Abstract
This study tested the validity of four measures of dietary restraint: Dutch Eating Behavior Questionnaire, Eating Inventory (EI), Revised Restraint Scale (RS), and the Current Dieting Questionnaire. Dietary restraint has been implicated as a determinant of overeating and binge eating. Conflicting findings have been attributed to different methods for measuring dietary restraint. The validity of four self-report measures of dietary restraint and dieting behavior was tested using: 1) factor analysis, 2) changes in dietary restraint in a randomized controlled trial of different methods to achieve calorie restriction, and 3) correlation of changes in dietary restraint with an objective measure of energy balance, calculated from the changes in fat mass and fat-free mass over a six-month dietary intervention. Scores from all four questionnaires, measured at baseline, formed a dietary restraint factor, but the RS also loaded on a binge eating factor. Based on change scores, the EI Restraint scale was the only measure that correlated significantly with energy balance expressed as a percentage of energy require d for weight maintenance. These findings suggest that that, of the four questionnaires tested, the EI Restraint scale was the most valid measure of the intent to diet and actual caloric restriction.
Keywords: dietary restraint, validity, assessment measures, calorie restriction, exercise, diet, energy balance
Introduction
Dietary restraint is defined as the intention to restrict food intake in order to control body weight (Herman & Mack, 1975). During the past 30 years, the construct of dietary restraint has been theorized to be a psychological determinant of overeating (Ruderman & Wilson, 1979), binge eating (Ruderman, 1986), and bulimia nervosa (Polivy & Hermann, 1985). The validity of the causal relationship between dietary restraint and overeating (often called the dietary restraint hypothesis) has been supported by a large number of laboratory studies that have established that overeating (counter-regulation) by participants defined as high in dietary restraint, often occurs as a response to a pre-load that disrupts dietary restraint (Heatherton, Herman, Polivy, King, & McGree, 1988; Lowe & Levine, 2005; Ruderman, 1986; Polivy, 1996). Over the past 30 years, a few studies have failed to support the hypothesized causal relationship between dietary restraint and overeating/binge eating (Dritschel, Cooper, & Charnock, 1993; Jansen, Oosterlaan, Mercklbach, & van den Hout, 1988; Lawson, Williamson, et al., 1995; Lowe & Kleifield, 1986; Smith, Geiselman, Williamson et al., 1998; Wardle & Beales, 1987). Several authors (e.g., Lowe & Levine, 2005; Ouwens, van Strien; & van der Staak, 2003; Stice, Fisher, & Lowe, 2004) have concluded that the mixed results of different studies are most likely due to different methods being used for measuring dietary restraint, i.e., the Restraint Scale versus several alternatives that are discussed below.
Most early studies of dietary restraint utilized either the Restraint Scale (Herman & Mack, 1975) or a later revision (Herman & Polivy, 1980). Both laboratory and cross-sectional studies that reported support for the dietary restraint hypothesis have used the Restraint Scale to measure dietary restraint (Heatherton et al., 1988; Lowe & Levine, 2005). Given the inconsistency of findings of studies using different scales, the measurement of the dietary restraint construct has become a source of controversy. Two other widely used questionnaires for measuring dietary restraint have been developed: the Three Factor Eating Questionnaire (Stunkard & Messick, 1985) and the Dutch Eating Behavior Questionnaire (Van Strien et al., 1986). The studies that failed to support the dietary restraint hypothesis used these two alternative methods (Ouwens, et al., 2003).
Lowe (1993) proposed a three factor theory of dieting which hypothesized that the dietary restraint construct is multi-dimensional and provided a three-factor model of dieting: 1) frequency of dieting/overeating, 2) current dieting, and 3) weight suppression. He noted that one explanation for the conflicting results of studies that tested the dietary restraint hypothesis was that measures of dietary restraint purport to assess the intent to diet, not actual dieting (caloric restriction). Based upon this reasoning, we believed that it was important to include a measure of current dieting in this study and we developed a Current Dieting Questionnaire for this purpose.
In the midst of this controversy that has spanned almost 30 years, concerns about the safety of dieting were raised due to the potential for weight cycling following a period of intentional food/calorie restriction (Brownell & Rodin, 1994). These concerns led to a substantial backlash against dieting that has been termed the anti-dieting movement (Hill, 2004; Lowe & Levine, 2005). Controlled trials of non-dieting treatments have yielded inconsistent weight loss across many studies of overweight/obese adults (Foster & McGuckin, 2001). Conversely, in 2000, a consensus panel of experts concluded that the potential benefits of dieting for weight loss substantially outweighed the potential adverse effects (National Task Force on the Treatment and Prevention of Obesity, 2000). Also, during the past decade, a series of randomized controlled trials of the effects of dieting and non-dieting approaches for weight loss (Goodrick, Poston, Kimball, Reeves, & Foreyt, 1998; Presnell & Stice, 2003; Reeves et al., 2001) and weight gain prevention (Klem, Wing, Simkin-Silverman, & Kuller, 1997) have investigated the changes in binge eating. All of these studies have reported decreased frequency of overeating or binge eating following dieting or non-dieting treatment. Interventions involving caloric restriction were associated with weight loss (Goodrick et al., 1998; Prenell & Stice, 2003), but these trials did not directly measure dietary restraint. In one of the few studies that compared measures of dietary restraint before and after treatment, Safer and colleagues (2004) concluded that the two measures of dietary restraint used in the study, i.e., Eating Disorder Evaluation (Fairburn & Cooper, 1993) and the Eating Inventory (Stunkard & Messick, 1988) assessed different constructs, i.e., dieting to lose weight versus dieting to avoid weight gain.
In summary, many research studies have questioned the validity of the dietary restraint hypothesis. Nevertheless, controversy about the psychosocial consequences of dieting persist (Polivy & Herman, 2002). Evidence from a variety of sources suggests that at the core of this controversy is the validity of the different methods used to measure dietary restraint. The primary aim of this study was to test the validity of four different questionnaires that have been developed to measure dietary restraint. The study was conducted as an ancillary project to a six-month randomized controlled trial (RCT) that tested three approaches for inducing calorie restriction in overweight (BMI from 25.0 to 29.9) adult men and women who were screened for the absence of an eating disorder. The study utilized three strategies for testing the validity of the four different measures of dietary restraint: 1) inter-correlations among the measures using correlations and factor analysis, 2) changes in the measures of dietary restraint during the RCT of calorie restriction, and 3) correlations of changes in self-report measures of dietary restraint with changes in total energy balance, using changes in fat mass and fat-free mass measured by dual x-ray absorptiometry (Pullar & Webster, 1977).
