Abstract
Cytokines may be crucially involved in the pathogenesis of inflammatory bowel diseases (IBD), but it remains controversial whether interferon (IFN)-γ, a typical proinflammatory cytokine, is an essential mediator to cause the disorders. In the present study, IFN-γ–/– and wild-type (WT) C57BL/6 mice were fed 2·5% dextran sodium sulphate (DSS) in drinking water for 7 days, in order to investigate DSS-induced intestinal inflammation. The DSS-treated WT mice exhibited a robust production of IFN-γ in the gut, a remarkable loss of body weight, as well as high rate of mortality (60%). In striking contrast, IFN-γ deficient mice did not develop DSS-induced colitis, as indicated by the maintenance of body weight and survival rate of 100%. Severe intestinal inflammation was demonstrated exclusively in WT animals in terms of the shortening of the bowel as well as the elevation of the disease activity index, myeloperoxidase (MPO) activity and serum haptoglobin level. Histological study of DSS-treated WT intestine revealed disruption of mucosal epithelium and massive infiltration of inflammatory cells, while the organ from IFN-γ–/– mice remained virtually normal in appearance. Enzyme-linked immunosorbent assay (ELISA) analyses indicated abundant production of three chemokines, i.e. monokine induced by interferon-γ (MIG), interferon-inducible protein 10 (IP-10) and monocyte chemoattractant protein-1 (MCP-1), in the DSS-irritated intestine of WT but not of IFN-γ–/– mice. The present results demonstrate clearly that IFN-γ plays indispensable roles in the initiation of DSS colitis, and some chemokines are produced in an IFN-γ-dependent fashion.
Keywords: cytokine, dextran sulphate sodium-induced colitis, inflammatory bowel disease, interferon-gamma
Introduction
The inflammatory bowel diseases (IBD) are chronic disorders of the gastrointestinal tract characterized by diarrhoea, haemorrhage, lower abdominal pain and body weight loss [1]. IBD affect especially young people who suffer throughout their life from these symptoms with frequent remissions and exacerbations. Crohn's disease (CD) and ulcerative colitis (UC) are categorized as typical IBD. Although the pathogenesis of IBD has not been elucidated fully, there is increasing evidence that a series of cytokines [2] and chemokines [3] are produced locally in the inflammatory lesions and play important roles in the progression of the diseases.
Dextran sodium sulphate (DSS)-induced colitis is widely regarded as a useful murine model of IBD, promoting understanding of the cellular and molecular basis of IBD [4,5]. It has been reported that the expression profile of cytokines as well as histological changes in acute DSS-induced colitis are similar to those observed in human IBD, particularly UC [6]. In DSS-induced acute colitis, massive infiltrates appear in the inflammatory lesions, consisting mainly of T and B lymphocytes, macrophages and neutrophils, which produce a variety of proinflammatory cytokines including tumour necrosis factor (TNF)-α, interleukin (IL)-6, IL-8, IL-12, IL-17 and interferon (IFN)-γ[6,7]. Among them, IFN-γ is a typical proinflammatory cytokine with pleiotropic functions including antiviral activity, augmentation of major histocompatibility complex (MHC) expression and stimulation of T and natural killer (NK) cells [8]. Accumulating evidence has implicated IFN-γ as being crucially involved in chronic inflammatory diseases of various organs such as rheumatoid arthritis [9].
However, it remains controversial whether IFN-γ plays indispensable roles in the pathogenesis of IBD. Some reports showed that IFN-γ is produced abundantly by cultured colonic mucosal tissue [10] and intestinal lamina propria mononuclear cells [11–13] from patients of CD [10,12–14] and UC [13], while robust production of IFN-γ is also seen in the colon of DSS-treated mice [7]. A neutralization antibody against IFN-γ partially, but significantly, ameliorated chronic intestinal inflammation in the DSS-induced colitis murine model [15], as well as colitis in severe combined immunodeficient (SCID) mice that had been transplanted with CD45RBhigh CD4+ T cells [16]. Although these studies suggest that IFN-γ is a key cytokine that is crucially involved in induction and progression of IBD, other studies do not support this notion. In that regard, it has been reported that IFN-γ was not produced significantly by lymphoid cells in the intestinal mucosa of patients of CD [17] and UC [17–19], as well as haematopoietic cells in IBD patients [20,21]. The proportion of IFN-γ-producing T cells [22] was reportedly decreased in IBD patients. In contrast to the study by Obermeier et al. [15], DSS-induced colitis was not affected significantly by administration of anti-IFN-γ neutralization antibody in another similar study [23]. Moreover, Camoglio et al. and Tozawa et al. demonstrated that IFN-γ receptor–/– mice developed inflammatory colitis after administration of 2, 4, 6-trinitrobenzen sulphonic acid (TNBS) to a similar extent as WT mice [24,25].
To investigate further the roles of IFN-γ in the development of IBD, we administered IFN-γ-deficient mice with DSS and examined acute intestinal inflammation in the animals. We also estimated expression levels of some chemokines in the colon in an attempt to investigate the mechanisms of IFN-γ-mediated IBD pathogenesis.
Materials and methods
Animals
All the animal experiments were performed according to the approved guidelines of Kyoto Prefectural University of Medicine. IFN-γ–/– mice have been described previously [26]. They were fed a standard diet (Oriental Yeast, Tokyo, Japan) and housed under specific pathogen free (SPF) conditions. Acute colitis was induced by administering 2·5% DSS (mol. wt 5000; lot no. CEN0649, Wako, Japan) in drinking water for 7 days. Healthy control animals received tap water only.
IFN-γ concentration in the colonic tissue
Colon was removed from the animals at day 7 and rinsed with chilled phosphate-buffered saline (PBS). After being weighed, the specimen was placed in PBS supplemented with complete miniproteinase inhibitor cocktails (Roche Molecular Biochemicals, Mannheim, Germany) (1 ml per 100 mg of tissue). After homogenization, the sample was centrifuged at 11 000 g for 15 min at 4°C to precipitate the insoluble cellular debris, and supernatant was stored at −80°C until assayed. The concentration of IFN-γ was evaluated using mouse IFN-γ Quantikine enzyme-linked immunosorbent assay ELISA kits (R&D Systems, Minneapolis, MN, USA).
