Abstract
PURPOSE
To describe two cases of peripapillary retinal schisis in patients with glaucoma without evidence of optic nerve pits, pseudopits, or X-linked retinoschisis.
DESIGN
Two observational case reports and literature review.
METHODS
Imaging of the peripapillary nerve fiber layer and schisis cavities was completed in two patients, and one patient was followed over time.
RESULTS
The first patient, diagnosed with narrow angle glaucoma, was noted to have peripapillary schisis in the right eye with matching changes on visual field and optical coherence tomographic (OCT) results. Follow-up examination revealed that the schisis disappeared in the right eye while appearing in the left. The findings were verified with high-speed ultra-high-resolution OCT performed in both eyes. The second case involved a patient with anatomically narrow angles, high intraocular pressure (IOP), and peripapillary schisis extending into the macula.
CONCLUSIONS
Peripapillary retinoschisis may represent a unique sequelae of intraocular fluctuations in patients with uncontrolled glaucoma. Further studies are needed to better understand this disease process.
Macular and peripapillary retinoschisis have historically been linked to X-linked retinoschisis, optic nerve pits, or colobomas.1–4 We obtained institutional review board exemption to report two cases involving peripapillary retinoschisis without apparent optic nerve pits, pseudopits, or colobomas, and to discuss the potential association between spontaneous retinal schisis resolution and increased intraocular pressure (IOP).
CASE 1
A 48-year-old woman with a nine-year history of glaucoma presented with IOPs of 31 right eye (OD) and 21 left eye (OS) and occludable angles. Manifest refraction was −1.00 diopters OD and −0.75 diopters OS. The OD had peripapillary retinoschisis extending into the macula with no apparent vitreous detachment or optic nerve pit, although there was inferotemporal cupping to the disk margin in the area of the schisis. Visual field testing was normal in the OS, and there was a superior arcuate scotoma in the OD. Standard optical coherence tomography (OCT) (StratusOCT; Carl Zeiss Meditec, Dublin, California, USA) artifactually reported schisis cavities as retinal nerve fiber layer (RNFL) thickening (Figure 1); Heidelberg retinal tomography revealed normal RNFL in the OS and RNFL thinning in the inferotemporal segment of the OD. IOP improved after bilateral laser peripheral iridectomies and bimatoprost therapy.
FIGURE 1.
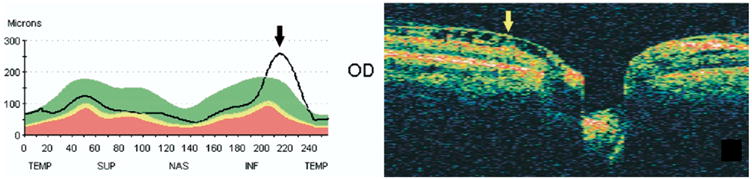
(Left) Optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) scan of schisis in right eye (OD) artifactually reported as RNFL thickening inferotemporally (arrow). (Right) StratusOCT optic nerve head scan of OD showed inner retinal schisis cavities in peripapillary region (arrow).
One year later, IOPs were 21 OD and 26 OS with patent iridectomies. StratusOCT and high-speed ultra-high-resolution OCT showed resolution of schisis on the right-side with RNFL thinning (Figure 2). StratusOCT in the OS showed multiple peripapillary schisis cavities extending into the macula that were not present on previous testing, and high-speed ultra-high-resolution OCT scans revealed distinctive splitting of the peripapillary RNFL and inner plexiform layer (Figure 3; see Supplemental Figure and Videos at AJO.com).
FIGURE 2.
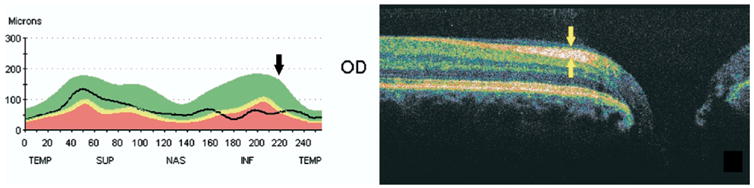
(Left) StratusOCT retinal nerve fiber layer (RNFL) scan showing RNFL thinning (arrow) and (Right) high-speed, ultra-high-resolution optical coherence tomography (OCT) (6 × 1.4-mm slice) of peripapillary retina and macula of OD showing resolution of schisis cavities (arrows).
FIGURE 3.
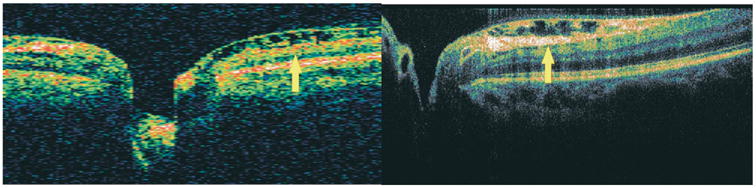
(Left) Peripapillary StratusOCT and (Right) high-speed, ultra-high-resolution optical coherence tomography (OCT) (6 × 1.4-mm slice) of left eye showing peripapillary and macular schisis cavities (arrows).