Methods
Participants
A complete description of the recruitment and screening procedures and participant characteristics is provided elsewhere (Heilbronn et al., 2006). Participants were overweight at screening (25 ≤ BMI ≤ 30 kg/m2), non-smoking adult men (25–50 years of age) and women (25–45 years of age). Besides being overweight, participants were otherwise healthy and not taking medications other than oral contraceptives. Potential participants were screened for mental health problems (American Psychiatric Association, 1994), e.g., depression, anxiety disorders, or psychotic disorders, using the Structured Clinical Interview for DSM-IV Axis I Disorders, Non-patient Edition (SCID-I/NP; First, Spitzer, Gibbon, & Williams, 2002). Participants were screened for the presence of eating disorders with the Interview for Diagnosis of Eating Disorders, version Four (IDED-IV; Kutlesic et al., 1998). The presence of a mental health problem or an eating disorder was an exclusion criterion.
Forty-eight participants completed a five-week baseline assessment period and were randomly assigned to one of four treatment arms for the six-month study: 1) calorie restriction (CR; 25% calorie restriction of baseline energy requirements), 2) CR plus exercise (CR+EX; 12.5% CR plus 12.5% increase in energy expenditure by structured exercise), 3) low-calorie diet (LCD; 890 kcal/day liquid diet until 15% of body weight was lost, followed by a weight maintenance diet), and 4) control (weight maintenance diet; Step 1 American Heart Association diet). For the purposes of this study, the CR, CR+EX, and LCD groups were defined as “dieting” conditions. We hypothesized that these “dieting” conditions would be associated with increased dietary restraint and greater weight loss in comparison to the control group and that “dieting” would be associated with negative energy balance. If these two hypotheses were supported, we hypothesized that some of the measures of dietary restraint would be negatively correlated with an objective measure of energy balance.
Two participants did not complete the six-month study (both withdrew before any follow-up assessments were conducted), one each in the LCD and control arms, and their data were not included in the study sample. The descriptive characteristics of the participants (who completed the study, n = 46) at baseline are summarized in Table 1. The sample was predominantly white (n = 28, 61%) and 57% of the sample was female. The average age of the sample was 38 years. Average body mass index was 27.7, indicating that the participants were overweight but not obese. Mean scores on the measures of dietary restraint, overeating, and binge eating suggested that the degree of dietary restraint, disinhibition, and binge eating was within normal limits (Anderson, Williamson, Duchmann, Gleaves, & Barbin, 1999; Gorman & Allison, 1995).
Table 1.
Characteristics of the study sample (n=46) at baseline.
| Characteristic | n | Mean | Std Error | Min-imum | Max-imum |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 26 | ||||
| Female | 20 | ||||
| Race | |||||
| White | 28 | ||||
| African American | 16 | ||||
| Asian or Latino | 2 | ||||
| Age (year) | 38.0 | 0.95 | 26 | 49 | |
| Weight (kg) | 81.6 | 1.51 | 61.7 | 104.7 | |
| BMI (kg/m 2) | 27.7 | 0.25 | 24.8 | 31.5 | |
| Body Fat (%) | 32.0 | 1.07 | 16.9 | 45.4 | |
| Dieting Measurement Scales | |||||
| DEBQ – Restraint subscale | 24.5 | 1.10 | 10 | 43 | |
| Current Dieting Questionnaire | 1.3 | 0.18 | 0 | 3 | |
| Eating Inventory - Restraint Subscale | 7.8 | 0.61 | 1 | 18 | |
| Restraint Scale – Concern for Dieting | 6.4 | 0.59 | 1 | 16 | |
| Restraint Scale – Weight Fluctuation | 6.9 | 0.37 | 2 | 12 | |
| Restraint Scale – Total Score | 13.4 | 0.78 | 3 | 28 | |
| Eating Inventory – Disinhibition Subscale | 5.7 | 0.51 | 1 | 12 | |
| MAEDS – Binge Eating Subscale | 47.8 | 1.55 | 28 | 67 | |
Table Note: Abbreviations: DEBQ = Dutch Eating Behavior Questionnaire, MAEDS = Multidimensional Assessment of Eating Disorder Symptoms.
Assessment Methods
To test the validity of the four measures of dietary restraint, the research design required questionnaire measures of dietary restraint and current dieting as well as questionnaire measures of overeating and binge eating. In addition, measures of energy balance were required. These assessment methods are summarized below.
Measures of Dietary Restraint, Current Dieting, Overeating, and Binge Eating
Revised Restraint Scale (RS)
The first measure of dietary restraint was developed by Herman and Mack (1975) and was later revised to a 10-item scale by Herman and Polivy (1980), which is the version used in this study and is the version that has been used in most research studies related to tests of the dietary restraint hypothesis (Gorman & Allison, 1995; Polivy, 1997). Factor analytic studies of the RS have reported that it contains two subscales: 1) concern for dieting and 2) weight fluctuations (Gorman & Allison, 1995). The validity of these subscales and the total RS score were tested in this study. Many studies of the RS have established its reliability and validity (Gorman & Allison, 1995).
Eating Inventory/Three Factor Eating Questionnaire
In 1985, Stunkard and Messick developed the Three Factor Eating Questionnaire, which was renamed the Eating Inventory (EI; Stunkard & Messick, 1988). The EI has three scales: 1) dietary (cognitive) restraint, 2) disinhibition, and 3) perceived hunger. The dietary restraint and disinhibition scales are not correlated, but the perceived hunger and disinhibition scales are positively correlated (Williamson et al., 1995). In this study, the dietary restraint scale was selected for assessment of construct validity. The disinhibition scale was selected to measure overeating. Recent studies of the EI Dietary Restraint scale have reported that it contains two subscales called Rigid and Flexible Control of eating (Westenhoefer, 1991; Westenhoefer, Stunkard, & Pudel, 1999). These two subscales, as defined by the 14 original items of the Dietary Restraint scale (Westenhoefer, et al, 1999), were tested for treatment effects and for correlations with the measure of energy balance. The reliability and validity of these EI scales have been established in many studies (Gorman & Allison, 1995).
