Abstract
Background
Occupational and population-based studies have related exposure to fine particulate air pollution, and specifically particulate matter from vehicle exhausts, to cardiovascular diseases and lung cancer.
Objectives
We have established a large retrospective cohort to assess mortality in the unionized U.S. trucking industry. To provide insight into mortality patterns associated with job-specific exposures, we examined rates of cause-specific mortality compared with the general U.S. population.
Methods
We used records from four national trucking companies to identify 54,319 male employees employed in 1985. Cause-specific mortality was assessed through 2000 using the National Death Index. Expected numbers of all and cause-specific deaths were calculated stratifying by race, 10-year age group, and calendar period using U.S. national reference rates. Standardized mortality ratios (SMRs) and 95% confidence intervals (CIs) were calculated for the entire cohort and by job title.
Results
As expected in a working population, we found a deficit in overall and all-cancer mortality, likely due to the healthy worker effect. In contrast, compared with the general U.S. population, we observed elevated rates for lung cancer, ischemic heart disease, and transport-related accidents. Lung cancer rates were elevated among all drivers (SMR = 1.10; 95% CI, 1.02–1.19) and dockworkers (SMR = 1.10; 95% CI, 0.94–1.30); ischemic heart disease was also elevated among these groups of workers [drivers, SMR = 1.49 (95% CI, 1.40–1.59); dockworkers, SMR = 1.32 (95% CI, 1.15–1.52)], as well as among shop workers (SMR = 1.34; 95% CI, 1.05–1.72).
Conclusions
In this detailed assessment of specific job categories in the U.S. trucking industry, we found an excess of mortality due to lung cancer and ischemic heart disease, particularly among drivers.
Keywords: diesel, ischemic heart disease, lung cancer, mortality, occupation, traffic exposure, trucking industry
Population-based studies have related exposure to fine particulate air pollution (Dominici et al. 2006; Laden et al. 2006; Pope et al. 2002, 2004), and specifically particulate matter (PM) from vehicle exhausts (Dominici et al. 2006; Garshick et al. 2004; Hoek et al. 2002; Laden et al. 2000; Le Tertre et al. 2002; Nafstad et al. 2003, 2004; Nyberg et al. 2000; Peters et al. 2004) to cardiovascular diseases and lung cancer. We have established a large retrospective cohort study of mortality in the unionized U.S. trucking industry. Each job category in this population has distinct exposure patterns: drivers are exposed directly to traffic; dockworkers are exposed to trucks in the yard and propane and liquified natural gas exhaust from forklifts; shop-workers are exposed to short-term vehicle exposures during repairs; and other terminal-based personnel have little exposure to vehicle exhaust (Davis et al. 2006; Smith et al. 2006). To provide insight into mortality patterns associated with these exposures we examined rates of cause-specific mortality by the different job categories in the trucking industry compared with the general U.S. population.
Materials and Methods
The Trucking Industry Particle Study
The Trucking Industry Particle Study was designed to assess the risk of lung cancer mortality in trucking industry workers with exposures to diesel and other vehicle exhausts. The study consists of three parts: a) a retrospective cohort study of lung cancer mortality among Teamsters Union members employed in 1985 in four participating companies; b) an extensive national exposure assessment designed to determine the factors influencing exposure to diesel and other vehicle exhausts, including job title, diesel vehicle use, and size and location of assigned terminal (Davis et al. 2006; Smith et al. 2006); and c) a mailed questionnaire sent to current workers to assess the distribution of smoking habits by job title and terminal characteristics (Jain et al. 2006). The Brigham and Women’s Hospital, Harvard School of Public Health, and VA Boston Institutional Review Boards approved the protocol. Cohort participants were not contacted directly, and therefore could not provide informed consent. Individuals completing the smoking questionnaire were sent a cover letter describing the goals of the study and other key aspects of informed consent, and were assumed to have given consent by completing the questionnaire.
We obtained detailed work history information for all 58,326 unionized trucking industry employees (54,319 men and 4,007 women) who had worked for at least 1 day in 1985 at one of the participating companies. Information available on each individual included social security number, age, race, sex, date of hire, last date of work, and daily job title and terminal (i.e., workplace) location through 2000. In one of the four companies, computer files were only available for the active workers starting in 1993. Therefore, we included only workers at that company who were working in 1985 and were still working in 1993.
Job titles
Job titles and duties were uniform across the four companies. Table 1 includes the description and work location for each job title. An individual contributed person-time through 2000 in each job category for which he or she had at least 1 day of work experience. The time periods did not have to be consecutive. Intercity long haul drivers, city pick-up and delivery (P&D) drivers, and combination drivers (loading dock workers who also drive P&D trucks) were grouped together into a “driver” category, and all other job titles were considered “non-drivers.”
