Summary points
• Of the adult Western population, 10-15% will develop gallstones, with between 1% and 4% a year developing symptoms
• The incidence of gallstones increases with age, with family history being an important risk factor
• People with asymptomatic gallstones develop gallstone related problems at a rate of 1%-4% a year, with small stones being more dangerous than large as they can cause pancreatitis
• Ursodeoxycholic acid does not reduce symptoms from gallstones but may be useful in preventing their formation in high risk groups
• Percutaneous cholecystostomy is a good treatment for patients at high surgical risk
• Day case laparoscopic cholecystectomy should be the default for elective procedures.
• Cholecystectomy should be performed on the index admission for biliary symptoms
About 10-15% of the adult Western population will develop gallstones, with between 1% and 4% a year developing symptoms.1 From April 2005 to March 2006, 49 077 cholecystectomy procedures took place in England,2 a 10th of the number of procedures in the United States.3
The management of gallstone disease is changing rapidly, with an increase in day case surgery and in cholecystectomy during the index admission for cholecystitis and with the advent of natural orifice transluminal endoscopic surgery.
This review focuses on the problems that gallstones cause and their optimal treatment based on current evidence.
Who gets gallstones?
Gallstones occur when there is an imbalance in the chemical constituents of bile that results in precipitation of one or more of the components. Why this occurs is unclear, although certain risk factors are known.
Gallstones are seen in all age groups but the incidence increases with age.4 The old adage “fat and fertile, female and forty” tells only part of the story. Oestrogen does cause more cholesterol to be excreted into bile, and obesity (body mass index >30) is a risk factor.4 However, genetics also plays a part, accounting for 25% of the phenotypic variance among twins,5 thereby adding a fifth “f” (family history) to the adage. Other risk factors include pregnancy, rapid weight loss (such as after obesity surgery), parenteral nutrition, loss of bile salts (terminal ileitis or after ileal resection), and diabetes via the metabolic syndrome.4
What problems do gallstones cause?
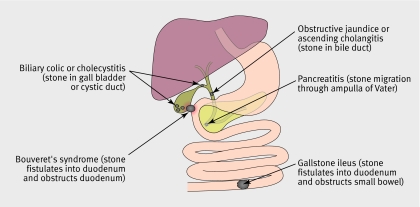
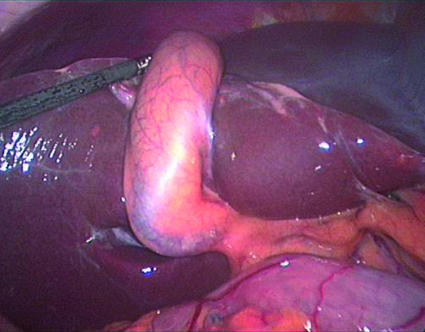
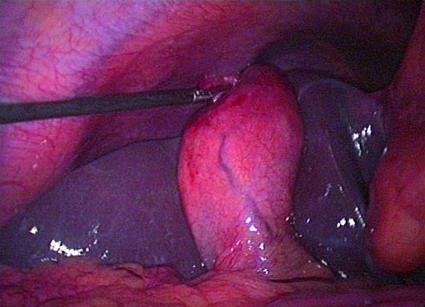
Gallstones can cause various problems (figure 1), the most common being biliary colic (56%) (fig 2) and acute cholecystitis (36%) (fig 3), as shown in a study from the United States, which mirrors our experience in the United Kingdom.6
Fig 1 Problems caused by gallstones
Fig 2 Laparoscopic photograph of gall bladder in patient with symptoms of biliary colic
Fig 3 Laparoscopic photograph of gall bladder in patient with symptoms of cholecystitis
Biliary colic/cholecystitis
Biliary colic and cholecystitis share a spectrum of symptoms, and no exact time course or definition exists to separate them. The tableoutlines the symptoms and signs.