Dutch Eating Behavior Questionnaire (DEBQ)
In 1986, Van Strien, et al. reported a similar self-report inventory called the DEBQ; it measures: 1) Restrained Eating, 2) Emotional Eating, and 3) External Eating. For the purposes of this study, only the Restrained Eating scale was administered. The construct validity of this scale was tested. The reliability and validity of the DEBQ has been established (Gorman & Allison, 1995).
Current Dieting Questionnaire (CDQ)
This three-item self-report questionnaire was developed in a pilot investigation to assess current dieting, as described by Lowe (1993). The three questions identified in the pilot study were: 1) “I am trying to lose weight by eating less,” 2) “I choose foods that are low in fat because I am trying to lose weight,” and 3) “Are you now watching what you eat in order to lose weight?” In the pilot investigation, these questions were found to have a high level of internal consistency (alpha = .85). The response format for these questions was “true” or “false” for the first two questions and “yes” or “no” for the third question. The validity of the CDQ was tested in this study to evaluate whether a brief measure of current dieting was a valid indicator of intent to diet and/or actual caloric restriction.
Multidimensional Assessment of Eating Disorder Symptoms (MAEDS)
The MAEDS (Anderson et al., 1999) is a reliable and valid self-report inventory that measures six symptom domains related to eating disorders: binge eating, restrictive eating, purgative behavior, fear of fatness, avoidance of forbidden foods, and depression. Scores on all scales are standardized using t-scores. For the purposes of this study, scores on the Binge Eating scale were used in the correlation and factor analyses.
Interview for Diagnosis of Eating Disorders, version 4 (IDED-IV; Kutlesic et al., 1998). The IDED-IV was used to screen for the presence of eating disorders at baseline, an exclusion criterion for the study. The IDED-IV is an interview method that has been validated for the diagnosis of anorexia nervosa, bulimia nervosa, and binge eating disorder using DSM-IV criteria (American Psychiatric Association, 1994). Persons who reported 4 of the 8 combined symptoms of anorexia or bulimia nervosa were excluded from the study.
Body weight and composition
Measures of metabolic body weight and composition were collected at baseline and at months 3 and 6 of follow-up. Body weight was determined by the mean of two consecutive measurements obtained in the morning following an overnight fast and corrected for the weight of a hospital gown. Whole body percent body fat was also measured twice by dual energy x-ray absorptiometry (DXA; Hologics QDR 4500A, Bedford, MA).
Energy balance
The energy balance of each participant was calculated at month 6 of the intervention, from changes in body energy stores (fat mass and fat-free mass) versus the energy intake calculated for weight maintenance at baseline. Baseline energy intake was calculated from two fourteen day measures of energy expenditure by doubly labeled water with adjustments made, if necessary, during two weeks of feeding at our Center. To convert the changes in fat mass (FM) and fat-free mass (FFM) to energy, the following energy coefficients were used: for weight loss, 1g of FM = 9.3 kcal and 1g of FFM = 1.1 kcal; for weight gain, 1g FM = 13.1 kcal and 1g FFM = 2.2 kcal (Pullar & Webster 1977). Therefore the mean daily change in body energy stores from baseline to month 6 is equal to the change in FM (multiplied by the energy coefficient) plus the change in FFM (multiplied by the energy coefficient), divided by the number of days between the body composition assessments by DXA (see formula below).
Energy balance is then determined by dividing the daily change in energy stores by the energy intake required for weight maintenance and expressed as a percentage of baseline energy intake (see formula below).
A positive number indicates a positive energy balance or weight gain whereas a negative number indicates a negative energy balance or weight loss. Since measures of dietary restraint are probably only sensitive to changes in energy intake, the energy balance score from the CR+EX group was estimated from the 12.5% of caloric restriction only. For this calculation we had to assume that because half of the energy deficit was derived from caloric restriction and half from an increase in exercise expenditure, the changes in body composition were the result of equal contributions from diet and exercise.
Procedures
A complete description of the study procedures is provided in Heilbronn et al. (2006). Participants completed a four-week baseline assessment period, during which total daily energy expenditure (TEE) was calculated using the doubly labeled water (DLW) technique. For the first two weeks, TEE was determined with DLW while participants ate their usual diet at home. For the second two-week DLW period, participants consumed a weight maintenance diet provided to them by the Pennington Center’s Metabolic Kitchen. All meals were provided to participants; they ate breakfast and dinner on weekdays at the Pennington Center, and lunch and weekend meals were packed to go. The questionnaires were completed during an inpatient stay at each measurement period.
Following baseline testing, participants were randomly assigned to: CR, CR+EX, LCD, or Control group. All participants were provided with food for the first 12 weeks of the study, and they ate a self-selected diet from weeks 13 to 21. Near the end of the study (weeks 22 to 24), participants were again provided food. During these in-feeding periods, participants were served a diet consistent with the American Heart Association (AHA) Step 1 recommendations (≤ 30% fat). The LCD participants were provided with 890 kcal/day of formula diet (Health One, Health and Nutrition Technology, Carmel, CA) in the form of 5 shakes, one of which was supplemented with 10 g of fat and consumed as a muffin to reduce the risk of gallstone development. Once an LCD participant reached the goal weight (15% reduction from baseline body weight), they were prescribed a self-selected weight maintenance diet, consistent with the AHA recommendations. Participants in the CR+EX group increased energy expenditure by 12.5% with structured exercise. Individual exercise prescriptions were provided to each participant, and at least 3 of 5 exercise sessions each week were conducted in the laboratory under supervision.
To help participants adhere to their prescribed diet and exercise plans, they met with registered dietitians and exercise physiologists as needed, and they attended weekly group sessions led by a doctoral-level psychologist. Cognitive-behavioral techniques were utilized to foster adherence to the protocol, including self-monitoring of diet and physical activity, behavioral contracting, and stimulus control.
