Patent fallopian tubes are a prerequisite for normal human fertility. However, patency alone is not enough—normal function is crucial. Although patients often view them as either open or “blocked,” the fallopian tubes are highly specialised organs. They have a critical role in picking up eggs and transporting eggs, sperm, and the embryo. The fallopian tubes are also needed for sperm capacitation and egg fertilisation. Because the egg is fertilised in the fallopian tubes and the first stages of development of the embryo occur during its four day journey to the uterine cavity, the tubes are also important in nutrition and development. The fallopian tubes are vulnerable to infection and surgical damage, which may impair function by affecting the delicate fimbriae or the highly specialised endosalpinx. A fallopian tube obstruction occurs in 12% to 33% of infertile couples,1 and so tubal patency should be investigated early.
Causes of tubal damage
Infection
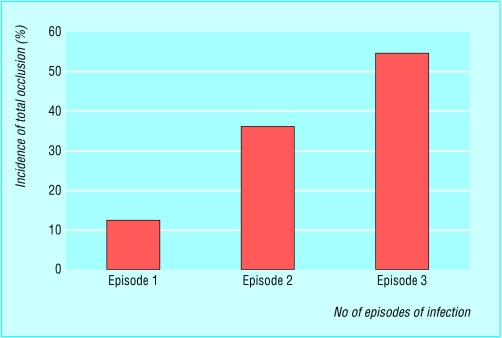
Pelvic infection is a major cause of tubal subfertility. Infective tubal damage can be caused by sexually transmitted diseases, or can occur after miscarriage, termination of pregnancy, puerperal sepsis, or insertion of an intrauterine contraceptive device. The severity of tubal subfertility after pelvic infection depends on the number and severity of episodes.2 Although a history of symptomatic pelvic inflammatory disease may heighten suspicion of tubal damage, most women with tubal infertility do not report it. Even in women with serological evidence of past chlamydial or gonococcal infections, most are unaware of the infection.
Figure 1.
Incidence of tubal occlusion after pelvic infection
Chlamydia trachomatis
Chlamydia trachomatis accounts for around half the cases of acute pelvic inflammatory disease in developed countries. It is the commonest sexually transmitted agent in the United Kingdom. Chlamydial infections are often not diagnosed because they are usually asymptomatic or have few signs of infection. Both symptomatic and asymptomatic chlamydial infections can damage the reproductive tract. In women, they can cause urethritis, cervicitis, endometritis, and salpingitis, which may result in peritubal adhesions. These adhesions may cause subfertility, ectopic pregnancy, and chronic pelvic pain. Delayed treatment increases the risk of these sequelae and transmission of the infection to sexual partners.
Gonorrhoea
Gonorrhoea is particularly common in young, urban women of low socioeconomic groups and in people who have several sexual partners. It may present as a localised infection of the lower genital tract, as an invasive infection of the upper genital tract, or as disseminated disease with systemic manifestations; however, it may be asymptomatic. Infection with chlamydia is concurrent in 30-50% of patients from whom gonococcus is isolated.
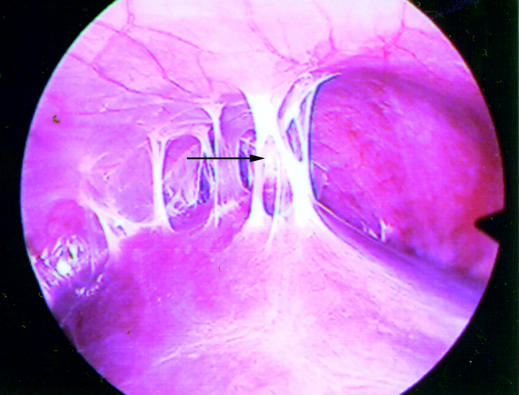
Figure 2.
