Editor—In their review of the severe acute respiratory syndrome (SARS) Wong et al emphasise lymphopenia as a hallmark feature.1 Panesar suggested that glucocorticoids or stimulation of the hypothalamic-pituitary-adrenal axis leads to lymphocyte margination and that patients without lymphopenia may have adrenal insufficiency.2
Apoptosis may also explain the lymphopenia of SARS. In severe paramyxovirus infections in humans such as measles, lymphopenia is commonly present and associated with more severe disease. One of us with Carrington recently reported that lymphopenia is also seen with another paramyxovirus infection: respiratory syncytial virus, which causes bronchiolitis in young children.3
Children with more severe bronchiolitis from respiratory syncytial virus infection have significantly lower absolute lymphocyte counts than those with mild disease. Bronchiolitis is ubiquitous and, in the developed world, the commonest reason a child under 1 year of age is admitted to hospital. Studies in mice show that not only is the lymphocyte immune response to virus essential in controlling the virus but it also causes disease.4 The fact the immune response is both saint and sinner is believed to be why the use of ribavirin has proved less effective in bronchiolitis than was first hoped.
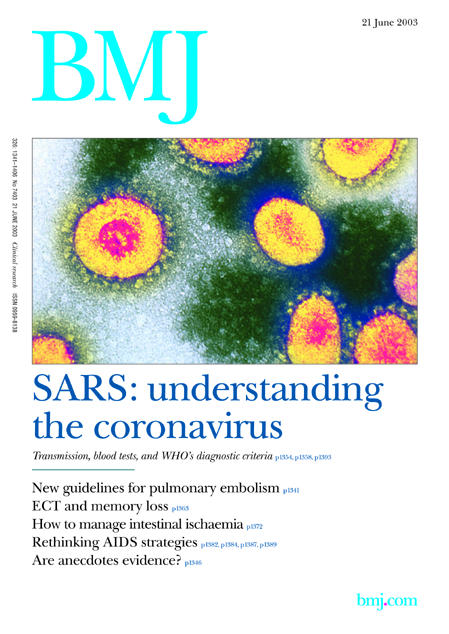
Figure 1.
SARS, respiratory syncytial virus disease, measles, and sepsis show parallels in the occurrence of lymphopenia. In sepsis and measles apoptosis is believed to be the mechanism of lymphopenia. In models of sepsis, for example, inhibitors of apoptosis ameliorate illness and prevent death.5 There may be important therapeutic implications for patients with SARS from these new research areas.
Competing interests: None declared.
References
- 1.Wong RS, Wu A, To KF, Lee N, Lam CW, Wong CK, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ 2003;326: 1358-62. (21 June.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panesar NS. Lymphopenia in SARS. Lancet 2003;361: 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Donnell DR, Carrington D. Peripheral blood lymphopenia and neutrophilia in children with severe respiratory syncytial virus disease. Pediatr Pulmonol 2002;34: 128-30. [DOI] [PubMed] [Google Scholar]
- 4.Openshaw PJ. Immunopathological mechanisms in respiratory syncytial virus disease. Springer Semin Immunopathol 1995;17: 187-201. [DOI] [PubMed] [Google Scholar]
- 5.Hotchkiss RS, Chang KC, Swanson PE, Tinsley KW, Hui JJ, Klender P, et al. Caspase inhibitors improve survival in sepsis: a critical role of the lymphocyte. Nat Immunol 2000;1: 496-501. [DOI] [PubMed] [Google Scholar]