Statistical Analyses
Pearson correlations were performed on the baseline variables. Following these analyses, a principal components factor analysis with Varimax (orthogonal) rotation was performed to test whether the various measures of dietary restraint were assessing the same versus distinct behavioral dimensions. We next examined the effect of caloric restriction on dietary restraint by using a repeated measures model to test for time effects, treatment effects, and time by treatment interactions. Changes from baseline among the measures of dietary restraint were the dependent variables in the repeated measures model, with baseline measures used as covariates. Alpha was set at p < .05 for all analyses. The change in energy balance from baseline to Month 6 was analyzed using analysis of variance with treatment group as an independent effect. Pearson correlations were conducted between changes in energy balance at Month 6 with changes in dietary restraint measures from baseline to Month 6. All statistical analyses used SAS version 8.2.
Results
Correlations and Factor Analyses
Table 2 summarizes the results of correlations among the measures obtained at baseline, before random assignment to treatment arms. These correlations indicate that the DEBQ Restraint scale, Current Dieting Questionnaire, EI Restraint Scale, and RS total score were positively correlated. The total RS was significantly correlated with measures of binge eating/overeating, i.e., EI Disinhibition scale and MAEDS binge eating scale. Examination of the correlations of the two subscales of the RS indicates that the RS Concern for Dieting scale was positively correlated with all other measures of dietary restraint and with the two measures of binge eating/overeating. In contrast, the RS Weight Fluctuations subscale was not significantly correlated with other measures of dietary restraint or binge eating/disinhibition.
Table 2.
Intercorrelations among scales measuring dietary restraint and binge eating at baseline.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1) DEBQ – Restraint subscale | - | .46** | .69** | .55** | .63** | .16 | .12 | .25 |
| 2) Current Dieting Questionnaire | - | .40 | .35 | .36 | .17 | .03 | .08 | |
| 3) Eating Inventory - Restraint Subscale | - | .51** | .59 | .13 | −.07 | .14 | ||
| 4) Restraint Scale – Total Score | - | ---- | ---- | .42** | .54** | |||
| 5) Restraint Scale – Concern for Dieting | - | .28 | .40** | .59** | ||||
| 6) Restraint Scale – Weight Fluctuation | - | .25 | .20 | |||||
| 7) Eating Inventory – Disinhibition Subscale | - | .77** | ||||||
| 8) MAEDS – Binge Eating Subscale | - |
Table Note: Abbreviations: DEBQ = Dutch Eating Behavior Questionnaire, MAEDS = Multidimensional Assessment of Eating Disorder Symptoms,
p < .05,
p < .01
Table 3 summarizes the results from the factor analyses. Table 3A presents the results when the RS total score was entered. Based on analysis of eigenvalues and percent variance, two factors were retained accounting for 73% of the variance. The results of the factor analysis indicated that the first factor measured intent to diet with all four measures of restraint, i.e., DEBQ Restraint, Current Dieting Questionnaire, EI Dietary Restraint, and RS total score loading on Factor 1. The second factor measured binge eating/overeating, with the EI Disinhibition scale, MAEDS binge eating scale, and RS total score loading on Factor 2. Therefore, the RS loaded on factors reflecting dietary restraint and binge eating/overeating. In a follow-up analysis, we tested the factor structure when the total RS score was replaced with the two subscales of the RS. These results are summarized in Table 3B. Again, based on analysis of eigenvalues and percent variance, two factors were retained, accounting for 67% of the variance. As shown in Table 3B, four measures loaded on Factor 1, dietary restraint: DEBQ Restraint, Current Dieting Questionnaire, EI Dietary Restraint, and RS Concern for Dieting subscale. Three measures loaded on Factor 2, binge eating/overeating: EI Disinhibition scale, MAEDS binge eating scale, and the Concern for Dieting subscale of the RS. The RS Concern for Dieting subscale was associated with both constructs, i.e., dietary restraint and binge eating/overeating whereas the RS Weight Fluctuation subscale was correlated with the binge eating construct.
Table 3.
Factor Structure and Item Loadings for Questionnaires.
| Table 3A | Factor 1 | Factor 2 |
|---|---|---|
| Factor 1: Dietary Restraint | ||
| DEBQ – Restraint subscale | *.86 | .17 |
| Current Dieting Questionnaire | *.70 | −.01 |
| Eating Inventory - Restraint Subscale | *.87 | −.01 |
| Restraint Scale – Total | *.63 | *.58 |
| Factor 2: Binge Eating | ||
| Eating Inventory – Disinhibition Subscale | − .06 | *.93 |
| MAEDS – Binge Eating Subscale | .13 | *.92 |
|
| ||
| Table 3B | Factor 1 | Factor 2 |
|
| ||
| Factor 1: Restraint | ||
| DEBQ – Restraint subscale | *.85 | .19 |
| Current Dieting Questionnaire | *.69 | .02 |
| Eating Inventory - Restraint Subscale | *.88 | .02 |
| Restraint Scale – Concern for Dieting | *.67 | *.59 |
| Factor 2: Binge Eating | ||
| Eating Inventory – Disinhibition Subscale | −.11 | *.92 |
| MAEDS – Binge Eating Subscale | .09 | *.92 |
| Restraint Scale – Weight Fluctuation | .20 | *.40 |
Table Note: signifies a factor loading greater than or equal to 0.40. Abbreviations: DEBQ = Dutch Eating Behavior Questionnaire, MAEDS = Multidimensional Assessment of Eating Disorder Symptoms.
Changes in Dietary Restraint during the RCT of Calorie Restriction
Figure 1 illustrates the mean change scores from baseline that were observed for the four measures of dietary restraint/dieting behavior, i.e., the DEBQ Restraint scale, the Current Dieting Questionnaire, the EI Dietary Restraint scale, and the total score for the Restraint Scale. A statistically significant main effect for treatment was observed for all four measures: DEBQ Restraint scale (F = 4.33, p < .01), Current Dieting Questionnaire (F= 10.54, p < .0001), the EI Dietary Restraint scale (F = 6.12, p< .002), and the total score for the Restraint Scale (F = 3.83, p < .02). Significant changes over time were also observed for the DEBQ Restraint scale (F = 13.22, p< .001), the Current Dieting Questionnaire (F = 4.10, p < .05), and the EI Dietary Restraint scale (F = 4.47, p < .05) but were not observed for the total score for the Restraint Scale (F = 1.88, p > .05). The interaction of treatment and time was not statistically significant for any of the measures.
Figure 1.