Perihepatic adhesions (arrow) seen at laparoscopy usually associated with pelvic gonorrhoeal or chlamydial infection (Fitz-Hugh-Curtis syndrome)
Genital tuberculosis
Genital tuberculosis can cause simple tubal block, tubo-ovarian abscesses, or dense pelvic adhesions (frozen pelvis).
Incidence of tubal occlusion rises with the number of pelvic infections the patient has had
Genital tuberculosis is more common in UK inner city areas with increasing immigrant populations
Post-pregnancy sepsis
Post-pregnancy sepsis (post-abortion and puerperal infection) may be associated with salpingitis and endometritis. Endometritis with retained products of pregnancy followed by vigorous curettage can result in denudation of the endometrium; intrauterine adhesions (synechiae) can form, which may wholly or partially occlude the uterine cavity. This is an unusual, but important, cause of infertility (Asherman's syndrome), and the patient generally presents with oligomenorrhoea or amenorrhoea, although the hormone profile of the patient is normal.
Figure 3.
Hysterosalpingogram showing contrast filling defects caused by intrauterine adhesions. The arrows show the areas of front to back adhesion partially occluding the cavity and disrupting the normal endometrium
Intrauterine contraceptive devices
Upper genital tract infection associated with intrauterine contraceptive devices is temporally linked to the insertion of the device. Increased risk occurs in the first 20 days after insertion. Beyond the first month after insertion the risk of upper genital tract infection is small. The risk of infertility after the use of an intrauterine contraceptive device is stopped is not increased, nor is fertility impaired even when the device is removed (usually because of complications, such as menorrhagia).
Endometriosis
Complete tubal occlusion is rarely caused by pelvic endometriosis. Tubal distortion and limitation of fimbrial mobility caused by the associated pelvic adhesions is more likely.
Surgery
Complications after surgery
Previous laparotomy is a recognised risk factor for tubal subfertility, but a history of perforated appendix in childhood does not seem to have a long term negative effect on female fertility.
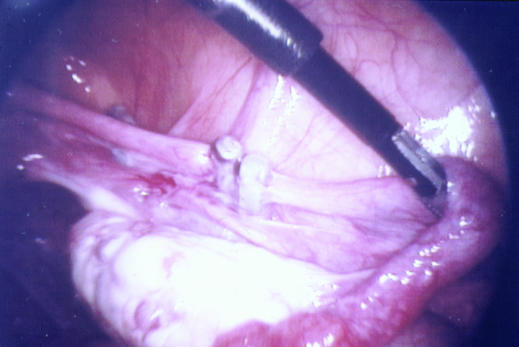
Figure 4.
Laparoscopy showing two Filshie clips on the right fallopian tube. Double application has no benefit as it is no more effective and destroys a greater length of tube, making reversal less likely to be successful
Sterilisation
People who change their mind after tubal interruption and wish to conceive can have surgical reconstruction of the fallopian tubes or in vitro fertilisation. The results of surgical reversal will depend on the method used to perform the sterilisation (clips, rings, diathermy, or excision), the site of sterilisation, the length of tube remaining, and ovulatory and sperm factor.
Prevention of tubal damage
Practising safe sex is important in reducing sexually transmitted diseases and their sequelae. Screening women of reproductive age for chlamydial infection has been shown to reduce its prevalence and the incidence of pelvic inflammatory disease. Aggressive treatment of suspected pelvic inflammatory disease reduces late sequelae.3
The sexual partners of patients must be treated rapidly to decrease the risk of reinfection. The management of women undergoing induced abortion should include a strategy for minimising the risk of post-abortion pelvic inflammatory disease. Women undergoing invasive uterine procedures (hysteroscopy, hysterosalpingo-contrast sonography, and hysterosalpingography) should be screened for chlamydia or receive prophylactic antibiotics.