Symptoms and signs of biliary colic and acute cholecystitis
| Pain | Nausea or vomiting | Tenderness in right upper quadrant | Inflammatory signs | |||
|---|---|---|---|---|---|---|
| Type | Location | Duration | ||||
| Biliary colic | Colic | Upper abdomen or right upper quadrant | <8 hours | Yes | No | No |
| Acute cholecystitis | Colic | Upper abdomen or right upper quadrant | >8 hours | Yes | Yes | Yes |
Jaundice
If the bile duct becomes partially or completely obstructed, bilirubin, conjugated in the liver with glucoronic acid, cannot be excreted into the bowel and the levels increase in the bloodstream. The patient becomes jaundiced, and as a result of excretion of the water soluble conjugated bilirubin, the urine becomes dark. The stools are pale owing to an absence in the faeces of stercobilin, a breakdown product of bilirubin in the intestine. Obstruction leading to jaundice is caused most commonly by a stone migrating into the bile duct but can be due to compression of the common hepatic duct by a stone in the neck of the gall bladder or cystic duct (Mirizzi's syndrome).
Ascending cholangitis
Ascending cholangitis results from infection in a partially or completely obstructed bile duct. Stasis leads to an increase in the resident bacterial flora. The risk is increased if there is potential for added infection to be introduced into the obstructed biliary system—for example, during endoscopic retrograde cholangiopancreatography. Charcot's triad is diagnostic (fever—usually with rigors—jaundice, and right upper quadrant pain).
Pancreatitis
During the passage of stones from the gallbladder into the bowel, transitory obstruction of the biliopancreatic duct (the common channel) occurs in the region of the ampulla, which initiates premature activation of enzymes in the pancreas, leading to pancreatitis (gallstone migration theory). The resulting pain is classically epigastric, constant, radiating through to the back, and relieved by bending forwards. Vomiting is often profuse.
Bouveret's syndrome and gallstone ileus
Gallstones may fistulate directly into the duodenum from the gallbladder during a period of often silent inflammation. The stone can impact in the duodenum leading to duodenal obstruction (Bouveret's syndrome). Alternatively, it can impact at the narrowest section of healthy small bowel, situated where the embryological vitello-intestinal duct once existed in the terminal ileum (a Meckel's diverticulum is the embryological remnant). This leads to small bowel obstruction known as gallstone ileus—a misnomer, as the small bowel obstruction is mechanical and not an ileus. Gallstone ileus is often diagnosed intraoperatively, though supine abdominal radiography may show air in the biliary tree (as a result of the fistula) or indeed the stone.
Gallbladder cancer
Gallstones are a known risk factor for gallbladder cancer. However, this cancer is rare, accounting for 0.3% of patients with gallstone disease in a study from the United States. Furthermore, it is usually either advanced at presentation or discovered as an incidental finding during cholecystectomy.6
How are biliary colic and cholecystitis diagnosed?
The patient's history is crucial in diagnosing biliary colic or cholecystitis. Examination will help to identify the presence of biliary inflammation and exclude the presence of masses or hepatomegaly, which can cause pain in the right upper quadrant. Liver function tests are a useful indicator of a possible stone in the bile duct. Ultrasonography is the key diagnostic test used to identify the presence of stones, biliary tract dilatation, and thickening of the wall of the gall bladder indicating chronic disease. However, although the accuracy of ultrasonography in detecting gallstones is quoted as 98% in textbooks7 we could find no studies showing this. Certainly the absence of stones on ultrasound scans does not exclude their existence, as very small stones or sludge can be missed. If clinically the diagnosis is highly likely, an interval ultrasound scan should be performed.
What if gallstones are found incidentally?
People with asymptomatic gallstones develop problems related to gallstones at a rate of 1%-4% a year.1 This means that for most of the population, prophylactic cholecystectomy is unnecessary as the balance of risks and benefits is in favour of “watch and wait.” However, a young patient will have a higher risk of developing problems, as there is more time in which to do so, and the balance may therefore favour treatment. In addition, small stones can be more dangerous than large ones. A well conducted case series study from the Netherlands involving 528 patients identified small stones as an independent risk factor for pancreatitis.8
In general, the decision to treat should be made on a case by case basis, taking into account the age of the patient, the ultrasound findings, and the presence of any symptoms, regardless of how vague these are.
Treatment
Non-surgical
Analgesia for acute attack of biliary colic or cholecystitis
In the acute, out of hospital setting, diclofenac and an opioid (morphine or pethidine) are very effective, used in combination or separately. Since the symptoms are often associated with vomiting, a suppository or injection is recommended.