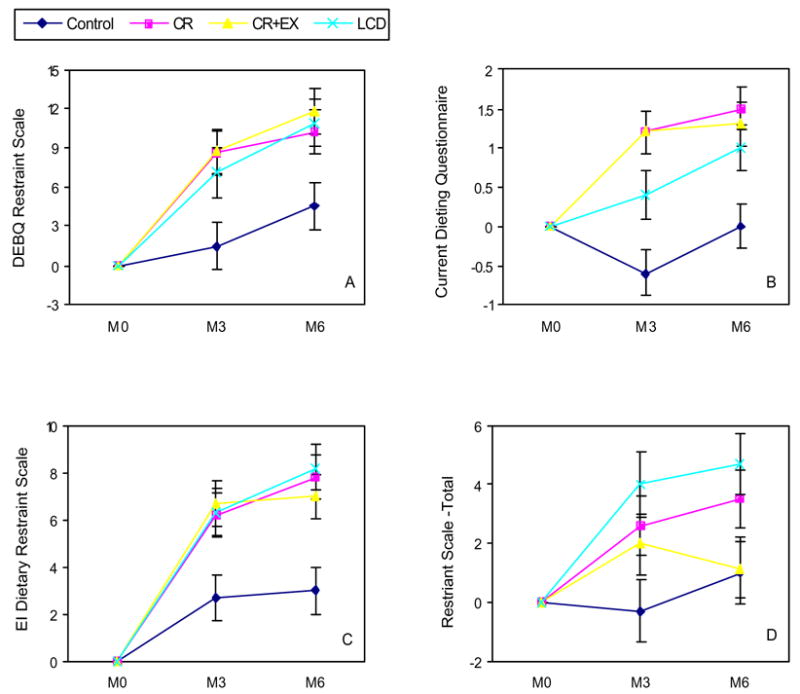
Changes in measures of dietary restraint as a function of treatment arm.
Figure 1A shows the results using the DEBQ Restraint scale. All three groups that were prescribed some form of caloric restriction (CR, CR + EX, and LCD) were had increased dietary restraint scores at 3 and 6 months, and all three “dieting” conditions had higher mean Restraint scores in comparison to the Control group at both 3 and 6 months. The mean Restraint score of the Control group at six months, but not at three months, was significantly elevated in comparison to baseline.
Figure 1B depicts a very similar pattern for scores on the CDQ. The mean score for the LCD group at three months did not differ from baseline, and the mean score for the LCD group at three months was significantly lower that those for the CR and CR+EX groups. At the six-month measurement, the three “dieting” conditions did not differ and all three groups reported mean scores that were significantly higher than those for the control group and differed from baseline scores (p < .05). The scores for the Control group at 3 and 6 months did not differ from baseline.
Figure 1C illustrates the findings related to the EI Dietary Restraint scale. The same pattern of scores was observed, with all three “dieting” groups reporting higher scores in comparison to the Control group at months 3 and 6 (p < .05). In comparison to baseline scores, the 3 and 6-month scores for all four groups were significantly elevated (p < .05). Secondary analyses of the Rigid and Flexible Control subscales also found significant treatment effects for both subscales (p < .05), indicating that all three “dieting” groups reported increased Rigid and Flexible Control scores in comparison to the control group at Month 6.
Figure 1D summarizes the findings for the total score of the Restraint Scale. A different pattern was observed for this measure. Scores for the Control group did not change from baseline and did not differ from the CR+EX group at any measurement point. The CR and LCD groups differed from the CR+EX group and the Control group at 3 and 6 months (p < .05). The mean scores for both the CR and LCD groups were elevated in comparison to baseline at 3 and 6 months (p < .05).
The pattern of data for the Restraint Scale was further explored by testing for changes in the two subscales: concern for dieting and weight fluctuations. These data are summarized in Figure 2. Examination of the concern for dieting subscale indicated a significant main effect for treatment (F = 3.15, p < .04), but not for time or the interaction of treatment and time. Figure 2A summarizes the pattern of findings. The CR and CR+EX groups differed from the Control group at three months, but at six- months, only the CR group differed from the Control group. The CR group reported significantly increased scores at 3 and 6 months. The CR+EX group reported significantly increased dietary restraint at month 3 and the LCD group reported significantly increased dietary restraint at Month 6.
Figure 2.
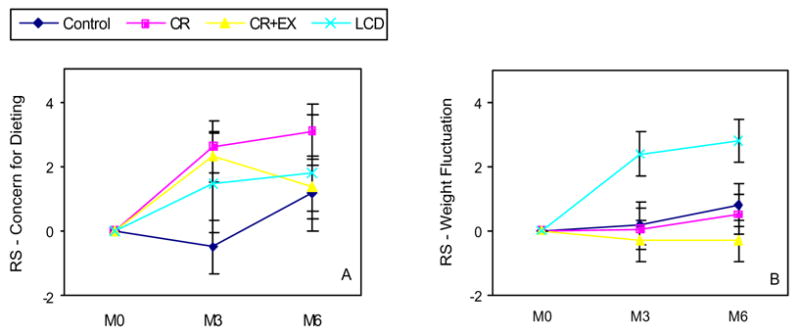
Changes in the subscales of the Restraint Scale as a function of treatment arm.
Examination of the weight fluctuations subscale indicated a significant main effect for treatment (F = 5.26, p < .04), but not for time or the interaction of treatment and time. Figure 2B depicts the pattern of findings. The LCD group reported significantly higher scores at 3 and 6 months in comparison to all other groups, which did not differ. Furthermore, only the LCD group reported significant increases from baseline.
Changes in Body Weight and Body Composition
A complete description of the results related to change in body weight is provided elsewhere (Heilbronn et al., 2006). Weight loss (mean and SEM) at Month 6 for each group was: 1) CR = −10.4 ± 0.9%, 2) CR+EX = −10.0 ± 0.8%, 3) LCD = −13.9 ± 0.7%, and 4) Control = −1.0 + 1.1%. Compared to the control group, fat mass was significantly reduced in the three “dieting” conditions at Months 3 and 6 (p < .001). At Month 3, but not Month 6, the LCD group lost significantly more fat mass compared to the CR and CR+EX groups (p < .01). At Month 3, the CR and LCD groups lost significantly more fat-free mass compared to the control (p < .01), and at Month 6 the CR, CR+EX, and LCD group lost significantly more fat-free mass compared to the control group (p <.001).
