Abstract
Objective
The objective of this study was to investigate the effects of a structured 6-week neuropsychological course on the executive functioning of older adults with cognitive complaints.
Methods
A randomised controlled design was used involving 69 community dwelling individuals aged 55 years and older. Both objective and subjective measures were included to assess executive functioning. General linear model with repeated measures analysis of variance was used to examine the intervention effects.
Results
After the intervention, the participants in the intervention group were significantly less annoyed by their cognitive failures, were better able to manage their executive failures and reported less anxiety symptoms than those in the waiting list control group.
Conclusion
These findings indicate that a combination of psycho-education and training has the potential to change the attitude of older individuals towards their cognitive functioning.
Practice implications
Because this training focussed on cognitive functions that are among the first to decline in older adults and the subjective evaluation of the people after training was quite favourable, the proposed intervention may be considered a valuable contribution to cognitive interventions for older adults.
Keywords: Aging, Cognitive functioning, Executive functioning, Training, Psycho-education
1. Introduction
Most cognitive functions decline with age. Working memory functions less well [1], inhibitory mechanisms become less efficient [2,3], and performance in dual task situations is reduced [4]. Working memory, inhibition, and shifting between two tasks are frequently seen as aspects of executive functioning [5]. This is important because executive functioning is a basic condition for everyday functioning of older adults and poor executive functioning may be a threat to independent living and successful aging [6–8]. For example, older people may experience difficulties in planning their leisure time activities, managing their finances, coping with novel situations, or learning to deal with new strategies and procedures, such as using computers, Internet services, cellular phones and other electronic devices. All these activities require that the proper goal is selected and maintained in memory while the task is executed. In addition, when performing such complex tasks, it is important to be able to divide a task into simpler tasks and to set priorities for the execution of subordinate goals [9,10]. Although many older adults experience difficulties with planning activities, the effect of behavioural interventions to improve these cognitive functions in older adults has not been a focus of much research. Most interventions for older individuals directed at improving cognitive functioning, also called neuropsychological interventions, focus on memory functioning and recently also memory self-efficacy [11,12]. It is therefore a challenging opportunity to examine whether older individuals benefit from an intervention directed at executive functions, notably organization and planning of activities in daily life.
The intervention protocol of goal management training (GMT) [13], was originally developed to teach patients with brain injury a strategy to improve their ability to plan activities and to structure intentions. The GMT was based on the theoretical framework of disorganization of behaviour [9,14]. This theory states that any line of activity requires a list of goals or task requirements that are used to create a structure of actions or mental operations by which these goals are achieved. In performing a task, the current state of affairs and the goal state are compared, and appropriate actions or mental operations are selected in order to reduce any mismatch. This process continues until there is no mismatch between the current state and the goal state. Given that the number of actions that can actually be performed at any one time is limited, it is important to inhibit irrelevant actions that will not contribute to a particular goal. The GMT contains several stages that are based on this notion. First, participants have to be aware of the current state of affairs (‘‘stop’’). Then the appropriate goals have to be selected (‘‘what do I have to do?’’), and if needed goals have to be partitioned into subordinate goals (‘‘split’’). In the final stage (‘‘checking’’), the outcome of the selected actions is compared with the goals to be achieved.
The GMT has been evaluated in 30 patients with mild to severe brain injury, who were randomly assigned to groups who received GMT or motor skill training. Participants who followed the GMT showed significant gains on everyday paper-and-pencil tasks designed to mimic tasks that are problematic for patients with problems in executive functioning [15]. The problems and topics used in the original GMT are also applicable to older adults without clear cut brain dysfunction or psychopathology, because older adults show reduced performance on executive functioning tasks, which may impact their daily life functioning. We developed a dedicated structured course based on the GMT for use in older adults. The adapted course consists of 12 sessions (two sessions per week). Apart from the original GMT, psycho-education was added to the adapted intervention in order to provide information to the participant about cognitive functioning in general and the mechanism behind failures in daily life in particular. The adapted intervention was tested according to a randomised waiting list control design [16–18]. The success of this intervention was evaluated in terms of its effectiveness in (1) reducing complaints and cognitive failures, (2) reducing mood related complaints and (3) in improving objective cognitive functioning. The effectiveness of the intervention was evaluated on cognitive complaints and failures, because the focus of the intervention is on real life activities that emphasize complaints and problems experienced by the participants. Furthermore, there is much evidence available that subjective evaluation of cognitive functioning does not always predict objective test performance [19–21]. Therefore, we evaluated the effectiveness of the intervention both on self-reported problems and cognitive test performance. It is important to investigate anxiety symptoms and mood, because these emotional states may influence or be influenced by cognitive complaints and subjective attitudes toward cognitive functioning. This is in line with a controlled intervention study that indicated that an experimental neuropsychological intervention program significantly reduced mood-related complaints [22]. During the course, participants practised activities encountered in real life with emphasis on the complaints and problems experienced by the participants. We therefore expected that the training would have most impact on complaints and cognitive failures participants experienced.