CASE 2
A 64-year-old woman who had received a diagnosis of anatomically narrow angles and IOPs of 26 OD and 28 OS was referred for bilateral laser peripheral iridectomy. Manifest refraction was +0.50 diopters OD and +1.00 diopters OS. Examination revealed occludable angles bilaterally with optic nerve cupping greater on the left-side. No vitreous detachments or optic nerve pits were noted, and the neuroretinal rims were intact. Ultrasound biomicroscopy (Ophthalmic Technologies, Toronto, Ontario, Canada) revealed occludable angles in both eyes. Dilated fundus examination and StratusOCT revealed inferotemporal peripapillary schisis OD extending into the macula. IOP stabilized after bilateral laser peripheral iridectomies (LPIs) and the schisis persisted through six months of follow-up.
Retinoschisis, splitting of retinal layers, is most commonly categorized as senile or juvenile. Senile retinoschisis results from the coalescence of outer plexiform or nerve fiber layer microcystic spaces in areas of peripheral cystoid degeneration. Juvenile X-linked retinoschisis, on the other hand, presents with schisis cavities in the fovea and periphery of the retina corresponding histologically to nerve fiber layer, and inner nuclear and/or outer plexiform layer splitting.5
In the two cases we report, both patients had a history of narrow angles with increased IOP. Peripapillary schisis extending into the macula was evident in both cases despite the absence of pits on clinical examination and imaging. Further, the thinning of the RNFL in case one was masked by and perhaps related to the schisis in the patient’s OD. It is possible that small changes in axial length accompanying fluctuations in IOP may have played a role in schisis formation. These changes may lead to vitreous traction, with or without microscopic breaks in the inner retina related to high IOP, and eventual development of schisis. Controlling IOP fluctuations in case 1 may have resulted in schisis resolution. Given the modest IOP reductions in our patient, this is a potential but unlikely explanation for the spontaneous resolution of retinoschisis.
In conclusion, we report two cases of isolated peripapillary and macular retinoschisis in the absence of any obvious or visible optic nerve head pits. In one case, the retinoschisis resolved in one eye while appearing in the fellow eye. We present, for the first time, high-speed ultra-high-resolution OCT evidence of retinoschisis in one case and show involvement of specific retinal layers without detectable evidence of an optic nerve pit.
Supplemental Data
Acknowledgments
This study was supported in part by National Institutes of Health contracts R01-EY013178-06, RO1-EY11289-20, and P30-EY008098, The Eye and Ear Foundation, Pittsburgh, Pennsylvania, an unrestricted grant from Research to Prevent Blindness, Inc, New York, New York, National Science Foundation contract ECS-0119452, Air Force Office of Scientific Research contract FA9550-040-1-0011, and Medical Free Electron Laser Program contract FA9550-040-1-0046. Dr Fujimoto and Dr Schuman received royalties from intellectual property licensed by MIT to Carl Zeiss Meditec. Dr Schuman received research support from Carl Zeiss Meditec. Involved in design and conduct of study (M.Y.K., J.S.S.); collection of data (M.Y.K., G.W., H.I.); management (M.Y.K., J.S.S.); analysis (M.Y.K., H.I., G.W., V.J.S., M.W.); interpretation of the data (M.Y.K., H.I., G.W., V.J.S., M.W.); and preparation, review, or approval of the manuscript (M.Y.K., R.J.N., J.S.S., J.G.F., J.S.D.).
References
- 1.Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106:61–67. doi: 10.1001/archopht.1988.01060130067030. [DOI] [PubMed] [Google Scholar]
- 2.Brown GC, Shields JA, Patty BE, Goldberg RE. Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979;97:1341–1344. doi: 10.1001/archopht.1979.01020020083020. [DOI] [PubMed] [Google Scholar]
- 3.Spaide RE, Costa DL, Huang SJ. Macular schisis in a patient without an optic disk pit optical coherence tomographic findings. Retina. 2003;23:238–240. doi: 10.1097/00006982-200304000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Tantri A, Vrabec TR, Cu-Unjieng A, Frost A, Annesley WH, Jr, Donoso LA. X-linked retinoschisis: a clinical and molecular genetic review. Surv Ophthalmol. 2004;49:214–230. doi: 10.1016/j.survophthal.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Madjarov B, Hilton GF, Brinton DA, Lee SS. A new classification of the retinoschises. Retina. 1995;15:282–285. doi: 10.1097/00006982-199515040-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