Changes in Energy Balance as a Function of Treatment Arm
Figure 3A illustrates mean changes in energy balance from baseline to month six for each of the treatment arms. The LCD group had the greatest decrease in energy balance, showing a greater degree of energy restriction, followed by the CR group and the CR+EX group. All three groups had larger energy deficit in comparison to the control group, and this energy deficit represents a significant change from the energy balance state at baseline. The energy balance of the control group did not change from baseline.
Figure 3.
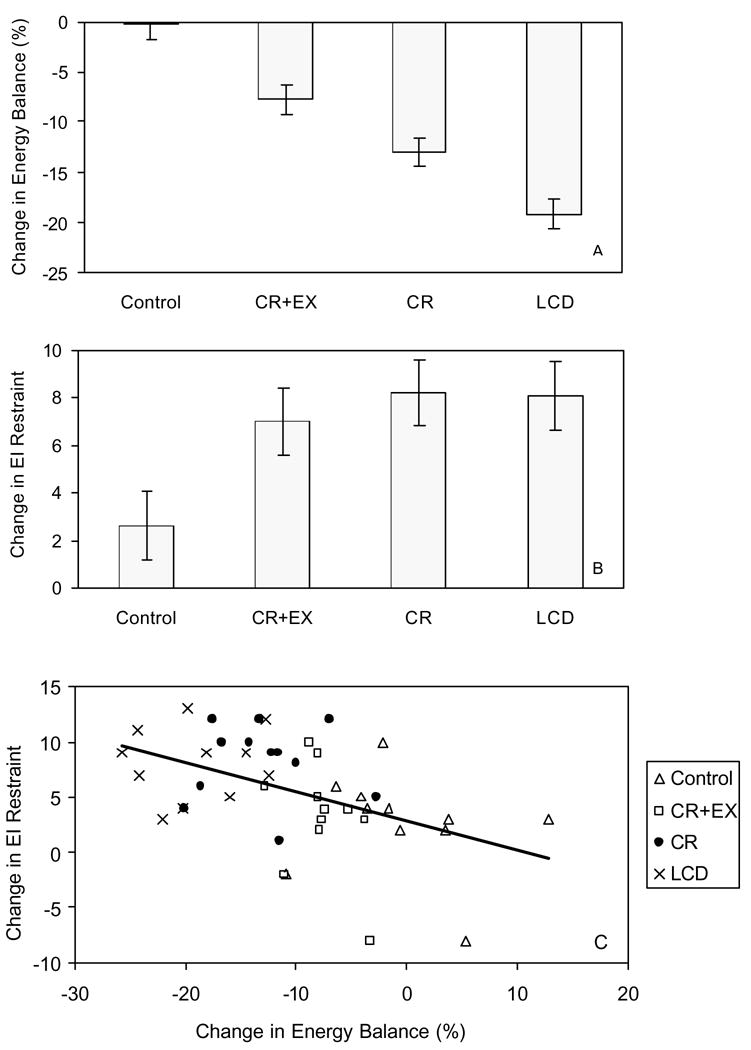
3A.Changes in energy balance for the four treatment arm at Month 6; 3B.Change in EI restraint Scale for the four treatment arms at Month 6; 3C, Correlation of changes in EI restraint scores and energy balance at Month 6.
Correlations of Dietary Restraint and Energy Balance
As evident in Figure 3A, the three “dieting” conditions were associated with negative energy balance after six months of caloric restriction, while the control group had very little change in energy balance. Figure 3B shows the changes in the EI Dietary Restraint scale at six-months, as a function of treatment arm. All three “dieting” conditions were associated with increased restraint, in comparison to the control group. Table 4 summarizes the correlations between energy balance at six months and changes in the questionnaire data from baseline to Month 6. Considering all of the participants in the four treatment arms (n =46), only one of the measures of dietary restraint, the EI Restraint Scale was significantly correlated (r = −0.46) with energy balance, indicating that increased dietary restraint was associated with negative energy balance. Figure 3C illustrates the correlation between changes in the EI Restraint scale and energy balance after six months of calorie restriction. Examination of Figure 3C shows that changes in the EI Restraint Scale were associated with the overall pattern of energy balance. However, within the treatment arms (see Table 4) this relationship was only observed in the CR+EX group. These low correlations were probably influenced by the very small number of participants (n = 11 or 12) within each treatment arm and the relatively low variability within each group for the measure of energy balance and dietary restraint. Similar correlations with energy balance were found for changes in the Rigid Control subscale (r = −0.33, p < .05) and for changes in the Flexible Control subscale (r = −0. 34, p < .05). Noteworthy, the significant correlation of changes in the RS weight fluctuation scale and energy balance (r = 0.65) was positive and in the opposite direction of the prediction that increased restraint is associated with negative energy balance. Correlations of actual (not change) scores of the dietary restraint measures at baseline and at six months were also computed. None of these correlations were in the predicted direction (negative correlation) and statistically significant
Table 4.
Correlations between changes in dietary restraint and change in energy balance at Month 6.
| Treatment | Change DEBQsum | Change DQtotal | Change EI RES | Change RS Total | Change RS CD | Change RS WF |
|---|---|---|---|---|---|---|
| All | −0.15 | −0.08 | −0.46* | −0.24 | −0.26 | −0.04 |
| CR | 0.52 | 0.17 | −0.02 | 0.13 | 0.06 | 0.07 |
| CR+EX | −0.20 | −0.25 | −0.67* | 0.03 | −0.15 | 0.24 |
| Control | −0.02 | 0.28 | −0.19 | −0.24 | −0.34 | 0.18 |
| LCD | 0.14 | 0.44 | 0.09 | 0.29 | −0.18 | 0.65* |
Table Note: Abbreviations: DEBQ = Dutch Eating Behavior Questionnaire, DQ = Current Dieting Questionnaire, EI = Eating Inventory, RS = Restraint Scale, CD = Concern for Dieting, WF= Weight Fluctuations.
p < .05
Discussion
The results of this validity study suggest that the four measures of dietary restraint that were tested in this study do not measure the same theoretical construct. As noted by Lowe (1993), the dietary restraint construct could involve: 1) the frequency of dieting/overeating, 2) current dieting (or caloric restriction), and 3) weight suppression. Others have also suggested that some measures of dietary restraint may also measure susceptibility for overeating. This study tested the extent to which four measures that purport to measure the dietary restraint construct assess these four domains. The study also tested several important measurement issues, e.g., whether measures of dietary restraint measure: a) intent to diet, b) intent to diet and susceptibility to overeating, and c) actual changes in energy balance derived from six months of caloric restriction. In general, the results of this study were limited by the relatively small sample size. The small sample size is especially relevant for interpreting the results of the factor analyses (which were not cross-validated) and the correlations with energy balance. Also, the small sample size did not allow for analysis of the validity of the four measures of dietary restraint as a function of sex, due to insufficient statistical power. This limitation is regrettable given the robust finding that there are sex differences on measures of dietary restraint (Gorman & Allison, 1995).