2. Methods
2.1. Participants
The participants were recruited through media advertisements asking for people aged 55 years and older with complaints about their cognitive functioning to participate in the study. In the advertisements, several examples of cognitive complaints were mentioned, such as distraction (‘have you repeatedly experienced that you forget something that you are doing, because you were distracted by a telephone call?’), difficulty with dual tasking (‘have you experienced repeatedly that something went wrong while doing more than one activity in a time?’), and planning problems (‘do you have difficulties with planning a party or holiday trip’). Participants were enrolled if they had a score of 24 or more on the mini-mental state examination (MMSE) [11,23], had a good comprehension of the Dutch language, were able to travel independently to the research centre, and had not previously participated in a neuropsychological research programme. People with documented evidence of neurological diseases of the central nervous system (e.g. dementia or Parkinson’s disease) or a major psychiatric disorder were excluded. The local medical ethics committee approved the study and all participants gave their informed consent.
2.2. Goal management course
The goal management training (GMT) was originally developed in Ireland/Canada for brain-injured patients [13,15]. The aim of this structured and interactive intervention is to teach individuals a strategy to improve planning activities and to structure intentions. We translated the training manual into Dutch and adapted the content to make it applicable to healthy older people with problems in executive functioning. One major addition to the GMT was the introduction of ‘psycho-education’ to explain the various cognitive functions and their role in normal behaviour and in problems in daily life. The programme was also adapted to consist of 12 sessions, one individual session and 11 group sessions. The content of each session and the order in which topics were addressed were laid down in a protocol. The group sessions involved two trainers, a healthcare psychologist with extensive experience in interventions for people with cognitive problems and a research psychologist. Each training group consisted of seven participants or less, to ensure sufficient individual attention during the sessions. The groups were homogeneous with respect to sex, since the complaints reported by women and men apply to different situations and topics (e.g. shopping versus technical maintenance). There were 10 female and 2 male groups. Each session lasted 1–1.5 h and was held in a room at the University. There were two sessions a week, for 6 consecutive weeks. All sessions were structured: homework and last week’s topics were discussed first, and each participant had to report at least one failure and one success in daily life (25–35 min). Emotional experiences accompanying the failures or successes were addressed in each session. Next, information about a new stage of the strategy was introduced or a stage that was discussed in a previous session was extended (25–35 min). At the end of each session, participants received homework exercises and handouts containing a summary of the session (10 min). All topics were illustrated with practical examples or exercises.
The goals for the first two sessions were to get acquainted with the trainer and the rest of the group and with the purpose of the course, to discuss the expectations of the training, and to increase insight into the complaints about executive functioning, for example by discussing examples of complaints. In the third and fourth sessions, high-risk situations were identified, the stop strategy was introduced using an automatic pilot metaphor and a personal catchphrase was chosen (e.g. ‘just a second’ or ‘wait a minute’). The stop strategy was extended in session 5 by means of a relaxation technique and a discussion of cognitive information processing and working memory. In the individual session, personal problems and expectations about the course were discussed, additional questions about the training were answered, and the interaction with the other course participants was discussed. Sessions 7 and 8 focused on stating a goal. Furthermore, inhibition of relevant goals and conflicting goal scenarios were important topics in these sessions. Sessions 9 and 10 were used to discuss splitting a complex task into smaller goals and then to prioritise these subgoals. The topic of session 11 was the mechanism of checking ongoing goals and activities. Finally, in the last session an overview was given.
2.3. Procedure
A dual baseline and two follow-up assessments were used in this randomised controlled trial. Before the first measurement, all participants were screened for executive complaints and problems by means of a structured interview. Demographic variables, MMSE score, complaints about cognitive functioning, and information from significant others were obtained. Furthermore, participants were asked to evaluate their ability to prepare and plan several activities, such as planning a party, preparing a vacation and operating a mobile phone. Participants were excluded when they were characterized by any of the following: the presence of isolated memory problems without executive problems, the absence of any objective cognitive complaint or problems, the presence of pathological cognitive problems (dementia or related conditions as assessed by neuropsychological assessment) and the presence of cognitive complaints or performance deficits in other cognitive domains (e.g. mild cognitive impairment) [35,36]. Based on this structured clinical interview, persons were selected who experienced executive problems. Inclusion of patients was based upon presence of complaints or behavioural problems in the domain of executive functioning. In most cases the clinical interview provided sufficient information in order to determine whether participants had executive complaints or not. These participants were characterised by chaotic or behaviour characterised by a high level of distractibility, concentration problems and/or difficulty to perform activities according to a plan. If it remained unclear whether a person had executive complaints or problems, the case was discussed extensively in a team coordinated by an experienced clinical neuropsychologist (RP).