General assessment of colitis
Colon length was measured as an indication of colonic inflammation [27]. Briefly, the animals were anaesthetized with Sevoflurane and killed by exsanguination. The colon was resected between the ileocaecal junction and the proximal rectum, close to its passage under the pelvisternum. The colon was placed onto a non-absorbent surface and measured with a ruler, taking care not to stretch the tissue.
Body weight, occult and rectal bleeding and stool consistency were monitored daily after DSS administration. Occult bleeding was detected based on the peroxidase activity of haem in stool (occult blood slide 5 Shionogi; Shionogi, Osaka, Japan). Disease activity index (DAI) was determined by scoring change in body weight, occult blood and gross bleeding as described in Table 1[28,29].
Table 1.
Scoring system for the disease activity index (DAI). The degrees of body weight loss, stool consistency and occult/gross blood in stools were quantified as described. The DAI was calculated as the sum of the three scores [28,29].
| Score | Weight loss (%) | Stool consistency | Occult/gross blood in stools |
|---|---|---|---|
| 0 | ≤ 1 | Normal stool (well-formed pellets) | Normal (no blood in stools) |
| 1 | 1 <≤ 5 | ||
| 2 | 5 <≤ 10 | Loose stools (pasty and semiformed stools that did not adhere to the anus) | Positive occult blood in stools |
| 3 | 10 <≤ 20 | ||
| 4 | 20 < | Diarrhoea (liquid stools that adhere to the anus) | Gross bleeding in stools |
Haptoglobin concentration in mouse serum
Blood was collected from mice via the abdominal aorta under anaesthesia. The haptoglobin concentrations in the sera were determined by mouse haptoglobin ELISA Kit (Life Diagnostics Inc., West Chester, PA, USA) according to the manufacturer's protocol.
Histological observation and scoring
Colon was removed from mice killed with Sevoflurane, and divided into three parts (distal, middle and proximal parts) of approximately equal lengths. The specimens were fixed in 4% paraformaldehyde, embedded in paraffin and sliced into sections of 3 μm thickness. The sections were stained with haematoxylin and eosin (H&E), and histological analysis was performed in a blinded fashion. The histological score of individual mouse was calculated by the sum of the scores of all three parts as described in Table 2[15,23].
Table 2.
Histological scores. The degrees of epithelial damage (E) and infiltration (I) were quantified as described, and histological score was defined as the sum of the two parameters [15,23].
| Score | Epithelial damage (E) | Infiltration (I) |
|---|---|---|
| 0 | Normal morphology | No infiltrate |
| 1 | Loss of goblet cells | Infiltrate around crypt basis |
| 2 | Loss of goblet cells in large areas | Infiltrate reaching to muscularis mucosae |
| 3 | Loss of crypts | Extensive infiltration reaching the muscularis mucosae, thickening of the mucosa with abundant oedema |
| 4 | Loss of crypts in large area | Infiltration of the submucosa |
Myeloperoxidase (MPO) activity
Colon was rinsed with chilled PBS and homogenized in 0·5% hexadecyltrimethylammonium bromide (HTAB) solution (1 ml per 50 mg of tissue) by the Polytron PT1200C (Kinematica AG, Littau/Luzern, Swizerland). The homogenate was centrifuged at 11 000 g for 15 min at 4°C and supernatant was stored at −80°C until assayed. The MPO activity was determined using a myeloperoxidase assay kit (CytoStore, Calgary, Canada) according to the manufacturer's instructions.
Chemokine concentrations in the colonic tissue
Colon was rinsed with chilled PBS and homogenized (1 ml per 50 mg of tissue). After centrifugation at 11 000 g for 15 min at 4°C, the supernatant was stored at −80°C until assayed using mouse CXCL9/MIG, CXCL10/IP-10 and CCL2/JE/MCP-1 Quantikine ELISA kits (R&D Systems).
Statistical analysis
Survival curves for the treatment groups were compared using the log-rank test, while histological scores were analysed by the Mann–Whitney U-test. For other comparisons, Student's t-test was used.
Results
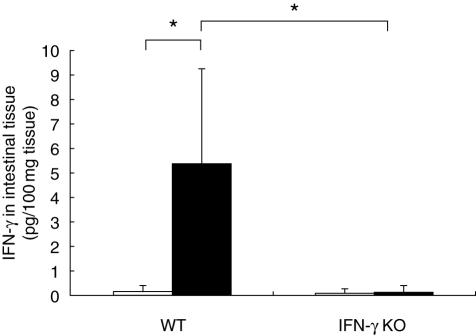
IFN-γ was significantly produced in DSS colitis
We first assessed the expression levels of IFN-γ in the colon of WT and IFN-γ–/– mice that were administered orally with 2·5% of DSS to induce acute colitis. Untreated mice were also analysed as controls. It was demonstrated clearly that the untreated WT mice produced a very low level of IFN-γ in the colon, if any, while the cytokine was drastically induced after daily administration with DSS for 7 days (Fig. 1). As expected, IFN-γ–/– mice did not express the cytokine at a detectable level, regardless of whether they had received the administration with the irritant (Fig. 1).
Fig. 1.
Interferon (IFN)-γ was produced abundantly in dextran sodium sulphate (DSS)-induced colitis. Wild-type (left) and IFN-γ knock-out (right) mice were treated with DSS for 7 days (closed bars) or left untreated (open bars). Colonic tissue was homogenized, and the resultant lysate was subjected to enzyme-linked immunosorbent assay to detect IFN-γ. Means ± s.d. of IFN-γ concentrations are shown (n = 6 in each group). *P < 0·01.