Table 1.
Job titles, duties, and job location in the unionized trucking industry.
| Job group | Duties | Location |
|---|---|---|
| Long-haul driver | Drive heavy-duty tractor–trailer trucks between cities | Highway truck cab |
| P&D driver | Drive tractors and smaller single-bodied trucks within cities or rural areas; pick-up and deliver cargo between terminal docks and consumers | In and out of truck cab |
| Dockworker | Load and unload cargo; may operate forklifts | Loading dock |
| P&D/dockworker (combination) | Combination job: performs activities of either P&D driver or dockworker; more likely at smaller terminals | As noted above for each job |
| Mechanic | Repair and maintain tractors; job may include fueling | Truck repair shop |
| Hostler | Drive small tractor units that do not comply with emissions standards, moving trailers between the freight dock and the terminal yard | Terminal yard |
| Clerks | Cashiers, dock clerks, dispatchers, customer service representatives, and others not regularly near diesel vehicles | Offices, occasionally dock |
Mortality follow-up
Vital status, date of death, and cause-specific mortality from 1985 through 2000 was obtained through searching the National Death Index [National Center for Health Statistics (NCHS), Hyattsville, MD]. Matching criteria included social security number; month and year (± 1) of birth; and first name, middle initial, and last name. From 1985 to 2000, there were a total of 4,950 deaths (4,875 men and 75 women).
Cause of death
Annual cause-specific death rates by 10-year age group and race were obtained from the CDC WONDER database [Centers for Disease Control and Prevention (CDC) 2005]. Due to the small number of females, only males were used in the analysis. We considered causes of death by major disease classification, as well as additional causes potentially associated with fine particulate air pollution and diesel and other vehicle exhausts. These additional causes included lung cancer (Bhatia et al. 1998; Diesel Epidemiology Expert Panel 1999; Lipsett and Campleman 1999), bladder cancer (Boffetta and Silverman 2001), ischemic heart disease (Pope et al. 2004), and obstructive lung disease (defined as “chronic lower respiratory disease”) (Hart et al. 2006).
Statistical analysis
Expected numbers of all and cause-specific deaths were calculated by multiplying the person-years in each race-, 10-year-age-, and calendar period–specific stratum by the national reference rates for the entire cohort and stratified by driver versus nondriver. Standardized mortality ratios (SMRs) were calculated as the ratio of observed to expected deaths. We calculated 95% confidence intervals (CIs) under the assumption that the observed numbers of deaths follow a Poisson distribution.
To assess the potential impact of smoking on our interpretation of comparisons of mortality rates in the trucking industry with the general population, we calculated birth cohort–specific smoking rates for both groups. Year of birth and ever-smoking and current smoking rates for the trucking industry were obtained from the mailed questionnaire (Jain et al. 2006). Equivalent ever-smoking rates for the male U.S. population in 1988 were obtained from the 1997 Surgeon General’s report (National Cancer Institute 1997). Because rates were available by race only, we calculated combined rates weighting by the racial distribution of the trucking cohort. Current smoking rates for 2003 were obtained from the “Chartbook on Trends in Human Health” for the male U.S. population, regardless of race (NCHS 2006).
Results
Among the 54,319 male employees, there were 756,311.7 person-years of follow-up time. Demographics of the study population by driver status at the end of follow-up are presented in Table 2. The mean age of the full cohort in 1985 (± SD) was 42.2 ± 10.0, and the drivers were slightly older than the nondrivers. The median age of death was 61.9 years, lower than the national median for all males (73.2 years of age in 1992; NCHS 1994). The majority of the deaths occurred among the individuals who were at least 40 years of age in 1985. The majority of the population was white (83.1%). The mean duration of work for drivers and nondrivers was 20.3 ± 8.1 years and 17.1 ± 10.0 years, respectively. Of the cohort, 82% did not switch driver/nondriver status. The majority of the switching was between the dockworker (nondriver) and combination worker/P&D driver job titles.
Table 2.