After screening and before the baseline measurements, participants were randomly assigned to the intervention group or waiting list control group. The method of randomisation was a block design with block size 2, with stratification for age and sex. The investigator who was responsible for randomisation was not involved in the training procedures. All participants were informed about this randomisation procedure and were told that if they were assigned to the waiting list control group, they would have the opportunity to follow the training after the study closure. The individuals in the control group did not receive an intervention or training during the study (waiting period). At the last measurement, participants in the control group were asked whether they had, on their own initiative, followed a course to improve their cognitive functioning: none of them had. All participants (training group and control group) were tested twice, before the intervention group received the intervention. This ‘dual baseline procedure’ was used in order to reduce practice and procedure-learning effects [37]. The mean interval between measurements 1 and 2 was 17 days (S.D. = 5.8). Both the control group and the intervention group were tested immediately after the intervention group had completed the intervention, which was 8 weeks after measurement 2. The fourth measurement (long-term effect) took place 7 weeks later. All statistical analyses were performed using data from the second baseline assessment and the two subsequent follow-up measurements.
2.4. Outcome measures
2.4.1. Subjective executive functioning
The cognitive failure questionnaire (CFQ) was used to evaluate subjective executive functioning. This instrument consists of 25 items measuring the frequency of everyday cognitive ‘failures’ in the area of memory, attention, perception and action [24–26]. Participants were asked to indicate on a five-point scale how often they usually experienced each particular cognitive failure (never, very rarely, occasionally, quite often and very often). A higher score on the CFQ indicates more cognitive failures. The CFQ has been validated in Dutch [24].
Perceived degree of hindrance, worry, and annoyance about subjective executive functioning were scored with the questionnaire used in the Maastricht aging study, a longitudinal study on normal cognitive aging [27]. This questionnaire contained four questions focusing on the perceived degree of hindrance, worry, and annoyance about these failures. Each question has five possible answers ranging from ‘not at all’ to ‘a lot’.
Management of reported executive failures was evaluated using the following instrument. On the basis of information from the screening interviews, 10 complaints were selected that were reported most often by the included participants (e.g. doing more than one activity at a time, performing activities according to a plan, estimating the time needed for an activity). The included participants scored each item on a scale ranging from 1 (‘cannot manage this at all’) to 10 (‘have no problems at all’). The 10 values were summed to compute a total score, ranging from 10 to 100. Cronbach’s alpha for this 10-item instrument was 0.68, based on data taken from the baseline measurements.
2.4.2. Mood
Symptoms of depression and anxiety were determined by the subscales depression and anxiety of the SymptomCheck-List 90 (SCL-90). The SCL-90 is a widely used multidimensional checklist for psychopathological complaints [28,29]. Scores range from 0 (good) to 80 (poor) for depression, and from 0 (good) to 50 (poor) for anxiety.
2.4.3. Objective test performance
The stroop colour word test (SCWT) involves three cards displaying forty stimuli each [30,31]. The first card contains colour words printed in black ink, which have to be read. The second card contains coloured patches, which have to be named. The third card displays colour names printed in incongruously coloured ink. Individuals are instructed to name the ink colour of the printed words. By subtracting the time needed for the last part from the mean score of the first and second parts, an interference score can be calculated, which was used as an outcome measure. This interference score can be regarded as a measure of inhibition of a habitual response, which depends on adequate levels of executive functioning [32].
2.5. Other measures
Four subtasks of the Groningen intelligence test (GIT) were used to make a reliable estimation of IQ [33]. The four subtasks involved were—(1) arithmetic: the correct completion of as many addition sums as possible in 1 min, (2) vocabulary: indicating which of five alternative words is synonymous with a given word, (3) visuoconstruction: indicating which two-dimensional shapes from a larger set are needed to exactly fill up a given space and (4) verbal reasoning: indicating which of five alternatives is related in the same way to a given word as two words in an example.
Level of education was indexed on an 8-point ordinal scale—1: primary education, 2: lower vocational education, 3: intermediate general secondary education, 4: intermediate vocational education, 5: higher general secondary education/university preparatory education, 6: higher vocational preparatory education, 7: higher professional education and 8: university education [34].
The mini-mental state examination (MMSE; [23]) was used as a screening instrument for dementia and consists of the scales orientation, registration, recall, attention, language and construction. A maximum score of 30 can be obtained.
2.6. Statistical analyses
First, we examined whether this study population indeed experienced more cognitive failures (CFQ total score and additional questions) and had a lower score on the interference measure of the SCWT than a general population. Using Student’s t-tests, we compared the baseline performance on these outcome measure of the participants in this study with that of age-, sex- and education-matched healthy community-dwelling individuals who participated in the Maastricht aging study, a large-scale longitudinal population study examining determinants of cognitive aging. These participants were randomly recruited from a patient register of collaborating general practices in the south of The Netherlands (for more details see [27]).