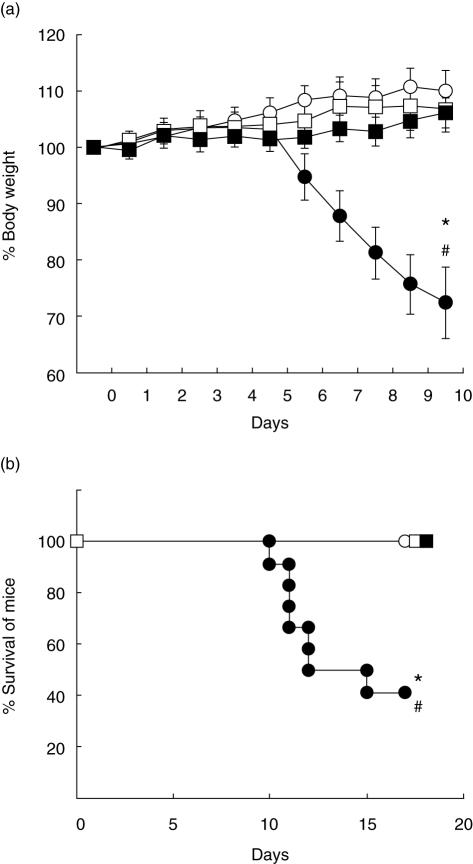
IFN-γ KO mice did not exhibit a significant sign of inflammatory colitis after DSS administration
When WT mice were administered with DSS for 7 days, they lost weight drastically starting at day 6 after initiation of the DSS treatment (Fig. 2a), and approximately 60% of mice had died by day 17 (Fig. 2b). In striking contrast, IFN-γ–/– mice treated with DSS did not lose body weight to a statistically significant degree on day 10, and their survival rate remained 100%.
Fig. 2.
Interferon (IFN)-γ–/– mice did not develop colitis after dextran sodium sulphate (DSS) administration. Wild-type (WT) (circles) and IFN-γ–/– (squares) mice were given 2·5% DSS for 7 days (closed symbols) or left untreated (open symbols) (n = 12 mice for WT groups and n = 11 mice for IFN-γ–/– groups). (a) Body weight (BW) was measured daily and means ± s.d. of percentage of BW are plotted. *P < 0·001 versus untreated WT on day 10; #P < 0·001 versus DSS-treated IFN-γ–/– on day 10. (b) Survival rates of the mice are shown. *P < 0·005 versus untreated WT; #P < 0·01 versus DSS-treated IFN-γ–/–.
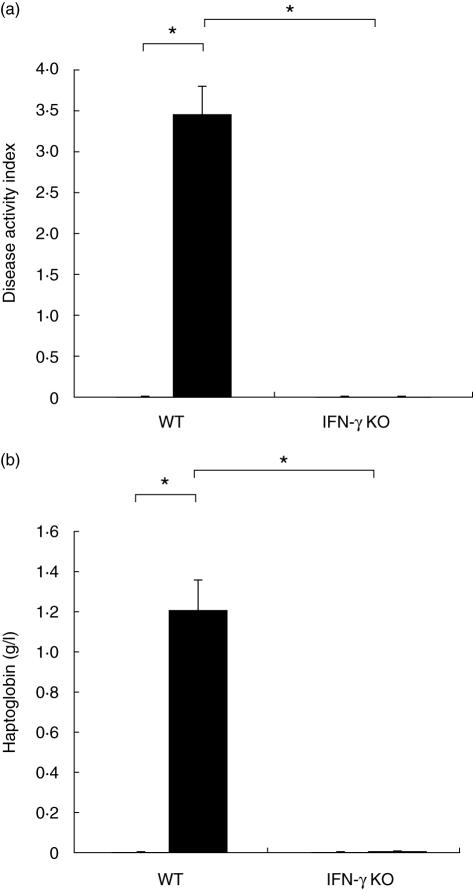
After DSS treatment, WT mice showed occult and rectal bleeding as well as diarrhoea, which were not evident in IFN-γ–/– mice given the same medication. The severity of colitis was expressed as the DAI based on three parameters, i.e. the degrees of body weight loss, diarrhoea and haemorrhage (Table 1). The DAI was remarkably higher in DSS-treated WT mice compared with non-treated WT animals (Fig. 3a). In contrast, no significant difference was demonstrated between scores for DSS-treated and non-treated IFN-γ–/– mice.
Fig. 3.
Disease activity index (DAI) and serum haptoglobin level did not increase in interferon (IFN)-γ–/– mice. WT and IFN-γ–/– mice were administered with dextran sodium sulphate (DSS) for 7 days (closed bars) or left untreated (open bars). The DAI (a) and serum haptoglobin levels (b) were determined on day 7. Data represent the means ± s.d. (a), n = 12 mice for WT groups and n = 11 mice for IFN-γ–/– groups; (b), n = 5 mice. *P < 0·001.
We then measured the concentration of serum haptoglobin, which is a typical acute-phase protein with a diagnostic significance for the progression of systemic inflammation [7]. As shown in Fig. 3b, the haptoglobin was almost undetectable in the sera of untreated mice regardless of their genetic background, while the serum concentration of the protein was remarkably high in WT mice that received DSS administrations. In sharp contrast, the IFN-γ–/– mice did not show any significant elevation in the serum titre of the inflammatory marker in spite of receiving daily treatments with DSS for 7 days. These results are compatible with the colitis symptoms described above, suggesting strongly that the IFN-γ–/– mice were extremely resistant to the intestinal inflammation triggered by DSS.