Characteristics of the males in the cohort by driver/nondriver status.
| Drivers | Nondrivers | Total | |
|---|---|---|---|
| Total no. | 36,299 | 18,020 | 54,319 |
| No. of deaths | 3,693 | 1,182 | 4,875 |
| Race (no.) | |||
| White | 30,668 | 14,489 | 45,157 |
| Black | 3,359 | 1,575 | 4,934 |
| Other | 2,272 | 1,956 | 4,228 |
| Age in 1985 (years, mean ± SD) | 44.0 ± 9.1 | 38.6 ± 10.6 | 42.2 ± 10.0 |
| Age at death (years, mean ± SD) | 61.3 ± 8.6 | 59.2 ± 10.6 | 60.8 ± 9.2 |
| Year of hire (mean ± SD) | 1974 ± 8.0 | 1976 ± 7.9 | 1975 ± 8.0 |
| Total years of work (mean ± SD) | 20.3 ± 8.1 | 17.1 ± 10.0 | 19.2 ± 8.9 |
The SMRs for all-cause and cause-specific mortality by major disease classification are presented in Table 3. As expected in a working cohort, there was evidence of a healthy worker effect; the SMR for all-cause mortality was 0.72 (95% CI, 0.70–0.74), and most of the cause-specific SMRs are < 1, including malignant neoplasms as a group and diseases of the circulatory system. However, the specific SMRs for lung cancer (SMR = 1.04; 95% CI, 0.97–1.12) and ischemic heart disease (SMR = 1.41; 95% CI, 1.33–1.49) were elevated.
Table 3.
Cause-specific mortality in the Trucking Industry Particle Study cohort (n = 54,319 men), 1985–2000.
| Cause of death | ICD-9 | ICD-10 | Observed | Expected | SMR | 95% CI |
|---|---|---|---|---|---|---|
| All causes | 4,875 | 6791.9 | 0.72 | 0.70–0.74 | ||
| Infectious and parasitic diseases | 1–139 | A0–99, B0–99 | 86 | 278.4 | 0.31 | 0.25–0.38 |
| Malignant neoplasms | 140–208 | C0–97, D0–9 | 1,735 | 2003.86 | 0.87 | 0.83–0.91 |
| Bladder cancer | 188 | C67 | 29 | 36.3 | 0.80 | 0.56–1.15 |
| Lung cancer | 162 | I33–34 | 769 | 737.8 | 1.04 | 0.97–1.12 |
| Diabetes | 250 | E10–14 | 103 | 173.5 | 0.59 | 0.49–0.72 |
| Blood diseases | 280–289 | D50–89 | 15 | 21.5 | 0.70 | 0.42–1.17 |
| Mental disorders | 290–319 | F1–99 | 30 | 86.0 | 0.35 | 0.24–0.50 |
| Nervous system diseases | 320–389 | G0–98 | 59 | 99.6 | 0.59 | 0.46–0.76 |
| Circulatory system diseases | 390–459 | I0–99 | 1,793 | 2472.1 | 0.73 | 0.69–0.76 |
| Ischemic heart disease | 410–414 | I20–25 | 1,133 | 803.8 | 1.41 | 1.33–1.49 |
| Cerebrovascular disease | 430–438 | I60–69 | 167 | 242.9 | 0.69 | 0.59–0.80 |
| Respiratory system diseases | 480–519 | J10–18, J40–98 | 322 | 437.4 | 0.74 | 0.66–0.82 |
| Chronic lower respiratory disease | 490–494, 496, 519.9 | J40–47 | 212 | 253.1 | 0.84 | 0.73–0.96 |
| Digestive system diseases | 520–579 | K0–92 | 143 | 321.9 | 0.44 | 0.38–0.52 |
| Skin diseases | 680–709 | L0–98 | 3 | 5.1 | 0.59 | 0.19–1.84 |
| Musculoskeletal system diseases | 710–739 | M0–99 | 4 | 15.5 | 0.26 | 0.10–0.69 |
| Symptoms of congenital anomalies | 780–799 | Q0–99 | 47 | 63.5 | 0.74 | 0.56–0.99 |
| Accidents, homicide, suicide | 800–999 | V0–99, W0–98 X0–98, Y0–98 | 431 | 645.2 | 0.67 | 0.61–0.73 |
| Transport-related accidents | 800–848 | V0–99 | 178 | 189.4 | 0.94 | 0.81–1.09 |
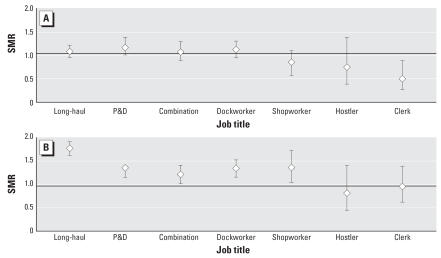
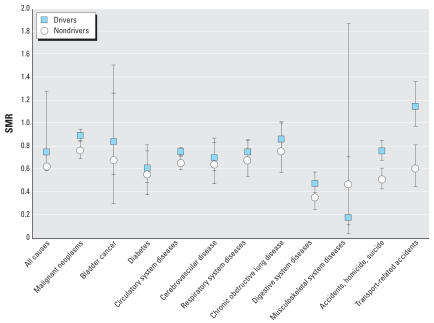
When assessed by specific job title, we observed elevated SMRs for lung cancer among the long-haul drivers, P&D drivers, combination workers, and dockworkers, with SMRs ranging from 1.08 for the combination workers to 1.16 for the P&D drivers (Figure 1). Among all drivers and dock-workers, the SMRs were 1.10 (95% CI, 1.02–1.19) and 1.10 (95% CI, 0.94–1.30), respectively. Although there was an overall deficit of deaths caused by circulatory system disease, ischemic heart disease mortality was elevated among these same job titles [all drivers SMR = 1.49 (95% CI, 1.40–1.59); dock-worker SMR = 1.32 (95% CI, 1.15–1.52)], as well as among the shop workers (SMR = 1.34; 95% CI, 1.05–1.72). In Figure 2, we also present the SMRs for the remaining causes of death by driver status. Transport-related accidents were elevated in drivers only (SMR = 1.15; 95% CI, 0.97–1.37). We found no evidence of increased bladder cancer, obstructive lung disease, or cerebrovascular mortality. All results were similar in analyses that removed the company with information available only on workers who were still working in 1993.