Diagnosis of tubal subfertility
Infection screening
Chlamydia antibody testing is a simple and cheap screening test for the likelihood of tubal subfertility. The predictive value of testing will depend on the cut-off level of the immunoglobulin G titre chosen and the criteria applied for tubal factor subfertility. Recent studies concluded that the optimum cut-off titre should be 16 because it gives the best combination of sensitivity and specificity. However, high titres of chlamydial antibodies in infertile women indicate the need for early laparoscopy to assess tubal status.
Table 1.
Suitable antibiotics for prophylaxis after invasive uterine procedures
| • Doxycycline 100 mg orally, twice daily for a week |
| • Ofloxacin 400 mg orally twice daily plus clindamycin 450 mg orally four times daily or metronidazole 500 mg orally twice daily, all for a week |
The 31st Royal College of Obstetricians and Gynaecologists Study Group on the Prevention of Pelvic Infection recommended that non-pregnant women under 35 years undergoing uterine instrumentation (for example, intrauterine contraceptive device insertion, infertility laparoscopy, hysteroscopy, or endometrial sampling) should be screened for relevant organisms using a sensitive technique before the procedure, or failing that, should receive appropriate prophylactic antibiotics
Hysterosalpingo-contrast sonography
Hysterosalpingo-contrast sonography is a simple outpatient procedure using ultrasonography. An echocontrast fluid is introduced into the uterine cavity via a 5 French cervical balloon catheter so that the uterine cavity, ovaries, and fallopian tube patency can be assessed accurately. The use of transvaginal ultrasonography avoids exposure to x rays and is particularly suitable as a diagnostic test in patients with a low likelihood of tubal disease. Finding a normal cavity and bilateral fill and spill of contrast is reassuring, but where there is doubt, hysterosalpingography or a laparoscopy and dye hydrotubation test should be done. Transvaginal ultrasonography can sometimes be useful in detecting hydrosalpinges.
Figure 5.
A dilated hydrosalpinx diagnosed by sonohysterography. The sausage shaped, dark hydosalpinx (filled with saline) stands out clearly against background structures
Hysterosalpingography
Hysterosalpingography is a simple, safe, and inexpensive x ray based contrast study of the uterine cavity and the fallopian tubes with a 65% sensitivity and 83% specificity for detecting tubal blockage.
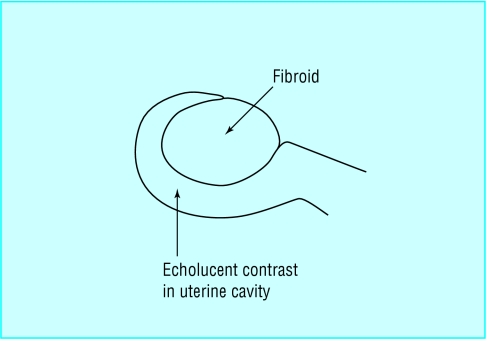
Figure 6.

Hysterosonogram showing an intracavity fibroid outlined by ultrasonic contrast medium
Proximal tubal occlusion can be associated with mild peritoneal endometriosis. The mechanism is unclear, but the occlusion is thought to be caused by a combination of the deposition of intraluminal debris from retrograde menstruation and raised tubal perfusion pressure.4
Distal tubal blockage, which is commonly caused by pelvic inflammatory disease, is usually associated with distension of the ampullary portion of the fallopian tube (hydrosalpinges) and variable degree of loss of the internal mucosal folds.
Figure 8.