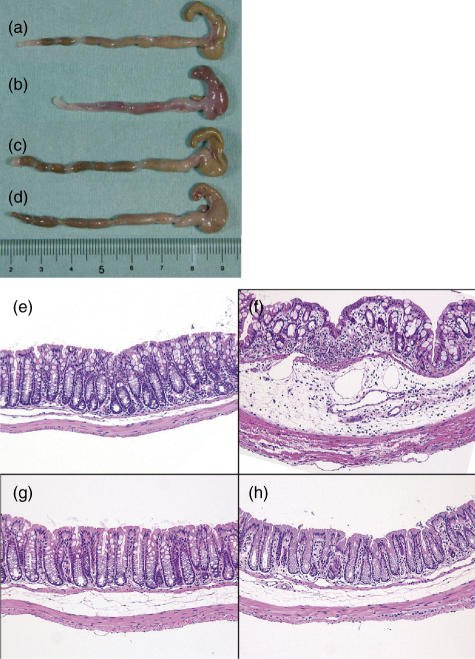
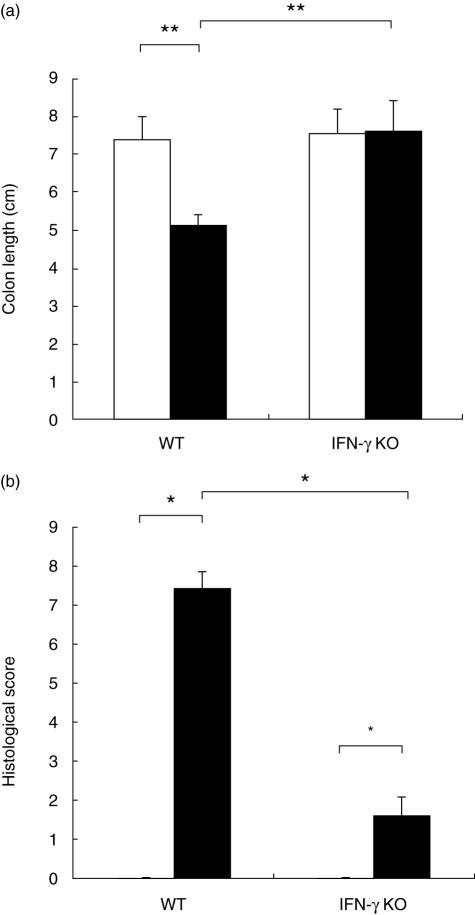
Morphological assessment also confirmed insusceptibility of IFN-γ null mice to DSS colitis
Bowels were resected from WT and IFN-γ–/– mice and subjected to macroscopic and histopathological examination. The gross appearance of the organs from the DSS-treated WT mice showed obvious reddening and shortening of the colon, which are typical signs of acute intestinal inflammation (Fig. 4a,b). On the other hand, macroscopic findings failed to indicate any significant change in the colon of IFN-γ–/– mice after the treatment with DSS (Fig. 4c,d). Statistical analysis confirmed that the mean length of colon of DSS-treated WT mice was significantly shorter than that of DSS-untreated mice, while the colon of IFN-γ KO mice did not shrink in length after DSS administration (Fig. 5a).
Fig. 4.
Macroscopic and microscopic findings of the colonic inflammation. Wild-type (a, b, e, f) and interferon (IFN)-γ–/– (c, d, g, h) mice were administered with dextran sodium sulphate (DSS) for 7 days (b, d, f, h) or left untreated (a, c, e, h). Shown are the representative gross appearance (a–d) and microscopic views of haematoxylin and eosin-stained sections (e–h) of the colons. Original magnification in (b) × 100.
Fig. 5.
Evaluation of morphological changes of dextran sodium sulphate (DSS)-induced colitis. Wild-type and interferon (IFN)-γ–/– mice were administered with DSS for 7 days (closed bars) or left untreated (open bars). Macroscopic as well as microscopic observation was performed as in Fig. 4, and the colon lengths (a) and histological scores (b) are plotted. Data represent the mean ± s.d. (a) n = 10 mice for each group; (b) n = 4 mice for each group, and three sections were examined for each mouse. *P < 0·05, **P < 0·001.
These results were confirmed by microscopic observations. The WT animals administered with DSS represented obvious manifestations of inflammatory colitis, including loss of crypts, mucosal erosions, ulcers andinfiltration of inflammatory cells (Fig. 4f), while the specimens from the DSS-administered IFN-γ–/– mice were virtually normal in appearance except for minimum epithelial injury (Fig. 4h).
To quantify these findings, histological scores were calculated based on the scoring system described in Materials and methods and Table 2. The mean histological score for DSS-treated IFN-γ–/– mice was significantly lower than that of WT mice that were given DSS (Fig. 5b). The data demonstrate that toxicity of DSS was attenuated in the mice genetically engineered to lack IFN-γ.
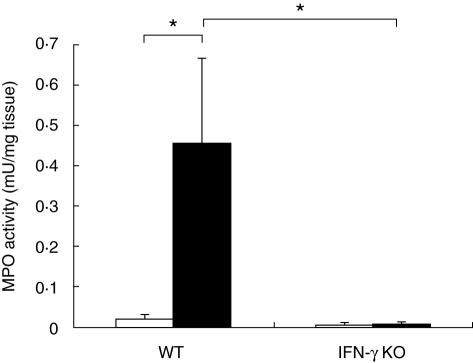
MPO activity was not elevated in the colon of IFN-γ–/– mice after DSS administration
Because MPO is a useful indicator of the extent of neutrophil infiltration, the colon was homogenized and MPO activity in the supernatant was measured. As shown in Fig. 6, WT mice treated with DSS showed drastically higher MPO activity compared with untreated WT mice, consistent with the severe intestinal inflammation in these animals. In contrast, any significant increase in the enzyme activity was not revealed in DSS-treated IFN-γ–/– mice, confirming that the genetically modified animals do not develop colitis in this experimental model (Fig. 6).
Fig. 6.
Myeloperoxidase (MPO) activity was elevated in colonic mucosa of wild-type (WT) but not of interferon (IFN)-γ knock-out mice. WT and IFN-γ–/– mice were fed dextran sodium sulphate (DSS) for 7 days (closed bars) or left untreated (open bars). The colons were homogenized and MPO activities in the lysates were measured as described in Materials and methods. Data represent the mean ± s.d. (n = 6 mice in each group). *P < 0·001.
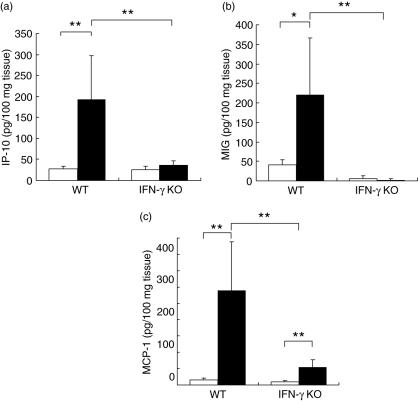
IFN-γ–/– mice are incapable of producing MIG, IP-10 and MCP-1 in response to DSS stimulation
We hypothesized that the absence of intestinal infiltrates in the DSS-stimulated IFN-γ–/– mice may be due to the lack of some chemoattractants that can be elicited in WT animals. Among the series of chemokines, we paid particular attention to IP-10 and MIG that were implicated in the pathogenesis of IBD [3,30,31]. We also examined MCP-1 that was reportedly detected in the intestine of IBD patients [3,32,33]. Interestingly, ELISA analyses proved elevation of both IP-10 (Fig. 7a) and MIG (Fig. 7b) in WT mouse colon that had been irritated by DSS, whereas neither of the chemokines was significantly secreted in the intestinal tissue of IFN-γ–/– mice. Similarly, DSS medication drastically induced MCP-1 in WT mice but not in IFN-γ null animals (Fig. 7c). The findings suggest strongly that these three chemokines may contribute to DSS-induced colitis, and IFN-γ may be responsible for the induction of the chemoattractants.