Figure 1.
SMRs of lung cancer (A) and ischemic heart disease (B) by job title in the U.S. trucking industry compared with the general U.S. population. Error bars indicate 95% CIs.
Figure 2.
SMRs for selected causes of death by driver/nondriver status in the U.S. trucking industry compared with the general U.S. population. Error bars indicate 95% CIs.
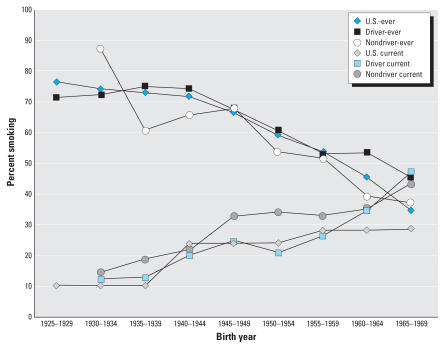
Figure 3 shows the comparison of the ever-smoking and current smoking rates in the surveyed trucking population with the birth cohort–specific rates in the general U.S. male population. For both drivers and non-drivers, the ever-smoking rates were similar to the general population. Current smoking rates among the drivers track with the U.S. population, except for the two youngest birth cohorts, and the rate of current smoking is highest among the nondrivers.
Figure 3.
Comparison of birth cohort–specific U.S. ever-smoking and current smoking rates with rates of drivers and nondrivers in the trucking population.
Discussion
As expected in a working population, there was a deficit in overall and all-cancer mortality and in most other causes of death, likely due to the healthy worker effect. In contrast, there were 31 excess deaths due to lung cancer and 329 due to ischemic heart disease—a 41% excess—in this “healthy worker” population compared with the general U.S. population. Lung cancer rates were elevated among all drivers and dock-workers; ischemic heart disease was also elevated among these jobs, as well as among shop workers. Transport accidents were only elevated in the driver categories.
Because this was a retrospective cohort study using company records to identify the cohort, no information was available on potential confounders such as smoking or diet. However, smoking histories were available from a representative survey of currently employed and recently retired workers (Jain et al. 2006). Birth cohort–specific ever-smoking rates were similar to the male U.S. general population rates available in 1988. These data were limited in that there were proportionally fewer older workers included in the mail survey compared with the retrospective cohort study, and recent information on birth cohort–specific ever-smoking rates were not available. However, current smoking rates based on the mail survey were similar to U.S. birth cohort–specific rates in 2003; among the nondrivers, who had the lowest risks, rates were actually slightly higher than the U.S. population for most birth cohorts. For the drivers, however, differences from the general population were evident only in the younger birth cohorts who contributed < 1% of the total deaths. Therefore, excess smoking in this population compared with the general U.S. population is unlikely to explain the elevated lung cancer and ischemic heart disease rates. Chronic obstructive pulmonary disease and other diseases of the respiratory system, which are predominantly related to smoking, were not elevated, providing further support for this conclusion. In contrast, diet and other lifestyle information were not available and may partially explain the elevated rates of ischemic heart disease (Pearson et al. 2002). Other factors that may also contribute to lung cancer risk, including family history and history of obstructive lung disease, are also not known, but these are not likely to be associated with exposure and are unlikely to be confounders.
Another potential limitation is the representativeness of these unionized workers to the rest of the U.S. trucking industry. Work practices among unionized companies are well-defined and the workforce is stable. It is possible that equipment-maintenance practices in these companies are more stringent than in the general trucking industry. However, there is wide variation even among our included companies, which has not been an important determinant of exposure in our exposure assessment studies (Smith et al. 2006). Finally, there is no reason to believe that these findings by job title would not be applicable to equivalent jobs in other nonunionized companies.