Although the participants were randomly assigned to the two groups, possible differences could exist between the study groups by chance. Therefore, differences in demographic characteristics (age and education), intelligence, and MMSE score between the two groups were examined using Student’s t-tests. A χ2-test was used to analyse group differences with respect to sex and marital status (married/cohabiting versus others). General linear model (GLM) with repeated measures analysis of variance was used to examine the effects of the intervention. Analyses were performed with group (two levels: intervention group and control group) as between subject variable and time (two levels: first follow-up and second follow-up) as the within subject factor. Baseline scores at measurement 2 were treated as covariates in this model to control for baseline group differences. Consistent with the rules for clinical trials, all analyses were based on the groups as randomised, according to the principle of ‘intention-to-treat’, i.e. all participants were analysed in the groups to which they were originally randomised, regardless of whether they had received or adhered to the allocated intervention [38]. Randomisation took place after the first baseline measurement. Analyses were performed using the SPSS for Macintosh Program Series, Version 10 (SPSS-Inc., Chicago), with p = 0.05 as significance level.
3. Results
3.1. Recruitment of participants
Two hundred and six people aged 55–82 were screened for participation. Of these 101 were excluded: 82 had no executive problems or complaints, 18 had already participated in a neuropsychological research program and 1 had limited mobility. Thirty-six adults refused to participate after reading the informed consent or after the screening procedure due to insufficient motivation or interest. Sixty-nine participants were randomised to the intervention or control group. The intervention group started with 38 persons, of whom 35 received the training and 3 persons decided after randomisation not to start with the intervention, but who stayed in the study and provided follow-up data. Main reasons for not starting in the course were health-related problems or being too busy with other activities or work. After the dual baseline, 1 person in the intervention group dropped out because of illness. The control group consisted of 31 participants. One person of the control group refused to participate after the dual baseline measurement, because of a lack of interest. Thus, data for 37 people in the intervention group and 30 people in the control group were analysed. Results of recruitment and randomisation are given in Fig. 1. Post hoc power analysis on the available number of participants using a critical effect size of 0.15 and an α level of 0.05 resulted in a power of 0.88 for this study [39].
Fig. 1.
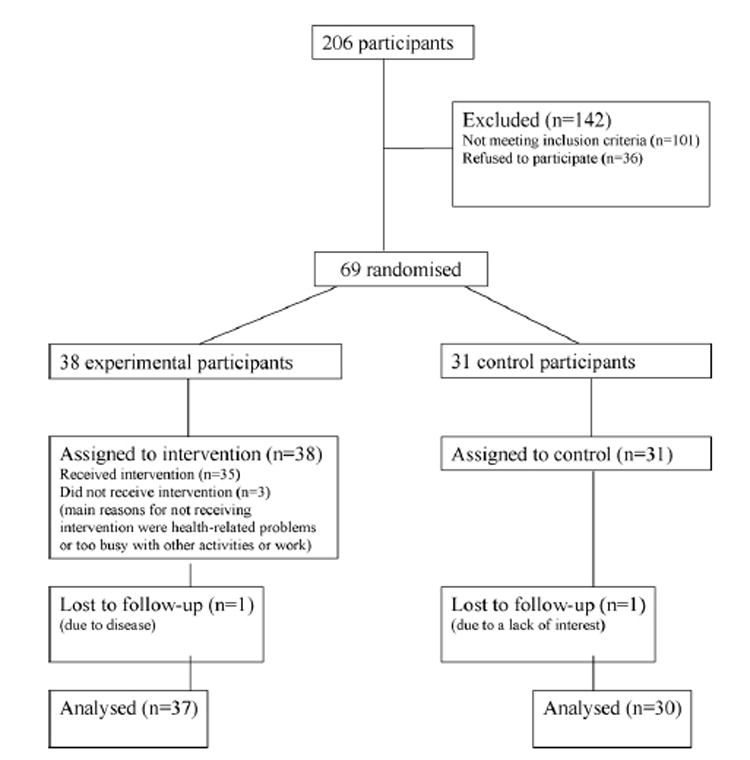
Flowchart of the participants.
3.2. Comparison with participants from the Maastricht aging study
After matching for age (two groups), sex and education (two groups), the study participants reported more cognitive failures on the CFQ total score (t(1, 134) = 7.23, p < 0.01), more hindrance (t(1, 134) = 7.66, p < 0.01), more worry (t(1, 134) = 5.98, p < 0.01), and more annoyance (t(1, 134) = 5.13, p < 0.01) about these failures than did participants enrolled in the Maastricht aging study. In addition, they reported more anxiety symptomatology (t(1, 133) = 2.41, p < 0.02) and had worse scores on the interference score of the stroop colour word test (t(1, 132) = 3.63, p < 0.01).
3.3. Baseline characteristics
Demographic characteristics and mean MMSE and IQ scores are summarised in Table 1. The intervention group and the control group did not differ on age (t(1, 67) = −0.65, p = 0.52), sex (χ2 = 0.06, p = 0.81), educational level (t(1, 67) = −0.43, p = 0.67), marital status (χ2 = 0.01, p = 0.94) or MMSE score (t(1, 67) = −1.27, p = 0.21). The IQ scores of the intervention group were slightly, but significantly, lower than those of the control group (t(1, 67) = −1.99, p = 0.05).
Table 1.