Fig. 7.
Monokine induced by interferon-γ (MIG), interferon-inducible protein 10 (IP-10) and monocyte chemoattractant protein-1 (MCP-1) were not drastically induced in colon of interferon (IFN)-γ–/– mice. Wild-type and IFN-γ–/– mice were treated with dextran sodium sulphate (DSS) for 7 days (closed bars) or left untreated (open bars). The colons were homogenized and the concentrations of IP-10 (a), MIG (b) and MCP-1 (c) in the lysates were measured by enzyme-linked immunosorbent assay. Data represent the means ± s.d. (n = 8 mice in each group). *P < 0·005, **P < 0·001.
Discussion
The present study clearly demonstrated that IFN-γ–/– mice manifested attenuated colitis after stimulation with DSS, in terms of the degree of body weight loss, DAI, histological score and MPO activity. IFN-γ was increasingly produced in the colon of DSS-treated WT mice that showed severe IBD-like symptoms. The data indicated that the proinflammatory cytokine may be essentially involved in the development of DSS-induced colitis in mice. In the colon of IFN-γ–/– mice, in contrast to WT mice, IP-10, MIG and MCP-1 were not drastically up-regulated after DSS exposure, suggesting strongly that these chemokines play important roles in the IFN-γ-mediated pathogenesis of DSS colitis probably by triggering the recruitment of leucocytes to the intestinal tissue.
It has been reported that, at the initiation of DSS colitis, DSS exerts direct toxicity to the colonic epithelial cells [34–37], subsequently increasing the permeability of the intestinal mucosa [38] and allowing transport of luminal bacterial products from the bowel lumen to submucosal tissue. DSS may also permit bacterial invasion into the mucosa by preventing macrophages from ingesting the microbes [34,39,40]. However, it has not been elucidated how these initial events triggered by DSS lead to recruitment and activation of leucocytes and in turn inflammation of the colon. Our data suggest strongly that local secretion of IFN-γ and subsequent IFN-γ-dependent induction of chemokines may, at least partly, explain the aetiological link between the DSS-mediated epithelial damage and inflammation. Another possible contribution of IFN-γ to the pathogenesis of colitis may be the impairment of a barrier function of intestinal epithelial cells [41,42].
It has been reported that anti-IFN-γ antibody failed to block, or only partially affect, development of IBD in mice [15,16,23]. The findings may not contradict our results because a small amount of IFN-γ may have survived the neutralization, while the mice with IFN-γ null phenotype completely lack the cytokine. Therefore, it may be reasonable to suppose that a trace concentration of IFN-γ at focal areas may be sufficient to cause colonic inflammation. This point should be important if IFN-γ neutralization is applied to clinical use.
IFN-γ has been shown to play an indispensable role in the infiltration of leucocytes into some organs. Propionibacterium acnes infection induced infiltration of macrophages into the liver of WT mice but not of IFN-γ–/– mice [43]. Similar findings were reported in the acetaminophen-induced hepatitis model, in which intrahepatic infiltration of leucocytes including neutrophils, macrophages and T cells was reduced in IFN-γ–/– mice compared with that in WT mice [44]. Administration of Clostridium difficile Toxin A induced massive neutrophil infiltration in the ileum of WT mice, while IFN-γ–/– mice showed only faint infiltrates in this ileitis model [45]. Our data are consistent with these earlier reports, demonstrating that IFN-γ was responsible for infiltration of leucocytes into inflammatory lesions in the DSS-induced colitis (Figs 4e–h and 6).
IP-10 and MIG are CXC chemokines that are secreted by a variety of cells at the focal areas of inflammation [14,46,47]. IP-10 is up-regulated in some Th1-mediated inflammatory disorders in human, such as psoriasis [48,49], multiple sclerosis [50,51], rheumatoid arthritis [52], sarcoid granulomatous disease [53], allograft rejection [54,55] and IBD [3,31]. MIG is induced in glomerulonephritis [56] and murine IBD models [57]. MCP-1 is a CC chemokine that has been implicated in monocyte attraction in a number of inflammatory states, i.e. rheumatoid arthritis [58], psoriasis [59], fulminant hepatic failure [60], allogeneic graft rejection [61] and IBD [3,32]. In the inflamed intestinal mucosa of patients of the CD, MCP-1 is produced by macrophages, smooth muscles and endothelial cells [62]. Although all three chemokines can be induced by IFN-γ[63,64], it has not been clarified whether or not the chemokine induction in IBD is dependent on IFN-γ. It also remains to be elucidated whether the chemokines are critically involved in the inflammatory infiltration in the bowel of IBD. The present study clearly indicates that IFN-γ is a prerequisite to the production of IP-10, MIG and MCP-1 in DSS-induced colitis (Fig. 7). Absence of inflammatory cells in DSS-stimulated IFN-γ–/– intestine (Figs 4h and 6) suggests strongly that these chemokines are important mediators to cause cellular infiltration into intestinal lesions, although further studies are required to uncover the functions of each chemokine.
Our present study focused on the acute phase of experimental colitis, in which the infiltrates in the inflammatory colon predominantly consist of neutrophils and macrophages [35]. The IFN-γ-dependent production of the chemokines, especially IP-10 and MIG, may subsequently provoke accumulation of CXCR-3-expressing T cells that are seen usually in the chronic phase of colitis. In this regard, the IFN-γ-chemokine pathway may be important to understand the mechanisms of transition from acute to chronic intestinal inflammation.
Finally, it is noteworthy that the present study strongly suggests IFN-γ to be an ideal target molecule to control IBD, providing a promising strategy for therapeutic molecular targeting for IBD.
Acknowledgments
The present work was supported by a grant-in-aid of the Japanese Ministry of Education, Culture, Sports, Science and Technology. We are grateful to Drs S. Kokura and T. Okuda (Department of Medicine, Kyoto Prefectural University of Medicine, Kyoto, Japan) for technical suggestion and helpful discussion. We also thank Dr W. T. V. Germeraad (University of Maastricht, Maastricht, the Netherlands) for critical reading of the manuscript.