The observed elevations in lung cancer mortality are consistent with results from previous occupational and general population studies. Results from > 30 studies in a variety of occupational groups with diesel and vehicle exhaust exposures, including truck and other professional drivers, have been quite consistent with relative risks for lung cancer ranging from 1.2 to 1.4 (Bhatia et al. 1998; Diesel Epidemiology Expert Panel 1999; Lipsett and Campleman 1999). In a case–control study of lung cancer mortality in the U.S. unionized trucking industry, Steenland et al. (1990) observed age- and smoking-adjusted odds ratios of 1.27 for long-haul truck drivers, 1.31 for P&D drivers, 1.69 for shopworkers, and 0.92 for dockworkers, compared with workers in the same union but not in trucking-related jobs. Nyberg et al. (2000) in Stockholm County, Sweden, and Nafstad et al. (2003) in Oslo, Norway, reported an association between lung cancer risk and historical exposures to traffic after adjustment for smoking. The American Cancer Society (Pope et al. 1995, 2002) and the Harvard Six Cities Study (Dockery et al. 1993; Laden et al. 2006), two population-based prospective cohort studies in the United States, also observed elevated lung cancer mortality with increasing levels of PM from combustion sources. Nevertheless, the association of lung cancer with exposure to diesel exhaust is still being questioned (Hesterberg et al. 2006; Stober et al. 1998).
Exhaust exposures in the trucking industry are from diesel, gasoline, and propane sources. Trucking industry employees who drive trucks are mainly exposed to combustion particles attributable to gasoline and diesel traffic in the cities and on the highways where they work and drive. Loading-dock workers are currently exposed to exhaust from propane forklifts. Diesel forklifts were used during the 1980s and 1990s, and gasoline forklifts were used before that time. Historically there has been concern about lung cancer risk from diesel exhaust since older diesel engines produced more PM on a mass basis than other emission sources. These particles are mainly < 1.0 μm in diameter and contain mutagenic and carcinogenic organic carbons, including poly-cyclic aromatic hydrocarbons (Diesel Working Group 1995). Despite extensive efforts, the specific mechanisms and dose whereby diesel exhaust might cause lung cancer in humans remain uncertain, and there is no animal model relevant to human exposures (U.S. Environmental Protection Agency 2002). Although the size distribution of particles in gasoline emissions is similar to that in diesel emissions (Allen et al. 2001; Fraser et al. 2003; Geller et al. 2005; Kittelson et al. 2003; Kleeman et al. 2000; Zielinska et al. 2004) and the particles include mutagenic compounds, lung cancer risk as a result of gasoline particle exposure has not been extensively studied. Propane forklift emissions include ultrafine PM (Guo et al. 2004; Rundell 2003), but the composition of these particles has not been well characterized.
There have been fewer studies investigating the relationship between occupational exposure to vehicle exhaust and ischemic heart disease risk. In Danish bus, taxi, and truck drivers, rates of hospital admissions for ischemic heart disease were elevated 20–80% compared with other employed Danish men (Hannerz and Tuchsen 2001). Gustavsson et al. (1996) found a significantly elevated risk of myocardial infarction among long-distance truck drivers in Sweden [relative risk (RR) = 1.31]. The risk was not elevated among short-distance truck drivers, but relatively few were included in the study. In a case–control study assessing cardiovascular risk factors in survivors of first-time myocardial infarction, male bus and taxi drivers who worked for > 1 year had a nonsignificantly elevated risk (RR = 1.49; 95% CI, 0.90–2.45; and RR = 1.34; 95% CI, 0.82–2.19, respectively). The risk among truck drivers was 1.10 (95% CI, 0.79–1.53) (Bigert et al. 2003). However, the literature shows that there is growing evidence of an association of exposures to vehicle exhaust with ischemic heart disease in the general population. In Sweden, Nafstad et al. (2004) also observed an association with ischemic heart disease. In the Netherlands, Hoek et al. (2002) observed an RR of cardiopulmonary deaths of 1.71 (95% CI, 1.10–2.67) for each 10 μg/m3 of black smoke, a marker of traffic. Peters et al. (2004) found that exposure to traffic was associated with the time of onset of myocardial infarction. Finally, an analysis based on specific elements from particles in six U.S. cities found greater effects on daily mortality rates (particularly for cardiovascular deaths) attributable to particles from mobile sources than to particles from other sources (Laden et al. 2000).