Drug dissolution therapy
Ursodeoxycholic acid has been shown to be useful in preventing gallstones. A prospective study examining the rate of formation of gallstones in 152 patients after obesity surgery (a known risk factor for developing gallstones) randomised patients to 500 mg of daily ursodeoxycholic acid or to placebo, for six months or until stones developed. The researchers found that gallstone formation was significantly less likely to occur with ursodeoxycholic acid than with placebo at 12 months (3% v 22%) and at 24 months (8% v 30%).9
However, ursodeoxycholic acid does not seem to be useful once stones have developed. A prospective, randomised, double blind, placebo controlled trial from the Netherlands in 177 highly symptomatic patients with gallstones scheduled for cholecystectomy found that ursodeoxycholic acid did not reduce biliary symptoms.10
Percutaneous drainage
Percutaneous cholecystostomy allows resolution of sepsis in patients at high surgical risk. A retrospective review of 55 patients treated by percutaneous transhepatic cholecystostomy found a successful biliary drainage rate of 98%; 95% of patients recovered well and left hospital.11
Surgical
Laparoscopic versus open surgery
A Cochrane review comparing laparoscopic with open cholecystectomy found no differences in mortality, complications, or operative time.3 However, laparoscopic cholecystectomy, when compared with classic open cholecystectomy, was associated with a significantly shorter hospital stay (difference, −3 days (95% confidence interval −3.9 days to −2.3 days)) and quicker convalescence (−22.5 days (−36.9 days to −8.1 days)). These results support the recommendation by surgeons for laparoscopic cholecystectomy rather than open cholecystectomy.
However, a Cochrane review comparing laparoscopic with small incision (<8 cm) cholecystectomy found no differences in mortality, complications, and postoperative recovery.12 In addition, small incision cholecystectomy had a significantly shorter operative time. The complication rate in the studies reviewed was high: 17% in the laparoscopic group versus 17.5% in the small incision group, if gallbladder perforation is excluded as a complication. These rates are higher than those in the Cochrane review comparing laparoscopic with open cholecystectomy (5.4% and 10.1% respectively).3
The conclusions of the Cochrane reviews are reinforced by more recent publications from Finland and Sweden.13 14
Day case surgery
A randomised clinical trial of day case versus “overnight stay” laparoscopic cholecystectomy from Sweden found no difference in complication rate or patients' acceptance, though the day case procedures cost less.15 A feasibility study from the Royal Berkshire Hospital identified an acceptable complication rate for overnight stay surgery of 14.3% and readmission rate of 1.9% among 154 patients having day case surgery and classified as grade 1 or 2 according to the American Association of Anaesthesiologists preoperative grading system for physical status (1=normal healthy patient, 5= moribund patient).16
The NHS Institute for Innovation and Improvement2 showed that the average length of stay for laparoscopic cholecystectomy is 2.6 (range 1.2 to 6) days. If the average length of stay was reduced by one day, there would be an annual saving for the NHS of about 35 400 bed days (£8m (€12m; $16m)), based on a bed day cost of £225). A trust performing 300 elective inpatient laparoscopic cholecystectomies a year could expect to save about £100 000 a year by performing 40% as day case procedures and reducing the length of stay for the rest by one day. Currently, the national average day case laparoscopic cholecystectomy rate is 6.4%, with the highest performing trusts achieving a rate of 40%-50%.2
When should cholecystectomy be performed after an emergency admission for biliary colic or cholecystitis?
A Cochrane review compared early laparoscopic cholecystectomy (within seven days of onset of symptoms) with delayed laparoscopic cholecystectomy (more than six weeks after index admission) with regard to benefits and harms.17 The review included five trials with 451 randomised patients. It found no difference in bile duct injury or conversion rate to open surgery, although the conversion rate was high in both early cholecystectomy (20.3%) and delayed cholecystectomy (23.6%). The total hospital stay was three days shorter in the early surgery group. The researchers concluded that early laparoscopic cholecystectomy is safe and shortens hospital stay but that further trials are needed as the confidence intervals were wide. Further evidence for early cholecystectomy comes from a prospective case series from Taunton.18 This study showed a 28.5% readmission rate with gallstone related complications for people on the waiting list for surgery after emergency admission with acute cholecystitis. The authors concluded that all patients presenting as an emergency with symptomatic gallstones and are admitted should be offered cholecystectomy, a point echoed by the NHS Institute for Innovation and Improvement.2
Although the conversion rate (from laparoscopic to open surgery) was high in the randomised studies included in the Cochrane review, an audit before and after implementation of a specialist led service for urgent cholecystectomy in Portsmouth illustrated a fall in the conversion rate from 32% to 12%.19 The same study showed a reduction in the rate of unplanned readmissions, from 19% to 3.6%.