References
- 1.Hanauer SB. Inflammatory bowel disease: epidemiology, pathogenesis, and therapeutic opportunities. Inflamm Bowel Dis. 2006;12:S3–9. doi: 10.1097/01.mib.0000195385.19268.68. [DOI] [PubMed] [Google Scholar]
- 2.Rogler G, Andus T. Cytokines in inflammatory bowel disease. World J Surg. 1998;22:382–9. doi: 10.1007/s002689900401. [DOI] [PubMed] [Google Scholar]
- 3.Danese S, Gasbarrini A. Chemokines in inflammatory bowel disease. J Clin Pathol. 2005;58:1025–7. doi: 10.1136/jcp.2005.030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elson CO, Sartor RB, Tennyson GS, Riddell RH. Experimental models of inflammatory bowel disease. Gastroenterology. 1995;109:1344–67. doi: 10.1016/0016-5085(95)90599-5. [DOI] [PubMed] [Google Scholar]
- 5.Byrne FR, Viney JL. Mouse models of inflammatory bowel disease. Curr Opin Drug Discov Devel. 2006;9:207–17. [PubMed] [Google Scholar]
- 6.Egger B, Bajaj-Elliott M, MacDonald TT, Inglin R, Eysselein VE, Buchler MW. Characterisation of acute murine dextran sodium sulphate colitis: cytokine profile and dose dependency. Digestion. 2000;62:240–8. doi: 10.1159/000007822. [DOI] [PubMed] [Google Scholar]
- 7.Melgar S, Karlsson A, Michaelsson E. Acute colitis induced by dextran sulfate sodium progresses to chronicity in C57BL/6 but not in BALB/c mice: correlation between symptoms and inflammation. Am J Physiol Gastrointest Liver Physiol. 2005;288:G1328–38. doi: 10.1152/ajpgi.00467.2004. Epub 6 January 6 2005. [DOI] [PubMed] [Google Scholar]
- 8.Farrar MA, Schreiber RD. The molecular cell biology of interferon-gamma and its receptor. Annu Rev Immunol. 1993;11:571–611. doi: 10.1146/annurev.iy.11.040193.003035. [DOI] [PubMed] [Google Scholar]
- 9.Skurkovich B, Skurkovich S. Anti-interferon-gamma antibodies in the treatment of autoimmune diseases. Curr Opin Mol Ther. 2003;5:52–7. [PubMed] [Google Scholar]
- 10.Sasaki T, Hiwatashi N, Yamazaki H, Noguchi M, Toyota T. The role of interferon gamma in the pathogenesis of Crohn's disease. Gastroenterol Jpn. 1992;27:29–36. [PubMed] [Google Scholar]
- 11.Fais S, Capobianchi MR, Pallone F, et al. Spontaneous release of interferon gamma by intestinal lamina propria lymphocytes in Crohn's disease. Kinetics of in vitro response to interferon gamma inducers. Gut. 1991;32:403–7. doi: 10.1136/gut.32.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fais S, Capobianchi MR, Silvestri M, Mercuri F, Pallone F, Dianzani F. Interferon expression in Crohn's disease patients: increased interferon-gamma and -alpha mRNA in the intestinal lamina propria mononuclear cells. J Interferon Res. 1994;14:235–8. doi: 10.1089/jir.1994.14.235. [DOI] [PubMed] [Google Scholar]
- 13.Noguchi M, Hiwatashi N, Liu Z, Toyota T. Enhanced interferon-gamma production and B7-2 expression in isolated intestinal mononuclear cells from patients with Crohn's disease. J Gastroenterology. 1995;30:52–5. [PubMed] [Google Scholar]
- 14.Farber JM. Mig and IP-10: CXC chemokines that target lymphocytes. J Leukoc Biol. 1997;61:246–57. [PubMed] [Google Scholar]
- 15.Obermeier F, Kojouharoff G, Hans W, Scholmerich J, Gross V, Falk W. Interferon-gamma (IFN-gamma) and tumour necrosis factor (TNF)-induced nitric oxide as toxic effector molecule in chronic dextran sulphate sodium (DSS)-induced colitis in mice. Clin Exp Immunol. 1999;116:238–45. doi: 10.1046/j.1365-2249.1999.00878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powrie F, Leach MW, Mauze S, Menon S, Caddle LB, Coffman RL. Inhibition of Th1 responses prevents inflammatory bowel disease in scid mice reconstituted with CD45RBhi CD4+ T cells. Immunity. 1994;1:553–62. doi: 10.1016/1074-7613(94)90045-0. [DOI] [PubMed] [Google Scholar]
- 17.Lieberman BY, Fiocchi C, Youngman KR, Sapatnekar WK, Proffitt MR. Interferon gamma production by human intestinal mucosal mononuclear cells. Decreased levels in inflammatory bowel disease. Dig Dis Sci. 1988;33:1297–304. doi: 10.1007/BF01536683. [DOI] [PubMed] [Google Scholar]
- 18.Breese E, Braegger CP, Corrigan CJ, Walker-Smith JA, MacDonald TT. Interleukin-2- and interferon-gamma-secreting T cells in normal and diseased human intestinal mucosa. Immunology. 1993;78:127–31. [PMC free article] [PubMed] [Google Scholar]
- 19.Melgar S, Yeung MM, Bas A, et al. Over-expression of interleukin 10 in mucosal T cells of patients with active ulcerative colitis. Clin Exp Immunol. 2003;134:127–37. doi: 10.1046/j.1365-2249.2003.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakamura M, Saito H, Kasanuki J, Tamura Y, Yoshida S. Cytokine production in patients with inflammatory bowel disease. Gut. 1992;33:933–7. doi: 10.1136/gut.33.7.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elsasser-Beile U, von Kleist S, Gerlach S, Gallati H, Monting JS. Cytokine production in whole blood cell cultures of patients with Crohn's disease and ulcerative colitis. J Clin Lab Anal. 1994;8:447–51. doi: 10.1002/jcla.1860080618. [DOI] [PubMed] [Google Scholar]
- 22.Van Damme N, De Keyser F, Demetter P, et al. The proportion of Th1 cells, which prevail in gut mucosa, is decreased in inflammatory bowel syndrome. Clin Exp Immunol. 2001;125:383–90. doi: 10.1046/j.1365-2249.2001.01638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hans W, Scholmerich J, Gross V, Falk W. Interleukin-12 induced interferon-gamma increases inflammation in acute dextran sulfate sodium induced colitis in mice. Eur Cytokine Netw. 2000;11:67–74. [PubMed] [Google Scholar]