The association between ischemic heart disease and combustion-related PM is supported by animal experiments (Sun et al. 2005; Suwa et al. 2002). A potential mechanism appears to be related to systemic inflammation in which the inhalation of PM provokes a low grade systemic inflammatory response and changes in blood coagulability (Peters et al. 2001; Riediker et al. 2004; Schwartz 2001; van Eeden et al. 2001). ST segment depression during exercise has also been associated with fine particulate air pollution (Pekkanen et al. 2002) and exposure to black carbon, suggesting a specific association with traffic (Gold et al. 2005; Lanki et al. 2006). Taken together, these results suggest an adverse effect of traffic and other combustion-related PM on ischemic heart disease mortality.
There are workplace conditions, work practices, and lifestyle choices associated with the trucking industry that may have an impact on life expectancy and mortality from specific causes independent of exposures to traffic and other sources of vehicle exhaust. As in any occupational SMR analysis, we were unable to control for known risk factors of the diseases of interest other than age, sex, and race. However, our mail survey demonstrates that at least one factor—smoking—was unlikely to explain our results. In this detailed assessment of specific job groupings, we conclude that there is an excess of mortality due to lung cancer and ischemic heart disease in the U.S. trucking industry, particularly among drivers. Further research is required to assess the contribution of lifestyle and personal habits to these health risks in trucking industry workers. However, our findings are consistent with previous occupational and general population studies relating PM exposures to lung cancer and cardiovascular disease and suggest that vehicle exhaust from a variety of sources contributes to this risk.
Footnotes
We thank M.J. Canner for programming assistance, the Teamster Health and Safety Office, and the participating companies.
This study was supported by grant R01 CA90792 from the National Institutes of Health/National Cancer Institute.
REFERENCES
- Allen JO, Mayo PR, Hughes LS, Salmon LG, Cass GR. Emissions of size-segregated aerosols from on-road vehicles in the Caldecott tunnel. Environ Sci Technol. 2001;35(21):4189–4197. doi: 10.1021/es0015545. [DOI] [PubMed] [Google Scholar]
- Bhatia R, Lopipero P, Smith AH. Diesel exhaust exposure and lung cancer. Epidemiology. 1998;9(1):84–91. doi: 10.1097/00001648-199801000-00017. [DOI] [PubMed] [Google Scholar]
- Bigert C, Gustavsson P, Hallqvist J, Hogstedt C, Lewne M, Plato N, et al. Myocardial infarction among professional drivers. Epidemiology. 2003;14(3):333–339. doi: 10.1097/00001648-200305000-00014. [DOI] [PubMed] [Google Scholar]
- Boffetta P, Silverman DT. A meta-analysis of bladder cancer and diesel exhaust exposure. Epidemiology. 2001;12(1):125–130. doi: 10.1097/00001648-200101000-00021. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC WONDER. 2005. [[accessed 19 August 2005]]. Available: http://wonder.cdc.gov/
- Davis ME, Smith TJ, Laden F, Hart JE, Ryan LM, Garshick E. Modeling particle exposure in US trucking terminals. Environ Sci Technol. 2006;40(13):4226–4232. doi: 10.1021/es052477m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diesel Epidemiology Expert Panel. Diesel Emissions and Lung Cancer: Epidemiology and Quantitative Risk Assessment. Cambridge, MA: Health Effects Institute; 1999. [[accessed 26 June 2007]]. Available: http://pubs.healtheffects.org/getfile.php?u=282. [Google Scholar]
- Diesel Working Group. Diesel Exhaust: Critical Analysis of Emissions, Exposure, and Health Effects. Cambridge, MA: Health Effects Institute; 1995. Special Report. [Google Scholar]
- Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329(24):1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA. 2006;295(10):1127–1134. doi: 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser MP, Buzcu B, Yue ZW, McGaughey GR, Desai NR, Allen DT, et al. Separation of fine particulate matter emitted from gasoline and diesel vehicles using chemical mass balancing techniques. Environ Sci Technol. 2003;37(17): 3904–3909. doi: 10.1021/es034167e. [DOI] [PubMed] [Google Scholar]
- Garshick E, Laden F, Hart JE, Rosner B, Smith TJ, Dockery DW, et al. Lung cancer in railroad workers exposed to diesel exhaust. Environ Health Perspect. 2004;112:1539–1543. doi: 10.1289/ehp.7195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller MD, Sardar SB, Phuleria H, Fine PM, Sioutas C. Measurements of particle number and mass concentrations and size distributions in a tunnel environment. Environ Sci Technol. 2005;39(22):8653–8663. doi: 10.1021/es050360s. [DOI] [PubMed] [Google Scholar]