Demographic characteristics of the participants in the study
| Experimental (N = 37) | Control (N = 30) | p-Value | |
|---|---|---|---|
| Age | 62.35 (5.39) | 63.27 (5.95) | 0.52 |
| Sex (%women) | 82% | 83% | 0.81 |
| Education (1–8) | 3.57 (1.76) | 3.77 (2.01) | 0.67 |
| Marital status (%living together/married) | 68% | 67% | 0.94 |
| IQ | 113.70 (12.70) | 119.43 (10.32) | 0.05 |
| MMSE (0–30) | 28.49 (1.30) | 28.90 (1.35) | 0.21 |
Note: Student’s t-tests were used for age, education, intelligence and MMSE-score. Sex and marital status were analysed using χ2-test. MMSE: mini-mental state examination.
3.4. Effects of the goal management training
The intervention group experienced less annoyance after the training than did the control group (F(1, 62) = 5.94, p = 0.02, η2 = 0.09, see Table 2). Interaction effects between group and time were not significant (F(1, 62) = 0.05, p = 0.82), indicating that the intervention effect was already present immediately after the intervention and did not change after 7 weeks follow-up. Furthermore, participants in the intervention group were better able to manage executive failures after training (F(1, 63) = 4.28, p = 0.04, η2 = 0.06). The interaction effect between group and time was not significant (F(1, 63) = 0.84, p = 0.36); thus there was no difference between the first follow-up measurement and the second follow-up measurement. The total score on the CFQ, and the additional questions concerning hindrance and worries about cognitive failures did not significantly improve after participants followed the training compared to control participants. The interaction effect between group and time of anxiety was significant, indicating that the effect of the intervention on anxiety symptoms was not present immediately after the intervention, but the level of anxiety symptomatology changed after the intervention (F(1, 61) = 5.51, p = 0.02, η2 = 0.08). The anxiety symptoms of the intervention group reduced, while the waiting list control group reported more anxiety symptoms (see Fig. 2). The intervention had no effect on the interference score of the SCWT (see Table 2).
Table 2.
Adjusted means, standard error of the mean (S.E.M.) and results of tests for group differences of the subjective measures, mood and objective test performance
| Short-term post-intervention, mean (S.E.M.) | Long-term post-intervention, mean (S.E.M.) | Main effect, p-value | Interaction effecta, p-value | |
|---|---|---|---|---|
| Subjective measures | ||||
| CFQ total score | ||||
| Experimental | 40.29 (1.43) | 40.83 (1.40) | 0.208 | 0.981 |
| Control | 42.81 (1.60) | 43.38 (1.56) | ||
| CFQ hindrance | ||||
| Experimental | 2.84 (0.10) | 2.76 (0.11) | 0.298 | 0.551 |
| Control | 2.93 (0.11) | 2.95 (0.12) | ||
| CFQ worries | ||||
| Experimental | 2.67 (0.11) | 2.62 (0.11) | 0.192 | 0.108 |
| Control | 2.99 (0.12) | 2.65 (0.12) | ||
| CFQ annoyance | ||||
| Experimental | 2.37 (0.14) | 2.49 (0.15) | 0.018 | 0.821 |
| Control | 2.81 (0.15) | 2.98 (0.17) | ||
| Executive complaintsb | ||||
| Experimental | 63.35 (0.91) | 62.21 (0.93) | 0.043 | 0.363 |
| Control | 60.19 (1.03) | 60.13 (1.05) | ||
| Mood | ||||
| Depression | ||||
| Experimental | 24.71 (7.59) | 24.03 (6.87) | 0.997 | 0.431 |
| Control | 25.38 (8.72) | 25.55 (9.38) | ||
| Anxiety | ||||
| Experimental | 14.57 (3.25) | 13.23 (2.65) | 0.341 | 0.020 |
| Control | 14.31 (4.82) | 14.62 (5.27) | ||
| Objective test performance | ||||
| SCWT interference | ||||
| Experimental | 19.63 (0.93) | 21.07 (0.96) | 0.846 | 0.182 |
| Control | 20.92 (1.09) | 20.25 (1.09) |
CFQ: cognitive failure questionnaire, SCWT: stroop colour word test. Follow-up group differences were analysed using analysis of variance, adjusted for baseline score.
a Interaction effect between time (first follow-up and second follow-up) and group (intervention group and control group).
b Higher score reflect less complaint about executive functioning.
Fig. 2.