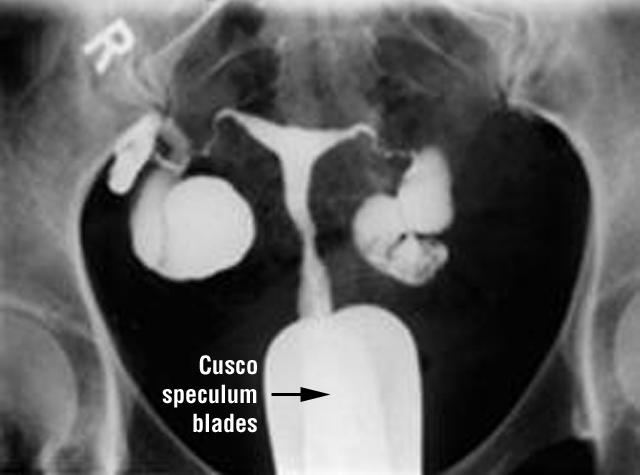
Hysterosalpinogram showing bilateral hydrosalpinges filled with x ray contrast that has been instilled via the cervix. The Cusco speculum blades and the thread of the metal cannula are seen at the base of the picture
Laparoscopy and dye hydrotubation test
A laparoscopy and dye hydrotubation (“lap and dye”) test is the most reliable, albeit expensive, tool used to diagnose tubal subfertility. It is usually performed as a day case surgical procedure under general anaesthesia. When there is no prior information about the uterine cavity, the test can be combined with hysteroscopy for maximum information. Morphological abnormalities of the fallopian tubes can be seen directly, and the general pelvic appearance may give some clue as to the likely cause of any abnormalities found. When comparing hysterosalpingography with laparoscopy, keep in mind that both procedures provide more information than on the condition of the fallopian tubes alone. Hysterosalpingography provides information about the status of the uterine cavity, whereas laparoscopy allows inspection of the intra-abdominal cavity, excludes peritoneal disease, and allows laparoscopic surgery. The latter has become especially important because it was recently shown that laparoscopic treatment of early endometriosis improves fertility prospects by 13% over the next nine months.
Table 2.
Comparison of hysterosalpingography with laparoscopy
| Hysterosalpingography | Laparoscopy and dye hydrotubation |
| • Outpatient procedure | • Day surgery procedure |
| • Analgesia adequate | • General anaesthesia required |
| • Simple, inexpensive | • Expensive |
| • Gives uterine cavity information | • Shows outer contour of the uterus only (unless with hysteroscopy) |
| • Tubal patency tested | • Shows appearance of tubes and their patency; also appearance of ovaries and pelvic peritoneum |
| • Screening test | • Definitive test |
| • Not particularly sensitive for mild distal tubal disease or endometriosis | • Distal tubal disease or endometriosis can be diagnosed and treated |
An expert advisory group of the chief medical officer for England supported opportunistic screening for chlamydia in sexually active women under 25 years, and in older women who have a new sexual partner or have had two or more partners in the past year
Management options
“Expectant” management
Patients with tubal subfertility still have a chance (albeit reduced) of natural conception, but this will depend on the extent of the damage. Patients with severe tubal disease can become pregnant while they are on waiting lists for in vitro fertilisation. However, treatment with in vitro fertilisation or tubal surgery is more effective than “expectant” management.
Transcervical tubal cannulation
Transcervical tubal cannulation is an outpatient procedure indicated in cases of proximal occlusion. In 80-90% of cases it is successful in restoring the patency of at least one fallopian tube. About 30% of patients get pregnant in the first three to six months after the procedure.5 Because of its simplicity, transcervical tubal cannulation should be considered as a first line treatment for patients with proximal occlusion.
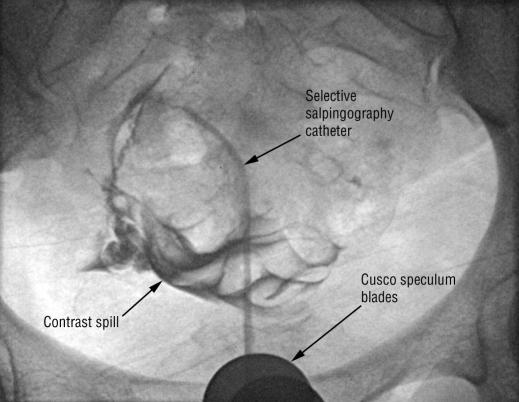
Figure 9.