- Gold DR, Litonjua AA, Zanobetti A, Coull BA, Schwartz J, MacCallum G, et al. Air pollution and ST-segment depression in elderly subjects. Environ Health Perspect. 2005;113:883–887. doi: 10.1289/ehp.7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Lee SC, Chan LY. Indoor air quality in ice skating rinks in Hong Kong. Environ Res. 2004;94(3):327–335. doi: 10.1016/S0013-9351(03)00116-6. [DOI] [PubMed] [Google Scholar]
- Gustavsson P, Alfredsson L, Brunnberg H, Hammar N, Jakobsson R, Reuterwall C, et al. Myocardial infarction among male bus, taxi, and lorry drivers in middle Sweden. Occup Environ Med. 1996;53(4):235–240. doi: 10.1136/oem.53.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannerz H, Tuchsen F. Hospital admissions among male drivers in Denmark. Occup Environ Med. 2001;58(4):253–260. doi: 10.1136/oem.58.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart JE, Laden F, Schenker MB, Garshick E. Chronic obstructive pulmonary disease mortality in diesel-exposed railroad workers. Environ Health Perspect. 2006;114:1013–1017. doi: 10.1289/ehp.8743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesterberg TW, Bunn WB, III, Chase GR, Valberg PA, Slavin TJ, Lapin CA, et al. A critical assessment of studies on the carcinogenic potential of diesel exhaust. Crit Rev Toxicol. 2006;36(9):727–776. doi: 10.1080/10408440600908821. [DOI] [PubMed] [Google Scholar]
- Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA. Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet. 2002;360(9341):1203–1209. doi: 10.1016/S0140-6736(02)11280-3. [DOI] [PubMed] [Google Scholar]
- Jain N, Hart JE, Smith TJ, Garshick E, Laden F. Smoking behavior in trucking industry workers. Am J Ind Med. 2006;49(12):1013–1020. doi: 10.1002/ajim.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kittelson D, Watts W, Jihnson JP, Zarling D, Schauer JJ, Kasper A, et al. Proceedings of U.S. Department of Energy 9th Diesel Engine Emissions Reduction Conference (DEER 2003), 24–28 August 2003. Newport, RI. Washington, DC: U.S. Department of Energy; 2003. [[accessed 19 June 2007]]. Gasoline vehicle exhaust particle sampling study; pp. 1–11. Available: http://www.osti.gov/bridge/servlets/purl/829821-SQYKH6/native/829821.pdf. [Google Scholar]
- Kleeman MJ, Schauer JJ, Cass GR. Size and composition distribution of fine particulate matter emmitted from motor vehicles. Environ Sci Technol. 2000;34(7):1132–1142. doi: 10.1021/es981276y. [DOI] [Google Scholar]
- Laden F, Neas LM, Dockery DW, Schwartz J. Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Environ Health Perspect. 2000;108:941–947. doi: 10.2307/3435052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laden F, Schwartz J, Speizer FE, Dockery DW. Reduction in fine particulate air pollution and mortality: extended follow-up of the Harvard Six Cities Study. Am J Respir Crit Care Med. 2006;173(6):667–672. doi: 10.1164/rccm.200503-443OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanki T, de Hartog JJ, Heinrich J, Hoek G, Janssen NA, Peters A, et al. Can we identify sources of fine particles responsible for exercise-induced ischemia on days with elevated air pollution? The ULTRA study. Environ Health Perspect. 2006;114:655–660. doi: 10.1289/ehp.8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Tertre A, Medina S, Samoli E, Forsberg B, Michelozzi P, Boumghar A, et al. Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Community Health. 2002;56(10):773–779. doi: 10.1136/jech.56.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsett M, Campleman S. Occupational exposure to diesel exhaust and lung cancer: a meta- analysis. Am J Public Health. 1999;89(7):1009–1017. doi: 10.2105/ajph.89.7.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nafstad P, Haheim LL, Oftedal B, Gram F, Holme I, Hjermann I, et al. Lung cancer and air pollution: a 27 year follow up of 16 209 Norwegian men. Thorax. 2003;58(12):1071–1076. doi: 10.1136/thorax.58.12.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nafstad P, Haheim LL, Wisloff T, Gram F, Oftedal B, Holme I, et al. Urban air pollution and mortality in a cohort of Norwegian men. Environ Health Perspect. 2004;112:610–615. doi: 10.1289/ehp.6684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. Smoking and Tobacco Control Monograph 8. Rockville, MD: National Cancer Institute; 1997. [[accessed 19 June 2007]]. Changes in Cigarette-Related Disease Risk and Their Implication for Prevention and Control. Available: http://cancercontrol.cancer.gov/tcrb/monographs/8/index.html. [Google Scholar]
- NCHS. Advance Report of Final Mortality Statistics 1992. 3. Vol. 45. Hyattsville, MD: National Center for Health Statistics; 1994. [Google Scholar]