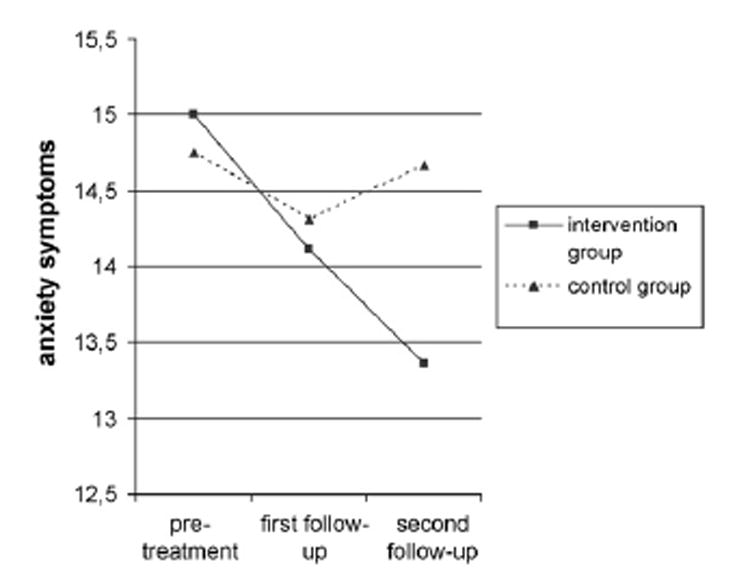
Differences between groups on anxiety symptoms.
Additional analyses were performed adjusting for the small but significant difference in IQ between the two groups. A similar pattern of results was found: participants in the intervention group experienced less annoyance (F(1,61) = 5.22, p = 0.03) and were better able to manage executive failures (F(1, 62) = 4.32, p = 0.04) after the training than did control participants. Again, an interaction effect was found for anxiety symptomatology (F(1, 60) = 6.48, p = 0.01).
4. Discussion and conclusion
4.1. Discussion
The aim of this study was to evaluate a structured course for older adults that included the principles of GMT and psycho-education, using a randomised waiting list control group design. After the intervention, participants in the training group were better able to manage previously reported cognitive failures and were less annoyed by cognitive failures than were participants in the waiting list control group. Participants who had received the intervention reported that they were better able to perform activities according to a plan, to estimate the time needed for an activity, and they were less distracted during an everyday activity. Thus, after being taught to identify situations characterized by a risk of cognitive failure and to state appropriate goals when confronted with such situations, the trained participants appeared to be better able to structure activities in daily life and to work according to a plan. Accordingly, strategies to cope with cognitive dysfunctioning and attitudes toward cognitive problems did improve.
Participants who had received the intervention reported less anxiety symptoms, 7 weeks after the end of the intervention. This effect was not present immediately after the intervention. Instead, the analyses showed that after participants followed the intervention the anxiety symptomatology was reducing. It is possible that an improved ability to structure activities and cope with cognitive complaints may eventually cause a reduction in anxiety symptoms on the long run. This is in line with previous research that demonstrated that cognitive functioning can influence emotional states [40].
The intervention diminished annoyance and improved the management of reported executive problems, but the effect sizes were modest. Levine et al. [15], who used brain injury patients, found that the intervention significantly improved objective cognitive performance (on paper and pencil tests), whereas this improvement was not found in the healthy older adults included in the present study. After the intervention, participants did not improve on an objective test measuring executive functioning. One explanation for this finding is that the older adults in the present study were not as impaired as patients with brain injury, and therefore their capacity for improvement on objective test performance may have been more limited. Another explanation is related to the fact that the intervention group was compared to a waiting list control group. Participants in the waiting list control group did not receive the intervention during the study period, but it is possible that the expectation of the participants assigned tot the waiting list to receive an intervention in the near future may have positive effects on their functioning. This would result in an underestimation of the effect of the intervention. Apart from the modest effect sizes, a second limitation of the study may be the influence of receiving attention and talking about the experienced problems during the intervention. This may have had positive effects on functioning of the participants. Ideally, future studies should include a second control group that received an intervention without the neuropsycholo-gical elements and psycho-education.
The participants of this study were selected on problems with executive functions, such as being chaotic and disorganised, and being often distracted, etc. They all reported more cognitive failures, more annoyance, hindrance and worry about these failures than age-, sex- and education-matched people from the Maastricht aging study. In addition, they were more sensitive to interference on the stroop colour word test. This indicates that the selected group was indeed a group of older adults who experienced cognitive failures and who may be less able to cope with these problems. Based on extensive evaluations by the trainers, it appears to be particularly important to select persons with executive problems because these individuals are more likely to benefit from such a training program. Moreover, people should be motivated and have the intellectual capacity to cope with the information they receive via psycho-education. People with less insight into their functioning may not be able to apply the strategy, in particular the stop stage that requires insight into the problem when cognitive failures occur. In summary, the course is especially suitable for persons with executive problems who have insight in to their functioning and the intellectual capacity to process the information given via psycho-education. It is interesting to investigate in the future the applicability of this intervention to neuropsychological patient groups with these characteristics. In addition, because of the relatively short duration, this intervention could be offered as a pre-training before a dedicated intervention.
4.2. Conclusion
The structured course based on the GMT tested in this study appears to improve the ability of healthy older people who experience cognitive problems to manage executive failures and to be less annoyed with cognitive failures.