Postoperative complications
Cholecystectomy is not without risk. Complications include haematoma in the gall bladder bed, infection (usually of the haematoma), bile leak, inadvertent injury (to the bowel or bile duct), and retained stone in the bile duct. The most serious is bile duct injury, occurring at a rate of 0.2% in both laparoscopic and open surgery.3 Further surgery may be needed to repair the bile duct or to join the bile duct to the bowel by anastomosis. In addition, bile duct injury is often further complicated by concomitant hepatic vascular injury.
Possibilities for the future
A new era is developing in the treatment of gastrointestinal conditions. It seems feasible that major intraperitoneal surgery may be performed without skin incisions, with access to the peritoneal cavity via natural orifices, the mouth (via the stomach), the rectum, and the vagina, using flexible endoscopes. This experimental technique is known as natural orifice transluminal endoscopic surgery. Although no research has yet been published on resections in humans, the first report of cholecystectomy in a porcine model was published in 2005.20 The principle is gathering momentum, and developments are likely to be rapid, with working groups set up to move the concept forward.21
Sources and selection criteria
We searched the PubMed MeSH database for the term “gallstones”, with the subheadings: complications, diagnosis, diet therapy, drug therapy, economics, epidemiology, aetiology, genetics, history, mortality, surgery, therapy, and ultrasonography. We limited the search to human, English, adult (19+ years) and to articles published in the past five years. The search resulted in 533 hits. We displayed abstracts of interest using AbstractPlus, which provides links to related articles. In addition, we searched the Cochrane Library and our personal archive of references.
Additional educational resources
For healthcare professionals
WebSurg (www.websurg.com)—A free virtual surgical university, accessible from anywhere in the world through the internet. Although geared to surgical training, it is also useful for the non-specialist wanting an update. It provides operative technique, video clips, and expert opinion about a wide variety of surgical conditions
For patients
Patient UK (www.patient.co.uk)—Comprehensive, free, up to date health information as provided by general practitioners to patients during consultations (www.patient.co.uk/showdoc/23068740/).
A patient's story
About two years ago, I started to experience bouts of abdominal pain, initially low grade but increasing to crescendos of severe pain lasting several hours. It was often associated with nausea but no vomiting. My symptoms initially occurred once every month or two, but more recently, every few weeks. My general practitioner organised an ultrasound scan, which showed that I had gallstones. I was referred to a specialist. However, while waiting to be seen in the clinic, I had two visits to the accident and emergency department and received morphine for pain control. After my second visit to the emergency department, I saw my general practitioner again, who did a blood test, only to find my liver tests were abnormal, and urgent admission to hospital was arranged. An ultrasound scan showed I now had a stone in my bile duct. I was operated on during that hospital stay, which included laparoscopic removal of my gall bladder and the bile duct stone. I had a drain left in when I went home, but I came back to the outpatient department two days later for the drain to be removed. I now feel well and am pain free; long may it last.
Tips for non-specialists
• If a patient has intermittent symptoms suggesting gallstone disease and if an ultrasound scan confirms the presence of gallstones, he or she should be referred to a specialist unit for possible cholecystectomy
• A patient with ongoing, unrelenting symptoms of gallstone disease should be referred to the emergency surgical unit for assessment and an index admission cholecystectomy
Contributors: Both authors performed the literature search. GS wrote the article and ANK edited it. Both authors are guarantors.
Competing interests: None declared.
Provenance and peer review: Commissioned and externally peer reviewed.