- NCHS. Health, United States, 2006 with Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2006. [[accessed 18 June 2007]]. Available: http://www.cdc.gov/nchs/data/hus/hus06.pdf. [PubMed] [Google Scholar]
- Nyberg F, Gustavsson P, Jarup L, Bellander T, Berglind N, Jakobsson R, et al. Urban air pollution and lung cancer in Stockholm. Epidemiology. 2000;11(5):487–495. doi: 10.1097/00001648-200009000-00002. [DOI] [PubMed] [Google Scholar]
- Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA Guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. Circulation. 2002;106(3):388–391. doi: 10.1161/01.CIR.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- Pekkanen J, Peters A, Hoek G, Tiittanen P, Brunekreef B, de Hartog J, et al. Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: the Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air (ULTRA) study. Circulation. 2002;106(8):933–938. doi: 10.1161/01.CIR.0000027561.41736.3C. [DOI] [PubMed] [Google Scholar]
- Peters A, Frohlich M, Doring A, Immervoll T, Wichmann HE, Hutchinson WL, et al. Particulate air pollution is associated with an acute phase response in men; results from the MONICA-Augsburg Study. Eur Heart J. 2001;22(14):1198–1204. doi: 10.1053/euhj.2000.2483. [DOI] [PubMed] [Google Scholar]
- Peters A, von Klot S, Heier M, Trentinaglia I, Hormann A, Wichmann HE, et al. Exposure to traffic and the onset of myocardial infarction. N Engl J Med. 2004;351(17):1721–1730. doi: 10.1056/NEJMoa040203. [DOI] [PubMed] [Google Scholar]
- Pope CA, III, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002;287(9):1132–1141. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CA, III, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109(1):71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- Pope CA, III, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE, et al. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med. 1995;151(3 Pt 1):669–674. doi: 10.1164/ajrccm/151.3_Pt_1.669. [DOI] [PubMed] [Google Scholar]
- Riediker M, Cascio WE, Griggs TR, Herbst MC, Bromberg PA, Neas L, et al. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am J Respir Crit Care Med. 2004;169(8):934–940. doi: 10.1164/rccm.200310-1463OC. [DOI] [PubMed] [Google Scholar]
- Rundell KW. High levels of airborne ultrafine and fine particulate matter in indoor ice arenas. Inhal Toxicol. 2003;15(3):237–250. doi: 10.1080/08958370304502. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and blood markers of cardiovascular risk. Environ Health Perspect. 2001;109(suppl 3):405–409. doi: 10.2307/3434788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TJ, Davis ME, Reaser P, Natkin J, Hart JE, Laden F, et al. Overview of particulate exposures in the US trucking industry. J Environ Monit. 2006;8(7):711–720. doi: 10.1039/b601809b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenland NK, Silverman DT, Hornung RW. Case-control study of lung cancer and truck driving in the Teamsters Union. Am J Public Health. 1990;80(6):670–674. doi: 10.2105/ajph.80.6.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stober W, Abel UR, McClellan RO. Revisiting epidemiological key studies on occupational diesel exhaust exposure and lung cancer in truck drivers. Inhal Toxicol. 1998;10:1045–1078. doi: 10.1080/089583798197286. [DOI] [Google Scholar]
- Sun Q, Wang A, Jin X, Natanzon A, Duquaine D, Brook RD, et al. Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. JAMA. 2005;294(23):3003–3010. doi: 10.1001/jama.294.23.3003. [DOI] [PubMed] [Google Scholar]
- Suwa T, Hogg JC, Quinlan KB, Ohgami A, Vincent R, van Eeden SF. Particulate air pollution induces progression of atherosclerosis. J Am Coll Cardiol. 2002;39(6):935–942. doi: 10.1016/S0735-1097(02)01715-1. [DOI] [PubMed] [Google Scholar]
- U.S. Environmental Protection Agency. Health Assessment Document for Diesel Engine Exhaust. Washington, DC: U.S. Environmental Protection Agency; 2002. [Google Scholar]
- van Eeden SF, Tan W, Suwa T, Mukae H, Terashima T, Fujii T, et al. Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM10) Am J Respir Crit Care Med. 2001;164(5):826–830. doi: 10.1164/ajrccm.164.5.2010160. [DOI] [PubMed] [Google Scholar]
- WHO. International Classification of Diseases, Ninth Revision. Geneva: World Health Organization; 1977. [Google Scholar]
- WHO. International Classification of Diseases, Tenth Revision. Geneva: World Health Organization; 1993. [Google Scholar]
- Zielinska B, Sagebiel J, Arnott WP, Rogers CF, Kelly KE, Wagner DA, et al. Phase and size distribution of polycyclic aromatic hydrocarbons in diesel and gasoline vehicle emissions. Environ Sci Technol. 2004;38(9):2557–2567. doi: 10.1021/es030518d. [DOI] [PubMed] [Google Scholar]