- 24.Camoglio L, te Velde AA, de Boer A, ten Kate FJ, Kopf M, van Deventer SJ. Hapten-induced colitis associated with maintained Th1 and inflammatory responses in IFN-gamma receptor-deficient mice. Eur J Immunol. 2000;30:1486–95. doi: 10.1002/(SICI)1521-4141(200005)30:5<1486::AID-IMMU1486>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 25.Tozawa K, Hanai H, Sugimoto K, et al. Evidence for the critical role of interleukin-12 but not interferon-gamma in the pathogenesis of experimental colitis in mice. J Gastroenterol Hepatol. 2003;18:578–87. doi: 10.1046/j.1440-1746.2003.03024.x. [DOI] [PubMed] [Google Scholar]
- 26.Tagawa Y, Sekikawa K, Iwakura Y. Suppression of concanavalin A-induced hepatitis in IFN-gamma(-/-) mice, but not in TNF-alpha(-/-) mice: role for IFN-gamma in activating apoptosis of hepatocytes. J Immunol. 1997;159:1418–28. [PubMed] [Google Scholar]
- 27.Axelsson LG, Landstrom E, Bylund-Fellenius AC. Experimental colitis induced by dextran sulphate sodium in mice: beneficial effects of sulphasalazine and olsalazine. Aliment Pharmacol Ther. 1998;12:925–34. doi: 10.1046/j.1365-2036.1998.00357.x. [DOI] [PubMed] [Google Scholar]
- 28.Cooper HS, Murthy SN, Shah RS, Sedergran DJ. Clinicopathologic study of dextran sulfate sodium experimental murine colitis. Laboratory Invest. 1993;69:238–49. [PubMed] [Google Scholar]
- 29.Naito Y, Takagi T, Kuroda M, et al. An orally active matrix metalloproteinase inhibitor, ONO-4817, reduces dextran sulfate sodium-induced colitis in mice. Inflamm Res. 2004;53:462–8. doi: 10.1007/s00011-004-1281-1. [DOI] [PubMed] [Google Scholar]
- 30.MacDermott RP, Sanderson IR, Reinecker HC. The central role of chemokines (chemotactic cytokines) in the immunopathogenesis of ulcerative colitis and Crohn's disease. Inflamm Bowel Dis. 1998;4:54–67. doi: 10.1097/00054725-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Uguccioni M, Gionchetti P, Robbiani DF, et al. Increased expression of IP-10, IL-8, MCP-1, and MCP-3 in ulcerative colitis. Am J Pathol. 1999;155:331–6. doi: 10.1016/S0002-9440(10)65128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reinecker HC, Loh EY, Ringler DJ, Mehta A, Rombeau JL, MacDermott RP. Monocyte-chemoattractant protein 1 gene expression in intestinal epithelial cells and inflammatory bowel disease mucosa. Gastroenterology. 1995;108:40–50. doi: 10.1016/0016-5085(95)90006-3. [DOI] [PubMed] [Google Scholar]
- 33.Mazzucchelli L, Hauser C, Zgraggen K, et al. Differential in situ expression of the genes encoding the chemokines MCP-1 and RANTES in human inflammatory bowel disease. J Pathol. 1996;178:201–6. doi: 10.1002/(SICI)1096-9896(199602)178:2<201::AID-PATH440>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 34.Okayasu I, Hatakeyama S, Yamada M, Ohkusa T, Inagaki Y, Nakaya R. A novel method in the induction of reliable experimental acute and chronic ulcerative colitis in mice. Gastroenterology. 1990;98:694–702. doi: 10.1016/0016-5085(90)90290-h. [DOI] [PubMed] [Google Scholar]
- 35.Dieleman LA, Ridwan BU, Tennyson GS, Beagley KW, Bucy RP, Elson CO. Dextran sulfate sodium-induced colitis occurs in severe combined immunodeficient mice. Gastroenterology. 1994;107:1643–52. doi: 10.1016/0016-5085(94)90803-6. [DOI] [PubMed] [Google Scholar]
- 36.Mashimo H, Wu DC, Podolsky DK, Fishman MC. Impaired defense of intestinal mucosa in mice lacking intestinal trefoil factor. Science. 1996;274:262–5. doi: 10.1126/science.274.5285.262. [DOI] [PubMed] [Google Scholar]
- 37.Ni J, Chen SF, Hollander D. Effects of dextran sulphate sodium on intestinal epithelial cells and intestinal lymphocytes. Gut. 1996;39:234–41. doi: 10.1136/gut.39.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kitajima S, Takuma S, Morimoto M. Changes in colonic mucosal permeability in mouse colitis induced with dextran sulfate sodium. Exp Anim. 1999;48:137–43. doi: 10.1538/expanim.48.137. [DOI] [PubMed] [Google Scholar]
- 39.Ohkusa T, Okayasu I, Tokoi S, Araki A, Ozaki Y. Changes in bacterial phagocytosis of macrophages in experimental ulcerative colitis. Digestion. 1995;56:159–64. doi: 10.1159/000201236. [DOI] [PubMed] [Google Scholar]
- 40.Dieleman LA, Palmen MJ, Akol H, et al. Chronic experimental colitis induced by dextran sulphate sodium (DSS) is characterized by Th1 and Th2 cytokines. Clin Exp Immunol. 1998;114:385–91. doi: 10.1046/j.1365-2249.1998.00728.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Madara JL, Stafford J. Interferon-gamma directly affects barrier function of cultured intestinal epithelial monolayers. J Clin Invest. 1989;83:724–7. doi: 10.1172/JCI113938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiba H, Kojima T, Osanai M, Sawada N. The significance of interferon-gamma-triggered internalization of tight-junction proteins in inflammatory bowel disease. Sci STKE. 2006;2006:pe1. doi: 10.1126/stke.3162006pe1. [DOI] [PubMed] [Google Scholar]
