baldessarini RJ, Tohen M. Is there a long-term protection effect of mood-altering agents in unipolar affective disorders? In: Casey DE, Christensen AV, editors. Psychopharmacology: current trends. Berlin: Springer-Verlag; 1988. p. 130-9. [DOI] [PubMed]
- 18.Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press; 1990. p. 693-4.
- 19.Lepkifker E, Horesh N, Floru S. Long-term lithium prophylaxis in recurrent unipolar depression. Acta Psychiat Belg 1985; 85: 434-43. [PubMed]
- 20.Maj M, Veltro F, Pirozzi R, Lobrace S, Magliano L. Pattern of recurrence of illness after recovery from an episode of major depression: A prospective study. Am J Psychiatry 1992;149:795-800. [DOI] [PubMed]
- 21.Bech P. Rating scales for mood disorders: applicability, consistency and construct validity. Acta Psychiatr Scand 1988; 78 (Suppl 345): 45-55. [DOI] [PubMed]
- 22.Berghöfer A, Kossmann B, Müller-Oerlinghausen B. Course of illness and pattern of recurrences in patients with affective disorders during long-term lithium prophylaxis: a retrospective analysis over 15 years. Acta Psychiatr Scand 1996;93:349-54. [DOI] [PubMed]
- 23.Coppen A, Abou-Saleh MT. Plasma folate and affective morbidity during long-term lithium therapy. Br J Psychiatry 1982; 141:87-9. [DOI] [PubMed]
- 24.Post R. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 1992; 149: 999-1010. [DOI] [PubMed]
- 25.Post R, Weiss SRB. Neurobiological models of recurrence in mood disorder. In: Charney DS, Nestler EJ, Bunney BS, editors. Neurobiology of mental illness. Oxford: Oxford University Press; 1999.
- 26.Franchini L, Zanardi R, Smeraldi E, Gasperini M. Early-onset of lithium prophylaxis as a predictor of good long-term outcome. Eur Arch Psychiatry Clin Neurosci 1998;249:227-30. [DOI] [PubMed]
- 27.Baethge C, Smolka MN, Gruschka P, Berghofer A, Schlattmann P, Bauer M, et al. Does prophylaxis-delay in bipolar disorder influence outcome? Results from a long-term study of 147 patients. Acta Psychiatr Scand 2003;107(4):260-7. [DOI] [PubMed]
- 28.Baethge C, Gruschka P, Berghöfer A, Bauer M, Müller-Oerlinghausen B, Bschor T, et al. Prophylaxis of schizoaffective disorder with lithium or carbamazepine: outcome after long-term follow-up. J Affect Disord. In press. [DOI] [PubMed]
- 29.Baethge C, Tondo, L, Bratti IM, Bschor T, Bauer M, Viguera MC, et al. Prophylaxis-latency and outcome in bipolar disorders. Can J Psychiatry. In press. [DOI] [PubMed]
- 30.Baldessarini RJ, Tohen M, Tondo L. Maintenance treatment in bipolar disorder. Arch Gen Psychiatry 2000;57:490-2. [DOI] [PubMed]