4.3. Practice implications
As this neuropsychological intervention was relatively short, with 12 sessions, and because the subjective evaluation of the people after training was quite favourable, the intervention may be considered a valuable contribution to cognitive interventions for older adults. The findings may be important for health care, because many community-dwelling older adults experience cognitive complaints and therefore may seek medical attention unnecessarily. The finding that the training yielded positive effects on the subjective experience of the participants is important, because subjective motivations eventually trigger individuals to seek professional help. Use of the course could prevent people from using the health care system for the relatively modest complaints. Moreover, the fact that executive functions, such as planning activities, performing multiple tasks, and managing novel situations, are among the first functions to decline in older people makes it important to implement an effective intervention that addresses the problems associated with a failure of executive function.
Acknowledgments
We thank Janneke Spauwen, Jaimie Luermans, Lia van de Kooi and Viviane Thewissen for assistance with neuropsy-chological testing. Financial support from the Dutch Research Council is greatfully acknowledged (NWO: 014-91-047).
References
- 1.Van der Linden M, Bredart S, Beerten A. Age-related differences in updating working memory. Brit J Psychol. 1994;85:145–52. doi: 10.1111/j.2044-8295.1994.tb02514.x. [DOI] [PubMed] [Google Scholar]
- 2.Zacks R, Hasher L. Cognitive gerontology and attentional inhibition: a reply to Burke and McDowd. J Gerontol B Psychol Sci Soc Sci. 1997;52:274–83. doi: 10.1093/geronb/52b.6.p274. [DOI] [PubMed] [Google Scholar]
- 3.Persad CC, Abeles N, Zacks RT, Denburg NL. Inhibitory changes after age 60 and their relationship to measures of attention and memory. J Gerontol B Psychol Sci Soc Sci. 2002;57:223–32. doi: 10.1093/geronb/57.3.p223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glass JM, Schumacher EH, Lauber EJ, Zurbriggen EL, Gmeindl L, Kieras DE, Meyer DE. Aging and the psychological refractory period: task-coordination strategies in young and old adults. Psychol Aging. 2000;15:571–95. doi: 10.1037//0882-7974.15.4.571. [DOI] [PubMed] [Google Scholar]
- 5.Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The unity and diversity of executive functions and their contributions to complex ‘‘Frontal Lobe’’ tasks: a latent variable analysis. Cognitive Psychol. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- 6.Grigsby J, Kaye K, Baxter J, Shetterly SM, Hamman RF. Executive cognitive abilities and functional status among community-dwelling older persons in the San Luis Valley Health and Aging Study. J Am Geriatr Soc. 1998;46:590–6. doi: 10.1111/j.1532-5415.1998.tb01075.x. [DOI] [PubMed] [Google Scholar]
- 7.Cahn-Weiner DA, Boyle PA, Malloy PF. Tests of executive function predict instrumental activities of daily living in community-dwelling older individuals. Appl Neuropsychol. 2002;9:187–91. doi: 10.1207/S15324826AN0903_8. [DOI] [PubMed] [Google Scholar]
- 8.Rowe JW, Kahn RL. Successful aging. Gerontologist . 1997;37:433–40. doi: 10.1093/geront/37.4.433. see comments. [DOI] [PubMed] [Google Scholar]
- 9.Duncan J. Disorganisation of behavior after frontal lobe damage. Cognitive Neuropsychol. 1986;3:271–90. [Google Scholar]
- 10.De Jong R. Adult age differences in goal activation and goal maintenance. Eur J Cognitive Psychol. 2001;13:71–89. [Google Scholar]
- 11.Valentijn SAM, Van Hooren SAH, Bosma H, Touw D, Jolles J, Van Boxtel MPJ, Ponds RWHM. The effects of two types of memory training on subjective and objective memory performance in healthy individuals aged 55 years and older: a randomised controlled trial. Patient Educ Couns. 2005;57:106–14. doi: 10.1016/j.pec.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Commissaris K, Verhey FR, Jolles J. A controlled study into the effects of psycho-education for patients with cognitive disturbances. J Neuropsych Clin Neurosci. 1996;8:429–35. doi: 10.1176/jnp.8.4.429. [DOI] [PubMed] [Google Scholar]
- 13.Robertson IH, Levine B. Goal management training. 2000 Unpublished manuscript. [Google Scholar]
- 14.Duncan J, Emslie H, Williams P, Johnson R, Freer C. Intelligence and the frontal lobe: the organization of goal-directed behavior. Cognitive Psychol. 1996;30:257–303. doi: 10.1006/cogp.1996.0008. [DOI] [PubMed] [Google Scholar]
- 15.Levine B, Robertson IH, Clare L, Carter G, Hong J, Wilson BA, Duncan J, Stuss DT. Rehabilitation of executive functioning: an experimental-clinical validation of goal management training. J Int Neuropsychol Soc. 2000;6:299–312. doi: 10.1017/s1355617700633052. [DOI] [PubMed] [Google Scholar]