X ray film of a patent fallopian tube after transcervical tubal cannulation. The selective salpingography cannula points at the right cornu and contrast spills through into the pelvis
Surgery
Surgical treatment and its outcome are related to the site and extent of tubal damage. Reversal of tubal ligation is one of the main indications for tubal microsurgery. Laparoscopic adhesiolysis has the best results if the adhesions are the only factor responsible for subfertility. Distal tubal occlusion may be treated using a laser or more traditional instruments to open the phimosed fimbrial end. Where the tubes are irreversibly damaged and there are large, communicating hydrosalpinges, salpingectomy (laparoscopic or open) is recommended as the success of in vitro fertilisation is impaired by their presence.
In vitro fertilisation
As in vitro fertilisation can achieve a higher chance of pregnancy for all types of tubal subfertility, it should be regarded as effective treatment. Couples should be referred early because in vitro fertilisation success is strongly related to age. However, about 20% of pregnancies resulting from in vitro fertilisation are multiple pregnancies, with attendant risks and complications.
Table 3.
Main issues in tubal subfertility
| • Problems with fallopian tubes are responsible for up to one third of cases of female subfertility |
| • Major damage to the fallopian tubes can occur after infection or abdominal surgery |
| • Prophylactic antibiotics given at uterine instrumentation are effective in reducing pelvic inflammatory disease and tubal damage |
| • Tubal damage cannot be excluded by the lack of a history of pelvic inflammation |
| • The number and severity of the episodes of pelvic inflammatory disease are strongly correlated with the degree of tubal damage |
| • Measurement of serum C trachomatis antibody titres may be useful in identifying patients with high likelihood of tubal damage |
| • Hysterosalpingo-contrast sonography is a useful test to confirm tubal patency and to assess uterine cavity and ovarian morphology without exposure to x rays |
| • Hysterosalpingography is a simple, safe, inexpensive x ray contrast study for assessing the uterine cavity and fallopian tubes |
| • The laparoscopy and dye hydrotubation test is useful in the diagnosis of peritubal adhesions and endometriosis, and for the accurate assessment of the optimal management options and prognosis |
| • Hysterosalpingo-contrast sonography, hysterosalpingography, and laparoscopy and dye hydrotubation tests play complementary roles in the investigation of subfertility in women |
| • In vitro fertilisation is more effective in all cases of tubal damage than tubal surgery, which is only suitable for peritubal adhesions, reversal of sterilisation, and tubocornual anastomosis in selected cases and selected centres with appropriate expertise |
Yacoub Khalaf is a consultant gynaecologist and subspecialist in reproductive medicine at Guy's and St Thomas's NHS Hospital Trust, and consultant in the Guy's and St Thomas's assisted conception unit.
The ABC of subfertility is edited by Peter Braude, professor and head of department of women's health, Guy's, King's, and St Thomas's School of Medicine, London, and Alison Taylor, consultant in reproductive medicine and director of the Guy's and St Thomas's assisted conception unit. The series will be published as a book in the winter.
Competing interests: None declared.
References
- 1.Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, et al. Population study of causes, treatment, and outcome of infertility. BMJ 1985;291: 1693-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins JA, Wrixon W, Janes LB, Wilson EH. Treatment-independent pregnancy among infertile couples. N Engl J Med 1983;309: 1201-6. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Pelvic inflammatory disease: guidelines for prevention and management. Morb Mortal Wkly Rep 1991: 1-33.
- 4.Karande VC, Pratt DE, Rao R, Balin M, Gleicher N. Elevated tubal perfusion pressures during selective salpinography are highly suggestive of tubal endometriosis. Fertil Steril 1995;64: 1070-3. [DOI] [PubMed] [Google Scholar]
- 5.Woolcot R, Petchpud A, O'Donnell P, Stanger J. Differential impact on pregnancy rate of selective salpingography, tubal catheterization and wire-guide recanalization in the treatment of proximal fallopian tube obstruction. Hum Reprod 1995;10: 1423-6. [DOI] [PubMed] [Google Scholar]