References
- 1.Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg 2004;91:734-8. [DOI] [PubMed] [Google Scholar]
- 2.NHS Institute for Innovation and Improvement. Focus on: cholecystectomy—a guide for commissioners. 2006. www.institute.nhs.uk/quality_and_value/high_volume_care/focus_on%3a_high_volume_care.html
- 3.Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 2006;(4):CD006231. [DOI] [PMC free article] [PubMed]
- 4.Shaffer EA. Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol 2006;20:981-96. [DOI] [PubMed] [Google Scholar]
- 5.Katsika D, Grjibovski A, Einarsson C, Lammert F, Lichtenstein P, Marschall HU. Genetic and environmental influences on symptomatic gallstone disease: a Swedish study of 43,141 twin pairs. Hepatology 2005;41:1138-43. [DOI] [PubMed] [Google Scholar]
- 6.Glasgow RE, Cho M, Hutter MM, Mulvihill SJ. The spectrum and cost of complicated gallstone disease in California. Arch Surg 2000;135:1021-5. [DOI] [PubMed] [Google Scholar]
- 7.Karani J, Sutton D. Textbook of radiology and imaging Oxford: Churchill Livingstone, 2003:715.
- 8.Venneman NG, Buskens E, Besselink MG, Stads S, Go PM, Bosscha K, et al. Small gallstones are associated with increased risk of acute pancreatitis: potential benefits of prophylactic cholecystectomy? Am J Gastroenterol 2005;100:2540-50. [DOI] [PubMed] [Google Scholar]
- 9.Miller K, Hell E, Lang B, Lengauer E. Gallstone formation prophylaxis after gastric restrictive procedures for weight loss: a randomized double-blind placebo-controlled trial. Ann Surg 2003;238:697-702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Venneman NG, Besselink MG, Keulemans YC, Vanberge-Henegouwen GP, Boermeester MA, Broeders IA, et al. Ursodeoxycholic acid exerts no beneficial effect in patients with symptomatic gallstones awaiting cholecystectomy. Hepatology 2006;43:1276-83. [DOI] [PubMed] [Google Scholar]
- 11.Spira RM, Nissan A, Zamir O, Cohen T, Fields SI, Freund HR. Percutaneous transhepatic cholecystostomy and delayed laparoscopic cholecystectomy in critically ill patients with acute calculus cholecystitis. Am J Surg 2002;183:62-6. [DOI] [PubMed] [Google Scholar]
- 12.Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus small-incision cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev 2006;(4):CD006229. [DOI] [PMC free article] [PubMed]
- 13.Harju J, Juvonen P, Eskelinen M, Miettinen P, Paakkonen M. Minilaparotomy cholecystectomy versus laparoscopic cholecystectomy: a randomized study with special reference to obesity. Surg Endosc 2006;20:583-6. [DOI] [PubMed] [Google Scholar]
- 14.Ros A, Nilsson E. Abdominal pain and patient overall and cosmetic satisfaction one year after cholecystectomy: outcome of a randomized trial comparing laparoscopic and minilaparotomy cholecystectomy. Scand J Gastroenterol 2004;39:773-7. [DOI] [PubMed] [Google Scholar]
- 15.Johansson M, Thune A, Nelvin L, Lundell L. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg 2006;93:40-5. [DOI] [PubMed] [Google Scholar]
- 16.Leeder PC, Matthews T, Krzeminska K, Dehn TC. Routine day-case laparoscopic cholecystectomy. Br J Surg 2004;91:312-6. [DOI] [PubMed] [Google Scholar]
- 17.Gurusamy KS, Samraj K. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev 2006;(4):CD005440. [DOI] [PubMed]
- 18.Cheruvu CV, Eyre-Brook IA. Consequences of prolonged wait before gallbladder surgery. Ann R Coll Surg Engl 2002;84:20-2. [PMC free article] [PubMed] [Google Scholar]
- 19.Mercer SJ, Knight JS, Toh SK, Walters AM, Sadek SA, Somers SS. Implementation of a specialist-led service for the management of acute gallstone disease. Br J Surg 2004;91:504-8. [DOI] [PubMed] [Google Scholar]
- 20.Park PO, Bergstrom M, Ikeda K, Fritscher-Ravens A, Swain P. Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis (videos). Gastrointest Endosc 2005;61:601-6. [DOI] [PubMed] [Google Scholar]
- 21.Rattner D, Kalloo A. ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc 2006;20:329-33. [DOI] [PubMed] [Google Scholar]