Three of the measures, DEBQ, EI, and RS, contain questions that ask directly about an intention to engage in dieting to manage body weight, and in principle all four instruments ask questions about actual behavior that would result in caloric restriction, i.e., what Lowe (1993) called “current dieting.” Thus, all four measures ask questions related to the frequency or intensity of dieting. Results of the correlations and factor analyses indicated that the four questionnaires were highly correlated and all loaded on a dietary restraint factor. The RS total score was also positively correlated with measures of overeating (EI disinhibition scale) and binge eating (MAEDS binge eating scale) and the RS total score loaded on the binge eating factor, as well as the dietary restraint factor (Table 3). Analyses of the RS subscales indicate that this pattern of correlations was primarily determined by the relationship of the concern for dieting subscale with measures of dietary restraint and binge eating/overeating. The weight fluctuation scale was not correlated with any of the other measures. These findings are generally consistent with earlier results (e.g., Heatherton et al., 1988; Laessle, Tuschl, Kotthaus, & Pirke, 1989), and they suggest that the RS measures both the intent to diet and susceptibility for overeating. In contrast, the other measures, DEBQ, EI, and CDQ, only measured the dietary restraint construct, i.e., intent to diet.
As shown in Figure 1, the DEBQ, EI, and CDQ were sensitive to measuring changes in dietary restraint regardless of the strategy that was employed, i.e., caloric restriction alone, a combination of caloric restriction and increased exercise, or following a low-calorie diet followed by self-management of food intake. Somewhat less consistent results were evident for the RS, in that it was less sensitive to changes in the CR+EX group. Figure 2 shows that the results were even less consistent when the two subscales of the RS were used to measure changes in dietary restraint, i.e., the intent to diet during a “dieting” program. These findings suggest that the DEBQ, EI, and CDQ were valid indicators of current dieting and since all of the “dieting” conditions were associated with significant weight loss, these measures are also valid indicators of weight suppression, when expressed as changes from baseline.
The correlations with energy balance indicated that changes in the EI Restraint scores (from baseline to six months) were associated with total negative energy balance during that same time period. Change scores for the DEBQ, CDQ, and RS were not significantly correlated with negative energy balance. Furthermore, actual scores on none of the dietary restraint measures was correlated with energy balance, regardless of whether the dietary restraint measures were administered at baseline (before “dieting” for three groups) or at six months (after “dieting”). This pattern of findings is informative for one important measurement issue. Cross-sectional studies (e.g., Stice et al., 2004) have reported that measures of dietary restraint do not measure actual caloric restriction. The results of this study indicate that these four measures of dietary restraint were not predictive of changes in energy balance and that they were not informative of a current state of negative energy balance. As can be seen in Table 4 and Figures 1 and 3C, only changes in the EI Restraint scale were indicators of objectively measured changes in energy balance. The implication of this finding is that measures of dietary restraint, especially the DEBQ, EI, and CDQ, may be good indicators of the intent to diet in cross-sectional research, but only one measure (EI Restraint), expressed as a change score, was found to be a valid indicator of actual caloric restriction. It is noteworthy that the two subscales of the EI Restraint scale, Rigid and Flexible Control, reflected results that were comparable to those observed for the full EI Restraint scale. These findings suggest that these EI Restraint subscales are sensitive to “dieting” interventions and are also valid indicators of energy balance when used as change scores.
Acknowledgments
This work was supported by research grant U01 AG20478 from the National Institutes of Health. LMR is supported by a Training Fellowship awarded by the NHMRC of Australia (ID 349553). Our gratitude is extended to the clinical staff of the Pennington Biomedical Research Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- Anderson DA, Williamson DA, Duchmann EG, Gleaves DH, Barbin JS. Development and validation of a multiaxial treatment outcome measure for eating disorders. Assessment. 1999;6:7–20. doi: 10.1177/107319119900600102. [DOI] [PubMed] [Google Scholar]
- Brownell KD, Rodin J. The dieting maelstrom. Is it possible and advisable to lose weight? American Psychologist. 1994;49:781–91. doi: 10.1037//0003-066x.49.9.781. [DOI] [PubMed] [Google Scholar]
- Dritschel B, Cooper PJ, Charnock D. Emotional arousal and overeating in eaters. Journal of Abnormal Psychology. 1993;101:348–351. doi: 10.1037//0021-843x.101.2.348. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge eating. Vol. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foster GD, McGuckin BG. Estimating resting energy expenditure in obesity. Obesity Research. 2001;5:367S–372S. [PubMed] [Google Scholar]
- Goodrick GK, Poston WS, 2nd, Kimball KT, Reeves RS, Foreyt JP. Nondieting versus dieting treatment for overweight binge-eating women. Journal of Consulting and Clinical Psychology. 1998;66:363–8. doi: 10.1037//0022-006x.66.2.363. [DOI] [PubMed] [Google Scholar]
- Gorman BS, Allison DB. Measures of restrained eating. In: Allison DB, editor. Handbook of assessment for eating behaviors and weight-related problems. Thousand Oaks, CA: Sage Publishing, Inc; 1995. pp. 149–184. [Google Scholar]
- Heatherton TF, Herman CP, Polivy J, King GA, Mc Gree ST. The (mis)measurement of restraint: an analysis of conceptual and psychometric issues. Journal of Abnormal Psychology. 1988;43:647–660. doi: 10.1037//0021-843x.97.1.19. [DOI] [PubMed] [Google Scholar]