- 43.Tsuji H, Mukaida N, Harada A, et al. Alleviation of lipopolysaccharide-induced acute liver injury in Propionibacterium acnes-primed IFN-gamma-deficient mice by a concomitant reduction of TNF-alpha, IL-12, and IL-18 production. J Immunol. 1999;162:1049–55. [PubMed] [Google Scholar]
- 44.Ishida Y, Kondo T, Ohshima T, Fujiwara H, Iwakura Y, Mukaida N. A pivotal involvement of IFN-gamma in the pathogenesis of acetaminophen-induced acute liver injury. FASEB J. 2002;16:1227–36. doi: 10.1096/fj.02-0046com. [DOI] [PubMed] [Google Scholar]
- 45.Ishida Y, Maegawa T, Kondo T, et al. Essential involvement of IFN-gamma in Clostridium difficile toxin A-induced enteritis. J Immunol. 2004;172:3018–25. doi: 10.4049/jimmunol.172.5.3018. [DOI] [PubMed] [Google Scholar]
- 46.Rollins BJ. Chemokines. Blood. 1997;90:909–28. [PubMed] [Google Scholar]
- 47.Baggiolini M. Chemokines and leukocyte traffic. Nature. 1998;392:565–8. doi: 10.1038/33340. [DOI] [PubMed] [Google Scholar]
- 48.Gottlieb AB, Luster AD, Posnett DN, Carter DM. Detection of a gamma interferon-induced protein IP-10 in psoriatic plaques. J Exp Med. 1988;168:941–8. doi: 10.1084/jem.168.3.941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flier J, Boorsma DM, van Beek PJ, et al. Differential expression of CXCR3 targeting chemokines CXCL10, CXCL9, and CXCL11 in different types of skin inflammation. J Pathol. 2001;194:398–405. doi: 10.1002/1096-9896(200108)194:4<397::aid-path899>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 50.Sorensen TL, Tani M, Jensen J, et al. Expression of specific chemokines and chemokine receptors in the central nervous system of multiple sclerosis patients. J Clin Invest. 1999;103:807–15. doi: 10.1172/JCI5150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Balashov KE, Rottman JB, Weiner HL, Hancock WW. CCR5(+) and CXCR3(+) T cells are increased in multiple sclerosis and their ligands MIP-1alpha and IP-10 are expressed in demyelinating brain lesions. Proc Natl Acad Sci USA. 1999;96:6873–8. doi: 10.1073/pnas.96.12.6873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patel DD, Zachariah JP, Whichard LP. CXCR3 and CCR5 ligands in rheumatoid arthritis synovium. Clin Immunol. 2001;98:39–45. doi: 10.1006/clim.2000.4957. [DOI] [PubMed] [Google Scholar]
- 53.Agostini C, Cassatella M, Zambello R, et al. Involvement of the IP-10 chemokine in sarcoid granulomatous reactions. J Immunol. 1998;161:6413–20. [PubMed] [Google Scholar]
- 54.Melter M, Exeni A, Reinders ME, et al. Expression of the chemokine receptor CXCR3 and its ligand IP-10 during human cardiac allograft rejection. Circulation. 2001;104:2558–64. doi: 10.1161/hc4601.098010. [DOI] [PubMed] [Google Scholar]
- 55.Agostini C, Calabrese F, Rea F, et al. Cxcr3 and its ligand CXCL10 are expressed by inflammatory cells infiltrating lung allografts and mediate chemotaxis of T cells at sites of rejection. Am J Pathol. 2001;158:1703–11. doi: 10.1016/S0002-9440(10)64126-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Romagnani P, Lazzeri E, Lasagni L, et al. IP-10 and Mig production by glomerular cells in human proliferative glomerulonephritis and regulation by nitric oxide. J Am Soc Nephrol. 2002;13:53–64. doi: 10.1681/ASN.V13153. [DOI] [PubMed] [Google Scholar]
- 57.Scheerens H, Hessel E, de Waal-Malefyt R, Leach MW, Rennick D. Characterization of chemokines and chemokine receptors in two murine models of inflammatory bowel disease: IL-10-/- mice and Rag-2-/- mice reconstituted with CD4+CD45RBhigh T cells. Eur J Immunol. 2001;31:1465–74. doi: 10.1002/1521-4141(200105)31:5<1465::AID-IMMU1465>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 58.Villiger PM, Terkeltaub R, Lotz M. Production of monocyte chemoattractant protein-1 by inflamed synovial tissue and cultured synoviocytes. J Immunol. 1992;149:722–7. [PubMed] [Google Scholar]
- 59.Gillitzer R, Wolff K, Tong D, et al. MCP-1 mRNA expression in basal keratinocytes of psoriatic lesions. J Invest Dermatol. 1993;101:127–31. doi: 10.1111/1523-1747.ep12363613. [DOI] [PubMed] [Google Scholar]
- 60.Czaja MJ, Geerts A, Xu J, Schmiedeberg P, Ju Y. Monocyte chemoattractant protein 1 (MCP-1) expression occurs in toxic rat liver injury and human liver disease. J Leukoc Biol. 1994;55:120–6. doi: 10.1002/jlb.55.1.120. [DOI] [PubMed] [Google Scholar]
- 61.Nadeau KC, Azuma H, Tilney NL. Sequential cytokine dynamics in chronic rejection of rat renal allografts: roles for cytokinesRANTES and MCP-1. Proc Natl Acad Sci USA. 1995;92:8729–33. doi: 10.1073/pnas.92.19.8729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grimm MC, Elsbury SK, Pavli P, Doe WF. Enhanced expression and production of monocyte chemoattractant protein-1 in inflammatory bowel disease mucosa. J Leukoc Biol. 1996;59:804–12. doi: 10.1002/jlb.59.6.804. [DOI] [PubMed] [Google Scholar]
- 63.Dwinell MB, Lugering N, Eckmann L, Kagnoff MF. Regulated production of interferon-inducible T-cell chemoattractants by human intestinal epithelial cells. Gastroenterology. 2001;120:49–59. doi: 10.1053/gast.2001.20914. [DOI] [PubMed] [Google Scholar]
- 64.Warhurst AC, Hopkins SJ, Warhurst G. Interferon gamma induces differential upregulation of alpha and beta chemokine secretion in colonic epithelial cell lines. Gut. 1998;42:208–13. doi: 10.1136/gut.42.2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]