- 16.Campbell M, Fitzpatrick R, Haines A, Kinmonth A, Sandercock P, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. Brit Med J. 2000;321:694–6. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodwin CJ. Research in psychology: methods and design. New York: John Wiley; 2002. [Google Scholar]
- 18.Wilson BA, Emslie HC, Quirk K, Evans JJ. Reducing everyday memory and planning problems by means of a paging system: a randomised control crossover study. J Neurol Neurosur Psychiat. 2001;70:477–82. doi: 10.1136/jnnp.70.4.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Commissaris CJAM, Ponds RWHM, Jolles J. Subjective forgetfulness in a normal Dutch population: possibilities for health education and other interventions. Patient Educ Couns. 1998;34:25–32. doi: 10.1016/s0738-3991(98)00040-8. [DOI] [PubMed] [Google Scholar]
- 20.Ponds RWHM, Jolles J. Memory complaints in elderly people: the role of memory abilities, metamemory, depression and personality. Educ Gerontol. 1996;22:341–57. [Google Scholar]
- 21.Bolla KI, Lindgren KN, Bonaccorsy C, Bleecker ML. Memory complaints in older adults. Fact or fiction? Arch Neurol. 1991;48:61–4. doi: 10.1001/archneur.1991.00530130069022. [DOI] [PubMed] [Google Scholar]
- 22.Allaire JC, Marsiske M. Well- and ill-defined measures of everyday cognition: relationship to older adults’ intellectual ability and functional status. Psychol Aging. 2002;17:101–15. doi: 10.1037/0882-7974.17.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. J Psychiat Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 24.Merckelbach H, Muris P, Nijman H, de Jong P. Self-reported cognitive failures and neurotic symptomatology. Pers Indiv Differ. 1996;20:715–24. [Google Scholar]
- 25.Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. The cognitive failure questionnaire (CFQ) and its correlates. Brit J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 26.Ponds RW, Commissaris KJ, Jolles J. Prevalence and covariates of subjective forgetfulness in a normal population in The Netherlands. Int J Aging Hum Dev. 1997;45:207–21. doi: 10.2190/MVQ1-WB58-875H-Y4X0. [DOI] [PubMed] [Google Scholar]
- 27.Jolles J, Houx PJ, van Boxtel MPJ, Ponds RWH, editors. Maastricht aging study: determinants of cognitive aging. Maastricht: Neuropsych Publishers; 1995. [Google Scholar]
- 28.Arrindell WA, Ettema JHM. SCL-90. Een multidimensionele psycho-pathologie indicator (the SCL-90. A multidimensional instrument for the assessment of psychopathology) Lisse, The Netherlands: Swets and Zeitlinger; 1986. [Google Scholar]
- 29.Derogatis LR. SCL-90: administration, scoring and procedures manual-I for the r(evised) version. Baltimore: Johns Hopkins School of Medicine, Clinical Psychometrics Research Unit; 1977. [Google Scholar]
- 30.Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–62. [Google Scholar]
- 31.Houx PJ, Jolles J, Vreeling FW. Stroop interference: aging effects assessed with the stroop colour word test. Exp Aging Res. 1993;19:209–24. doi: 10.1080/03610739308253934. [DOI] [PubMed] [Google Scholar]
- 32.Hanninen T, Hallikainen M, Koivisto K, Partanen K, Laakso MP, Riekkinen PJ, Sr, Soininen H. Decline of frontal lobe functions in subjects with age-associated memory impairment. Neurology. 1997;48:148–53. doi: 10.1212/wnl.48.1.148. [DOI] [PubMed] [Google Scholar]
- 33.Luteijn F, van der Ploeg FAE. Handleiding Groninger intelligentietest (GIT) Lisse. The Netherlands: Swets and Zeitlinger; 1983. manual Groningen intelligence test. [Google Scholar]
- 34.De Bie SE. Standaardvragen 1987—voorstellen voor uniformering van vraagstellingen naar achtergrondkenmerken en interviews (toward a standardization of questions concerning demographic variables in population studies) 2. Leiden, The Netherlands: Leiden University Press; 1987. [Google Scholar]
- 35.Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review): report of the quality standards subcommittee of the American academy of neurology. Neurology. 2001;56:1133–42. doi: 10.1212/wnl.56.9.1133. [DOI] [PubMed] [Google Scholar]
- 36.Jolles J, Verhey FR, Riedel WJ, Houx PJ. Cognitive impairment in elderly people. Predisposing factors and implications for experimental drug studies. Drug Aging. 1995;7:459–79. doi: 10.2165/00002512-199507060-00006. [DOI] [PubMed] [Google Scholar]
- 37.Collie A, Maruff P, Darby DG, McStephen M. The effects of practice on the test performance of neurologically normal individuals assessed at brief test–retest intervals. J Int Neuropsychol Soc. 2003;9:419–28. doi: 10.1017/S1355617703930074. [DOI] [PubMed] [Google Scholar]
- 38.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663–94. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 39.Buchner A, Faul F, Erdfelder E. GPOWER: a prior 1-, post hoc- and compromise power analyses for the Macintosh. 2.1. Bonn, Germany: Bonn University; 1992. [Google Scholar]
- 40.Den Hartog M. Cognitive performance in depression: patterns and determinants . Maastricht, The Netherlands: Neuropsych Publishers; 2002. [Google Scholar]