- Heilbronn LK, de Jonge L, Frisard MI, DeLany JP, Larson-Meyer DE, Rood J, et al. Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized controlled trial. JAMA. 2006;295:1539–48. doi: 10.1001/jama.295.13.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman CP, Mack D. Restrained and unrestrained eating. Journal of Personality. 1975;43:647–60. doi: 10.1111/j.1467-6494.1975.tb00727.x. [DOI] [PubMed] [Google Scholar]
- Herman CP, Polivy J. Restrained eating. In: Stunkard A, editor. Obesity. Philadelphia: Saunders; 1980. pp. 208–225. [Google Scholar]
- Hill AJ. Does dieting make you fat? British Journal of Nutrition. 2004;92:S15–8. doi: 10.1079/bjn20041135. [DOI] [PubMed] [Google Scholar]
- Jansen A, Oosterlaan J, Merckelbach H, van den Hout M. Nonregulation of food intake in restrained, emotional, and external eaters. Journal of Psychopathology and Behavioral Assessment. 1988;10:345–354. [Google Scholar]
- Klem ML, Wing RR, Simkin-Silverman L, Kuller LH. The psychological consequences of weight gain prevention in healthy, premenopausal women. International Journal of Eating Disorders. 1997;21:167–174. doi: 10.1002/(sici)1098-108x(199703)21:2<167::aid-eat7>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Kutlesic V, Williamson DA, Gleaves DH, Barbin JM, Murphy-Eberenz KP. The Interview for the Diagnosis of Eating Disorders-IV: Application to DSM-IV diagnostic criteria. Psychological Assessment. 1998;10:41–48. [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. Behavioral and biological correlates of dietary restraint in normal life. Appetite. 1989;12:83–94. doi: 10.1016/0195-6663(89)90098-6. [DOI] [PubMed] [Google Scholar]
- Lawson OJ, Williamson DA, Champagne CM, DeLany JP, Brooks ER, Howat PM, et al. The association of body weight, dietary intake, and energy expenditure with dietary restraint and disinhibition. Obesity Research. 1995;3:153–61. doi: 10.1002/j.1550-8528.1995.tb00131.x. [DOI] [PubMed] [Google Scholar]
- Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychological Bulletin. 1993;114:100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Kleifield EI. Cognitive restraint, weight suppression, and the regulation of eating. Appetite. 1988;10:159–68. doi: 10.1016/0195-6663(88)90009-8. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Levine AS. Eating motives and the controversy over cieting: Eating less than needed versus less than wanted. Obesity Research. 2005;13:797–806. doi: 10.1038/oby.2005.90. [DOI] [PubMed] [Google Scholar]
- National Task Force on the Treatment and Prevention of Obesity. Overweight, obesity, and health risk. Archives of Internal Medicine. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- Ouwens MA, van Strien T, van der Staak CP. Absence of a disinhibition effect of alcohol on food consumption. Eating Behavior. 2003;4:323–32. doi: 10.1016/S1471-0153(03)00033-3. [DOI] [PubMed] [Google Scholar]
- Polivy J. Psychological consequences of food restriction. Journal of the American Dietetic Association. 1996;96:589–92. doi: 10.1016/S0002-8223(96)00161-7. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Dieting and bingeing: A causal analysis. American Psychologist. 1985;40:193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. If at first you don't succeed. False hopes of self- change. American Psychologist. 2002;36:83– 88. [PubMed] [Google Scholar]
- Presnell K, Stice E. An experimental test of the effect of weight-loss dieting on bulimic pathology: Tipping the scales in a different direction. Journal of Abnormal Psychology. 2003;112:166–70. [PubMed] [Google Scholar]
- Pullar JD, Webster AJ. The energy cost of fat and protein deposition in the rat. British Journal of Nutrition. 1977;37:355–63. doi: 10.1079/bjn19770039. [DOI] [PubMed] [Google Scholar]
- Reeves RS, McPherson RS, Nichaman MZ, Harrist RB, Foreyt JP, Goodrick GK. Nutrient intake of obese female binge eaters. Journal of the American Dietetic Association. 2001;101:209–15. doi: 10.1016/S0002-8223(01)00055-4. [DOI] [PubMed] [Google Scholar]
- Ruderman AJ. Dietary restraint: A theoretical and empirical review. Psychological Bulletin. 1986;99:247–262. [PubMed] [Google Scholar]
- Ruderman AJ, Wilson GT. Weight, restraint, cognitions and counterregulation. Behavior, Research, and Therapy. 1979;17:581–590. doi: 10.1016/0005-7967(79)90102-5. [DOI] [PubMed] [Google Scholar]
- Safer DL, Agras WS, Lowe MR, Bryson S. Comparing two measures of eating restraint in bulimic women treated with cognitive-behavioral therapy. International Journal of Eating Disorders. 2004;36:83–8. doi: 10.1002/eat.20008. [DOI] [PubMed] [Google Scholar]
- Smith CF, Geislman PJ, Williamson DA, Champagne CM, Bray GA, Ryan D. Association of dietary restraint and disinhibition with eating behavior, body mass, and hunger. Eating and Weight Disorders. 1998;3:7–15. doi: 10.1007/BF03354907. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Lowe MR. Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment. 2004;16:51–59. doi: 10.1037/1040-3590.16.1.51. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint and hunger. Journal of Psychosomatic Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The Eating Inventory. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- Pullar JD, Webster AJ. The energy cost of fat and protein deposition in the rat. British Journal of Nutrition. 1977;37:355–363. doi: 10.1079/bjn19770039. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Frijters JE, van Staveran WA, Defares PB, Beurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Wardle J, Beales S. Restraint and food intake: an experimental study of eating patterns in the laboratory and in normal life. Behavior Research and Therapy. 1987;25:179–85. doi: 10.1016/0005-7967(87)90044-1. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J. Dietary restraint and disinhibition: Is restraint a homogenous construct? Appetite. 1991;16:45–55. doi: 10.1016/0195-6663(91)90110-e. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J, Stunkard AJ, Pudel V. Validation of the flexible and rigid control dimensions of dietary restraint. International Journal of Eating Disorders. 1999;26:53–64. doi: 10.1002/(sici)1098-108x(199907)26:1<53::aid-eat7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Lawson OJ, Brooks ER, Wozniak PJ, Ryan DH, Bray GA, et al. Association of body mass with dietary restraint and disinhibition. Appetite. 1995;25:31–41. doi: 10.1006/appe.1995.0039. [DOI] [PubMed] [Google Scholar]


